Chapter 13
Treating Your Ear, Nose, and Throat Symptoms
In This Chapter
 Knowing the complications of untreated or poorly managed allergies
Knowing the complications of untreated or poorly managed allergies
 Diagnosing sinus and ear infections
Diagnosing sinus and ear infections
 Clearing the nosy road to your ears and sinuses
Clearing the nosy road to your ears and sinuses
B ecause many people refer to allergic rhinitis as hay fever,sinusitisotitis media
Other conditions, such as tonsillitis (an inflammation of the tonsils), adenoid disease, and chronic cough can also be worsened by postnasal drip (nasal discharge that trickles down the back of your throat). This characteristic symptom of allergic rhinitis, which usually increases in severity when the ailment is poorly managed, can result in the spread of bacteria-laden mucus that irritates and/or infects the throat’s lining.
In addition, ineffectively treated allergic rhinitis and resulting postnasal drip can also adversely affect asthma patients with gastroesophageal reflux disease (GERD). This digestive disorder, which is the third most common cause of chronic cough in North America, is a trigger of asthma symptoms in a large number of asthmatics, especially in cases of nonallergic, adult-onset asthma. (See Chapter 5 for a more extensive discussion on GERD.)
This chapter explains the causes and symptoms of sinusitis and otitis media, and the appropriate methods of preventing and treating these ailments.
Complicating Your Allergies and Asthma: Sinusitis
If you’ve ever had cold or nasal symptoms that didn’t seem to go away, you may have actually been suffering from a form of sinusitis. This often painful condition develops as a result of swollen nasal and sinus passages that frequently result from allergic rhinitis. Many asthma patients often confuse sinusitis symptoms with the symptoms of a cold, flu, or allergy.
Sinusitis is one of the most common health problems in the United States. Current estimates are that sinusitis affects 35 million people each year. Because of the congestion and discomfort that sinusitis causes, it’s one of the most common reasons for doctor visits in the United States.

Recognizing common causes
In a significant number of sinusitis cases, allergic rhinitis precedes the start of a sinus infection. Research shows that more than half of all children in the United States who receive treatment for sinusitis also have allergic rhinitis.

Other factors (you may have one or more of these) that can also increase your chances of developing sinusitis include
 Upper respiratory viral infections: Viruses, such as those associated with the common cold, are the most frequent causes of sinusitis.
Upper respiratory viral infections: Viruses, such as those associated with the common cold, are the most frequent causes of sinusitis.
 Bacteria: The same family of germs that can cause acute otitis media (Streptococcus pneumonia, Haemophilus influenza, Moraxella catarrhalis) can cause acute bacterial sinusitis. Unlike viral infections, this type of sinusitis responds to antibiotic therapy.
Bacteria: The same family of germs that can cause acute otitis media (Streptococcus pneumonia, Haemophilus influenza, Moraxella catarrhalis) can cause acute bacterial sinusitis. Unlike viral infections, this type of sinusitis responds to antibiotic therapy.
 Fungal: This type of sinusitis infection can develop in otherwise healthy patients who have been on long-term antibiotic treatment or have been taking oral corticosteroids on a chronic basis. Aspergillus is the most common fungus that causes these types of cases and is also frequently implicated in cases of allergic fungal sinusitis. Characteristic signs and symptoms of this recurring fungal infection, which can often affect individuals with allergic rhinitis and/or asthma, are sinus infections and nasal polyps (growths in the nose).
Fungal: This type of sinusitis infection can develop in otherwise healthy patients who have been on long-term antibiotic treatment or have been taking oral corticosteroids on a chronic basis. Aspergillus is the most common fungus that causes these types of cases and is also frequently implicated in cases of allergic fungal sinusitis. Characteristic signs and symptoms of this recurring fungal infection, which can often affect individuals with allergic rhinitis and/or asthma, are sinus infections and nasal polyps (growths in the nose).
 Nasal rebound: Overuse of OTC nasal decongestants can also predispose you to sinusitis. (See Chapter 12 for more information.)
Nasal rebound: Overuse of OTC nasal decongestants can also predispose you to sinusitis. (See Chapter 12 for more information.)
 Anatomical obstructions: Nasal polyps, other growths, enlarged adenoids (particularly in children), and a deviated nasal septum (the great divide between the nostrils — see Chapter 7 for more details) can increase your chances of developing sinusitis.
Anatomical obstructions: Nasal polyps, other growths, enlarged adenoids (particularly in children), and a deviated nasal septum (the great divide between the nostrils — see Chapter 7 for more details) can increase your chances of developing sinusitis.
 Other diseases: Patients with cystic fibrosis, in which abnormally thick mucus is produced and the function of the cilia (tiny hair-like projections of certain types of cells that sweep debris-laden mucus through the airways) is impaired, frequently suffer from sinus infections. In addition, AIDS and other immune-deficiency diseases often weaken the body’s defenses to the point where bacteria and viruses can cause many types of infections, including sinusitis. These patients with compromised immune systems may be particularly vulnerable to various forms of fungal sinus infections.
Other diseases: Patients with cystic fibrosis, in which abnormally thick mucus is produced and the function of the cilia (tiny hair-like projections of certain types of cells that sweep debris-laden mucus through the airways) is impaired, frequently suffer from sinus infections. In addition, AIDS and other immune-deficiency diseases often weaken the body’s defenses to the point where bacteria and viruses can cause many types of infections, including sinusitis. These patients with compromised immune systems may be particularly vulnerable to various forms of fungal sinus infections.
Sinus science

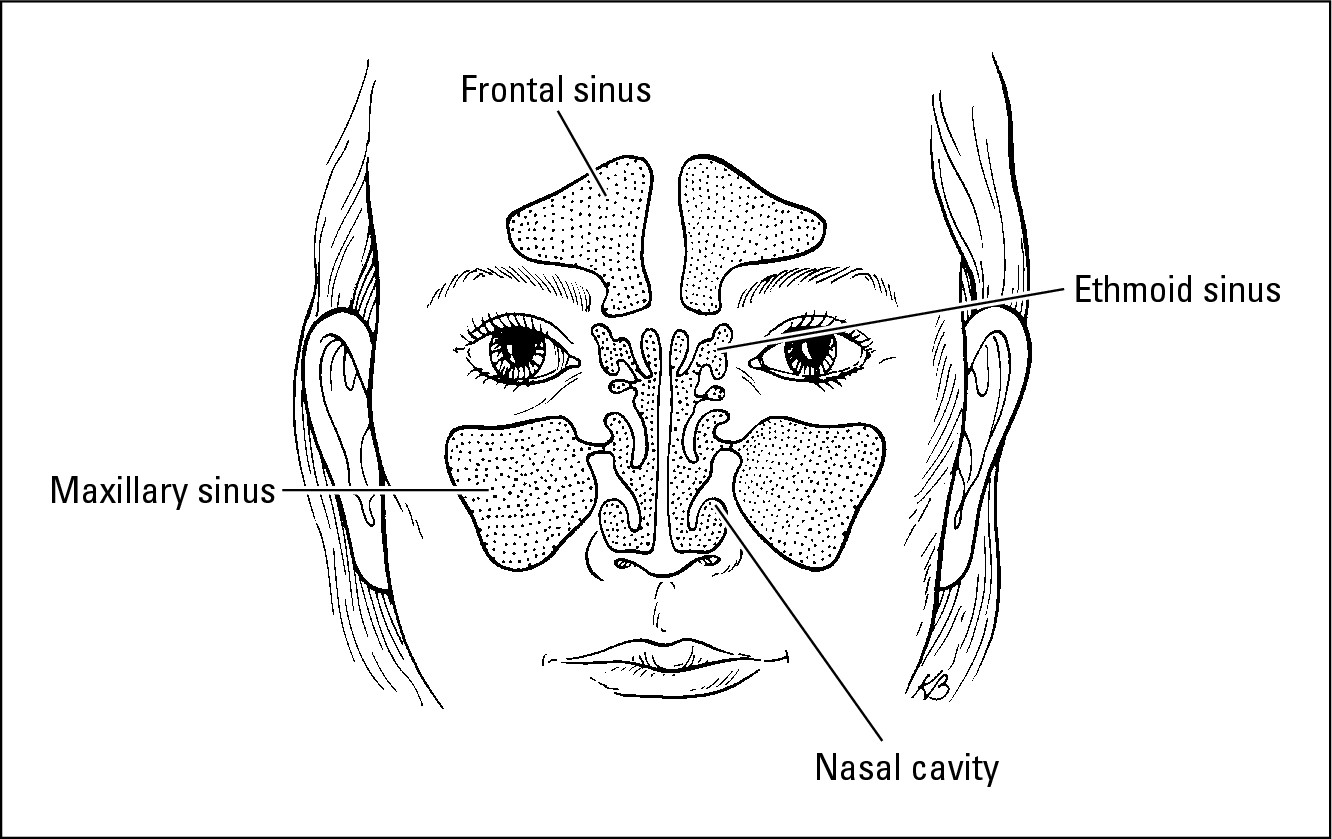
The three types of paranasal sinuses come in pairs (one on each side of the nose) and are named for the bones that house them. They include
 Maxillary sinuses: The largest of the sinuses, these sinuses are located in your cheekbones.
Maxillary sinuses: The largest of the sinuses, these sinuses are located in your cheekbones.
 Frontal sinuses: These sinuses reside in your forehead above your eyes.
Frontal sinuses: These sinuses reside in your forehead above your eyes.
 Ethmoid sinuses: These sinuses are immediately behind your eyes and nose.
Ethmoid sinuses: These sinuses are immediately behind your eyes and nose.
The other sinus affected by sinusitis is the sphenoid sinus, located behind your nose near the base of your brain.
|
Figure 13-1: Your sinuses are actually hollow cavities that surround your nasal cavity. |
|


Practical sinus
Sinuses are a vital part of your body’s defense against the airborne bacteria, viruses, irritants, and allergens that you constantly inhale. Under normal circumstances, the mucus in your sinuses traps most of these intruders. Cilia sweep the particle-laden mucus through connecting ostia (sinus drainage openings) into your nasal passages, which then drains into your throat. From your throat, the mucus moves into your stomach, where your digestive system can neutralize and eventually eliminate the offending substances.
In addition to helping clear your upper respiratory tract of particle-laden mucus, your sinuses serve other important roles. For example, your sinuses act as:
 Air pockets that lighten your skull — otherwise, your head would be too heavy for your neck. Calling someone an airhead is actually an anatomically correct statement.
Air pockets that lighten your skull — otherwise, your head would be too heavy for your neck. Calling someone an airhead is actually an anatomically correct statement.
 Resonance chambers that provide space for your voice to resonate.
Resonance chambers that provide space for your voice to resonate.
 Climate adjusters, warming and humidifying the air that you inhale.
Climate adjusters, warming and humidifying the air that you inhale.
 Insulators, which also warm the base of your brain, located directly behind your nose.
Insulators, which also warm the base of your brain, located directly behind your nose.
 Shock absorbers, protecting the inside of your skull from injury.
Shock absorbers, protecting the inside of your skull from injury.

Think of a swiftly flowing stream. If the stream dams up, the water usually stagnates and turns into a breeding ground for all sorts of organisms. The same process applies to your sinuses, which is why it’s crucial to avoid letting them turn into swamps.
How long has this been goin’ on?

 Acute sinusitis: Symptoms of acute sinusitis persist for up to three to four weeks, although some doctors may diagnose symptoms that continue for up to eight weeks as acute. Typical symptoms of acute sinusitis include
Acute sinusitis: Symptoms of acute sinusitis persist for up to three to four weeks, although some doctors may diagnose symptoms that continue for up to eight weeks as acute. Typical symptoms of acute sinusitis include
• Upper respiratory infection.
• Runny nose with infected mucus that often appears as cloudy, thick, yellowish, or greenish nasal discharge.
• Cloudy, yellowish, or greenish postnasal drip (often of such a quantity that you may need to swallow frequently).
• Facial pain or pressure around cheeks, eyes, and lower nose (mainly in adults, less commonly in children), especially while bending over or moving vigorously (for example, during exercise).
• Nasal congestion, headache, fever, and cough.
• A reduction or loss of the sense of smell, pain in upper teeth or the upper jawbone, and bad breath.
• In some children, nausea and vomiting due to gagging on infected mucus. Some children have persistent nocturnal cough and halitosis (bad breath).
 Chronic sinusitis: When your condition lasts longer than four weeks, doctors usually consider you a chronic sufferer. In many cases, chronic sinusitis can last for months with combinations of the same symptoms as acute sinusitis, although you may not have a fever. For this reason, many people with chronic sinusitis think that they suffer from frequent or constant colds.
Chronic sinusitis: When your condition lasts longer than four weeks, doctors usually consider you a chronic sufferer. In many cases, chronic sinusitis can last for months with combinations of the same symptoms as acute sinusitis, although you may not have a fever. For this reason, many people with chronic sinusitis think that they suffer from frequent or constant colds.
 Recurrent sinusitis: Doctors usually define recurrent sinusitis as three or more episodes of acute sinusitis per year. The recurring episodes may occur as a result of different causes. If you have recurrent sinusitis, your doctor may refer you to an allergist to determine whether allergies are the underlying cause of your condition. (See Chapter 11 for more details on allergy testing.)
Recurrent sinusitis: Doctors usually define recurrent sinusitis as three or more episodes of acute sinusitis per year. The recurring episodes may occur as a result of different causes. If you have recurrent sinusitis, your doctor may refer you to an allergist to determine whether allergies are the underlying cause of your condition. (See Chapter 11 for more details on allergy testing.)
Diagnosing sinusitis

 When did you first notice the symptoms?
When did you first notice the symptoms?
 What hurts? Where do you feel the pain?
What hurts? Where do you feel the pain?
 Does your family have a history of allergies and sinus problems?
Does your family have a history of allergies and sinus problems?
 What have you done to treat your symptoms? What sorts of medications have you taken, and what has been their effect?
What have you done to treat your symptoms? What sorts of medications have you taken, and what has been their effect?
Your doctor also conducts a physical exam of your nose and sinuses in order to confirm diagnosis. This exam may include
 Taking your temperature to check for fever and listening to your chest to see whether the infection has spread to your lungs.
Taking your temperature to check for fever and listening to your chest to see whether the infection has spread to your lungs.
 Lightly tapping your forehead and cheekbones to check for sensitivity in your frontal and maxillary sinuses.
Lightly tapping your forehead and cheekbones to check for sensitivity in your frontal and maxillary sinuses.
 Looking for infected mucus in your nose and the back of your throat. This exam may require insertion of a flexible fiber-optic device, known as an endoscope or a fiber-optic rhinoscope, so your doctor can clearly view potentially infected areas.
Looking for infected mucus in your nose and the back of your throat. This exam may require insertion of a flexible fiber-optic device, known as an endoscope or a fiber-optic rhinoscope, so your doctor can clearly view potentially infected areas.

Determining the best course of treatment
To effectively treat your sinusitis, you need to effectively manage your allergic rhinitis. In many cases, appropriately treating your allergic rhinitis also improves your sinusitis. As I explain in Chapter 10, avoidance and allergy-proofing are crucial tools you can use to effectively treat your allergies. Chapter 12 provides you with an in-depth explanation of allergy medications that you may find appropriate for your condition.
In addition to addressing your allergic rhinitis, doctors can also prescribe a variety of treatments for sinusitis, ranging from medication to irrigation to surgery.
Antibiotics

 Because the blood flow to your sinuses is poor, you may need to take your prescribed antibiotics for a while before you notice a beneficial effect. However, most cases of acute sinusitis respond to antibiotic treatment within two weeks.
Because the blood flow to your sinuses is poor, you may need to take your prescribed antibiotics for a while before you notice a beneficial effect. However, most cases of acute sinusitis respond to antibiotic treatment within two weeks.
 In cases of chronic sinusitis, don’t be surprised if your doctor prescribes a six- to eight-week course of antibiotic therapy with combined use of intranasal steroids (see Chapter 12) to eliminate your bacterial infection.
In cases of chronic sinusitis, don’t be surprised if your doctor prescribes a six- to eight-week course of antibiotic therapy with combined use of intranasal steroids (see Chapter 12) to eliminate your bacterial infection.
.jpg)
Other medications

Irrigation

Get steamed
Your doctor may also advise a simple home remedy to help clear your sinuses and relieve discomfort. This remedy consists of inhaling steam to liquefy and soften crusty mucus while moisturizing your inflamed passages.

1. Boil water in a kettle on the stove.
2. Carefully pour the boiling water in a pan or basin on a low table.
3. Sit at the table and drape a towel over your head, leaning over the pan or basin to form a kind of human tent with your head as the pole.
4. Hold your face a few inches above the steaming water and breathe the steam through your nose for approximately ten minutes.
Two steam treatments a day may provide relief. However, you still need to deal with the underlying cause of the sinus infection, so I don’t advise relying solely on this home remedy as the only therapy for your infectious sinusitis.
Sinus surgery
If other treatment methods don’t provide effective relief, you may need surgery, especially if physical obstructions, such as a deviated septum or nasal polyps, contribute to your condition. However, if allergic rhinitis is the underlying cause of your sinusitis, surgery alone won’t resolve your sinus problems. You must continue managing your allergic rhinitis to avoid further complications. By the same token, treating your allergies alone won’t reverse the damage that sinusitis may have already caused.
If your doctor thinks that surgery is advisable, she will refer you to an ear, nose, and throat specialist, or ENT, otherwise known as an otolaryngologist (remember that word for your next Scrabble game — you could score big). Before you consider surgery, make sure your doctor thoroughly reviews your medical history and evaluates your clinical condition.

The good news about surgery for your sinuses is that the two most common procedures are minimally invasive. An ENT specialist can perform them on an outpatient basis with local anesthesia, although he may use general anesthesia in certain cases. The two procedures most often used are
 Antral puncture and irrigation: This procedure opens up your sinuses so they can drain and irrigate properly, but is used less often now since the advent of fiber-optic surgery.
Antral puncture and irrigation: This procedure opens up your sinuses so they can drain and irrigate properly, but is used less often now since the advent of fiber-optic surgery.
 Functional endoscopic sinus surgery: This procedure is more com- plex than antral puncture and irrigation. Functional endoscopic sinus surgery often involves enlarging the ethmoid and maxillary sinus openings into the nasal cavity and removing and cleaning the infected sinus membranes, resulting in improved drainage. This procedure re-establishes the ventilation of your ethmoid, maxillary, and frontal sinuses. Otolaryngologists perform this type of surgery with high-tech computer-assisted instruments and navigation devices to ensure pinpoint accuracy.
Functional endoscopic sinus surgery: This procedure is more com- plex than antral puncture and irrigation. Functional endoscopic sinus surgery often involves enlarging the ethmoid and maxillary sinus openings into the nasal cavity and removing and cleaning the infected sinus membranes, resulting in improved drainage. This procedure re-establishes the ventilation of your ethmoid, maxillary, and frontal sinuses. Otolaryngologists perform this type of surgery with high-tech computer-assisted instruments and navigation devices to ensure pinpoint accuracy.
An ounce of prevention . . .

 Take the appropriate medications. See Chapter 12 for a complete listing.
Take the appropriate medications. See Chapter 12 for a complete listing.
 Drink plenty of water. Water keeps your mucus thin and fluid so your sinuses can drain more easily.
Drink plenty of water. Water keeps your mucus thin and fluid so your sinuses can drain more easily.
 Be nice to your nose. Blow it gently, preferably one nostril at a time.
Be nice to your nose. Blow it gently, preferably one nostril at a time.
 Avoid flying. If you have to travel by air while you have a cold or an allergy attack, use a topical nasal decongestant spray prior to takeoff. The spray prevents the sudden pressure changes from blocking your sinuses and ears.
Avoid flying. If you have to travel by air while you have a cold or an allergy attack, use a topical nasal decongestant spray prior to takeoff. The spray prevents the sudden pressure changes from blocking your sinuses and ears.
 Avoid swimming. You probably won’t feel like going to the beach or the pool if you have a cold or allergy attack, and your sinuses won’t enjoy the pressure changes that swimming and diving involve (scuba diving wouldn’t be a good idea either).
Avoid swimming. You probably won’t feel like going to the beach or the pool if you have a cold or allergy attack, and your sinuses won’t enjoy the pressure changes that swimming and diving involve (scuba diving wouldn’t be a good idea either).
Otitis Media

Middle ear infections and fluid in the ear are especially common in young children and infants. In fact, otitis media is the most common reason in the United States for pediatric visits, with doctors treating at least 10 million children annually for ear infections. Otitis media can have serious consequences for youngsters, in particular by adversely affecting a child’s development and learning ability due to potential hearing loss.
The most common forms of otitis media are
 Acute otitis media (AOM): This condition involves inflammation and infection of the middle ear and Eustachian tube. The peak incidence is between 6 months and 1 year of age, decreasing with age and with fewer episodes after 7 years of age.
Acute otitis media (AOM): This condition involves inflammation and infection of the middle ear and Eustachian tube. The peak incidence is between 6 months and 1 year of age, decreasing with age and with fewer episodes after 7 years of age.
 Otitis media with effusion (OME): Doctors also refer to this condition as serous otitis media — fluid in the middle ear. This condition, which occurs commonly in children ages 2 to 7 years, can lead to hearing loss if not treated properly.
Otitis media with effusion (OME): Doctors also refer to this condition as serous otitis media — fluid in the middle ear. This condition, which occurs commonly in children ages 2 to 7 years, can lead to hearing loss if not treated properly.
Revealing common causes
In a significant number of cases, allergic rhinitis precedes an ear infection. A long-term study of 2,000 children found that 50 percent of the patients with chronic and recurrent ear infections who were 3 years of age and older had allergic rhinitis.
Other conditions that can increase your chances of developing ear infections include
 Sinusitis. The same factors that can lead to sinus infections, such as exposure to allergens, tobacco smoke, pollutants, and other irritants, can also contribute to ear infections.
Sinusitis. The same factors that can lead to sinus infections, such as exposure to allergens, tobacco smoke, pollutants, and other irritants, can also contribute to ear infections.
 Enlarged adenoids.
Enlarged adenoids.
 Unrepaired cleft palate.
Unrepaired cleft palate.
 Nasal polyps.
Nasal polyps.
 Pacifier use by babies.
Pacifier use by babies.
 Defective or immature immune system.
Defective or immature immune system.
 Benign or malignant tumors.
Benign or malignant tumors.
 Teething. Some physicians believe that teething in young children can also contribute to ear infections, but no one has established a direct connection.
Teething. Some physicians believe that teething in young children can also contribute to ear infections, but no one has established a direct connection.

Getting an earful
The visible part of your ear — that funny-looking protrusion on the side of your head — is only the tip of the iceberg. Most of your ears’ functions take place inside your skull in chambers, tubes, and passages that register and conduct sound and also provide your sense of balance.

 Outer ear: Also known as the pinna, this structure is what many people think of as the ear. The primary function of this skin-covered flap of elastic cartilage is to funnel sound into the middle ear and to keep your eyeglasses on the side of your head.
Outer ear: Also known as the pinna, this structure is what many people think of as the ear. The primary function of this skin-covered flap of elastic cartilage is to funnel sound into the middle ear and to keep your eyeglasses on the side of your head.
 Middle ear: This air-filled chamber is bordered by the tympanic membrane (commonly known as the eardrum) and small bones that enable your eardrum to function. Through its connection (the Eustachian tube) to the nasopharynx (back of the nose), your middle ear also equalizes the air pressure on both sides of your eardrum.
Middle ear: This air-filled chamber is bordered by the tympanic membrane (commonly known as the eardrum) and small bones that enable your eardrum to function. Through its connection (the Eustachian tube) to the nasopharynx (back of the nose), your middle ear also equalizes the air pressure on both sides of your eardrum.
 Inner ear: Your inner ear contains sensory receptors that provide your hearing and balance. The hearing receptors are enclosed in the cochlea, a fluid-filled chamber, while the balance receptors are in the semi-circular canals (refer to Figure 13-2).
Inner ear: Your inner ear contains sensory receptors that provide your hearing and balance. The hearing receptors are enclosed in the cochlea, a fluid-filled chamber, while the balance receptors are in the semi-circular canals (refer to Figure 13-2).
 Eustachian tube (ET): Your Eustachian tube is an extension of the middle ear that connects to the nasopharynx. The ET, which is often the origin of ear infections, serves three important functions:
Eustachian tube (ET): Your Eustachian tube is an extension of the middle ear that connects to the nasopharynx. The ET, which is often the origin of ear infections, serves three important functions:
• The ET provides ventilation for your middle ear.
• The ET helps equalize air pressure inside your ear, buffering the eardrum from the force of external air, and helps dissipate the energy of sound waves from your inner ear into your throat.
• Because your ET is closed most of the time, it serves as an important barrier to viruses, bacteria, irritants, and allergens that enter your middle ear. Similar to the function of your sinuses, cilia in the middle ear sweep debris-laden mucus from your middle ear through the ET into the back of your nasal cavity. The cilia prepare the mucus for drainage into your throat and eventually into your stomach.
The ET briefly opens to allow the cilia to sweep mucus away when you swallow, yawn, sniff, or strain. In many children, however, the ET doesn’t fully develop until age 6, causing the ET to ineffectively ventilate, clear, or protect the middle ear. Therefore, large numbers of young children get middle ear infections.
|
Figure 13-2: See how the less visible part of your ear appears. |

|
Acute otitis media (AOM)
Many people suffer acute otitis media — an inflammation and infection of the middle ear and Eustachian tube — in early childhood. The main symptoms include
 Earache — sometimes with intense, stabbing pains — and fever. Occasionally, vomiting and diarrhea accompany this symptom.
Earache — sometimes with intense, stabbing pains — and fever. Occasionally, vomiting and diarrhea accompany this symptom.
 Possible hearing loss and occasional dizziness and ringing in the affected ear.
Possible hearing loss and occasional dizziness and ringing in the affected ear.
 With infants, high fever, irritability, and a tendency to pull on the affected ear.
With infants, high fever, irritability, and a tendency to pull on the affected ear.
 In some cases, discharge of infected fluid from the middle ear (if your eardrum has been perforated).
In some cases, discharge of infected fluid from the middle ear (if your eardrum has been perforated).
.jpg)
Because sinusitis and otitis media often coexist, doctors usually treat these conditions with the same medications. Treatment of AOM usually includes a course of antibiotics (available by prescription only) to rid your middle ear of infection. The antibiotic drugs that doctors commonly prescribe include
 Amoxicillin (Amoxil) or amoxicillin/potassium clavulanate (Augmentin)
Amoxicillin (Amoxil) or amoxicillin/potassium clavulanate (Augmentin)
 Clarithromycin (Biaxin) or azithromycin (Zithromax)
Clarithromycin (Biaxin) or azithromycin (Zithromax)
 Trimethoprim-sulfamethoxazole (Bactrim or Septra)
Trimethoprim-sulfamethoxazole (Bactrim or Septra)
 A third-generation cephalosporin antibiotic, such as cefuroxime (Ceftin), cefpodoxime (Vantin), cefprozil (Cefzil), and cefixime (Suprax)
A third-generation cephalosporin antibiotic, such as cefuroxime (Ceftin), cefpodoxime (Vantin), cefprozil (Cefzil), and cefixime (Suprax)
.jpg)
Otitis media with effusion (OME)
When you have otitis media with effusion (OME, also known as serous otitis media ), your middle ear traps infected or sterile fluid. The most common symptoms of OME are
 Plugged-up ears (similar to the discomfort that you may experience when descending in an airplane)
Plugged-up ears (similar to the discomfort that you may experience when descending in an airplane)
 Some hearing loss
Some hearing loss

OME treatments can also include nonprescription oral decongestants and nasal decongestant sprays, as well as topical nasal corticosteroid sprays. (For more information on these types of medicines, see Chapter 12.)

 Adenoidectomy: If your child’s Eustachian tube is chronically blocked and your child is more than 3 years old, your doctor may recommend removing your child’s adenoids. (Removing the tonsils is no longer an effective or appropriate procedure for treatment of ear problems.)
Adenoidectomy: If your child’s Eustachian tube is chronically blocked and your child is more than 3 years old, your doctor may recommend removing your child’s adenoids. (Removing the tonsils is no longer an effective or appropriate procedure for treatment of ear problems.)
 Myringotomy: The ENT surgeon makes a small incision in the eardrum that permits drainage of the trapped fluid. This procedure is helpful both for diagnostic purposes (to identify infecting organisms) and to relieve the severe pain, pressure, and fever associated with an acute middle ear infection.
Myringotomy: The ENT surgeon makes a small incision in the eardrum that permits drainage of the trapped fluid. This procedure is helpful both for diagnostic purposes (to identify infecting organisms) and to relieve the severe pain, pressure, and fever associated with an acute middle ear infection.
 Tympanostomy: This procedure includes surgically inserting small plastic tubes (known as pressure equalization or PE tubes) in the eardrum to equalize air pressure in the ear and to allow drainage of fluid from the middle ear and Eustachian tube down to the nasopharynx. ENT surgeons usually perform tympanostomies with a general anesthetic, and occasionally with local anesthetic (for older children or adults), as an outpatient procedure. In most cases, doctors recommend that PE tubes remain in place for 6 to 18 months or until they fall out. Children often don’t notice the tubes after they’ve been in place for a while. Generally, children with tubes shouldn’t go swimming. However, in some cases, an ENT surgeon may fit your child with earplugs, making water activities a possibility.
Tympanostomy: This procedure includes surgically inserting small plastic tubes (known as pressure equalization or PE tubes) in the eardrum to equalize air pressure in the ear and to allow drainage of fluid from the middle ear and Eustachian tube down to the nasopharynx. ENT surgeons usually perform tympanostomies with a general anesthetic, and occasionally with local anesthetic (for older children or adults), as an outpatient procedure. In most cases, doctors recommend that PE tubes remain in place for 6 to 18 months or until they fall out. Children often don’t notice the tubes after they’ve been in place for a while. Generally, children with tubes shouldn’t go swimming. However, in some cases, an ENT surgeon may fit your child with earplugs, making water activities a possibility.
Diagnosing ear infections

Other diagnostic procedures for both AOM and OME may include
 Audiometry: This procedure evaluates the effect of chronic middle ear effusions on a person’s hearing. Audiometry is especially important for children because hearing loss can cause delayed speech and language development.
Audiometry: This procedure evaluates the effect of chronic middle ear effusions on a person’s hearing. Audiometry is especially important for children because hearing loss can cause delayed speech and language development.
 Tympanometry: This procedure measures the eardrum’s response at various pressure levels and helps to diagnose middle ear effusions and Eustachian tube dysfunction.
Tympanometry: This procedure measures the eardrum’s response at various pressure levels and helps to diagnose middle ear effusions and Eustachian tube dysfunction.
Taking preventive measures
As with sinusitis, one of the most important steps you can take to prevent ear infections, if you also have allergic rhinitis, is to effectively treat your allergies, which includes using the avoidance measures that I describe in Chapter 10 and also the appropriate medications, if necessary, to manage allergic rhinitis symptoms, as I explain in Chapter 12.
You also need to take the preventive measures that I describe in the “Complicating Your Allergies and Asthma: Sinusitis” section of this chapter to keep your sinuses clear if you have an allergy attack or a cold or other upper respiratory infection.