Chapter 12
Relieving Your Nasal Allergies
In This Chapter
 Treating your nasal symptoms more effectively
Treating your nasal symptoms more effectively
 Choosing the right medications
Choosing the right medications
 Managing your nasal and eye symptoms
Managing your nasal and eye symptoms
 Getting nosy with nasal products
Getting nosy with nasal products
 Easing itchy, red eyes
Easing itchy, red eyes
M any people with asthma also have allergic rhinitis
The multiple allergens, which commonly trigger the allergic reactions that induce symptoms of allergic rhinitis, also often aggravate or worsen the respiratory symptoms associated with asthma. Remember, your airways, from your nasal passages down to the smallest bronchioles in your lungs, form a continuum.
You can take avoidance measures and allergy-proof your home and office to significantly improve your quality of life by decreasing your exposure to the substances that trigger your allergic reactions and, in most cases, your asthma episodes. (See Chapter 10 for more on allergy-proofing and avoidance measures.) However, because allergens, such as pollens, molds, and dust, are everywhere, complete avoidance can be difficult, if not impossible.
Fortunately, medications are available. If used properly — based on your physician’s advice — medications can prevent or relieve your allergic reactions. In this chapter, I explain how the most common nasal allergy medications work, what potential side effects they have, and how you can make smart choices to control your allergic reactions. Effectively treating those reactions is often the single most important factor in reducing — and in some cases even eliminating — many common respiratory symptoms, thus improving your asthma and your overall quality of life.
Getting Familiar with Pharmacology
The many drugs available for treating nasal allergies have various uses and characteristics. Some allergy medications are designed for one specific purpose, while others have more flexible uses. In general, nasal allergy medications fall into three categories of usage:
 Preventive: If used properly, these types of medications can keep your nasal symptoms from developing. For people who have chronic symptoms of rhinitis, allergic or nonallergic (see Chapter 7), the most effective approach is to use antihistamines (oral or nasal) and nasal corticosteroid medications preventively (see the “Using Nasal Corticosteroids” section, later in this chapter).
Preventive: If used properly, these types of medications can keep your nasal symptoms from developing. For people who have chronic symptoms of rhinitis, allergic or nonallergic (see Chapter 7), the most effective approach is to use antihistamines (oral or nasal) and nasal corticosteroid medications preventively (see the “Using Nasal Corticosteroids” section, later in this chapter).
 Stabilizing: These drugs can often stop a reaction that’s already in process before your immune system can release potent chemical mediators of inflammation, such as histamine and leukotrienes (see Chapter 6), that produce noticeable symptoms.
Stabilizing: These drugs can often stop a reaction that’s already in process before your immune system can release potent chemical mediators of inflammation, such as histamine and leukotrienes (see Chapter 6), that produce noticeable symptoms.
 Relief: Most of the commonly available over-the-counter (OTC) oral antihistamines and decongestants fall into this category. Most people use them to relieve the symptoms of rhinitis after symptoms have occurred. As I explain in this chapter, you’re usually not taking full advantage of medications, such as antihistamines and nasal corticosteroid sprays, if you only use them after your symptoms have started.
Relief: Most of the commonly available over-the-counter (OTC) oral antihistamines and decongestants fall into this category. Most people use them to relieve the symptoms of rhinitis after symptoms have occurred. As I explain in this chapter, you’re usually not taking full advantage of medications, such as antihistamines and nasal corticosteroid sprays, if you only use them after your symptoms have started.
Whether prescribed or purchased OTC, a few basic types of drugs are used to treat nasal allergies, including the following:
 Antihistamines (available in various forms OTC and by prescription)
Antihistamines (available in various forms OTC and by prescription)
 Antihistamine nasal sprays (available by prescription only)
Antihistamine nasal sprays (available by prescription only)
 Decongestants (available OTC, by prescription in oral form, or as nonprescription nasal sprays and drops)
Decongestants (available OTC, by prescription in oral form, or as nonprescription nasal sprays and drops)
 Combinations of antihistamine (OTC and prescription) and decongestant products (available in oral form) are also used for multisymptomatic relief, as I discuss in the section “Two for the Nose: Combination Products”
Combinations of antihistamine (OTC and prescription) and decongestant products (available in oral form) are also used for multisymptomatic relief, as I discuss in the section “Two for the Nose: Combination Products”
 Nasal corticosteroid sprays (available only in prescription form)
Nasal corticosteroid sprays (available only in prescription form)
 Mast cell stabilizer nasal sprays containing cromolyn (available OTC)
Mast cell stabilizer nasal sprays containing cromolyn (available OTC)
 Anticholinergic (drying) nasal sprays (available only in prescription form)
Anticholinergic (drying) nasal sprays (available only in prescription form)
To get the most out of your treatment, take the time to know what each medication can do to relieve your symptoms. I explain the uses and benefits of each product in this chapter.

Blocking Your Histamines: Antihistamines
As the name indicates, antihistamines are medications (available in tablet, capsule, liquid, and nasal spray forms, or by injection) that counter the effects of histamine — a chemical substance released by the body as the result of injury or in response to an allergen. First-generation (sedating) OTC antihistamines have been in use since 1942 and are frequently the first medication option for allergic rhinitis sufferers. I discuss the important differences between OTC and most newer, second-generation (nonsedating or less sedating) antihistamines in the section “Newer antihistamines,” later in this chapter.
Both first- and second-generation antihistamines block the effects of histamine and are most effective in controlling or alleviating symptoms of sneezing, runny nose, and itchy nose, eyes, and throat. However, these medications may not reduce nasal congestion. As a result, they’re frequently combined with a decongestant to relieve symptoms of congestion. In addition, antihistamines produce various side effects, depending on the type of product (OTC or prescription), dosage levels, and course of medication.

Histamine hints

Think of these receptors sites as locks. Histamine inserts itself like a key into the receptor site and triggers the familiar hay fever symptoms of allergic rhinitis. Antihistamines attach to the receptors before histamine gets to them. Because receptors accept only one chemical at a time, if antihistamines block histamine, allergic symptoms won’t be triggered.
A dose of prevention
Many people tend to use antihistamines only as rescue medications. However, these products usually work much better and give greater relief if taken preventively. Taking an antihistamine to relieve your symptoms is like closing the barn door after your horse has already bolted. You’re not going to get that horse back (although by closing the door, you’ll at least prevent any others from escaping).

 If you’re allergic to ragweed pollen, start using your medication at the beginning of August — before ragweed pollens are released in the middle of the month — and continue using the medication until after ragweed season is through. Even if you’re exposed to significant amounts of allergen, you’ll usually experience far fewer symptoms by using this type of preventive approach.
If you’re allergic to ragweed pollen, start using your medication at the beginning of August — before ragweed pollens are released in the middle of the month — and continue using the medication until after ragweed season is through. Even if you’re exposed to significant amounts of allergen, you’ll usually experience far fewer symptoms by using this type of preventive approach.
 If you know that animal dander triggers your allergic rhinitis and you plan to visit someone who has pets, take your antihistamine two to five hours beforehand. Also, remember to continue with the antihistamine after you leave, until you have an opportunity to change your clothing because dander probably will be on your clothes.
If you know that animal dander triggers your allergic rhinitis and you plan to visit someone who has pets, take your antihistamine two to five hours beforehand. Also, remember to continue with the antihistamine after you leave, until you have an opportunity to change your clothing because dander probably will be on your clothes.
First-generation OTC antihistamines
The most common variety of antihistamine medications is first-generation nonprescription products that are available in OTC form. Hundreds of these nonprescription antihistamine products line drugstore and supermarket shelves. Most of these products, however, are just different brand names for a few of the same active ingredients, such as:
 Brompheniramine maleate — the active ingredient in Dimetapp
Brompheniramine maleate — the active ingredient in Dimetapp
 Chlorpheniramine maleate — the active ingredient in Chlor-Trimeton
Chlorpheniramine maleate — the active ingredient in Chlor-Trimeton
 Clemastine fumarate — the active ingredient in Tavist-1
Clemastine fumarate — the active ingredient in Tavist-1
 Diphenhydramine hydrochloride — the active ingredient in Benadryl
Diphenhydramine hydrochloride — the active ingredient in Benadryl
.jpg)
.jpg)
 Many states in the United States consider people who take first-generation OTC antihistamines to be under the influence of drugs. The Federal Aviation Administration (FAA) prohibits pilots from flying if they take OTC antihistamines within 24 hours of flight time. Similar restrictions on the use of first-generation OTC antihistamines apply to truck and bus drivers and operators in other transportation industries.
Many states in the United States consider people who take first-generation OTC antihistamines to be under the influence of drugs. The Federal Aviation Administration (FAA) prohibits pilots from flying if they take OTC antihistamines within 24 hours of flight time. Similar restrictions on the use of first-generation OTC antihistamines apply to truck and bus drivers and operators in other transportation industries.
 Operating heavy machinery or engaging in activities that require alertness, coordination, dexterity, or quick reflexes while taking first- generation OTC antihistamines is dangerous.
Operating heavy machinery or engaging in activities that require alertness, coordination, dexterity, or quick reflexes while taking first- generation OTC antihistamines is dangerous.
 Avoid alcohol, sedatives, antidepressants, or other types of tranquilizers while taking first-generation OTC antihistamines.
Avoid alcohol, sedatives, antidepressants, or other types of tranquilizers while taking first-generation OTC antihistamines.
 First-generation OTC antihistamines can also produce other side effects including the following:
First-generation OTC antihistamines can also produce other side effects including the following:
• Dizziness
• Dryness of mouth and sinus passages
• Gastrointestinal irritation or distress
• Nasal stuffiness
• Urine retention (which can aggravate existing prostate problems)
 Recent studies show that children with allergic rhinitis who take diphenhydramine (the active ingredient in Benadryl) for their symptoms score significantly lower on learning ability tests than children who receive equivalent doses of loratadine (the second-generation OTC antihistamine Claritin).
Recent studies show that children with allergic rhinitis who take diphenhydramine (the active ingredient in Benadryl) for their symptoms score significantly lower on learning ability tests than children who receive equivalent doses of loratadine (the second-generation OTC antihistamine Claritin).

Newer antihistamines

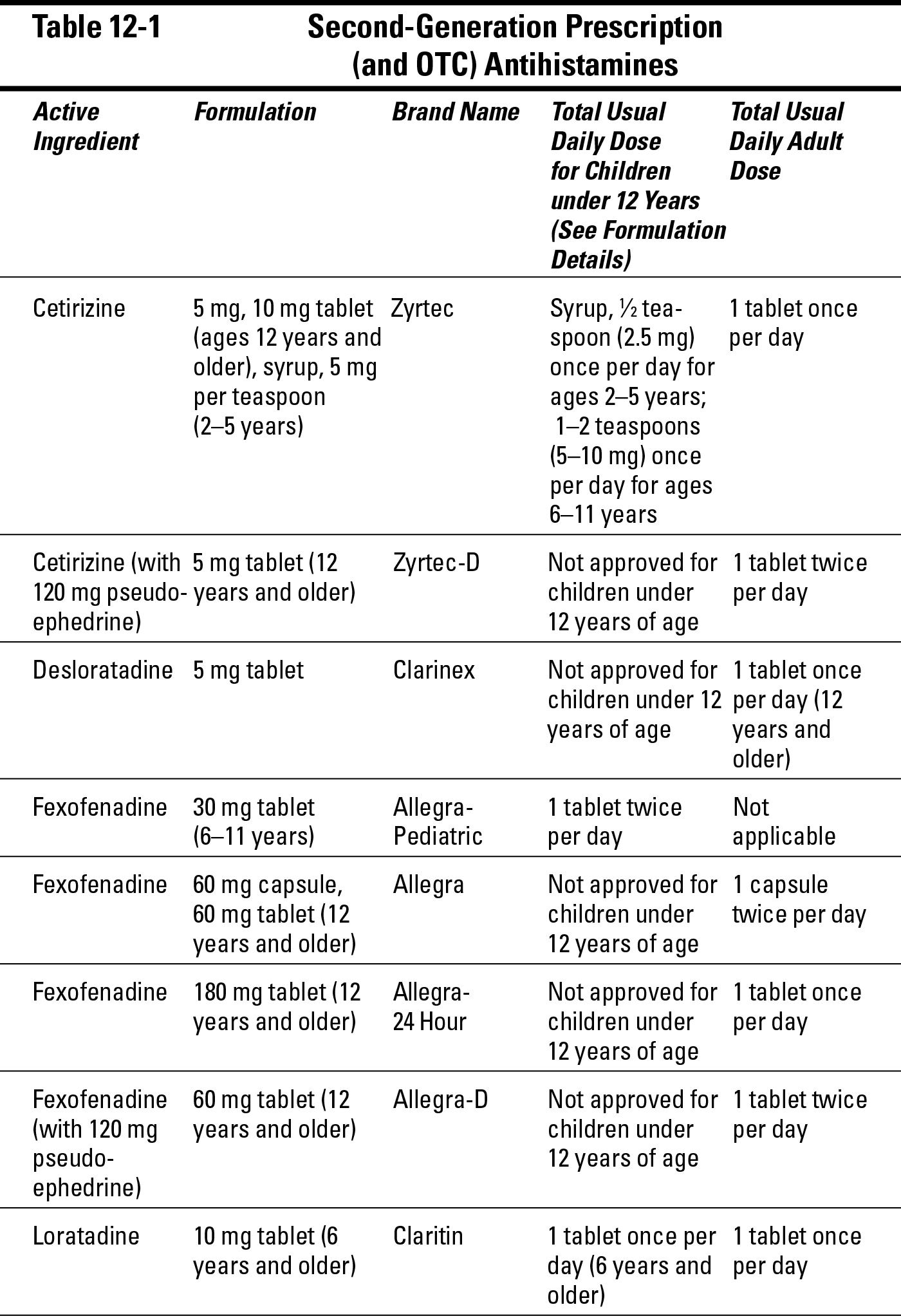
 Not crossing the blood-brain barrier, which means that second-generation products are nonsedating, such as fexofenadine (Allegra), loratadine (Alavert and Claritin) — reclassified by the FDA as an OTC product in 2002 — and desloratadine (Clarinex), or cause only mild sedative effects, as in the case of cetirizine (Zyrtec).
Not crossing the blood-brain barrier, which means that second-generation products are nonsedating, such as fexofenadine (Allegra), loratadine (Alavert and Claritin) — reclassified by the FDA as an OTC product in 2002 — and desloratadine (Clarinex), or cause only mild sedative effects, as in the case of cetirizine (Zyrtec).
 Side effects other than drowsiness, such as dry mouth, constipation, urine retention, or blurred vision, occur less frequently or are much less noticeable with second-generation antihistamines.
Side effects other than drowsiness, such as dry mouth, constipation, urine retention, or blurred vision, occur less frequently or are much less noticeable with second-generation antihistamines.
 Although second-generation antihistamines, whether prescription or OTC (such as loratadine — the active ingredient in Alavert and Claritin), can cost more than most first-generation nonprescription antihistamine products, the more recently developed products work longer and require only one or two doses per day to prevent or relieve allergic rhinitis symptoms.
Although second-generation antihistamines, whether prescription or OTC (such as loratadine — the active ingredient in Alavert and Claritin), can cost more than most first-generation nonprescription antihistamine products, the more recently developed products work longer and require only one or two doses per day to prevent or relieve allergic rhinitis symptoms.
 For the most part, second-generation products work as rapidly as the first-generation drugs. For example, desloratadine (Clarinex), loratadine (Claritin), and cetirizine (Zyrtec) usually start functioning within 30 minutes.
For the most part, second-generation products work as rapidly as the first-generation drugs. For example, desloratadine (Clarinex), loratadine (Claritin), and cetirizine (Zyrtec) usually start functioning within 30 minutes.
 Overall, patients who use second-generation antihistamines usually experience much less disruption or impairment in their daily lives.
Overall, patients who use second-generation antihistamines usually experience much less disruption or impairment in their daily lives.
Because of these factors, second-generation antihistamines (see Table 12-1) can greatly improve the treatment of allergic rhinitis. In my experience, asthma patients are far more likely to stick with second-generation antihistamines for the prescribed course, which often results in a more effective prevention of allergic rhinitis symptoms and a significant improvement of their respiratory symptoms and overall condition.
Seldane and Hismanal issues
.jpg)
Understanding the pros and cons of OTC Claritin and Alavert
The approval of loratadine (Alavert, Claritin) in 2002 as an OTC product may at first glance seem like great news for asthma and allergy sufferers. After all, you can buy medications formulated with loratadine right off the shelf at your local drug store, and those products now cost less than when you had to have your doctor prescribe them. However, since loratadine’s OTC reclassification, many physicians are concerned about some insurers and managed-care providers’ actions to no longer provide coverage of the cost of other second-generation prescription-only antihistamines.

That statement points out that these cost-cutting attempts will reduce access to treatment for millions of patients with asthma and allergies and will also have a negative effect on the health and safety of the general public. If your doctor determines that the most effective drug for your allergies is a second-generation prescription antihistamine (such as Allegra, Clarinex, or Zyrtec), you shouldn’t have to worry whether or not your health plan will cover the cost of that medication. In essence, the ACAAI and AAAAI are trying to make sure that you and your physician will make the decisions about your health in the exam room, rather than by number crunchers in HMO boardrooms. (For more on my concerns about the way managed-care plans can limit patients’ access to the most effective treatments for their conditions, see Chapter 3.)
Dosing a.m. to p.m.
.jpg)
Antihistamines and children

 Loratadine (Claritin): Your doctor can prescribe this medication in a once-a-day kid-friendly syrup or rapidly disintegrating tablet form (Alavert, Claritin RediTabs) for children as young as 6 years.
Loratadine (Claritin): Your doctor can prescribe this medication in a once-a-day kid-friendly syrup or rapidly disintegrating tablet form (Alavert, Claritin RediTabs) for children as young as 6 years.
 Cetirizine (Zyrtec): Your doctor can prescribe this medicine for children as young as 2 years in a once-a-day syrup form.
Cetirizine (Zyrtec): Your doctor can prescribe this medicine for children as young as 2 years in a once-a-day syrup form.
Antihistamine nasal sprays
On the front lines of allergic rhinitis treatment, a recent addition to the antihistamine arsenal in the United States is azelastine hydrochloride. The FDA approved azelastine for use as a nasal spray under the product name Astelin. Remember these basic facts about this nasal spray:
 Azelastine hydrochloride is highly effective for the treatment of seasonal allergic rhinitis symptoms, such as sneezing, runny nose, and itchy nose, eyes, and throat.
Azelastine hydrochloride is highly effective for the treatment of seasonal allergic rhinitis symptoms, such as sneezing, runny nose, and itchy nose, eyes, and throat.
 In contrast to most oral antihistamines, studies show that azelastine often helps reduce nasal congestion (stuffy nose), which may make it particularly useful in dealing with the congestion that often accompanies allergic rhinitis due to late-phase reactions (see Chapter 6).
In contrast to most oral antihistamines, studies show that azelastine often helps reduce nasal congestion (stuffy nose), which may make it particularly useful in dealing with the congestion that often accompanies allergic rhinitis due to late-phase reactions (see Chapter 6).
 You can use azelastine nasal spray in combination therapy with nasal corticosteroid sprays or oral antihistamines in cases that require greater prevention or relief. (See “Using Nasal Corticosteroids,” later in this chapter, for more information on these sprays.)
You can use azelastine nasal spray in combination therapy with nasal corticosteroid sprays or oral antihistamines in cases that require greater prevention or relief. (See “Using Nasal Corticosteroids,” later in this chapter, for more information on these sprays.)
 The recommended dosage for azelastine is two sprays in each nostril twice a day for patients older than 12 years and one spray in each nostril twice a day for children ages 5 to 11 years.
The recommended dosage for azelastine is two sprays in each nostril twice a day for patients older than 12 years and one spray in each nostril twice a day for children ages 5 to 11 years.
 The spray usually starts to take effect within three hours.
The spray usually starts to take effect within three hours.
 The FDA approved azelastine hydrochloride for the treatment of vasomotor rhinitis (nonallergic rhinitis; see Chapter 7) for ages 12 years and older. The recommended dosage is two sprays in each nostril twice a day.
The FDA approved azelastine hydrochloride for the treatment of vasomotor rhinitis (nonallergic rhinitis; see Chapter 7) for ages 12 years and older. The recommended dosage is two sprays in each nostril twice a day.
 Side effects may include a bitter taste and drowsiness in cases of prolonged use.
Side effects may include a bitter taste and drowsiness in cases of prolonged use.
Decongesting Your Nose
People commonly use decongestants to relieve their stuffy noses. You can find decongestants in two forms: systemic decongestants in tablet, capsule, or liquid forms, and decongestants in the form of nasal sprays or nose drops. Unlike antihistamines, no second-generation decongestants have yet been developed.
Oral decongestants
Nonprescription oral decongestants are among the most widely used OTC products in the world, and you can find them in various tablet, capsule, and liquid forms. These medications work by shrinking blood vessels, thus reducing the amount of fluid that leaks into tissues lining the nose, thereby decreasing nasal congestion. The most commonly used decongestants are pseudoephedrine and phenylephrine.
Pseudoephedrine is the most frequently used active ingredient in OTC oral decongestants, such as Sudafed, and in antihistamine-decongestant combinations such as Actifed and Dimetapp. This drug is the “D” (standing for decongestant) in the commonly used second-generation products known as Allegra-D, Claritin-D, and Zyrtec-D.
Remember the following information before using this type of decongestant:
 Systemic decongestants are often combined with other drugs, such as antihistamines, antipyretics (fever reducers), analgesics (pain relievers), antitussives (cough suppressants), or expectorants to provide multisymptom relief for headaches, fever, cough, sleeplessness, and other symptoms of the common cold, flu, allergic rhinitis, and other ailments.
Systemic decongestants are often combined with other drugs, such as antihistamines, antipyretics (fever reducers), analgesics (pain relievers), antitussives (cough suppressants), or expectorants to provide multisymptom relief for headaches, fever, cough, sleeplessness, and other symptoms of the common cold, flu, allergic rhinitis, and other ailments.
 Oral forms of systemic decongestants can cause side effects, such as sleeplessness, nervous agitation, loss of appetite, dryness of mouth and sinuses, difficulty urinating, high blood pressure, and heart palpitations if used consistently over a long period of time.
Oral forms of systemic decongestants can cause side effects, such as sleeplessness, nervous agitation, loss of appetite, dryness of mouth and sinuses, difficulty urinating, high blood pressure, and heart palpitations if used consistently over a long period of time.
.jpg)
 Because of the stimulant effect of oral decongestants, use them cautiously with children. (Believe it or not, most of the parents in my practice aren’t interested in unduly stimulating their kids.)
Because of the stimulant effect of oral decongestants, use them cautiously with children. (Believe it or not, most of the parents in my practice aren’t interested in unduly stimulating their kids.)
Nasal decongestants
Nonprescription decongestant nasal sprays and nose drops can provide quick and effective short-term relief of nasal congestion. However, only use them occasionally, and not for more than three to five days in a row, because long-term or consistent use can result in adverse effects such as nasal rebound (see the nearby sidebar of the same name).
.jpg)
 Naphazoline, found in Privine
Naphazoline, found in Privine
 Oxymetazoline, found in Afrin, Allerest, Dristan Long Lasting, and Sinex Long Lasting
Oxymetazoline, found in Afrin, Allerest, Dristan Long Lasting, and Sinex Long Lasting
 Phenylephrine, found in Neo-Synephrine, Sinex, and Little Noses (one-eighth percent formula for infants and children)
Phenylephrine, found in Neo-Synephrine, Sinex, and Little Noses (one-eighth percent formula for infants and children)
 Xylometazoline, found in Otrivin
Xylometazoline, found in Otrivin
The dosage levels and usage frequency of these medications vary depending on each product’s formulation and method of application. As always, carefully read all product instructions and warnings before using any medication.
The long-lasting products require no more than two doses a day to remain effective, but other short-acting products may work for only one to four hours. Therefore, you may need to apply short-acting products several times a day, as long as you don’t exceed safe dosage levels and don’t use the product continuously without checking first with your physician.
Nasal rebound
No, nasal rebound isn’t a new basketball technique. This condition, more formally known as rhinitis medicamentosa, results from prolonged overuse of OTC decongestant nasal sprays and drops. Overusing such medications can irritate and inflame the mucous membranes in your nose more than before you used the spray, leading to more serious nasal congestion.
Unfortunately, some people increase their use of the product as their congestion worsens, leading to a vicious cycle in which more use produces more congestion. When this happens, higher doses don’t clear the congestion — they only make it worse. To break this vicious cycle, stop using your OTC decongestant. Your doctor may also need to prescribe a short course of oral and/or nasal corticosteroids to clear your nasal congestion and allow you to tolerate the discontinuation of the OTC decongestant.
Remember, the warning on the label that directs you not to use the nasal decongestant spray or drops longer than three to five days really means three to five days and no more. If your stuffy nose persists beyond this point, consider using an oral decongestant.
Two for the Nose: Combination Products
Antihistamines and decongestants can often be more effective in treating the full range of allergic rhinitis symptoms if you combine them in one preparation. You can find numerous oral OTC combination products in tablet, capsule, and liquid forms on store shelves.
An antihistamine, such as chlorpheniramine or brompheniramine, is often combined with a decongestant, such as pseudoephedrine. These products are also frequently combined with other active ingredients — pain relievers, cough suppressants, and fever relievers, for example — to provide relief for a variety of ailments, such as cold and flu symptoms.
The onset of action and dosage frequency vary with different products. Tablets and capsules generally come in two varieties:
 Rapid release: These medications start working quickly but usually lose effectiveness within four hours.
Rapid release: These medications start working quickly but usually lose effectiveness within four hours.
 Sustained release: As you may expect, these products work the opposite way; they act slower but last longer than rapid release medications — usually six to eight hours or longer.
Sustained release: As you may expect, these products work the opposite way; they act slower but last longer than rapid release medications — usually six to eight hours or longer.
Non-drowsy OTC formulas may contain pain relievers, fever reducers, cough suppressants, or other active ingredients for multisymptom relief but don’t contain first-generation antihistamines, which cause drowsiness. Therefore, these formulas don’t usually provide relief from the sneezing, runny nose, and itchy nose, eyes, and throat that are significant symptoms of allergic rhinitis.
.jpg)
Analyzing the upside and downside

If my patient’s condition warrants a combination product, I usually prescribe a nonsedating antihistamine formulated with a decongestant, such as Allegra-D, or possibly a less sedating antihistamine formulated with a decongestant, such as Zyrtec-D. The decongestant (pseudoephedrine) in these products usually doesn’t produce as great a stimulant effect as other decongestants, such as phenylpropanolamine, which the FDA recently removed from the market. As a result, the patient gets the benefits of both a nonsedating antihistamine and a less stimulating decongestant action, minimizing the adverse downer or upper side effects.

One size fits all may not suit your condition
Although combination antihistamine and decongestant products may work well when you need quick relief, the products are less viable for long-term use because you can’t adjust the dosage levels of the individual active ingredients. Each dose, whether in tablet, capsule, or liquid form, delivers the same amount of antihistamine and decongestant (as well as other active ingredients) to your system whether you need relief from one symptom or the full range of ailments.
.jpg)
Using Nasal Corticosteroids


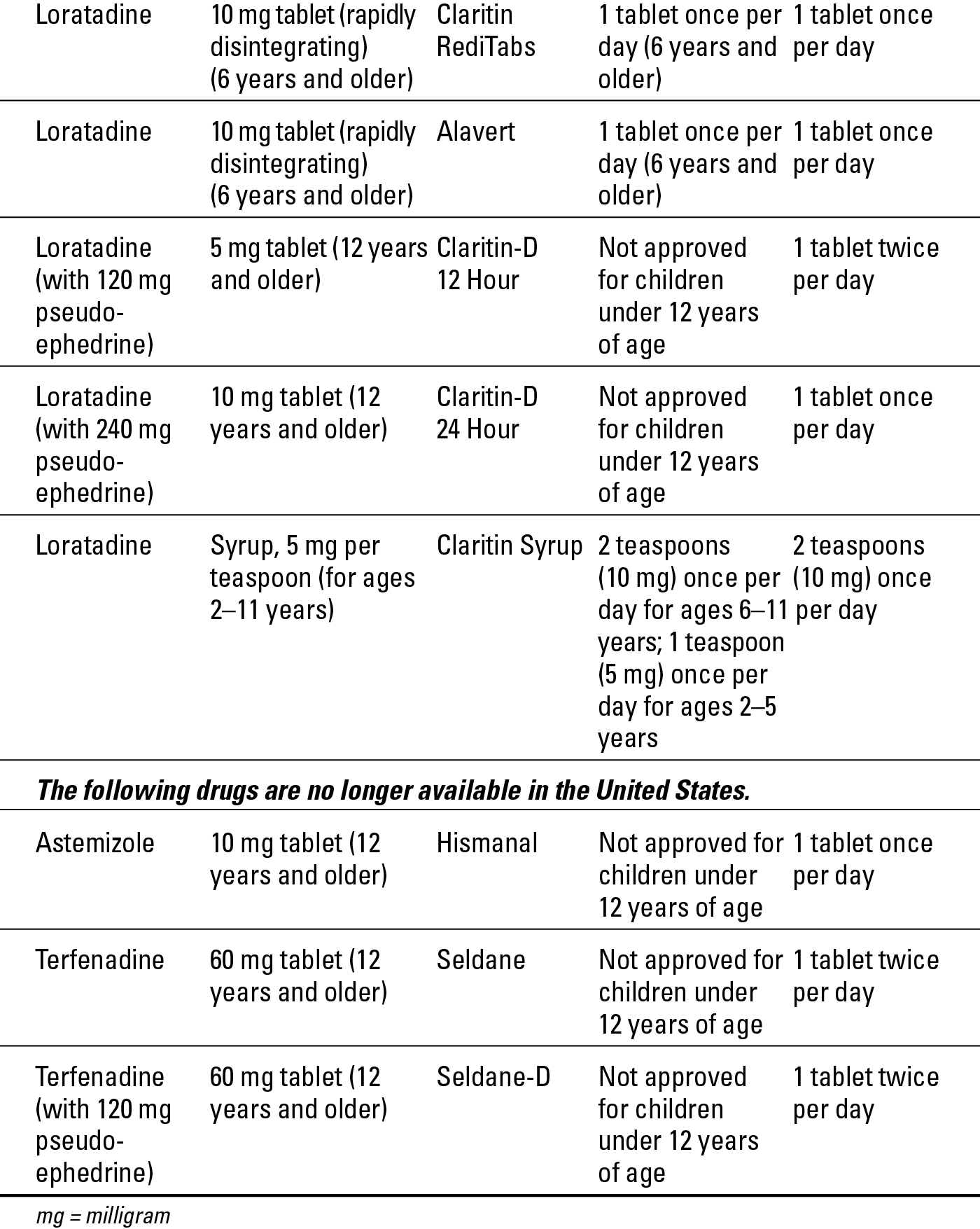
The spray is available by prescription only, and is administered by an aqueous (non-CFC propellant) mechanical pump. The following information can help you and your doctor decide whether nasal corticosteroids can work for you:
 Nasal corticosteroid sprays suppress the inflammation of nasal passages, thereby clearing your nose for easier breathing.
Nasal corticosteroid sprays suppress the inflammation of nasal passages, thereby clearing your nose for easier breathing.
 Nasal corticosteroid sprays are most effective if you use them daily as preventive medications. For a guide to safe dosage levels, see Table 12-2.
Nasal corticosteroid sprays are most effective if you use them daily as preventive medications. For a guide to safe dosage levels, see Table 12-2.
Never exceed dosage levels with these products to minimize the possibility of the medication causing systemic side effects, such as those associated with oral corticosteroids.
 Nasal corticosteroid sprays provide gradual relief of allergic rhinitis symptoms. Initially, you may need to use the medication for several days before the spray suppresses the inflammation. Full effectiveness may require two to three weeks of daily application.
Nasal corticosteroid sprays provide gradual relief of allergic rhinitis symptoms. Initially, you may need to use the medication for several days before the spray suppresses the inflammation. Full effectiveness may require two to three weeks of daily application.
 Only use nasal corticosteroids if your nose is clear enough for the spray to penetrate. If your nose is seriously congested, you may need to use a nasal decongestant for only the first three to five days just prior to administering the nasal corticosteroid spray.
Only use nasal corticosteroids if your nose is clear enough for the spray to penetrate. If your nose is seriously congested, you may need to use a nasal decongestant for only the first three to five days just prior to administering the nasal corticosteroid spray.
 In order to prevent injuring your septum (the bone that divides the nose into two nostrils), direct the spray away from the septum and slightly in the direction of your ears. You may even want to spray the product once in the air to judge the force of the spray before using it in your nose.
In order to prevent injuring your septum (the bone that divides the nose into two nostrils), direct the spray away from the septum and slightly in the direction of your ears. You may even want to spray the product once in the air to judge the force of the spray before using it in your nose.
 Using an aqueous (AQ) formulation of a nasal corticosteroid, because of its gentler action on the nasal lining, can often minimize the typical adverse side effects of nasal corticosteroid sprays, such as nasal irritation, burning, drying, and nosebleeds.
Using an aqueous (AQ) formulation of a nasal corticosteroid, because of its gentler action on the nasal lining, can often minimize the typical adverse side effects of nasal corticosteroid sprays, such as nasal irritation, burning, drying, and nosebleeds.
.jpg)

Steroids to avoid
Although nasal corticosteroid sprays are highly effective and generally safe for both adults and children when administered under a physician’s care, using other forms of steroids is less advisable and potentially unsafe. The following steroids are potentially harmful to you:
 Oral corticosteroids: I advise using quick bursts of short-acting oral steroids (such as prednisone or methylprednisolone) only in cases of severe nasal rebound or nasal polyps, where a decongestant nasal spray can’t penetrate sufficiently to decongest your nose. In such cases, you may require a short course of oral corticosteroids to sufficiently clear your congestion so you can use a nasal corticosteroid spray.
Oral corticosteroids: I advise using quick bursts of short-acting oral steroids (such as prednisone or methylprednisolone) only in cases of severe nasal rebound or nasal polyps, where a decongestant nasal spray can’t penetrate sufficiently to decongest your nose. In such cases, you may require a short course of oral corticosteroids to sufficiently clear your congestion so you can use a nasal corticosteroid spray.
 Intranasal injections: Cortisone shots into the nose aren’t appropriate treatment for allergic rhinitis because of their potential for serious side effects, including vision disturbances and possibly even blindness.
Intranasal injections: Cortisone shots into the nose aren’t appropriate treatment for allergic rhinitis because of their potential for serious side effects, including vision disturbances and possibly even blindness.
Cromolyn Sodium
Cromolyn sodium, an anti-inflammatory OTC nasal spray, may be highly effective in controlling symptoms of allergic rhinitis when you use it properly. (You can find this medicine under the brand name Nasalcrom.) Cromolyn sodium stabilizes mast cells, thereby preventing the release of histamine and other chemical mediators that can cause nasal inflammation.
To help determine whether cromolyn sodium nasal spray might work for you, check out these facts about its recommended use and effectiveness:
 Cromolyn sodium is most effective if you start using it two to four weeks before exposure to allergens. In cases of occupational allergic rhinitis or of limited exposure to allergens, using the spray immediately prior to an isolated, single, allergen exposure (before mowing the lawn or visiting a home with pet), if your nasal passages aren’t already congested, may also provide some relief.
Cromolyn sodium is most effective if you start using it two to four weeks before exposure to allergens. In cases of occupational allergic rhinitis or of limited exposure to allergens, using the spray immediately prior to an isolated, single, allergen exposure (before mowing the lawn or visiting a home with pet), if your nasal passages aren’t already congested, may also provide some relief.
 If allergic rhinitis symptoms are already present, you may need a short course of a combination antihistamine-decongestant for the first few days that you use cromolyn sodium.
If allergic rhinitis symptoms are already present, you may need a short course of a combination antihistamine-decongestant for the first few days that you use cromolyn sodium.
 Because cromolyn sodium has an excellent safety profile and produces no significant side effects, doctors may often prescribe it for children and pregnant women.
Because cromolyn sodium has an excellent safety profile and produces no significant side effects, doctors may often prescribe it for children and pregnant women.
 You can purchase cromolyn sodium in a metered spray form. The recommended dosage for adults and children older than 6 is one spray in each nostril, three to six times per day at regular intervals. Only administer cromolyn sodium to children between 2 and 6 years of age under the supervision of a doctor.
You can purchase cromolyn sodium in a metered spray form. The recommended dosage for adults and children older than 6 is one spray in each nostril, three to six times per day at regular intervals. Only administer cromolyn sodium to children between 2 and 6 years of age under the supervision of a doctor.
Skier’s nose
Ever notice how often skiers blow their noses? When I was training at National Jewish Hospital in Denver, I managed to get to the ski slopes occasionally. When I did, I noticed many boxes of tissues at the bottom of the ski lifts. As I discovered, the tissue boxes were there because of what people call skier’s nose, which is triggered by cold air and is symptomatic of vasomotor rhinitis (see Chapter 7).
I’ve since found that Atrovent Nasal Spray works well to prevent skier’s nose as well as jogger’s nose, if you use it before being exposed to cold air, and also for treatment after symptoms appear. However, doctors also use anticholinergic eye drops similar to ipratropium bromide (the active ingredient) to dilate patients’ eyes, so make sure that you keep the spray away from your eyes or you won’t see that mogul coming right at you.
Reducing Mucus with Anticholinergic Sprays

Some basic facts about anticholinergic sprays include
 Ipratropium bromide effectively reduces runny nose, as seen in conditions such as vasomotor (nonallergic) rhinitis (see the nearby “Skier’s nose” sidebar) or the common cold.
Ipratropium bromide effectively reduces runny nose, as seen in conditions such as vasomotor (nonallergic) rhinitis (see the nearby “Skier’s nose” sidebar) or the common cold.
 Ipratropium bromide has little effect on other allergic rhinitis symptoms, such as stuffy nose, sneezing, or itchy nose.
Ipratropium bromide has little effect on other allergic rhinitis symptoms, such as stuffy nose, sneezing, or itchy nose.
 Your doctor can prescribe Atrovent Nasal Spray in two strengths — 0.03 percent for relief of runny nose associated with allergic and nonallergic rhinitis in adults and children older than 6, and 0.06 percent for relief of runny nose associated with the common cold in adults and children older than 12.
Your doctor can prescribe Atrovent Nasal Spray in two strengths — 0.03 percent for relief of runny nose associated with allergic and nonallergic rhinitis in adults and children older than 6, and 0.06 percent for relief of runny nose associated with the common cold in adults and children older than 12.
 Spray two sprays per nostril two to three times per day (0.03 percent) or three or four times per day (0.06 percent) at regular intervals for the recommended dosage.
Spray two sprays per nostril two to three times per day (0.03 percent) or three or four times per day (0.06 percent) at regular intervals for the recommended dosage.
Treating Rhinitis with Leukotriene Modifiers
Leukotrienes play a significant role in asthma attacks. These chemicals, found in the mast cells that line the airways of the lungs and nose, enhance mucus production, constrict the bronchial passages, and promote further inflammation of the respiratory lining by attracting additional inflammatory cells into the airways.
Leukotriene modifiers, such as montelukast (Singulair) and zafirlukast (Accolate), approved for the treatment of asthma (see Chapter 15) are relatively newer drugs that competitively block leukotriene activity at the receptor site, thus decreasing the amount of mucus generated by exposure to allergens.
Studies have shown that leukotriene modifiers may effectively treat patients whose allergic rhinitis symptoms don’t respond solely to antihistamines. If you’re in that category, ask your doctor whether leukotriene modifiers may work for you. One of these drugs, Singulair, which the FDA recently approved for treatment of allergic rhinitis, also shows promise in treating symptoms of allergic conjunctivitis.
Keeping an Eye out for Allergic Conjunctivitis
Allergic conjunctivitis often coexists with allergic rhinitis. In fact, most of the same allergens involved in allergic rhinitis can trigger allergic conjunctivitis. Characteristic symptoms of this ailment include redness of the eyes and the underside of the eyelids, and swollen, itchy, and watery eyes.
Because the mechanisms of allergic rhinitis and allergic conjunctivitis are similar, conjunctivitis is often treated with some of the same types of drugs used to control rhinitis in solutions specifically formulated for safe use in the eye. Treatment can include
 Prescription antihistamines: Two newer second-generation prescription antihistamines, levocabastine (Livostin) and emedastine (Emadine), appear to be more effective than OTC antihistamines for the treatment of allergic conjunctivitis. Normal recommended dosage for both of these products is one drop per eye up to four times a day for up to two weeks.
Prescription antihistamines: Two newer second-generation prescription antihistamines, levocabastine (Livostin) and emedastine (Emadine), appear to be more effective than OTC antihistamines for the treatment of allergic conjunctivitis. Normal recommended dosage for both of these products is one drop per eye up to four times a day for up to two weeks.
 OTC decongestants: Products include Clear Eyes, Clear Eyes ACR, Visine A.C., Visine L.R., Visine Moisturizing, and Visine Original.
OTC decongestants: Products include Clear Eyes, Clear Eyes ACR, Visine A.C., Visine L.R., Visine Moisturizing, and Visine Original.
 Combinations of OTC antihistamines and decongestants: Product names include Naphcon-A, Vasocon-A, Ocuhist, Prefrin, and VasoClear.
Combinations of OTC antihistamines and decongestants: Product names include Naphcon-A, Vasocon-A, Ocuhist, Prefrin, and VasoClear.
 Mast cell stabilizers: This group of medications inhibits mast cells from releasing chemical mediators of inflammation, thus potentially preventing allergic symptoms from developing. These types of eye drop products include
Mast cell stabilizers: This group of medications inhibits mast cells from releasing chemical mediators of inflammation, thus potentially preventing allergic symptoms from developing. These types of eye drop products include
• Cromolyn sodium (Crolom, Opticrom): As I mention earlier in the chapter, cromolyn sodium works best if you use it preventively, prior to allergen exposure. Likewise, administer it on a regular basis, four times a day. For infrequent allergen exposure (when visiting someone with pets, for example), use cromolyn sodium immediately before you visit. This product has also demonstrated some effectiveness in treating forms of vernal conjunctivitis (a chronic eye condition that can cause severe burning and intense itching and marked sensitivity to bright light).
• Nedocromil sodium (Alocril): This medication, already available in a metered-dose inhaler (MDI) formulation for the treatment of asthma (Tilade), has recently been approved in the United States as an ophthalmic solution. Your doctor can prescribe it for itching eyes associated with allergic conjunctivitis. He also can prescribe it for children as young as 3. This product provides effective relief of both the early and late-phase allergic response (see Chapter 6). The normal dosage for Alocril is one to two drops in each eye twice per day.
• Lodoxamide (Alomide): This drug isn’t approved for use specifically for allergic conjunctivitis, but it has shown some effectiveness in clinical trials as a treatment for vernal conjunctivitis. Normal dosage is one to two drops per eye, four times per day, for up to three months.
 Nonsteroidal anti-inflammatory drugs (NSAIDs): Ketorolac (Acular) is a type of NSAID that can relieve the itching of seasonal allergic conjunctivitis. Normal dosage is one drop per eye, four times per day.
Nonsteroidal anti-inflammatory drugs (NSAIDs): Ketorolac (Acular) is a type of NSAID that can relieve the itching of seasonal allergic conjunctivitis. Normal dosage is one drop per eye, four times per day.
 Combination antihistamine and mast cell stabilizer: The most recent additions to allergic conjunctivitis eye products are olapatadine (Patanol), ketotifen (Zaditor), azelastine (Optivar), and epinastine (Elestat), which are available by prescription in the United States. The normal recommended dosage for Patanol is one drop in each affected eye twice per day, at an interval of six to eight hours. For Zaditor, the recommended dosage is one drop in each eye twice daily, every eight to twelve hours. The recommended dosage for Optivar and also for Elestat is one drop in each eye twice a day.
Combination antihistamine and mast cell stabilizer: The most recent additions to allergic conjunctivitis eye products are olapatadine (Patanol), ketotifen (Zaditor), azelastine (Optivar), and epinastine (Elestat), which are available by prescription in the United States. The normal recommended dosage for Patanol is one drop in each affected eye twice per day, at an interval of six to eight hours. For Zaditor, the recommended dosage is one drop in each eye twice daily, every eight to twelve hours. The recommended dosage for Optivar and also for Elestat is one drop in each eye twice a day.
.jpg)

If you experience severe allergic conjunctivitis, your doctor may prescribe an oral antihistamine, eye drops, and/or a combination of two different eye drop products for maximum relief of your symptoms.