MICROBE INFLUENCES ON THE BRAIN
MICROBES CAN AFFECT the brain by directly entering it or with signals from distant regions—most often from the gut. Signals, mostly from bacteria and viruses, can trigger neurons in the gut nervous system to send messages into brain circuits. Alternatively, signals can travel through the blood directly to the brain. Microbes from the gut can reach the brain by traveling in blood and crossing multiple barriers. Also, microbes can be transported along axons inside peripheral neurons to the brain.
Signals from a variety of sources in the gut—microbes, immune cells, lining cells, and food particles—can alter lining cells to allow entrance of microbes into the blood and then later facilitate entrance into brain tissue. While details are not yet clear, research has found potential associations between gut microbe signals and multiple brain problems—stress, depression, autism, schizophrenia, and degenerative brain diseases. For example, as already mentioned, microbes attracted by increased salt levels send signals that alter cognition. Cognition is affected by changes to blood flow and leakiness of vessels, independent of the well-known effect of salt on blood pressure.
Secreted gut microbe products—including neurotransmitters—are particularly influential in the fetus. They affect fetal brain development and, later, mental functions. Neurotransmitters sent from gut microbiota may or may not enter the brain. But microbes produce precursors of neurotransmitters that do enter the brain, affecting emotion circuitry. Without these precursors from gut microbes, major brain neurotransmitter levels are much lower.
Products from gut microbiota affect the brain in other ways. Molecules can alter hormones that affect behavior. Signals can be influential in determining the development of particular immune centers that affect behavior. Microbes can also boost immune functions and decrease the effects of stress. Probiotics, for instance, are becoming more well known as a way to enhance health and general well-being.
Recently, a large number of new types of gut microbe products have been found that could affect chemical compounds in the brain, including peptides, short fatty acids, and fats with attached sugars. This latter group of molecules made up of fats and sugars has an almost infinite number of possible combinations and forms. Bacteria can modify molecules from bile or amino acids in food to produce these new products. Various microbes produce multiple versions of similar new products, so people who eat the same foods can have different results.
MICROBE INFLUENCE ON BEHAVIOR AND BRAIN DEVELOPMENT
Microbe effects on animal brains are studied in laboratories and in the wild. Although more difficult than laboratory studies, observations in the wild show that specific microbe species cause diverse behavioral changes in animals. Laboratory research, mostly in mice, shows the influence that microbe products can have on behavior.
Many microbe species are able to modify behavior of their host animals to their own benefit. Aggressive behavior, for instance, is caused by the rabies virus, which enables viral transmission when an infected animal attacks another. Single-celled parasites in mice can stimulate the animals to become friendly with cats, enabling parasitical transmission to the cats that killed the mice. Research into the same chronic parasitic infection in humans (caused by the parasite Toxoplasma gondii) shows the possibility of correlations with psychiatric illness, such as suicidal ideas and delusions.
Various other effects in the wild have been observed. When one type of fungus infects an insect brain, it makes the insect climb to the top of the plant, where predators eat the insect, thereby spreading the illness. Another fungus influences grasshoppers to go to bodies of water, where the parasite can more easily produce eggs. Other infections make stickleback fish move to cold water, where infection increases and spreads. A virus stimulates crickets to mate as a way to transfer itself into other crickets.
These behaviors in animals are altered by microbes because of specific brain regions the microbes have entered. They can cause aggression, cognitive problems, pain, depression, and suicide. One causes paralysis and seizures. Another causes insomnia. Research with mice in laboratories does not yet show exactly what signals cause such brain effects, but the evidence for this influence is becoming increasingly clear.
When mice are raised without gut microbes, their behavior changes in multiple ways. Without particular microbes, stress hormones are much greater, and when the microbes are reintroduced, mice become normal. Raised without microbes, mice are anxious, not as sociable, and avoid others. If microbes are introduced in adulthood, the mice don’t remember childhood comrades but are sociable with new friends. Normal mice raised with microbes remember these childhood mates.
Distinct bacterial species produce variable amounts of anxiety in mice. On the other hand, particular probiotics were found to decrease anxiety, depression-like behavior, and repetitive behavior. The presence of these microbe colonies increases social function, memory, and cognition. These effects are dependent on the vagus nerve—the longest of the cranial nerves—which stretches from the brain to the gut and appears to be a conduit for these brain changes.
Microbe products also trigger anatomical brain changes. Mice raised without microbes (mostly bacteria) have more holes in the blood-brain barrier throughout life. Specific bacteria restore blood-brain barrier function even when given later in life. Microbe signals to the lining cells of the choroid plexus tighten the barrier to restrict entrance of random particles into the brain. As described in chapter eleven, these choroid cells line the ventricles of the brain. Without these microbe products, the barrier is more open. This implies that ongoing signals from microbes maintain the blood-brain barrier during normal function.
Also, sterilized mice without any microbiota have altered neuronal function. Without these microbes the levels of neurotransmitters decrease, and some neurotransmitters are missing altogether. By adding particular bacteria, neurotransmitters become normalized. Without microbes, blood flow to neurons is altered. Longtime use of antibiotics in mice produces fewer neurons in memory centers, but with probiotics and exercise, neurons increase. Also, with the overuse of antibiotics there is less myelin in some brain regions.
Evidence points to bacterial signals as necessary for brain development, along with signals from host animals’ cells and particular food particles. Excessive fat in diets produces socially isolated children with repetitive behavior. With probiotics, children’s behavior improves, research has shown. Microbes, and bacteria in particular, have various effects at different stages of brain development. Bacterial signals are needed for the early overgrowth of neurons in the fetus before they are pruned. Microbe signals also help with the massive pruning of neurons during the final stages of fetal development. These signals help direct neuron migration and myelin production. Also, without microbes, specific brain regions have the wrong amount of neurons, either too many or too few.
Microbial signals also influence supportive brain cells. They regulate the critical migration of new glial cells in the part of the autonomic nervous system that controls the function of the gastrointestinal tract. Without microbe signals, microglia develop abnormally.
TACTICS FOR ENTERING THE BRAIN
Against great odds, many microbes, including bacteria, viruses, protozoa, and tapeworms, can traverse multiple barriers and enter the nervous system. Each needs dozens of different tricks for the trip. Some attack neurons and others attack glial cells, such as myelin-producing oligodendrocytes. The bacterium that causes leprosy attacks peripheral glial cells, as described in chapter sixteen.
Many microbes trek from the gut into the bloodstream to the brain. Some travel in immune cells that enter the brain. Others are inside neurons and move from the periphery up along axons into the brain. When traveling in the blood, microbes must first cross capillaries, then they still have to invade a continuous layer of pericytes and then a layer of astrocytes to make it across the blood-brain barrier. Only a small fraction of bacteria and viruses can breach this many obstacles.
Microbes use many tactics for their travel into the brain and take advantage of signals created by choroid cells, capillaries, pericytes, and astrocytes. Bacterial appendages allow strong attachment to blood vessels, by reaching through a hole in the outer protective capsule that surrounds a particular bacterium. Appendages grab onto receptors on human cells in multiple places at once, stabilizing against the force of rapidly flowing blood. Some have a dozen varied attachment molecules. Also, signals can alter scaffolding molecules in the human cell, enabling better attachment. Signals can even stimulate choroid cells to help bacteria by altering molecules in the tight junctions of the blood-CSF barrier, thus widening the barrier for entry.
Moreover, choroid cells are tricked by signals to actively transport sacs filled with bacteria into the brain fluid. Signals from T cells, scavenger cells, and microglia mistakenly encourage choroid cells to take up vesicles with microbes inside as if they were general messages. Immune signals can also disrupt the choroid plexus lining with inflammation, which makes it easier for bacteria to cross the barrier. Some bacteria stay inside choroid cells and are able to influence the brain from there, sending inflammatory signals into spinal fluid.
Some microbes can do their work to sabotage the brain without direct entry. For example, the parasite that causes mosquito-borne malaria doesn’t enter the brain but rather lives in red blood cells. From inside the red blood cell, it sends signals that make its host stick to the capillaries near the brain. It then stimulates its red blood cell to send signals that join with messages from other cells, which can cause brain inflammation.
For the trip into the brain, microbes must be able to defend themselves from immune-cell attacks all along the way. They must be able to gather enough food, especially iron in the blood. Inside spinal fluid or brain tissues, microbes experience more attacks. To protect themselves in spinal fluid, bacteria produce proteins that counteract multiple immune confrontations. They also have special resistant capsules and systematic ways to gather iron in cerebrospinal fluid rather than in blood.
VIRUSES CROSSING BRAIN BARRIERS
Multiple viruses can attack the brain—rabies, measles, polio, herpes, and HIV, to name a few. Remarkably, with only a handful of genes, viruses can manipulate the multiple barriers guarding the brain.
Some viruses with only seven genes and ten proteins outmaneuver vastly more complex human cells and enter the brain. Although the first definitive signals used by a viral community have only recently been identified, the complex, evasive approach of viruses responding to human cell attack signals implies elaborate communication. Also, it is known that cells use viruses to deliver their own signals to comrades.
Viruses can attach to lining cells and inject a piece of their genetic material into the cell. HIV and other viruses, like measles, travel inside T cells—the very cells designed to kill them. These infected T cells send signal molecules that cause capillary cells to open the junctions between them, enabling the virus to enter the brain.
Viruses such as HIV and the virus that causes measles are able to stimulate astrocytes to make more cytokines that bring various immune cells and viruses into the brain. Some of these viruses then infect brain cells, such as microglia and neurons. West Nile virus triggers immune cells to stop blood cells from entering the brain. But, paradoxically, a few of the microbes enter the brain during this process, which causes brain infection.
Some viruses live inside neurons and other brain cells. One stays in peripheral nerves and can’t get to the brain. Another enters the brain by traveling along axons and then hibernates in the brain for years. Several viruses are secreted in vesicles from neurons, then microglia eat them. These viruses are broken up into pieces that are presented to T cells, which stops their reproduction. On the other hand, signals from the rabies virus inhibits this immune process.
Some viruses enter neurons in unprotected regions next to muscles. The rabies virus first lives in muscles and meets the axon at the neuromuscular junction. It then travels in a vesicle from the tip of the axon up to the neuron’s nucleus in the brain. Rabies and herpes viruses are surrounded by their own membranes. Because of this envelope, neurons are fooled into considering them as normal transportation sacs and take them in. Viruses without an envelope also fool neurons by hijacking a neuron’s own transport sacs. These sacs can be transported along the axon all the way from the peripheral nervous system to the brain.
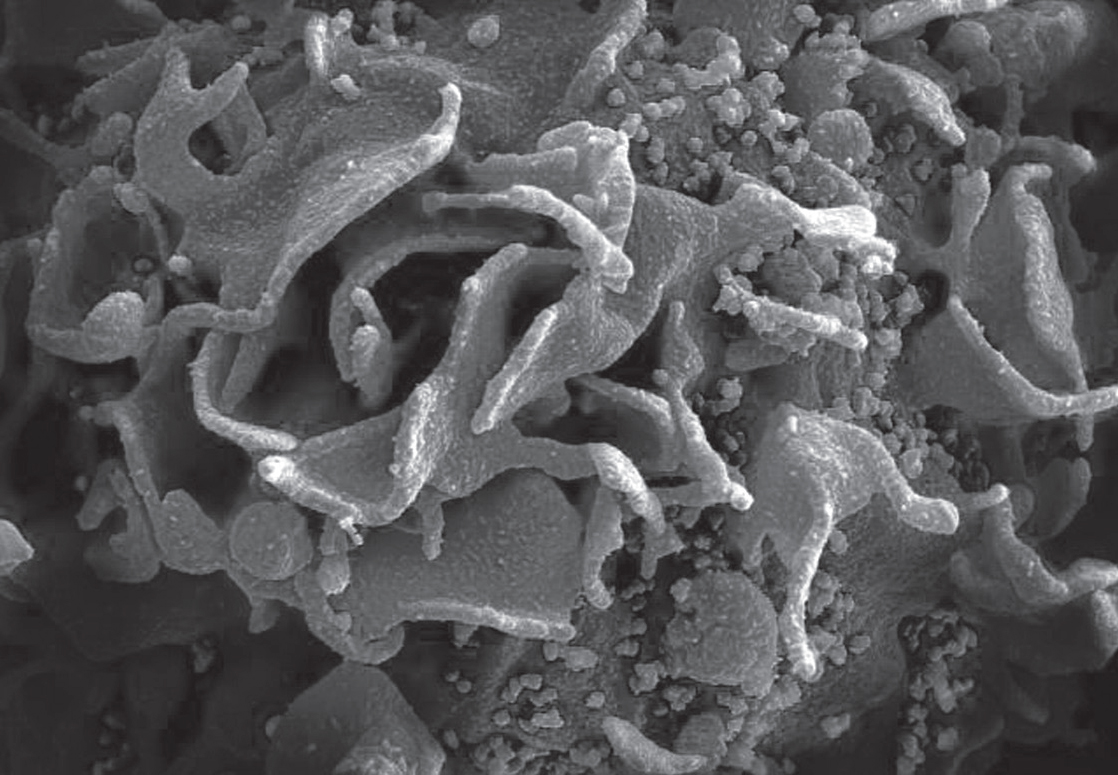
HIV virus on T lymphocytes. Electron micrograph. (Science Source/Science Source/Science Source)
There are other ways, too, that viruses commandeer neurons to help them spread disease. The polio virus is carried by particular motors inside the neuron. One of the most unique techniques is used by the herpes virus, with transport motors that carry cargo along microtubule highways of the spindly axon. Herpes alters the energy mechanism of the transport motor to speed it up. In this way, the virus can move rapidly from nerves near the skin to the neuron’s nucleus. After living in the nucleus for years, when activated, it goes back down the axon the same way to the skin region. Even more surprisingly, herpes travels as a whole virus, or it can be broken into parts for transport and then put back together once at its destination.
Viruses use yet other routes to enter the brain. Some come into contact with neurons near the nose and travel along axons into the brain, where they can affect multiple other circuits. Viruses can start in sensory nerves. They can also live in saliva and be transmitted among humans in this way. Entering neurons in a salivary gland, they travel to the brain. We will continue our discussion on viruses in the next chapter, which is devoted entirely to these incredibly evasive creatures.