Chapter 6
Understanding Asthma and the Role of Allergies
In This Chapter
 Understanding the immunologic basis of your asthma and allergic condition
Understanding the immunologic basis of your asthma and allergic condition
 Sensitizing your immune system
Sensitizing your immune system
 Classifying your immune system’s allergic responses
Classifying your immune system’s allergic responses
 Testing for potential immunodeficiencies
Testing for potential immunodeficiencies
 Improving your quality of life with immunotherapy
Improving your quality of life with immunotherapy
I n terms of germs, the world can still be a rough place. Despite major advances during the past 100 years in fighting infectious diseases and providing effective medical care, viruses, bacteria, fungi, and other potentially harmful agents remain constant threats to your health. That’s why your body’s defense network is so important to your well-being.
Your frontline defense against potentially infectious intruders is your skin. (Your mucous membranes, as well as your stomach’s highly acidic digestive juices, your gut’s beneficial bacteria, and certain nonspecific cells, also act as immediate defenders against uninvited guests.) The second, far more complex and fundamental defense apparatus in your body — and one of the most important keys to the survival of the human species — is your immune system.
Because numerous immune system processes can play important roles as underlying factors in asthma and allergy (as well as in many other diseases), doctors frequently need to apply their understanding of immunology (the science of immunity) when evaluating and treating asthma. I devote this chapter to explaining the immunologic basis of allergic asthma and other allergic reactions so that you can have a better understanding of what may be at the root of your ailment and to review with you what your physician considers when diagnosing and treating your condition.
Protecting Your Health: How Your Immune System Works
Your immune system’s most basic function is to distinguish between your body (self) and potentially harmful (non-self) agents. Your immune system performs the following functions to protect you:
 Recognizes foreign (therefore, potentially harmful) microorganisms, their products, and toxins, all known generally as antigens.
These substances can stimulate a response from your immune system and react with an antibody or a sensitized T-cell (a specialized immune system cell involved in cell-mediated immunity, as I explain in “Reacting to allergen exposures,” later in this chapter). Allergens, which usually consist of proteins, are particular types of antigens, which initiate an allergic response that often triggers respiratory symptoms in asthma patients.
Recognizes foreign (therefore, potentially harmful) microorganisms, their products, and toxins, all known generally as antigens.
These substances can stimulate a response from your immune system and react with an antibody or a sensitized T-cell (a specialized immune system cell involved in cell-mediated immunity, as I explain in “Reacting to allergen exposures,” later in this chapter). Allergens, which usually consist of proteins, are particular types of antigens, which initiate an allergic response that often triggers respiratory symptoms in asthma patients.
 Identifies self-antigens. These antigens are usually damaged and improperly functioning cells in your body. Malignant cells that can develop into tumor-causing cancerous cells are an example of self-antigens.
Identifies self-antigens. These antigens are usually damaged and improperly functioning cells in your body. Malignant cells that can develop into tumor-causing cancerous cells are an example of self-antigens.
 Assists in removing antigens from your body. Specialized immune system cells recognize, surround, and destroy these intruders through a complicated series of immunological processes.
Assists in removing antigens from your body. Specialized immune system cells recognize, surround, and destroy these intruders through a complicated series of immunological processes.
The immune system’s defense is vital to the survival of all animals. If your immune system functions properly, its protective function is an underlying, ongoing, and generally imperceptible aspect of your everyday existence.

 Autoimmune disorders: These disorders include serious diseases such as rheumatic fever, a rare complication of an inadequately treated strep infection of the upper respiratory tract (strep throat), in which the immune system can attack heart tissue cells that cross-react with Streptococcus bacterial antigens. This kind of complication is why taking the full course of antibiotic therapy your doctor prescribes for strep throat is important and that you return to your doctor’s office for a repeat throat culture to make sure that your infection has completely resolved. (For more information on cross-reactivity, see Chapter 11.)
Autoimmune disorders: These disorders include serious diseases such as rheumatic fever, a rare complication of an inadequately treated strep infection of the upper respiratory tract (strep throat), in which the immune system can attack heart tissue cells that cross-react with Streptococcus bacterial antigens. This kind of complication is why taking the full course of antibiotic therapy your doctor prescribes for strep throat is important and that you return to your doctor’s office for a repeat throat culture to make sure that your infection has completely resolved. (For more information on cross-reactivity, see Chapter 11.)
In other cases, the immune system (for reasons doctors are still working to discover) loses its ability to differentiate between certain self and non-self substances. This inability to distinguish can cause diseases such as systemic lupus erythematous, psoriasis, rheumatoid arthritis, and some forms of diabetes, when your immune system perceives otherwise functional and vital cells in your body as antigens and turns its firepower on them.
 Rejection of organ transplants: Doctors usually try to find a close genetic match between patient and organ donors to reduce the risk of the patient’s immune system rejecting the donated organ. In many cases, however, physicians still need to administer drugs to suppress the patient’s immune system and prevent organ rejection. This suppression of the immune system can then increase the risk of opportunistic infections, potentially harming the patient.
Rejection of organ transplants: Doctors usually try to find a close genetic match between patient and organ donors to reduce the risk of the patient’s immune system rejecting the donated organ. In many cases, however, physicians still need to administer drugs to suppress the patient’s immune system and prevent organ rejection. This suppression of the immune system can then increase the risk of opportunistic infections, potentially harming the patient.
 Allergic conditions: If you have asthma or allergies, you almost certainly have an immune system that works too well or overreacts. Doctors use the term hypersensitivity to refer to allergies because your immune system is overly sensitive to substances such as pollens, animal dander, and other types of allergens that offer no real threat to your health. With hypersensitivity, your immune system acts sort of like an alarm system that summons a SWAT team regardless of whether a cat burglar or just a cat is intruding on your property.
Allergic conditions: If you have asthma or allergies, you almost certainly have an immune system that works too well or overreacts. Doctors use the term hypersensitivity to refer to allergies because your immune system is overly sensitive to substances such as pollens, animal dander, and other types of allergens that offer no real threat to your health. With hypersensitivity, your immune system acts sort of like an alarm system that summons a SWAT team regardless of whether a cat burglar or just a cat is intruding on your property.
Classifying Immune System Components and Disorders
Your immune system consists of several related processes. Think of these processes as a civil defense network of arsenals, supply lines, logistical support, and command and control centers for the cells that actually defend your body. The most important organ and tissue components of your immune system include the following:

 Bone marrow: In your bone marrow, stem cells (early, nonspecific types of cells) originate, developing into B-cells (specialized types of plasma cells) that subsequently secrete distinct forms of plasma proteins, known as antibodies. These antibodies are divided into the following five classes of immunoglobulins (identified by the prefix Ig):
Bone marrow: In your bone marrow, stem cells (early, nonspecific types of cells) originate, developing into B-cells (specialized types of plasma cells) that subsequently secrete distinct forms of plasma proteins, known as antibodies. These antibodies are divided into the following five classes of immunoglobulins (identified by the prefix Ig):
• IgG: The major component of gamma globulin used for treating certain types of immune deficiencies, IgG antibodies account for at least three-quarters of your body’s antibodies. IgG antibodies along with IgM antibodies and your white blood cells defend you against bacterial infections. IgG antibodies also play an important role in preventing allergens from initiating an allergic reaction. As a response to immunotherapy (allergy shots), the production of IgG antibodies is believed to work by competing with IgE for antigen by binding to mast cells, thus preventing the subsequent release of chemical mediators of inflammation that produce asthma and allergy symptoms. (See “Reacting to allergen exposures,” later in this chapter, for more information.)
• IgM: About 5 percent of your antibodies belong to this class, which plays a role in the primary immune response and also enhances the role of IgG antibodies.
• IgA: The primary antibody in your mucous membrane surfaces, IgA antibodies reside in your saliva, tears, and in the secretions of the mucosal surfaces of your respiratory bronchi, gastrointestinal, and genital tracts, where these antibodies protect against infection. They’re also present in mother’s milk, thus providing antibody protection for breastfed newborns.
• IgD: This antibody class, which binds to the antigen at cell surface contact, seems to exist in very small quantities and plays a nonspecific role in the immune process.
• IgE: Although present in only minute quantities in your body, IgE antibodies (also known as reaginic antibodies) are key players in allergic reactions. Although everyone produces IgE antibodies, most allergy sufferers have an inherited tendency to overproduce these agents. IgE antibodies can induce other cells, particularly mast cells and basophils (special sentinel cells, as I explain in “Reacting to allergen exposures,” later in this chapter), to start a complex chain reaction that culminates in your allergy symptoms.
Mast cell surfaces have special IgE receptor sites. Two allergen-specific IgE antibodies linking to an allergen (such as pollen, animal dander, molds, dust mite allergens, insect sting venom, and certain foods and drugs) on the mast cell surface can trigger a Type I allergic reaction (see “Classifying Abnormal Immune Responses,” later in this chapter).
 Thymus: Secretions of special hormones (such as thymosin) from this gland are vital for regulating your immune system’s functions. The thymus also helps “educate” (encode) certain T-cells, which then play a key role in developing antibodies against antigens.
Thymus: Secretions of special hormones (such as thymosin) from this gland are vital for regulating your immune system’s functions. The thymus also helps “educate” (encode) certain T-cells, which then play a key role in developing antibodies against antigens.
 Lymph nodes: The lymphatic system provides drainage for your immune system. Your lymph nodes filter out material that comes from an infection. If you seem to have, for example, strep throat, your doctor checks for swollen lymph nodes downstream from the infected area (under your throat) as an indication of infection.
Lymph nodes: The lymphatic system provides drainage for your immune system. Your lymph nodes filter out material that comes from an infection. If you seem to have, for example, strep throat, your doctor checks for swollen lymph nodes downstream from the infected area (under your throat) as an indication of infection.
 Spleen: This organ filters and processes antigens in your blood.
Spleen: This organ filters and processes antigens in your blood.
 Lymphoid tissues: These important immune system participants, which include your tonsils, adenoids, appendix, and parts of your intestines, help process antigens.
Lymphoid tissues: These important immune system participants, which include your tonsils, adenoids, appendix, and parts of your intestines, help process antigens.
Inflaming you for a good reason
You may wonder why you’re equipped with IgE antibodies if they’re so problematic. This seemingly bothersome immunoglobulin is actually a significant part of the reason the human species has made it this far. During prehistoric days, in addition to the challenges of hunting and gathering daily meals (and trying not to become another animal’s chow in the process), humans also had to contend with all sorts of infec- tious agents, especially parasites.
The potent inflammatory action triggered when a parasite-specific antigen would bind with cell-bound IgE antibodies probably ensured that parasitic infections couldn’t affect enough humans to endanger the species. In fact, IgE antibod- ies remain important players in the immune responses of some people in less-developed regions of the world, where parasites continue to pose threats to human health — but where rates of asthma and allergies are much lower than in the more developed world. Occasionally, I see patients who have recently arrived from less-developed countries and who have highly elevated IgE and eosinophil (specialized white blood cells that play an important role in the inflammatory process) levels in their blood tests. In those cases, I rule out parasitic infections before moving on to a more likely diagnosis of an allergic condition. However, because parasites are such an extremely rare problem in the U.S. population, elevated IgE and eosinophil levels are almost always a sign that I’m dealing with an allergic patient.
In most modern-day humans, IgE antibodies play a role similar to that of fat cells. In prehistoric days, humans needed fat cells to store food and stave off hunger when their hunting and gathering was less than productive. Now human fat cells turn into love handles, and IgE antibodies trigger allergies.
Some researchers have hypothesized that exposure to key types of infections during childhood leads the immune system to function properly and focus primarily on developing antibodies against harmful agents that enter the body. However, for reasons that are currently the subject of intense scientific inquiry and debate, the vast majority of asthma and allergy sufferers have an immune system that also works overtime to protect the body against mostly harmless allergens.
According to some studies, attempts to provide near-antiseptic environments for infants and young children may partially be to blame for this type of overzealous immune system and the resulting high incidence of asthma and various allergies in the most developed parts of the world. One of the main arguments of this so-called “hygiene hypothesis” is that without a real threat to our health (such as infectious diseases) during our early years — and the widespread use nowadays of immunizations, antibiotic therapy, and better hygiene — the “bored” immune system fixates on any foreign protein, however innocent, which enters the body. As a result, the body’s immune system produces antibodies intended to destroy that relatively harmless invader the next time the immune system detects its presence.
Protecting and serving in many ways

 Humoral immunity: This component (which isn’t a vaccine against stand-up comedians) acts similarly to an internal air force, using B-cells (see “Classifying Immune System Components and Disorders,” earlier in this chapter) to produce and deploy antibodies (the immune system’s equivalent of high-tech weaponry). This component provides your body with its primary defense mechanism against bacterial infection and also plays a major role in developing allergies in people with a family history of atopy (the genetic susceptibility that can predispose the immune system to develop hypersensitivities and produce antibodies to otherwise harmless allergens).
Humoral immunity: This component (which isn’t a vaccine against stand-up comedians) acts similarly to an internal air force, using B-cells (see “Classifying Immune System Components and Disorders,” earlier in this chapter) to produce and deploy antibodies (the immune system’s equivalent of high-tech weaponry). This component provides your body with its primary defense mechanism against bacterial infection and also plays a major role in developing allergies in people with a family history of atopy (the genetic susceptibility that can predispose the immune system to develop hypersensitivities and produce antibodies to otherwise harmless allergens).
 Cell-mediated immunity: This component uses T-cells (see “Protecting Your Health: How Your Immune System Works,” earlier in this chapter) and related cell products (sort of like the army, battling in the trenches), rather than antibodies, to directly protect you against viruses, fungi, intracellular organisms, and tumor antigens.
Cell-mediated immunity: This component uses T-cells (see “Protecting Your Health: How Your Immune System Works,” earlier in this chapter) and related cell products (sort of like the army, battling in the trenches), rather than antibodies, to directly protect you against viruses, fungi, intracellular organisms, and tumor antigens.
 Phagocytic immunity: The function of this component is similar to a mop- up squad (or vultures and other scavengers), because it uses so-called scavenger cells (macrophages) that circulate throughout your body, looking for debris to clean up. This form of immunity doesn’t play a significant role in the allergic process.
Phagocytic immunity: The function of this component is similar to a mop- up squad (or vultures and other scavengers), because it uses so-called scavenger cells (macrophages) that circulate throughout your body, looking for debris to clean up. This form of immunity doesn’t play a significant role in the allergic process.
 Complement: This term describes a composite system of plasma and cell membrane proteins that interact with one another, as well as with antibodies, and serve as important mediators in your civil defense system, protecting the homefront like the Department of Homeland Security. Diseases associated with complement deficiency vary depending on which component of the complement system is lacking. Some people may have an increased susceptibility to infection, some may experience a rheumatic disorder (such as lupus erythematous or rheumatoid arthritis), and some may have hereditary angioedema (deep swellings) that occur without hives and can potentially cause life-threatening symptoms.
Complement: This term describes a composite system of plasma and cell membrane proteins that interact with one another, as well as with antibodies, and serve as important mediators in your civil defense system, protecting the homefront like the Department of Homeland Security. Diseases associated with complement deficiency vary depending on which component of the complement system is lacking. Some people may have an increased susceptibility to infection, some may experience a rheumatic disorder (such as lupus erythematous or rheumatoid arthritis), and some may have hereditary angioedema (deep swellings) that occur without hives and can potentially cause life-threatening symptoms.
Distinguishing between immune deficiencies and allergic conditions

If your doctor advises testing for immune deficiency, she isn’t necessarily ordering an HIV test. (Remember, HIV is the virus that causes AIDS.) Instead, your physician is most likely ordering immune-deficiency tests to rule out other types of diseases.

Keep in mind the following important points about immunodeficiencies and allergic conditions:
 In most cases, if you have allergies and a medical history of recurring infections, your over-responsive immune system is actually swamping your system with excess mucus that gets infected and indirectly causing your infections such as sinusitis or bronchitis.
In most cases, if you have allergies and a medical history of recurring infections, your over-responsive immune system is actually swamping your system with excess mucus that gets infected and indirectly causing your infections such as sinusitis or bronchitis.

 In more than 20 years of treating patients for recurring infections, I’ve seen only a handful of patients with immune deficiencies. In the vast majority of cases, I found that these patients actually had allergies.
In more than 20 years of treating patients for recurring infections, I’ve seen only a handful of patients with immune deficiencies. In the vast majority of cases, I found that these patients actually had allergies.
 If you have a bacterial infection such as sinusitis or bronchitis, your physician should evaluate whether your infection is a complication of allergic rhinitis (hay fever) and/or asthma before checking for much less common immune deficiencies.
If you have a bacterial infection such as sinusitis or bronchitis, your physician should evaluate whether your infection is a complication of allergic rhinitis (hay fever) and/or asthma before checking for much less common immune deficiencies.
.jpg)
 Doctors can rule out the vast majority of immune-deficiency syndromes by using simple blood tests that measure your blood count and anti-body levels. For this reason, I strongly advise against indiscriminately receiving gamma-globulin therapy (see the “Classifying Immune System Components and Disorders” section, earlier in this chapter) unless you first have an immune work-up that reveals a significant deficiency requiring this kind of treatment.
Doctors can rule out the vast majority of immune-deficiency syndromes by using simple blood tests that measure your blood count and anti-body levels. For this reason, I strongly advise against indiscriminately receiving gamma-globulin therapy (see the “Classifying Immune System Components and Disorders” section, earlier in this chapter) unless you first have an immune work-up that reveals a significant deficiency requiring this kind of treatment.
Immunizing and immunology
You often hear that life is a constant learning process. This statement is especially true for your immune system. In fact, your immune system is a seemingly limitless learning machine. It constantly memorizes countless antigens and remembers these encounters, allowing your defenses to react to future exposures.
The memory chips of any computer that you use in your lifetime pale in comparison to your immune system’s virtual total recall. Through the humoral component (see “Protecting and serving in many ways,” earlier in this chapter), your immune system can recognize hundreds of trillions of antigens and produce specific antibodies against each and every one of these substances. Compare this feat to remembering the name, looks, and characteristics of every single person, animal, and plant that you encounter throughout your lifetime (which could come in handy at your high school reunion).
Memorizing menaces to your health

Many ancient cultures recognized that people who survived infectious diseases were usually immunized against catching the same ailment again. In fact, ancient Chinese and Egyptian doctors practiced limited forms of immunization.
Fooling your immune system for your own good

Vaccines developed thanks to advances in immunology are the main reason that parents in the United States and many other parts of the world no longer need to worry about their children succumbing to a summer epidemic of polio. Other diseases that medical science has successfully brought under control as a result of immunizations include smallpox, diphtheria, pertussis (whooping cough), tetanus, chickenpox, measles, German measles (rubella), and mumps, as well as some forms of hepatitis and meningitis.
In fact, stimulating your immune system into producing a protective immune response against allergens is the underlying basis of immunotherapy (allergy shots), as I explain later in this chapter.
Classifying Abnormal Immune Responses
As I mention earlier in this chapter, your immune system can cause you trouble when it malfunctions, either because of a deficiency or by doing its job too well. Scientists refer to these abnormal responses according to four distinct classifications of reactions.

IgE-mediated reactions (Type I)
IgE-mediated reactions (Type I) result in immediate allergic reactions. Also known as immediate hypersensitivity, they often result from an insect sting or the injection of a drug such as penicillin in people who have extreme sensitivities to these triggers. The most dramatic and dangerous Type I reaction is anaphylaxis (see Chapter 1).
Allergic asthma, allergic rhinitis, and certain types of drug allergies are other examples. Because of the sudden onset of the allergic reaction, allergy skin testing (see Chapter 11) can provide quick results in identifying the triggers in many cases. For a more in-depth explanation of Type I reactions, see “Developing an Immediate Hypersensitivity,” later in this chapter.
Cytotoxic reactions (Type II)
Cytotoxic reactions (Type II) involve the destruction of cells, such as the reactions that result when red blood cells break down. This mechanism can potentially lead to anemia and fewer platelets, a situation that decreases your blood’s ability to clot.
Certain drugs, such as penicillin, sulfonamides, and quinidine, can trigger cytotoxic reactions. Type II reactions play a role in Rh-factor anemia and jaundice in newborns and are also the way a patient’s body may reject an organ transplant.
Immune complex reactions (Type III)
Manifestations of immune complex reactions (Type III) include fever, skin rash, hives, swollen, tender lymph nodes, and aching or painful joints. These types of reactions are among the ones that physicians usually refer to as serum sickness. Typically, these symptoms appear one to three weeks after taking final doses of drugs such as penicillin, sulfonamides, thiouracil, and phenytoin.
Type III reactions also play a role in the development of autoimmune disorders, such as systemic lupus erythematous, rheumatoid arthritis, some forms of diabetes, and certain types of kidney disease.
Cell-mediated reactions (Type IV)
Allergic contact dermatitis is one of the primary examples of cell-mediated reactions (Type IV), a localized, non-systemic reaction. Doctors also use the term delayed hypersensitivity to describe this process, in which contact with an allergen results in an allergic reaction hours or even days later. (For example, if you have allergic contact dermatitis, you may not realize that you’ve contacted poison ivy until you’re driving home from your weekend camping trip.)
Although the delayed reaction is rarely life-threatening, in some cases it may take longer to subside or disappear than reactions involving atopic conditions, such as immediate hypersensitivity (see “IgE-mediated reactions [Type I],” at the beginning of this section).
Developing an Immediate Hypersensitivity
Type I allergic reactions involve numerous complex processes, with many players taking part in various ways. This section explains the roles that the most important cells and chemicals play in developing your sensitivities and triggering your reactions.
Setting the stage for allergic reactions

 Mast cells: These connective-tissue cells play a pivotal role in allergic disease processes. Mast cells are primarily located near blood vessels and mucus-producing cells in the tissues that line various parts of your body. With allergies, doctors concern themselves with your mast cells’ actions in the lining of your eyes, ears, nose, sinuses, throat, the airways of your lungs, your skin, and your gastrointestinal (GI) tract.
Mast cells: These connective-tissue cells play a pivotal role in allergic disease processes. Mast cells are primarily located near blood vessels and mucus-producing cells in the tissues that line various parts of your body. With allergies, doctors concern themselves with your mast cells’ actions in the lining of your eyes, ears, nose, sinuses, throat, the airways of your lungs, your skin, and your gastrointestinal (GI) tract.
 Basophils: These cells live in your bloodstream near the surfaces of tissues and are important players in late-phase reactions. (See “Reacting to allergen exposures,” later in this chapter, for more information.)
Basophils: These cells live in your bloodstream near the surfaces of tissues and are important players in late-phase reactions. (See “Reacting to allergen exposures,” later in this chapter, for more information.)

Mast cells and basophils are among the first cells that antigens encounter when entering your body. These sentinel cells are coated with numerous IgE receptor sites that can accommodate IgE antibodies that are specific to various allergens (corresponding, for example, to different pollens and animal dander).
These cells also contain potent chemical mediators of inflammation that are released when IgE and a specific allergen cross-link and activate them, resulting in the inflammation that leads to allergic symptoms.
 Eosinophils: Other mediators, including those from mast cells, attract these white blood cells to the site of an allergic reaction and generate an array of inflammatory mediators, including enzymes that can cause tissue damage. Eosinophils also play prominent roles in late-phase reactions that affect some people with asthma, particularly with symptoms of chest congestion that can occur hours after an initial episode of asthma. (See “Reacting to allergen exposures,” later in this chapter.) If you have uncontrolled asthma, the chronic inflammatory process may lead to airway remodeling — the replacement of healthy tissue with scar tissue — and can potentially cause irreversible loss of lung function.
Eosinophils: Other mediators, including those from mast cells, attract these white blood cells to the site of an allergic reaction and generate an array of inflammatory mediators, including enzymes that can cause tissue damage. Eosinophils also play prominent roles in late-phase reactions that affect some people with asthma, particularly with symptoms of chest congestion that can occur hours after an initial episode of asthma. (See “Reacting to allergen exposures,” later in this chapter.) If you have uncontrolled asthma, the chronic inflammatory process may lead to airway remodeling — the replacement of healthy tissue with scar tissue — and can potentially cause irreversible loss of lung function.
Preventing this type of serious lung damage is one of the main goals of treating asthma early and aggressively, particularly with inhaled corticosteroids. (See Chapter 15 for an extensive survey of asthma-controller medications.) Because eosinophils tend to increase in the bloodstream of patients with allergic asthma, your doctor may order a complete blood count (CBC) including a peripheral eosinophil count when diagnosing your condition.

 Attract other inflammatory cells to the area to amplify the inflammatory reaction.
Attract other inflammatory cells to the area to amplify the inflammatory reaction.
 Cause tissue damage, often with accompanying pain and discomfort.
Cause tissue damage, often with accompanying pain and discomfort.
 Constrict the smooth muscles of your respiratory airways.
Constrict the smooth muscles of your respiratory airways.
 Dilate your blood vessels, leading to increased fluid leakage, which increases inflammatory action.
Dilate your blood vessels, leading to increased fluid leakage, which increases inflammatory action.
 Increase mucus secretions, resulting in a runny nose, watery eyes, cough, and chest congestion, depending on where the trigger causes the allergic reaction.
Increase mucus secretions, resulting in a runny nose, watery eyes, cough, and chest congestion, depending on where the trigger causes the allergic reaction.
 Promote the production of IgE and activate the eosinophils, thus supporting allergic inflammation.
Promote the production of IgE and activate the eosinophils, thus supporting allergic inflammation.
Reacting to allergen exposures

1. Your immune system receives exposure to an allergen.
Allergen exposures can result from the following occurrences:
• Inhaling: Inhalant allergens (or aeroallergens) such as pollens, molds, dust mite allergens, and animal dander often pass through your nose and/or your mouth, putting the allergens in contact with immune cells lining your nose, mouth, throat, and airways of the lungs. Common symptoms of these exposures include runny nose, sneezing, watery eyes, stuffy nose, postnasal drip, coughing, chest tightness, wheezing, and shortness of breath.
• Ingesting: You may swallow allergens, such as those contained in peanuts, shellfish, eggs, milk, or in drugs such as penicillin. These exposures can trigger oral symptoms such as itching and swelling of the tongue, lips, and throat; GI tract symptoms such as nausea, stomach cramps, vomiting, and diarrhea; skin reactions such as hives and angioedema; and respiratory symptoms such as coughing, wheezing, and shortness of breath.
• Injecting: Medical syringes and insect stingers are vehicles for injecting allergens. Injections can cause particularly severe reactions because allergens go directly into your bloodstream, which can spread the allergens rapidly to organs throughout your body. Penicillin shots are the most dramatic (and often severe) examples of drug-related anaphylaxis in people with penicillin hypersensitivities. The venom from stinging insects can also cause potentially life-threatening reactions.
• Touching (direct contact): Direct contact exposures typically involve Type IV delayed hypersensitivity responses, including reactions to poison ivy, nickel, and latex, among numerous others. Symptoms from direct contact usually result in localized, topical reactions such as skin rashes.
2. Your body develops an IgE antibody response to the allergen.
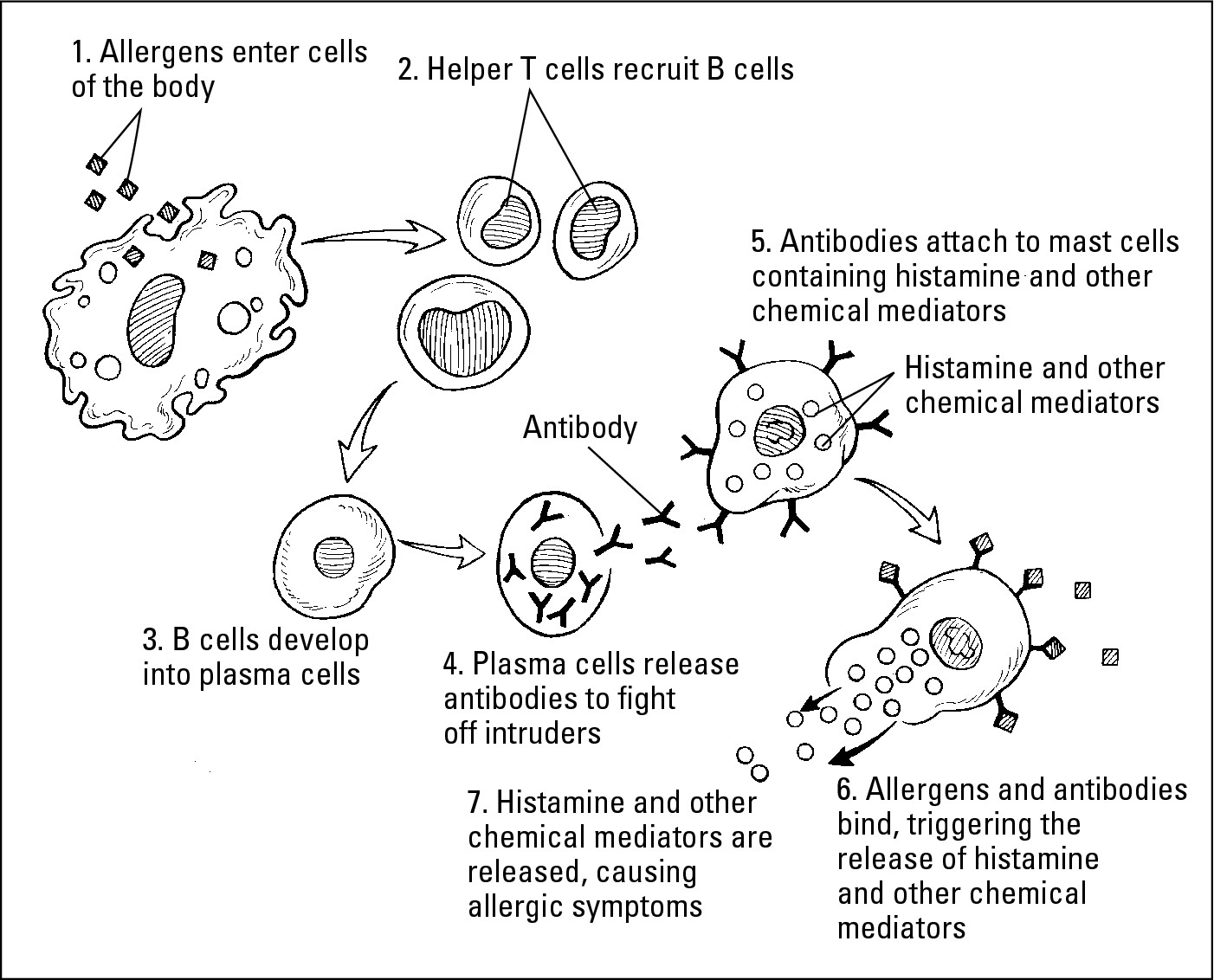
If you have an atopic predisposition for developing allergies, scavenger cells (macrophages) that usually rid your body of foreign proteins (such as allergens) act as antigen- (allergen-) presenting cells. This setup triggers T-cells to recruit B-cells that develop into plasma cells. This process culminates in the production of specific IgE antibodies designed against the allergen (see Figure 6-1).
3. Allergens bind to specific IgE antibodies attached to the surface of mast cells or basophils.
The first time you’re exposed to the allergen, you don’t typically experience a reaction. However, you produce specific IgE antibodies that bind to receptor sites on mast cells. Thus your immune system is sensitized, and further exposure to that allergen initiates an allergic response.
4. You’re re-exposed to the allergen.
The allergen attaches to two specific IgE antibodies on the mast cell surface.
|
Figure 6-1: The allergic inflam- matory response is a complex process involving many types of cells. |
|
5. The allergen cross-links to two specific IgE antibodies on the mast cell surface. This activates the mast cell to release its potent chemical mediators of inflammation, which affect various organs and trigger your allergic symptoms.
In some cases, particularly with reactions to insect stings and penicillin, you may think that your allergic reaction was the result of just a single exposure. In most instances, however, you received a prior, sensitizing exposure, perhaps in one of the following ways:
• With regard to insect stings, you may have been stung as a child. If that experience wasn’t traumatic and resulted only in a minor, localized reaction, you may have forgotten about it.
• Your first exposure to penicillin allergens may be even less memorable: The cow’s milk or beef that you eat can include this antibiotic from the animal’s feed.
Doing it one more time: The late-phase reaction
.jpg)
Because antihistamines and quick-relief bronchodilators are only effective for dealing with early-phase reactions, your doctor may need to prescribe corticosteroids to control late-phase symptoms. Immunotherapy is a unique form of treatment that helps decrease both early- and late-phase reactions to allergen exposures, as I explain in “Reaping the Benefits of Immunology,” later in this chapter.
Becoming hyperresponsive
Typically, if you’re chronically exposed to an allergen — for instance, animal dander — you may find that during ragweed season, your symptoms appear to become more bothersome even at lower levels of exposure than you have experienced previously. By increasing your allergen load (your total level of exposure, at any one time, to any combination of allergens that trigger your allergies — see Chapter 10), other allergens and irritants may be more likely to also cause problems for you. In this case, eliminating animal dander from your home could result in fewer asthma and/or allergy symptoms during ragweed season.
Conversely, although your friend’s cat may not be an issue for you most of the year, Fluffy’s dander may trigger your asthma and/or allergic rhinitis symptoms during ragweed season. That’s because exposure to the pollen causes you to develop a lower threshold for allergy symptoms (making you hyperresponsive ) when exposed to this friendly feline.
Reacting nonspecifically
Another reaction complication that occurs from chronic allergen exposure is an increase in nonspecific reactivity. Nonspecific reactivity develops when your nasal passages and breathing airways become so inflamed and sensitized by repeated, constant exposure to triggering allergens that nonallergic irritants also cause reactions. Nonspecific irritants often include
 Tobacco smoke (from cigarettes, cigars, pipes)
Tobacco smoke (from cigarettes, cigars, pipes)
 Fumes and scents from household cleaners, strongly scented soaps, and perfumes and colognes; from glues, solvents, and aerosols; and from unvented gas, oil, or kerosene stoves
Fumes and scents from household cleaners, strongly scented soaps, and perfumes and colognes; from glues, solvents, and aerosols; and from unvented gas, oil, or kerosene stoves
 Smoke from wood-burning appliances or fireplaces
Smoke from wood-burning appliances or fireplaces
 Air pollution
Air pollution
 Gases, from chemicals found primarily in the workplace
Gases, from chemicals found primarily in the workplace
.jpg)
Reaping the Benefits of Immunology
Immunology provides great benefits for treating asthma and other allergic conditions, enabling doctors to modify your immune system’s reactions to triggers of airway disease with immunotherapy (allergy shots). The immunologic response that results from immunotherapy promotes immune system actions that protect rather than damage your body, as I explain in Chapter 11.
Immunotherapy is the most effective way, in most cases, to treat the underlying causes of allergic ailments such as allergic asthma, allergic rhinitis (and allergic conjunctivitis), and allergies to insect stings.
Enhancing your future with immunology
The advances that medical science has made with immunology during the last century are among the greatest human achievements in the history of mankind, producing medical miracles that would’ve seemed like sheer fantasy 100 years ago. The continued progress in our understanding of immunology can enable medical researchers to find far more effective ways of preventing infectious diseases. Immunologic research has already helped control some forms of cancer with the use of interferons, anti-tumor antibody therapy, and other immunologic interventions.
In the quest for more effective medications to control asthma and other allergic disease symptoms, immunology has been the key to developing a new and innovative medication, based on using a high-tech antibody known as recombinant human monoclonal antibody (rhuMab), which is an anti-IgE antibody. The first drug in this class, omalizumab/ rhuMAb-E25 (Xolair) — recently approved by the FDA — binds immunologically with circulating IgE. This process prevents the binding of IgE to mast cells, thus blocking the initiation of the allergic reaction. (I discuss IgE antibodies more extensively in Chapter 17.)
The study of immunology matters a great deal to the whole human race. Physicians and scientists must continue to advance their knowledge about the immune system and unlock its secrets. The 21st century will see the development of vaccines for many serious diseases such as herpes; respiratory syncytial virus (RSV) infections, which cause bronchiolitis in infants (see Chapter 18); and the worldwide scourge of AIDS. Likewise, the 21st century will also result in the development of more effective forms of immunotherapy for allergies. Immunologic research may one day even produce a vaccine against allergies and asthma. (If that happens, and my patients no longer need my care, maybe I could fulfill my fantasy of trying out for a spot on the Senior Golf Tour.)