Chapter 16
Treating Asthma Episodes
In This Chapter
 Relieving asthma symptoms with short-term medications
Relieving asthma symptoms with short-term medications
 Considering anticholinergic therapy
Considering anticholinergic therapy
 Controlling worsening respiratory symptoms with oral corticosteroids
Controlling worsening respiratory symptoms with oral corticosteroids
Y ou can use quick-relief drugs, also known as rescue medications,
Quick-relief medications serve two main purposes:
 Short-term relief. To prevent a worsening of respiratory symptoms prior to exposure to asthma triggers, and/or before engaging in exercise or other strenuous activities that could trigger symptoms of exercise-induced asthma (EIA), as specified by your physician.
Short-term relief. To prevent a worsening of respiratory symptoms prior to exposure to asthma triggers, and/or before engaging in exercise or other strenuous activities that could trigger symptoms of exercise-induced asthma (EIA), as specified by your physician.
 Rescue. In cases where an asthma condition suddenly worsens — perhaps due to unanticipated exposure to allergens, irritants, or precipitating factors — quick-relief medications are essential for reversing rapidly deteriorating respiratory symptoms.
Rescue. In cases where an asthma condition suddenly worsens — perhaps due to unanticipated exposure to allergens, irritants, or precipitating factors — quick-relief medications are essential for reversing rapidly deteriorating respiratory symptoms.

 Short-acting beta
2
-adrenergic bronchodilators
Short-acting beta
2
-adrenergic bronchodilators
 Anticholinergics, which may provide added relief when combined with inhaled short-acting beta
2
-adrenergic bronchodilators
Anticholinergics, which may provide added relief when combined with inhaled short-acting beta
2
-adrenergic bronchodilators
 Oral corticosteroids, also referred to as systemic corticosteroids, which doctors prescribe in closely supervised courses to reestablish control of a patient’s asthma in cases of sudden, severe worsening of respiratory symptoms
Oral corticosteroids, also referred to as systemic corticosteroids, which doctors prescribe in closely supervised courses to reestablish control of a patient’s asthma in cases of sudden, severe worsening of respiratory symptoms
I discuss these three categories of short-term asthma medications in detail throughout this chapter and also list general dosage information for specific drugs in each class.
Relieving Symptoms with Short-Acting Bronchodilators
The primary class of medications that physicians prescribe for rescue treatment of asthma is inhaled or aerosol formulations of short-acting beta 2 - adrenergic (beta 2 -agonist) bronchodilators. These adrenaline-like drugs work by rapidly relaxing the smooth muscles in your airways, causing your airways to open, usually within five minutes of inhaling the medication.
In comparison to beta 2 -adrenergic pills and syrups, physicians consider inhaled or aerosol forms of bronchodilators the therapy of choice for treat-ing asthma symptoms that suddenly worsen, and for preventing EIA. When administered in their inhaled or aerosol formulations, beta 2 -adrenergic bronchodilators work faster, produce fewer side effects, and provide the most effective, prompt relief of acute respiratory symptoms.

The principal short-acting beta 2 -adrenergic bronchodilators prescribed in the United States include the following:
 Albuterol (Proventil, Ventolin)
Albuterol (Proventil, Ventolin)
 Bitolterol (Tornalate)
Bitolterol (Tornalate)
 Metaproterenol (Alupent)
Metaproterenol (Alupent)
 Pirbuterol (Maxair)
Pirbuterol (Maxair)
 Terbutaline (Brethaire, Brethine, Bricanyl)
Terbutaline (Brethaire, Brethine, Bricanyl)
 Levalbuterol (Xopenex), a new, improved version of albuterol, available in compressor-driven nebulizer (CDN) formulations for patients 6 and older
Levalbuterol (Xopenex), a new, improved version of albuterol, available in compressor-driven nebulizer (CDN) formulations for patients 6 and older
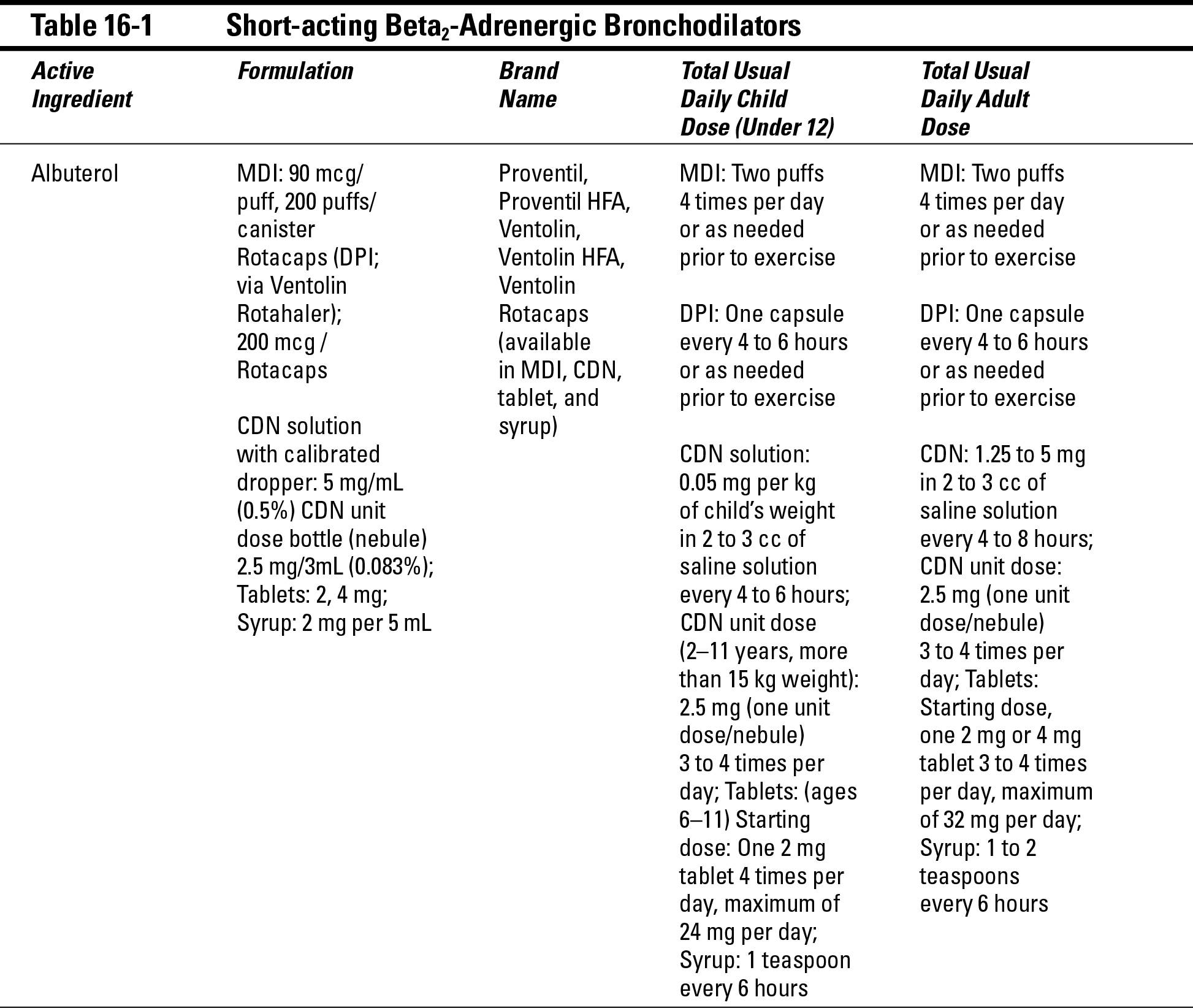
Table 16-1 provides detailed dosage information for individual short-acting beta 2 -adrenergic bronchodilators.
Using short-acting bronchodilators effectively
If you correctly use your prescribed long-term asthma medications prescribed by your physician, along with effectively avoiding allergens, irritants, and other potential triggers, you can control your asthma most of the time. However, given the unpredictable nature of most people’s lives, you may experience instances where your respiratory condition suddenly worsens, most often due to unexpected and unavoidable exposure to certain asthma triggers. (See Chapter 5 for details of asthma triggers.)
When these situations occur, make sure you discuss with your doctor what type of short-acting bronchodilator might work for you, based on your specific asthma condition, for the prompt relief of an asthma episode.

But, in those rare instances when these patients do need to resort to using their short-acting bronchodilator, they’ll most often be able to quickly regain control of their condition before it seriously worsens.
Getting more bronchodilation per breath

If your short-acting bronchodilator isn’t providing rapid relief of symptoms, determine if any of the following factors may be causing the problem:
 You’re not using the product properly. Make sure that your doctor shows you the proper technique for using your inhaler and reviews your technique during office visits.
You’re not using the product properly. Make sure that your doctor shows you the proper technique for using your inhaler and reviews your technique during office visits.
 Your canister may be empty. To check whether you need a new canister, remove the container from the actuator sleeve and put it in water (a sink works well for this test). If the canister starts floating to the top, it’s likely close to empty.
Your canister may be empty. To check whether you need a new canister, remove the container from the actuator sleeve and put it in water (a sink works well for this test). If the canister starts floating to the top, it’s likely close to empty.
 The mouthpiece (where you inhale) may be dirty or blocked. Keep your inhaler clean. (Chapter 14 provides details about cleaning your mouthpiece.)
The mouthpiece (where you inhale) may be dirty or blocked. Keep your inhaler clean. (Chapter 14 provides details about cleaning your mouthpiece.)
Choosing better bronchodilators
.jpg)
Although epinephrine is used in emergency treatment and in self-injection kits, such as EpiPen or Twinject, for cases of severe asthma attacks and anaphylaxis (a potentially life-threatening reaction that affects many organs simultaneously), routine use of the drug can cause serious adverse side effects, including shakiness, an increase in blood pressure, or a rapid or irregular heartbeat. Because of this danger, avoid using OTC bronchodilators if you have a heart condition.
Avoiding potential adverse side effects of short-acting bronchodilators

In most cases, patients experience few, if any, of the potentially unpleasant side effects of short-acting bronchodilators by using these medications only for the quick relief of worsening respiratory symptoms. As effective as quick-relief bronchodilators can be for rescue purposes — especially a recently approved product such as levalbuterol (see the “Introducing new and improved bronchodilation” section, later in the chapter) — only use short-acting bronchodilators as needed, rather than on a routine basis, especially if you have persistent asthma
Instead of using rescue products on a day-to-day basis to manage your respiratory symptoms, make sure that you’re consistently taking long-term medications your physician prescribes (as part of your overall asthma management plan) to maintain control over your asthma condition. (See Chap- ter 15 for detailed information on long-term products.)
Bucking bronchodilator dependence: Avoiding overuse of your quick-relief product
.jpg)
Ensuring that your asthma management plan is as effective as possible may mean that you need to take long-term anti-inflammatory medication, such as inhaled corticosteroids, on a regular basis to control your asthma (see Chap-ter 15).
Contact your doctor immediately if you’re using your short-acting beta 2 -adrenergic bronchodilator more often than once every one to two hours. Overusing this type of rescue medication at that rate (more frequently than once every one to two hours) is a sign that your asthma symptoms are worsening.

Taking many medicines can make matters worse
.jpg)
Introducing new and improved bronchodilation

Levalbuterol has been particularly useful when given by CDN to especially sensitive groups, such as the elderly and children. Because the FDA hasn’t yet approved levalbuterol for use in children under 6, physicians administer this drug off-label to that age group. Because albuterol (the parent com-pound of levalbuterol) has been safely used without any significant adverse effects for more than 25 years to treat infants and young children, physicians often feel comfortable prescribing levalbuterol (Xopenex) for children under age 6.
Quick fix versus long-term asthma management
Controlling asthma means treating the underlying inflammation of your airways. Don’t substitute the quick fix of an inhaled short-acting beta 2 -adrenergic bronchodilator for consistent, routine use of the appropriate long-term asthma medications that your doctor prescribes.
Think of your asthma as a smoldering campfire in your lungs. If you pay attention to the embers only after they flare up, containing the flames becomes a serious problem. The goal of your asthma management plan is to get your asthma under control to the extent that you only rarely use bronchodilators on an as-needed basis — usually to reduce the risk of symptoms when exposed to unavoidable asthma triggers or precipitating factors, especially exercise.
Also, beware of relying on inhaled short-acting bronchodilators, because the quick relief these products provide can also give you the false impression that your asthma is just a set of symptoms, rather than a serious, underlying medical problem. Imagine having a high fever and only taking a pain reliever to reduce your discomfort. You may temporarily feel better, but if the underlying cause of your high temperature is a severe inflammation, such as appendicitis, treating only the symptoms can lead to a very serious situation — in this case a ruptured appendix — because you may not realize the gravity of your condition, thus delaying necessary treatment.
Likewise, if zapping your wheezing with an inhaled short-acting beta 2 -adrenergic bronchodilator is the only way you deal with your persistent asthma, you may feel fine for a short while. However, if you use your peak-flow meter (see Chapter 4) to check your peak expiratory flow rate (PEFR), or if your doctor performs a spirometry procedure (see Chapter 2), you quickly realize that your airflow is significantly decreased and your lung functions are below normal. When based solely on how they’re feeling, the majority of asthma patients tend to underestimate the magnitude of their airway obstruction. Often, it isn’t until they can objectively measure their airflow, typically by using a peak-flow meter, that they really become aware of their deteriorating condition.
Reversing Airflow Obstruction with Anticholinergics


Anticholinergic medications are usually most effective for patients who have partially reversible airflow obstruction or who are prone to producing greater amounts of mucus. Doctors frequently prescribe these products for patients with chronic bronchitis and emphysema, collectively referred to as chronic obstructive pulmonary disease (COPD).
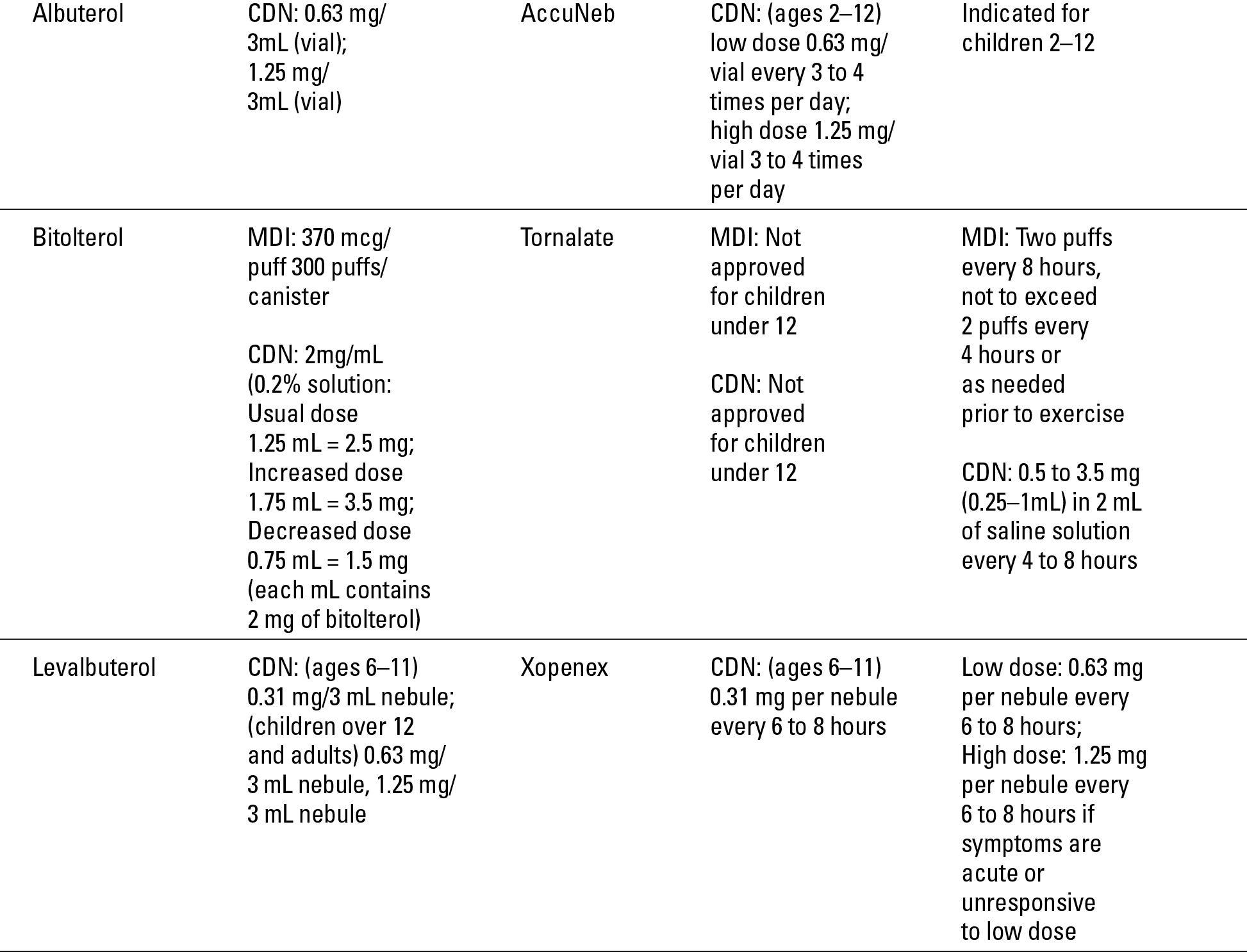
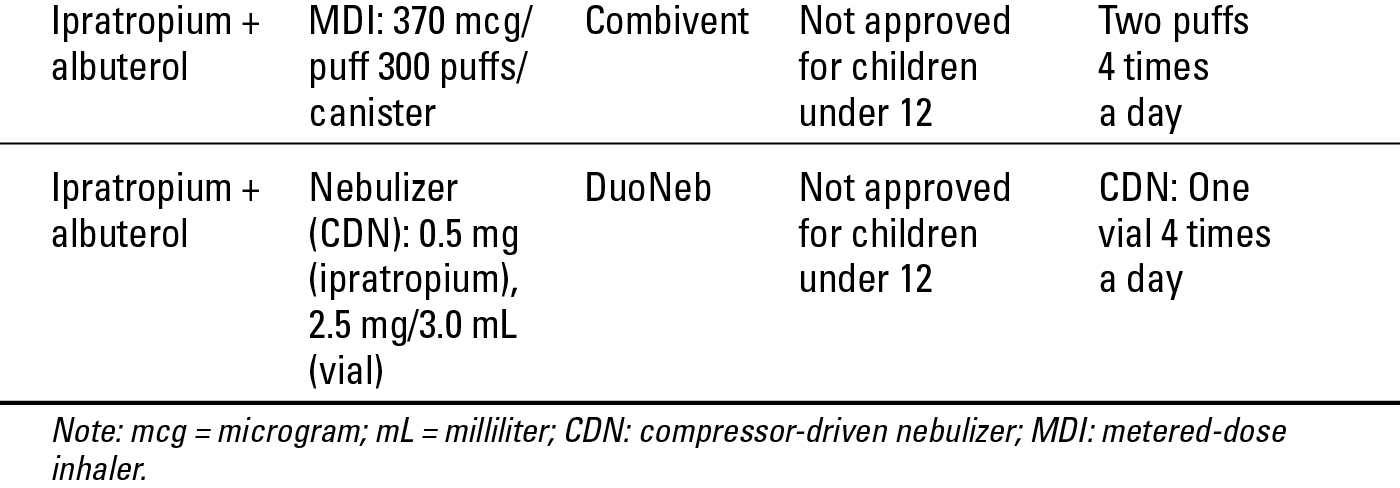
The principal anticholinergic used in the United States is ipratropium bromide, a quick-relief drug that doctors often prescribe in conjunction with a short-acting beta 2 -adrenergic bronchodilator for dilating the airways. Ipratropium bromide can provide greater bronchodilation when combined with a bronchodilator such as albuterol into a single inhaled product (Combivent). Table 16-2 lists general dosage information for anticholinergic medications.
Ipratropium bromide has an excellent safety profile and few potential adverse side effects. Those side effects can include dry mouth, airway secretions, and, in rare cases, wheezing. Don’t accidentally spray this product in your eyes, because it can temporarily blur your vision.

Looking at Short-Term, Rescue Use of Oral Corticosteroids
In addition to their use as long-acting medications, oral corticosteroids (see Chapter 15) can also play a quick-relief role in your asthma management. During moderate-to-severe asthma episodes, your doctor may use oral corticosteroids to rapidly gain control over worsening symptoms. In such cases, oral corticosteroids can help your other quick-relief medications work more effectively, resulting in a more rapid reversal or reduction of airway inflammation, speeding recovery, and reducing the rate of relapse.

.jpg)
Prolonged use of oral corticosteroids can lead to adverse systemic (affecting multiple organs of your body) side effects, including fluid retention, altered blood sugar levels, weight gain, peptic ulcers, mood alteration, high blood pressure, reduced bone density, and impaired immune functioning. For this reason, doctors often prescribe these drugs only as a last resort, and discontinue (by gradual tapering) them as soon as symptoms are under control.