MICROBES’ LOVE-HATE RELATIONSHIP WITH CANCER
CLINICAL RESULTS FROM TREATMENT with a new medication for metastatic skin cancer illustrate the importance of microbial conversations. Gut bacteria altered how various types of cancer responded to a medicine that released a brake on immune cell activity. The medication alters “checkpoints” in signal pathways inside immune cells. Checkpoints normally inhibit killer T cells from excessive damaging activity after eliminating microbial infections. These cancer medications block the checkpoints, which release killer T cells to increase the attack on cancer.
But only a quarter of the patients were helped by this medication. Only patients with a particular microbial species in their gut survived, and the others did not. With specific microbes, the medication was able to stimulate more killer T cells, which worked to chase out the cancer. With these specific microbial species, the entire immune system worked better. Without them, T cells didn’t attack the cancer cells because there were more regulatory T cells, not the killer variety. Based on this finding and studies with other medications, future projected treatments will need to include both medications and probiotics that contain particular microbial species.
Chapter eight of the first section described environmental factors that allow cancer to develop, often through damaging DNA. Microbes contribute to these factors in various ways. The more DNA that is damaged, the more cancer can survive. To accomplish this, microbes provide signals that alter cell pathways for DNA repair and cell reproduction. Microbes also stimulate inflammation, which promotes disorder and thus more mutations. Microbe conversations also help cancer cells subvert neighboring cells into helping the cancer spread.
CANCER-CAUSING MICROBES
Cancer-causing microbes can live in humans for many years, but only some people develop cancer from them. This is because multiple concurrent factors are needed. The longer an infection lasts, the more likely new elements will appear to join with microbe signals in producing cancer cells. Developing influences are also affected by evolving conversations among microbes, capillaries, connective cells, lining cells, and immune cells, as well as signaling among comrades in the cancer community.
Twenty percent of cancer types are influenced by microbes, with ten microbial species out of trillions definitely known to cause cancer. But exact mechanisms are only known for three viruses and one bacterium. Among other types of cancer, 10 percent are inherited. The rest are caused by responses to signals from the environment, including some food types, that join microbes in damaging DNA and producing errors in pathways that copy and repair DNA.
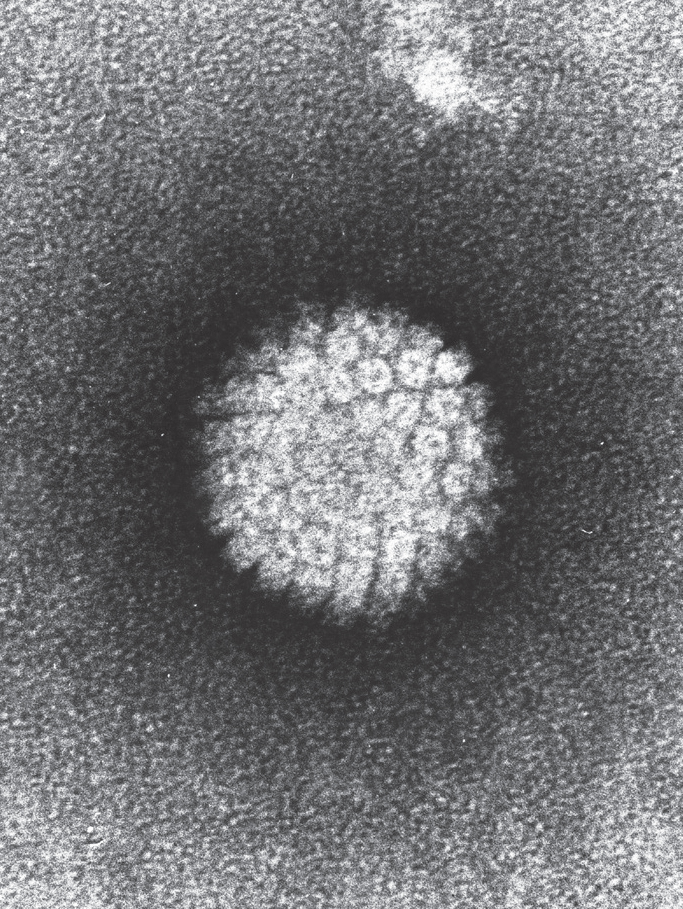
Papilloma virus stimulates cervical cancers, as well as many other types. Electron micrograph. (Laboratory of Tumor Virus Biology/Wikimedia Commons)
Very recently, a hidden cause for colon cancer was found in the collaborative efforts of several microbes. Colon cancer is the third most common cancer in the United States. New research showed two separate types of bacteria in the gut are needed to work together to stimulate the growth of this cancer by influencing immune responses. Either species alone is not sufficient to grow the cancer. More research is needed to decipher exact mechanisms.
Microbes living inside or nearby tumors can help or hurt cancer cells. Microbes can live right next to a tumor and contribute to its expansion, while other microbes will interfere with its growth. A recent clinical observation showed microbes embedded in a cancer colony that was traveling to a metastatic site. There, the microbes helped develop a new, friendly environment to enable the cancer’s further invasion.
INFLAMMATION, MICROBIAL SIGNALS, AND CANCER
Inflammation can lead to cancer, especially if it lasts a long time. Chronic inflammation is a breeding ground for cancer because, along with more microbial signals, it increases DNA breaks while decreasing repair mechanisms. Both microbes and inflammation stimulate reproduction of abnormal cells. During inflammation, microbial signals alter immune cell activity and also manufacture products from food that can lead to cancer. Inflammation in one area can also lead to cancer in another area. For example, gut inflammation can lead to cancer in the liver and prostate.
Altered environments can turn friendly microbes into damaging ones that produce inflammation, which can influence the growth of cancer. In one experiment with mice, researchers introduced two toxins, one that damages DNA and another that breaks gut lining cell barriers. Inflammation and cancer ensued. The toxins changed local microbial behavior, producing new types of waste products that altered the environment and increased inflammation. Bacteria that were previously friendly then latched onto broken surfaces. These bacteria also produced new signals and invaded tissue, which helped the cancer grow.
Surprisingly, a decrease of inflammation can also help produce cancer. Microbes often inhibit immune cells to benefit their own survival. HIV is particularly talented in this way and helps stimulate various types of cancer. Also, bacteria can target receptors on T cells to inhibit their immune attacks against cancer. Multiple new treatments attempt to release this inhibition and restimulate immune activity against cancer.
Altered digestion of food by microbes is integrally related to inflammation and microbial effects on cancer. Several products of metabolism can interact to increase or decrease inflammation. Ordinarily, microbes digest fiber in the gut and produce a molecule that behaves as an immune signal that decreases inflammation. As mentioned already, these microbial molecules from fiber can also help protect against diabetes. With mutations in nearby cells, similar products can do the opposite and increase inflammation as well as stimulate new cancer cells. With different mutations in the cancer, microbes near a cancer colony alter their own metabolism to produce the same molecules, but this time it kills the cancer.
ALTERING CELLULAR PATHWAYS THAT ENABLE CANCER GROWTH
Microbial signals can help cancer cells grow by influencing their internal metabolic pathways. These signals can allow cancer to grow without oxygen in new environments. Microbial signals alter cancer pathways related to cell division so that abnormal cell reproduction is not suppressed. These signals alter DNA repair pathways, increasing mutations that cause stomach and rectal cancer. Another cycle altered by microbial signals stops normal cellular aging and makes cells eternal, an essential element in out-of-control cancer cell reproduction.
Various microbial signals amplify each other’s effects in helping the cancer cause. One microbial signal damages a large multiprotein machine designed to notice and fix DNA breaks. At the same time, microbial proteins directly target DNA and break both strands, increasing mutations. Other signals increase the rate of reproduction of these abnormal cells. Signals also influence neighboring cells to send signals that are helpful to cancer growth. Together, these multiple concurrent actions are a powerful impetus for cancer development.

Helicobacter pylori bacteria are cofactors for stomach cancers. Electron micrograph. (A. Dowsett, Public Health England/Science Source)
One particular bacterial toxin has three separate actions; each action amplifies the others’ effects in encouraging cancer growth. The first action triggers a human cell to pick up the microbe. The second moves it to the internal cell compartment where proteins are manufactured. Bacteria are then altered and sent into the cell nucleus, where the third action breaks DNA and modifies checkpoints of excessive genetic activity. Other concurrent immune signals increase inflammation. Together, these signals allow abnormal cancer cells to rapidly reproduce.
One bacterial species can collaborate to produce stomach cancer by affecting multiple cell pathways at the same time for cell migration and rapid reproduction. One targeted pathway determines when stem cells will make cells that produce stomach cancer. At the same time, a molecule on the bacterial surface stimulates immune signals and more inflammation.
MICROBIAL INTERACTIONS RELATED TO FOOD
Various interactions of microbes with foods can increase the risk of cancer. Mutations of microbes that alter digestion can influence the growth of cancer. Specific microbes can influence the risk of cancer by responding to particular diets and metabolic disturbances, such as obesity. Among diets, high saturated fats especially increase the risk of cancer through interactions with microbes and inflammation. Bile acids and their products also enter into the equation, producing different levels of inflammation.
Microbes can influence cancer by eating and metabolizing food particles—fiber, saturated fats, ethanol, and estrogens in plant materials. Products of metabolism can break lining barriers in the gut, encouraging inflammation and cancer. These molecules can affect lining cell reproduction and can trigger lining cell suicide. Microbial products from fibers produce fatty acids that are signals, some to the brain. Three of these fatty acid signals are noted to produce inflammation. They can also increase gut lining cell reproduction that could potentially lead to cancer. An example of the opposite effect is when they decrease cancerous blood cells in leukemia.
Obesity is an altered metabolic state with increased inflammation in which microbes engage in complex interactions. In general, a good recipe for cancer includes microbes plus inflammation plus obesity. But even without obesity, cancer can be stimulated by a high-fat diet of the wrong kind, along with specific microbes and inflammation. This occurs in duodenal cancer, in which there are also simultaneous mutations of lining cells. Microbes are altered by the high fat and transmit signals to stimulate cancer growth.
CANCER TREATMENTS AND MICROBES
Microbes have multiple interactions with cancer treatments. They can increase the level of medications, causing either toxicity or increased effectiveness. For example, bacteria eat the medication given to pancreatic cancer patients, thus making treatment much less effective. Most cancer drugs have a narrow window of effect versus risk—just enough to kill the cancer cells, but not enough to kill other human cells. Various microbes produce enzymes that alter these risk levels. New research is attempting to calculate microbial effects before treatment.
Medication effects occur with interactions of microbes and immune cells. Cancer therapies now include immune signals, antibodies, and vaccines. They attempt to target pathways that trigger immune responses against cancer. Various microbes affect these treatments by altering local environments. Some antibiotics decrease effectiveness of cancer treatments by altering microbes that are essential to the treatment. Treatment responses are particularly difficult to predict when the environment includes vast amounts of varied microbes.
Microbes can be used as medications themselves. Although a small number of microbes have been used to fight cancer for years, results can vary based on multiple factors that are just now being discovered. Recently, the polio virus was modified to fight a deadly brain cancer. This therapy utilizes the natural ability of the virus to invade cells. Viral genes are altered in a lab so that the virus only attacks cancer cells, not other human cells that are the usual target, such as neurons.
Treatments now try to take advantage of the ways that both immune cells and microbes can work together to destroy cancer cells. Immune cells and microbes can together fight cancer cells, but they also can benefit cancer growth. Examples include transplants of white blood cells that interact with microbes in multiple ways. These interactions are based on the inflammation environment, particular medications, and radiation effects. When lining barriers are disrupted, all bets are off and microbes change their behavior, often unpredictably. Various antibiotics can also drastically alter the situation.
There are just too many factors that are not yet known. Both cancer cells and microbes are much more variable and dynamic than previously thought. They engage in very active conversations in their community that affect their survival. In the future, as details of cancer’s communication with immune cells, tissue cells, and microbes are better understood, new treatments could be developed for each cancer subtype and situation.