CAPILLARIES—THE “BRAIN CENTERS” OF TISSUE DEVELOPMENT
THE LARGEST ARTERIES AND VEINS carry fast-moving blood to and from the heart. These blood vessels branch out into smaller ones, which connect to the smallest of all blood vessels, the capillaries. In these tiny vessels, blood flow slows to a crawl, with only enough space for individual blood cells to slide through in single file. Here, the blood cells communicate with the capillaries and the nearby tissue cells to enable oxygen and carbon dioxide exchange through diffusion.
Capillaries, composed mostly of a single layer of lining cells, form intricate webs called vascular beds. These webs are embedded into tissue and bone. They extend into every part of the body and almost every crevice. With tens of billions of capillaries tracing through the human body, these vessels make up 90 percent of all blood vessels by area. Using advanced microscopes, researchers have begun to observe the subtle differences in the microenvironments of these vascular beds in each organ. Also, capillaries are unique to each organ.
Perhaps the most important recent discovery is that capillaries do more than funnel blood, oxygen, and nutrients to every corner of the body. Capillary lining cells are now found to be vital “brain centers” of tissue, stimulating, regulating, maintaining, and inhibiting the stem cells that make up each organ. This concept of capillaries directly influencing the growth of various tissue and bones goes back to Aristotle, who first proposed the notion that blood vessels somehow determine how organs and other tissue develop throughout the body.
But it has not been clear how blood vessels and tissues maintain their intricate relationship, or which first triggers production of the other. Until recently, there appeared to be only a few known functions of the lining cells, most importantly protecting blood flow as cells and signals course through every region of the body.

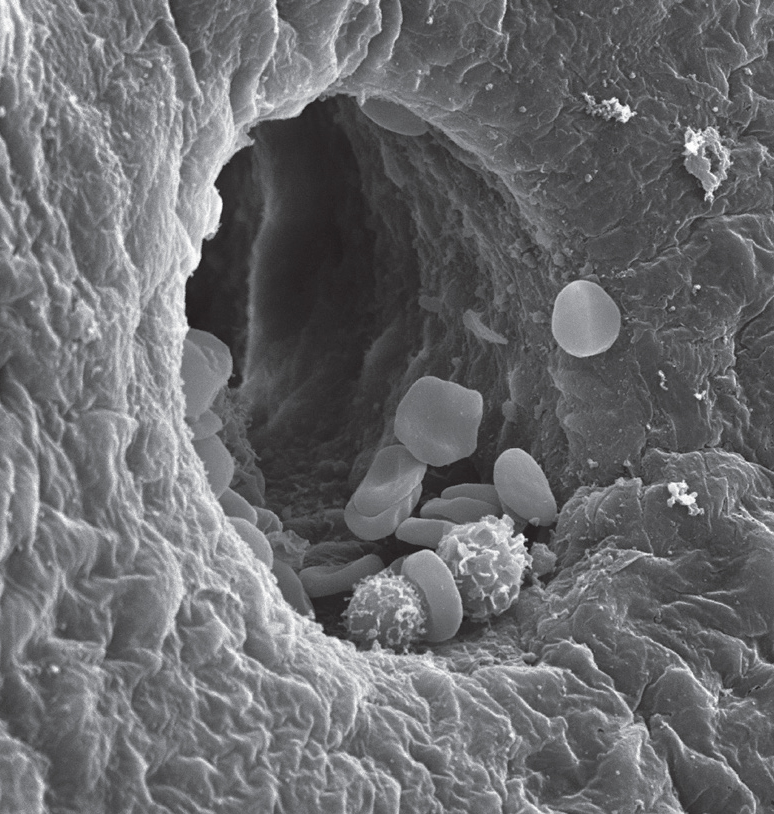
Red blood cell in a capillary, showing the capillary cell’s large nucleus. Electron micrograph. (Dennis Kunkel Microscopy/Science Source)
There is much we don’t yet know about capillaries, but new research is continuously surprising the scientific community. Somehow, capillaries are able to change their own shape for particular situations, such as becoming more tightly bound to adjacent cells, or altering cell properties to allow fluid through. Most of the examples of shape alterations are not well understood. But it is known that in the uterus, progesterone triggers holes in membranes that allow secretions to come out.
It was also recently found that capillaries use large sacs filled with information molecules for communicating with other cells. Launching these sacs can help other cells alter the matrix around blood vessels in unique ways for each tissue. This information helps build the unique capillary niches already observed in liver, bone, lung, and brain.
A CRITICAL BUILDING PARTNER
Scientists are now realizing that capillaries are vital building partners in all phases of tissue growth and also contribute to tissue maintenance. Capillaries send signals to maintain normal metabolism of tissue. They also regulate the growth of all tissue cells, including additional blood vessels when needed. Direction comes from discussions among stem cells, blood cells, tissue cells, and local neurons. When infections occur, capillary signals call for immune-response help and alert T cells into action. When rebuilding tissue, capillaries communicate with stem cells to avoid production of scars from excess fibers.
The Stem Cell Connection
Adult stem cells have been found in numerous areas throughout the body, including in the brain, liver, heart, gut, teeth, skin, and bones. Small groups of these stem cells appear to reside in a protected place, what’s known as a “stem cell niche” of each type of tissue or bone area where they are found. These niches are located next to capillaries, and conversations between them can occur with secreted molecular signals or by direct contact.
Capillaries also can easily send messages into the bloodstream for distant communication with immune cells and bone marrow cells. They somehow understand the precise needs of each diverse organ and either stimulate or inhibit stem-cell activity.
Surprisingly, an unusual type of capillary lining cell is able to transform into a stem cell when necessary. After these capillary cells have turned themselves into tissue stem cells, they then need instruction signals from other original capillary cells to operate.
Capillaries also secrete multiple signals for local tissue cells. Signals inform cells about the shape of the organ they’re in and its precise functions. During tissue rebuilding, signals sent in sequence direct production of three-dimensional spatial patterns. Tissue cells are instructed about the concentrations of cells needed for particular locations to form the exact size and contour of the tissues. Tissue cells don’t just take direction from capillaries; they also express their organ’s needs in two-way conversations among capillaries and stem cells.
Orchestrating the Rebuilding and Maintenance Process
Research shows that discussions among tissue cells and capillaries are needed to grow each organ and to rebuild tissue when damage occurs. Capillary conversations, for example, give specific directions to stem cells for building, maintaining, and rebuilding specific features of every organ. Capillaries determine whether stem cells should be quiet or whether they need stimulation to produce more cells. It’s also been recently found that capillaries are distinct in each organ.
Details of capillary conversations in each type of tissue are just now being discovered—in the brain, bone, liver, pancreas, gut, and muscle. For example, capillary signals send travel routes to immune cells, directing them to infected tissue and determining what goes in and out of the brain with signals to other barrier cells.
These discoveries occurred gradually. First, capillaries were observed helping to construct the pancreas and liver. Capillaries were then found to be vital for the spread of cancers. Further research found that capillaries are vital for normal development of the fetus and for maintenance of adult tissues. All of these discoveries are now known to be based on cellular conversations.
One of the defining characteristics of an organ is the matrix of molecules that sits between its tissue cells. This extracellular scaffolding holds together tissue architectures and produces specific local environments. Capillaries also direct the building of extracellular matrixes around blood vessels with characteristics needed for a specific organ, bone, or other body part.

Unusual rich capillary network of the epididymis. Electron micrograph. (Don W. Fawcett/Science Source)
Another type of cell—the pericyte—wraps around the capillary lining cells. Pericytes can contract like muscles and also take part in capillary discussions throughout the body. Pericytes are vital for the tight barrier around blood vessels in the brain, where the capillary lining cells converse with the pericytes about whether to allow immune cells out of blood vessels and into brain tissue. Both capillaries and pericytes operate independently, but in most types of tissue, capillaries integrate all of the conversations and, ultimately, direct local operations. There is more about pericytes in chapter thirteen.
Understanding How Capillaries Affect Individual Organs
The liver is an amazing organ. When it suffers trauma, it can restore up to 70 percent of its tissue, with capillaries orchestrating the rebuilding process. Capillary signals also stimulate the production of new blood vessels to supply nutrients for new liver tissue. Capillaries somehow understand how large the liver should be. They signal for new stem cells to build tissue until it reaches the exact size, and then inhibition starts.
When the liver can’t regenerate normally, it forms a type of scar tissue called fibrosis, which takes up the space that would have been normal tissue. Unfortunately, capillaries lead the development of the abnormal type of scar tissue as well. In short, if acute injury occurs in an otherwise healthy liver, capillaries stimulate normal growth. With chronic liver disease from alcohol or metabolic syndrome that causes cell exhaustion from constant rebuilding, capillaries direct other pathways to produce abnormal liver fibrosis.
Capillaries also contribute to lung function and tissue development. In the lungs, capillaries are interwoven with respiratory cells that exchange oxygen and carbon dioxide using microvilli protruding from their surfaces. The capillaries and lung cells must be almost touching for the gases to diffuse properly across them. Capillaries engage in a great amount of discourse, using a wide range of signal molecules related to producing the distinctive membranes that sit between capillaries and air space. They also stimulate the production of new lung cells after lung tissue is removed. Elaborate signaling back and forth produces more stem cells for the development of new tissue.
A somewhat similar situation occurs in the pancreas. Capillaries sit near cells that make insulin and are in constant communication about the body’s metabolism through signals in the blood. Capillaries can stimulate regeneration of pancreas cells to help regulate an unbalanced metabolism. Another process turns some of the capillaries into fat cells, and this alters metabolic actions related to fat. These altered cells are similar to stem cells in that they then need direction from normal capillaries.
Specialized sinusoid liver capillary with multiple red blood cells and two white blood cells. Electron micrograph. (Steve Gschmeissner/Science Source)
Capillaries that surround cardiac muscles also can help stimulate the heartbeat with signals. When capillaries sense low oxygen, they produce a particular signal. If heart muscle is damaged by low oxygen, capillaries dramatically increase their activity, stimulating repair, as well as stronger muscle contractions to help continue pumping blood.
Calling for Help
When tissue destruction occurs—caused by chemicals, trauma, low oxygen, or radiation—capillaries working with stem cells respond by calling for particular immune cells for each situation. These immune cells, nomadic in nature, might have to travel a great distance from bone marrow on the other side of the body. Also, signals from the capillaries to the bone marrow might first have to stimulate production of diverse cells needed for the specific rebuilding task.
In fact, capillaries direct the entire operation of getting immune cells to help when needed. During the entire transit of helper cells, the capillaries continue to send messages about the exact site of the problem. They stimulate other local cells along the way to take up the cause and produce factors that help guide the trekkers. These signals allow attachment of traveling cells onto blood vessels to enable movement in a particular direction, even against the flow of blood.
After the traveling blood cells arrive at the precise location, capillaries make sure they are the ones that are needed. When certain, the capillaries send signals to allow the blood cells’ exit from the blood vessel into tissues. Normally, to maintain blood vessel boundaries and keep fluid from seeping out of blood into tissue, capillaries are tightly connected to adjacent cells. For these helper immune cells to enter surrounding tissue, signals alter the capillary junctions, creating a path for cells in the blood to go through. With several more barriers between the blood and tissue in the brain, getting through is more complex.
A PARTNER IN BRAIN DEVELOPMENT
Capillaries are directly involved in the production of all brain cells, just as they are in stimulating stem cells in other organs. While production of new neurons in the brain greatly decreases in adult humans, supportive brain cells are produced in great numbers. (These supportive brain cells, called glia, are explained at length in chapters ten through twelve.)
In a developing fetus, billions of neurons are minted in all regions of the brain, and as life progresses, smaller numbers of new neurons are produced in select locations. In adults, these new neurons support memory centers and turnover of smell neurons. A recent study looked at brains of human adults who had died suddenly and found that up to hundreds of new neurons were produced each day in memory centers, even into old age. However, this study also noted that decreasing blood flow in the very old might make these new neurons somewhat less effective.
It is now known that capillaries sitting next to stem cells are part of the vital process of producing new neurons in the brain, as well as outside the brain in local tissues. In the brain, newly minted neurons stimulated with capillary signals migrate to locations where they are incorporated into active brain circuits. An example of locations outside the brain include the lungs, where capillary signals stimulate stem cells that produce local neurons. Another is the umbilical cord, where capillaries produce a signal necessary to produce new neurons.
Capillaries also stimulate production of supportive brain cells (again, each type detailed in subsequent chapters). Brain lining cells—called choroid lining cells—sit at the critical barrier between blood vessels and cerebrospinal fluid. Capillary lining cells use signals to regulate the stem cells that produce these choroid lining cells, telling the stem cells to either maintain a quiet state or produce more cells for the barrier. These choroid lining cells are discussed in chapter thirteen.
For regeneration of brain tissues after trauma and strokes, capillaries coordinate activity to greatly increase production of signals that nourish the new types of cells needed to clean up and repair damaged brain regions. Signals instruct brain stem cells to travel to particular places for more cell production. Signals include directions for travel and the stimulus to produce more cells. Crosstalk between capillaries and neurons is increased in this situation to regulate growth and energy usage for brain structures.
In the brain and several other organs, capillaries provide three distinct levels of support for producing new cells. In the first level of support, capillaries send signals that alter brain stem cells from a universal type that produces a wide range of cells to a limited type that produces just one particular cell, such as a neuron or lining cell. There are numerous different stem cell types that capillaries stimulate to produce more than a thousand types of neurons and multiple types of supportive brain cells. After signals to produce the limited-edition stem cell, capillaries then provide two additional levels of support.
The second level of support instructs limited-edition stem cells to move to exact locations in order to produce these particular brain cells where they are needed. One example is the production of cells that wrap insulation around axons to determine the speed of electrical signals for neuron circuits. The amount of insulation material—called myelin—is different in each location based on the signal speeds needed for various circuits. Capillaries instruct new limited-edition stem cells to travel to exact locations in the brain to find a particular neuron and produce a supportive brain cell that manufactures the appropriate amount of wrapping on the neuron’s axon.
The third level of stimulation from capillary cells comes when the brain is functioning normally. Capillaries send signals that stimulate maintenance of performance to both stem cells and brain cells.
TALKING WITH BONES
Bone in a normal, healthy body is constantly being remodeled. In the process, solid bone architectures are altered and blood cells are produced in the marrow. Bone builds and breaks down structures in a process directed by two distinct types of capillaries. One type stimulates production of new bone cells, and the other stimulates the bone cells to carve out sinusoid cave environments, where the capillaries reside in the bone. Other stem cells in the marrow participate in producing diverse blood cells. Bone marrow produces all types of blood cells for the entire body, and capillaries are positioned next to the stem cell niche in bone sinuses, where they converse about producing varieties of blood cells.
Capillaries in the bone respond to calls from tissue cells, immune cells, and other capillaries throughout the body seeking particular blood cells to respond to local emergencies. Capillary signals to stem cells can inhibit production when supplies are full and stimulate when more cells are needed. As in the brain, capillaries in bone marrow contribute three levels of instructional support to stem cells when producing the wide variety of blood and immune cells. In the first level, the capillaries initiate the production of more stem cells. The next set of signals limits the stem cell to a particular family of blood cells. The third level triggers specific cells in the lineage or inhibits production of cells that are only rarely needed.
Capillary signals stimulate stem cells for both white and red blood cells. One type of stem cell produces red blood cells and another produces white blood cells (described in chapter two). Stem cells for white blood cells transform into limited types to produce T lymphocytes (described in chapter three) and B lymphocytes. They also produce two lesser-known cells—the natural killer cell, which is similar to T cells but without as many capacities, and a B cell derivative that mass-produces antibodies.
Capillary signals also stimulate another type of white blood cell in the fetus, which travels to the brain. These cells live in the brain throughout adult life as the already mentioned resident immune cells, microglia. Another important cell in the white blood cell lineage is the large mother cell that produces platelets, which are described in the next chapter.
When bone marrow is depleted, perhaps during serious infection, capillaries change gear and send signals to repopulate it. The conversations to repopulate marrow are complex and consist of cascades of multiple signals in sequence. Some signals help avoid stem cell exhaustion, and others produce new stem cells to help. Other signals are global and stimulate production of all cell types at once—lymphocytes and red blood cells. If too many are produced, capillaries send inhibitory factors to shut down production.