Hypertension is very common especially as you get older
Hypertension (high blood pressure) is a major public health problem that affects more than one billion people worldwide.
•In the UK, 31.5 per cent of all men and 29 per cent of all women have high blood pressure.
•One in three adults with hypertension is not receiving treatment, as hypertension is not always diagnosed.
•One in two people with hypertension do not have adequate blood pressure control.
•The proportion of the population who have hypertension rises with increasing age; while only 10–20 per cent of people aged 35–44 years have hypertension, 60–70 per cent of people aged 65–74 years have it.
•Men and women who live until they are 85 have a 90 per cent chance of developing hypertension, so most people will develop high blood pressure if they live long enough.
•In the USA, 78 million people, which is approximately one in three adults, have been diagnosed with high blood pressure and the estimated annual cost to treat them is 90 billion dollars.
Over their lifetimes, hypertension affects men and women in equal numbers, although it is more common in women as they get older than men (Table 1).
The number of people with hypertension is predicted to increase by more than 50 per cent over the next 20 years. This is because of the increase in the number of people leading lifestyles that are unhealthy because they involve being less physically active, eating high-calorie and high-salt diets, drinking more alcohol, and becoming obese. The good news is that these lifestyle changes are what we call modifiable risk factors, and it is possible for people to implement a healthier lifestyle (Chapters 9 and 10 give advice on how to do it). GPs and practice nurses can also offer advice.
Table 1 Hypertension in men and women in different age groups
| Age | Men (%) | Women (%) |
| 20–34 | 11.1 | 6.8 |
| 35–44 | 25.1 | 19.0 |
| 45–54 | 37.1 | 35.2 |
| 55–64 | 54.0 | 53.3 |
| 65–74 | 64.0 | 69.3 |
| 75 and older | 66.7 | 78.5 |
| All | 34.1 | 32.7 |
Source Heart disease and stroke statistics – 2013 update: a report from the American Heart Association. Circulation 2013; 127:e6–245.1
Hypertension is the leading risk factor for many diseases
High blood pressure is the number one global risk factor for premature disease and carries a higher risk for this than smoking and alcohol consumption. High blood pressure has a substantial impact on the quality of many lives and is involved in heart disease, stroke, kidney failure and dementia. Around half of all people with heart disease and three-quarters of all those who have had a stroke have high blood pressure. Hypertension is the second most common cause for kidney failure that requires dialysis; diabetes is the most common cause for this. Most people diagnosed with high blood pressure are often obese, have high blood cholesterol levels and frequently develop diabetes, which are all risk factors for heart disease. This combination of risk factors, which is often referred to as metabolic syndrome, greatly increases the chances of heart disease and stroke.
How do you know if your blood pressure is high?
High blood pressure is often referred to as ‘the silent epidemic’ because it does not cause any symptoms until organ damage is apparent. GP surgeries and home monitoring programmes need to provide routine blood pressure readings for diagnosis and GP surgeries need to provide effective treatments for high blood pressure. In the UK, blood pressure checks are now a routine part of NHS health checks and everyone aged between 40 to 74, who do not have heart disease or previous stroke, should get a health check every five years. This involves completing a medical history, having a blood pressure check and routine blood tests so that GPs can calculate each person’s risk of heart disease.
The doctors and nurses in GP surgeries lead the way with screening and treatments for hypertension and only a small proportion of patients with high blood pressure are referred to hospital specialists, such as myself, for further investigation and treatment. If you are aged over 40 and have not had a health check recently that included measuring your blood pressure, then you should see your GP to request one. Many pharmacists also now provide a service to check blood pressure. Pharmacists can also advise on purchasing automated blood pressure monitors that are accurate and relatively inexpensive and can be used at home.
We need to look after people with high blood pressure better
Despite the availability of medications that effectively lower blood pressure and the relative ease of monitoring blood pressure, a significant proportion of people with high blood pressure are not identified in the first place. This is because large numbers of the population do not regularly see health professionals. Also, up to half of all people who are being treated for high blood pressure do not reach their target blood pressure levels (see Chapter 8), as people need to have the motivation to take the prescribed medication and make changes to their lifestyles. It is understandable that many of us do not like taking tablets when it does not make us feel better. High blood pressure is different to other conditions, such as arthritis or angina where effective treatment improves quality of life, because if your blood pressure is high, often there are no obvious signs or symptoms at all. There are no unpleasant symptoms to be alleviated by drugs, although you may sometimes experience symptoms, such as a headache, with high blood pressure. This means that drugs for hypertension are often prescribed to prevent other diseases, which doesn’t meet the perception of medicine as a cure for an existing, troublesome condition.
What is blood pressure?
Before we can look at how best to manage blood pressure, it is important to understand the term ‘blood pressure’. The Oxford Dictionary defines pressure as a ‘physical force’. A useful working definition for blood pressure is: the force in the circulation that pushes blood around the body.
All the cells in our bodies need a continuous supply of arterial blood, which carries oxygen and nutrients. A constant forward pressure is needed in the circulation to keep the blood flowing, and ensure that the organs and tissues remain healthy. Blood pressure is that forward pressure in our circulation. The pumping action of the heart generates this pressure that drives oxygen-rich blood to every cell in the body.
Cardiac output as a measure of heart function
The heart is an amazing muscular pump that generates the force required to push blood around your circulation. Each day the heart beats about 100,000 times at an average rate of 70 beats per minute. This equates to around 38 million beats per year and over 2.5 billion times for a lifetime of 70 years. It is incredible to think that your heart can achieve this level of work without needing repair of any sort.
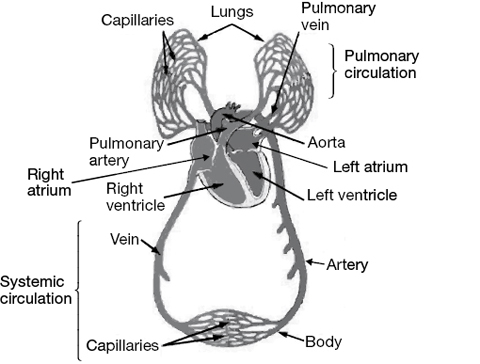
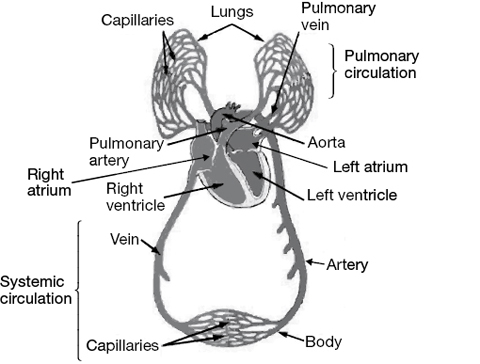
Figure 1 The circulatory system
The right-hand side of the heart pumps blood to the lungs where carbon dioxide is removed and oxygen is restored to the blood. The oxygenated blood is then returned to the muscular left ventricle of the heart, which then pumps the blood to the body’s vital organs and tissues. With each heartbeat, blood travels down small blood vessels called capillaries that supply the tissues. If lined up side-by-side, the estimated length of the circulatory system would be more than 50,000 miles (Figure 1).
Stroke volume
The force of the contraction of the heart can be measured as the stroke volume: this is the volume of blood that the heart ejects with every contraction that it makes. The average stroke volume is around 70 millilitres and if this figure is multiplied by the heart rate, it gives the cardiac output, which is approximately 5 litres per minute. Blood pressure is a combination of the force and rate of the heartbeat and the vascular resistance, that is, the resistance of the blood vessels to this force. This means that any increases in heart rate, stroke volume or vascular resistance will push blood pressure higher. In practice, the most common cause of high blood pressure is increased vascular resistance.
Blood pressure = force and rate of heartbeat x vascular resistance
What is vascular resistance?
The circulation of blood in the arteries involves a series of tubes of decreasing diameters carrying blood from the heart to the tissues. Artery walls have elastic and muscular tissue that allows them to stretch and absorb some of the force of the pumping blood with each heartbeat. The circular layer of muscle around the arteries can also change the width (diameter) of the arteries. The combined length of tubing in the arterial circulation produces a vascular resistance that has to be overcome for the blood to reach the cells.
Arterioles are the small arteries at the end of the circulation that branch out to supply the tiny blood vessels (capillaries) in the tissues. The arterioles have a relatively thick muscular wall and are some of the most highly regulated blood vessels in the circulation. They contribute most to the total vascular resistance and are constantly changing size to speed up or slow down tissue blood flow. The diameter of these resistance arterioles is under continuous regulation via a complex system of chemical and electrical nerve impulses (Figure 2).

Figure 2 Vasoconstriction and vasodilatation
•Vasoconstriction (a decrease in blood vessel diameter) occurs when the muscular layer in the arterial wall contracts. This increases vascular resistance.
•Vasodilatation (an increase in blood vessel diameter) occurs when the muscular layer in the arterial wall relaxes. This decreases vascular resistance.
Adrenaline is a powerful hormone that reduces the diameter of arteries (constriction), increases heart rate, and strengthens heart contractions; all of which leads to an increase in blood pressure. This is why adrenaline is used in medical emergencies where the blood pressure is dangerously low, such as after a cardiac arrest (when the heart stops) or anaphylaxis (a severe and life-threatening allergic reaction).
Most causes of high blood pressure are linked to an increase in the vascular resistance due to a decrease in the diameter of blood vessels (vasoconstriction) and many of the drug treatments for hypertension lower blood pressure by causing dilatation of blood vessels and, therefore, a decrease in the vascular resistance (Figure 3).
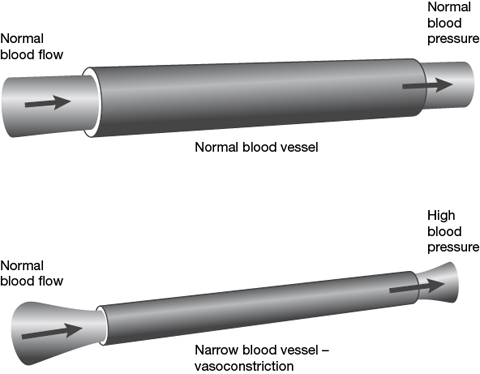
Figure 3 Diagram showing high blood pressure due to vasoconstriction and high vascular resistance
Can low blood pressure be a problem?
A very low blood pressure can also cause problems. Sometimes heart function abnormalities will cause a very slow heartbeat or reduce the contraction of the heart. This is an important cause of low blood pressure. Patients with severe heart failure may present with signs and symptoms of poor blood flow due to their low blood pressure. This is known as cardiogenic shock and is a life-threatening condition requiring urgent treatment to improve heart function. A common cause of cardiogenic shock is severe damage to the heart caused by a heart attack. Emergency hospital treatment to improve blood flow to the heart can be life-saving.
Other causes of low blood pressure include bleeding and dehydration. These conditions lead to a reduction in the circulating blood volume (hypovolaemic shock). Severe infection (septic shock) can also cause low blood pressure due to release of toxins and low vascular resistance. Acutely sick patients with low blood pressure are often treated in hospital intensive care units. These patients need to be carefully monitored and treated with intravenous fluids and drugs to increase vascular resistance. This will increase their blood pressure to acceptable levels, which will prevent organ damage caused by inadequate blood flow.
Systolic and diastolic blood pressure
Our blood pressure is made up of two components: a peak and a trough. The peak – systolic – blood pressure is generated by the contraction (systole) of the heart, during which blood is forcefully ejected from the heart. The trough – diastolic pressure – occurs when the heart relaxes (diastole) and blood pressure falls as the heart starts filling with blood. Blood pressure is measured in millimetres of mercury (mmHg). The systolic blood pressure is recorded first and then the diastolic pressure. Someone with a systolic blood pressure of 140 mmHg and diastolic blood pressure of 80 mmHg would be told that his or her blood pressure was 140 over 80, which is written as 140/80. Diastolic blood pressure does not fall rapidly between heartbeats because of the elasticity of the arteries. Some of the force generated by each heart contraction is stored as energy in the arteries as they stretch (this is known as the elastic reservoir capacity). This force is released during diastole to maintain pressure in the circulation. You can imagine this if you think of the air trapped in a blown-up balloon; the trapped air is under pressure due to the elastic forces stored in the balloon wall. The arteries act as pressure reservoirs that constantly absorb and release elastic force to maintain the pressure in the circulation.
What is pulse pressure?
The difference between systolic and diastolic blood pressure readings is known as the pulse pressure. As people get older the large arteries in the body become progressively stiffer. This causes an increase in systolic blood pressure, a decrease in diastolic blood pressure and a widening of the pulse pressure. A pulse pressure of more than approximately 55 mmHg in people aged over 60 is another risk factor for heart disease, because it often reflects an increased arterial stiffness caused by fatty deposits in the arterial wall. Another cause for a wide pulse pressure is damage to the aortic valve, which is the main heart valve that opens to let blood leave the heart during each heart contraction. During relaxation, or diastole, of the heart, the aortic valve closes to prevent blood leaking back into the heart. A faulty valve does not completely shut during diastole allowing blood to regurgitate back from the aorta to fill the heart. One of the signs of severe aortic valve incompetence is a wide pulse pressure.
Regulation of blood pressure
Baroreceptors and the autonomic nervous system
The body has a complex system for monitoring its own blood pressure. This system is continuously adapting to our physiological requirements to ensure that our blood pressure is maintained within a normal range. Specialised pressure sensors called baroreceptors are present in the aortic arch and carotid sinuses. These areas are richly innervated with nerve endings that respond to the stretching of the arterial wall during each heartbeat. The nerve inputs conduct signals back to the blood pressure-regulating centre located in the brain stem. This is the stem-like section of the brain that connects the brain hemispheres to the spinal cord, and, in evolutionary terms, is thought to be the oldest part of the brain. If the blood pressure rises suddenly, signals are sent from the baroreceptors to the brainstem, which acts to decrease blood pressure using the autonomic nervous system.
The two main systems used by the body for blood pressure balance are the autonomic system and the kidneys. Historically, hypertension research focused on how the kidneys control blood pressure. However, recent work to develop new hypertension treatments has increased the attention given to the role of the autonomic system. The autonomic nervous system comprises a complex network of nerves throughout the body that consists of the sympathetic nervous system and the parasympathetic nervous system. These two parts work in opposite ways, like yin and yang, to maintain balance (homeostasis) in the body. The sympathetic system prepares the body for action and increases blood pressure by increasing our heart rate, force of heart contractions and vascular resistance. Exercise and stress activate the sympathetic system and lead to increases in blood pressure. This means that it is important to have your blood pressure measured when you are sitting down and relaxed, with a resting heart rate that is typically between 60 and 100 beats per minute. If you have been rushed to the clinic, you must make sure that you are seated and comfortable before having a blood pressure reading. The parasympathetic system relaxes the body and decreases blood pressure by slowing the heart rate, reducing the force of heart contractions and lowering the vascular resistance. The baroreceptor system is excellent at adapting to sudden changes in blood pressure. It is very responsive and works in minutes. However, it is not as effective for persistent elevation in blood pressure, which is thought to be often caused by chronic over-activation of the sympathetic system.
Blood pressure control and the kidneys
The kidneys receive a significant portion of the blood flow during each heartbeat. As well as filtering the blood, the kidneys contain numerous specialised cells that monitor blood pressure. If blood pressure falls, the kidneys sense this as a reduced blood flow and activate the RAAS (renin–angiotensin–aldosterone) system. Cells in the kidneys release a chemical messenger (hormone) called renin. This acts via angiotensin II (which is a hormone produced by the liver) to stimulate the release of aldosterone from the adrenal glands. Aldosterone is a potent hormone that increases blood pressure by causing constriction in blood vessels. Aldosterone also promotes salt retention by the kidneys, leading to higher salt, or sodium, levels that cause an increased blood volume and elevation in blood pressure.
The RAAS system is the target of several classes of drugs used to treat high blood pressure. These drugs include angiotensin converting enzyme (ACE) inhibitors, angiotensin receptor blockers (ARBS) and aldosterone receptor blockers. The RAAS system acts more slowly than the baroreceptors and causes a more persistent elevation in blood pressure. Chronically high blood pressure is often caused by abnormalities of kidney function along with activation of the RAAS system.
Diurnal variation in blood pressure
Blood pressure varies throughout the day, following a daily pattern that gives higher readings in the morning and lower readings in the evening. Your blood pressure starts to rise a few hours after you wake up and continues to rise during the day, peaking at mid-afternoon, and at its lowest during the evenings and at night. The typical variation in blood pressure can be between 10–15 mmHg for the systolic pressure and 5–10 mmHg for diastolic pressure. Therefore, if your blood pressure is 150/90 mmHg in the afternoon it may be as low as 135/80 mmHg during the night.
In healthy people, sleep reduces both systolic and diastolic blood pressure by 10–15 per cent, which is known as nocturnal blood pressure dipping. This is caused by changes in the balance of the autonomic nervous system, with reductions in sympathetic drive and the predominance of parasympathetic activity. This sleep-related blood pressure dipping is important for normal cardiovascular health, and if it doesn’t happen, there is an increased risk of heart disease. Obstructive sleep apnoea, an intermittent obstruction to normal breathing (see Chapter 4), is a common cause of both daytime and nocturnal hypertension because of the frequent interruptions in breathing.
It is important to remember this normal diurnal variation in blood pressure when diagnosing hypertension, as this diagnosis is often made on the basis of a reading during the afternoon blood pressure peak. Diagnosing hypertension can be done more accurately when blood pressure levels are monitored throughout the day (see Chapter 4) and the calculation of average blood pressure, ideally, should be based on several readings.