Chapter 5
Just Say No to the Milk Mustache
Healing Gastrointestinal Problems: Annie’s Story
I have to share what an altering life change the Paleo Diet has been for me. As far back as I can remember, I have had GI [gastrointestinal] problems. I remember going to the hospital to receive barium treatments and always being mortified. I was constantly drinking castor oil, having Metamucil with my orange juice, and suppositories at four years old.
As I became an adult, I had terrible acid reflux, but I just assumed that the reflux was due to my pregnancies. At twenty years old, I started to have severe abdominal cramping—food would run through my body faster than it took to consume it. I was always exhausted and could gain ten pounds at a time.
Finally, when my weight was up to 163 pounds, I was not able to hang onto anything I ate, and I was always so tired I felt drugged, I made an appointment with one of my state’s top gastroenterologists. He immediately gave me a prescription for an antispasmodic because he believed that I had IBS [irritable bowel syndrome], and then scheduled a day to do an EDG [esophagogastroduodenoscopy]. I came back for my EDG, and the doctor found that I have GERD [gastrointestinal reflux disease] and a hiatal hernia; he suspects IBS. I still seemed to have a difficult time with eating anything baked or dairy, and I was still gaining weight and still “dumping” my food.
A month later, I went in to see my GI doctor. He told me not to drink any mixed drinks, white wines, or beer. I thought, Well, that is okay. I do not drink that often.
Two months went by. A coworker suggested the Paleo Diet. I immediately started it and eventually began hiking four miles every morning—I am now up to running, and I am not a runner!
My results: since the middle of March, I have lost 44 pounds. I am now 119 pounds and a size 2! I have energy again and feel fabulous. Oh yes, I have a flat tummy again!
The food I was eating was slowly killing me. That sounds so dramatic, but it seriously was. My doctor said my body was in starvation mode and would hang onto anything it could. My belly was always distended, and I appeared to be six months pregnant.
I love the Paleo Diet and cannot say enough about it. I truly believe my tummy issues are genetic, and I have been dealing with celiac symptoms, lactose intolerance, GERD, and IBS all of my life. I have bought The Paleo Diet for everyone in my family.
My signature lecture, “Origins and Evolution of the Western Diet: Health Implications for the 21st Century,” is based on a scientific paper I published in the American Journal of Clinical Nutrition in 2005. In this lecture, I trace the chronological introductions of all of the food groups and the foods that have become part of the contemporary U.S. and Western diet. When I lecture, I like to engage the audience so that it becomes not just a one-way presentation by me but rather an interactive give-and-take conversation. When I get to the part about milk and dairy products, I pose a question: “How do we know that our hunter-gatherer ancestors never ate this food group?” In the ensuing pause before a few people raise their hands and give the correct answer, I flip to the next slide. Immediately appears an unruly herd of about thirty African Cape buffalo, snorting and pawing the earth with powerful hooves supporting their one-ton bodies, crowned by enormous menacing horns.
Have you ever tried to approach a wild animal? How about milking one? This is an impossible task, to say the least. Until the dawn of agriculture ten thousand years ago and the subsequent domestication of dairy animals, milk, butter, cheese, and yogurt were never part of our ancestors’ menu.
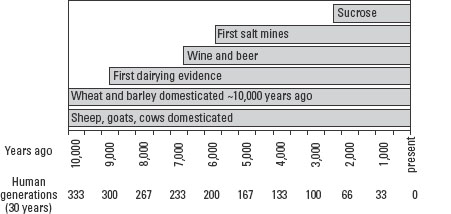
Although ten thousand years ago seems unimaginably distant compared to a single human life span, it is very recent on an evolutionary time scale. Only 333 human generations have come and gone since we first domesticated animals and began to consume their milk. As a species, we have had scant evolutionary experience to adapt to a food that now makes up about 10 percent of the calories in the American diet. Milk and dairy products have the enormous potential to disrupt our health and well-being through a variety of means that I barely touched on in The Paleo Diet. If you had any prior doubts about whether you should eat dairy foods, the information contained in this chapter should help you make an informed decision in the best interest of your health.
Milk and dairy products became part of the current Western diet during the period known as the Neolithic or New Stone Age, which began about 10,000 years ago and ended 5,500 years ago. The following graph shows just how recent dairy foods and other staples of the Western diet really are, when evaluated in an evolutionary time frame.
Unless you are lactose intolerant, have an allergy to milk and dairy products, or have been a devoted follower of the Paleo Diet, you probably don’t give a second thought to whether you should consume a food group that seems to be found nearly everywhere in the Western diet. Your favorite dairy foods may include ice cream, chocolate milk, fruit-flavored yogurt, or fancy imported cheeses. You may think that you are doing your body a favor by eating these calcium-rich foods. But remember this: we are the only species on the planet to consume another animal’s milk throughout our adult lives.
Introduction of Non-Paleo Foods into Human Diets
An increasing body of scientific evidence supports the evolutionary caution that this dietary practice is not necessarily harmless. The table below shows the sources and amounts of dairy foods in the U.S. diet.
These figures don’t tell the entire story, as dairy products are put into almost all processed foods. Take some time to read labels. If you are a milk chocolate addict, you are eating dairy, and the same goes for latté lovers. Nonfat milk solids, a major ingredient in chocolate, are also put into candy, cereal, bread, salami, bologna, sausages, baked goods, salad dressings, chips, condiments, soft drinks, and many other foods that come in a can, a jar, a bottle, a bag, or a plastic wrapper.
| Dairy Products | % Total Calories in U.S. Diet |
| Whole milk | 1.6 |
| Low-fat milks | 2.1 |
| Cheese | 3.2 |
| Butter | 1.1 |
| Other | 2.6 |
| Total | 10.6 |
Even though these tiny residues of milk in processed foods seem to be trivial, don’t fool yourself. Milk proteins and peptides (the building blocks of proteins) have a high potential to promote heart disease, cancer, allergies, and other health problems.
Let’s take a step back and look at the vast advertising campaign that the milk-processing industry has shoved down our throats for nearly twenty years. This glitzy promotional crusade with the “Got Milk” slogan depicts movie stars, sports personalities, politicians, and other public figures with a wet, white film of what appears to be milk on their upper lips. Implied in magazine ads, TV and radio commercials, and social media is the notion that all public figures with “milk mustaches” endorse dairy products, presumably because these are healthy and nutritious foods. Let’s stop for a minute and touch base with reality.
I haven’t drunk a glass of milk in nearly forty years, but if I were to, I certainly wouldn’t spill it all over my upper lip. This issue really doesn’t matter and is simply part of the industry’s advertising strategy—if the movie stars and the sports heroes do it, so should you. My question: why would a Wimbledon tennis champion, an Oscar-winning actress, and an Indy 500 race car driver blindly support a product they know virtually nothing about?
These public figures have spent their lifetimes honing talents, skills, and knowledge specific to their life callings. Yet when it comes to understanding milk’s intricate influence on our metabolism, hormonal function, and long-term health, most of these people are novices operating completely outside their areas of expertise, without knowledge or understanding of the facts. Like the public, they have bought into the milk-processing industry’s ad campaign, which portrays milk right along with motherhood, apple pie, and the American way.
This is exactly the message the milk-processing industry wants to convey to consumers because it sells more milk and dairy products, plain and simple. Is there a conspiracy by dairy industry middlemen, executives, and CEOs to sabotage our health and promote disease? Of course not. By and large, these people, just like the movie stars and the sports figures who endorse milk, are uninformed and blindly believe in their product. To them, the Got Milk and Milk Mustache advertising campaigns simply represent a logical corporate tactic to increase sales and maximize profits of a supposedly nutritious and healthful product.
As was the case with saturated fats, whether people should consume dairy products is divisive within the scientific community because the human experimental and epidemiological evidence is not necessarily conclusive and still can be interpreted in a variety of ways. Does milk prevent disease or does milk promote disease—or is the answer somewhere in between?
In an ideal world, this question could be decisively answered by well-controlled human experimental studies conducted during entire lifetimes. Unfortunately, these hypothetical lifelong experiments in real people will never be carried out because they would be impossible to control, incredibly expensive, and unethical. In lieu of these studies, conventional nutrition researchers are left with four scientific procedures to unravel the milk-drinking dilemma: (1) epidemiological studies, (2) animal studies, (3) tissue studies, and (4) short-term human experiments.
Unfortunately, traditional nutrition researchers are unaware of or don’t appreciate the most powerful research tool in all of biology. This concept could point them in the right direction when it comes to deciphering all of the conflicting information about dairy products and human health: the evolutionary template. Anybody who doesn’t use it might just as well do calculations with a pencil and paper, rather than with a computer. When the evolutionary template is combined with the four procedures scientists use to establish causality between diet and disease, we can make sense of all of the contradictory data and be sure of arriving at the correct answer.
George Santayana’s famous quote has influenced my thinking about life, as well as diet, for decades: “Those who cannot remember the past are condemned to repeat it.”
I am not the first scientist to recognize that milk and dairy consumption may have adverse effects on our health. One of the most vocal opponents to milk drinking was a physician, Frank Oski, M.D. (1932–1996), who was the department chairman of pediatrics at Johns Hopkins University from 1985 until 1996. He was a member of the National Academy of Sciences and the author or coauthor of three hundred academic papers and twenty books. A book he wrote in 1977, Don’t Drink Your Milk, was decades ahead of its time. Here is an excerpt:
The fact is: the drinking of cow milk has been linked to iron-deficiency anemia in infants and children; it has been named as the cause of cramps and diarrhea in much of the world’s population, and the cause of multiple forms of allergy as well; and the possibility has been raised that it may play a central role in the origins of atherosclerosis and heart attacks. . . . In no mammalian species, except for the human (and the domestic cat), is milk consumption continued after the weaning period [the period of breast-feeding]. Calves thrive on cow milk. Cow milk is for calves.
When you apply the evolutionary template to milk drinking, it becomes absolutely clear that cow’s milk was never intended to nourish another species—us—throughout our entire adult lives. It was specifically designed by natural selection to encourage rapid growth, support immune function, and prevent disease in young suckling animals. Newborn calves, like most mammals, are nearly helpless for the first few hours after birth. They are unable to stand up, much less sprint away from potential predators. For the first few days and weeks after birth, they can’t forage for food and are almost entirely dependent on their mothers’ milk for nourishment.
Milk is designed to make young animals grow rapidly and to prime their immune systems and prevent disease by allowing hormones and other substances in their mothers’ milk to enter their bloodstream. This is a brilliant evolutionary strategy to encourage survival for young suckling animals at the beginning of their lives, but it is a formula for disaster when adult humans consume a food intended only for the young of another species.
One of the telltale signs that there may be something wrong with milk drinking is that about 65 percent of all people on the planet can’t do it without experiencing gas, bloating, and digestive distress. Maybe we should be listening to our bodies.
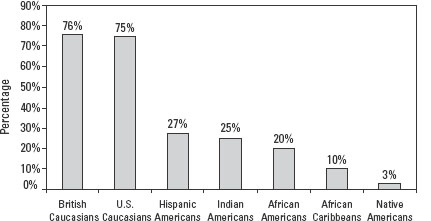
Milk is a mixture of carbohydrate, protein, and fat. Most of the carbohydrates in milk occur in the form of a sugar called lactose, which in turn is made up of two simple sugars: glucose and galactose. When we consume milk, ice cream, and other dairy products rich in lactose, it must first be broken down into these two simple sugars by an enzyme in our guts called lactase. About 65 percent of the world’s people haven’t inherited the genes to make lactase and are therefore lactose intolerant. The notable exceptions to this rule are people from Northern Europe and their descendants—because they maintain high gut lactase activity as adults, they can metabolize lactose into its two simple sugars and don’t experience gastrointestinal upset after drinking milk. In the following graph, you can see that the percentage of people with Northern European ancestry who can digest lactose without discomfort is much higher than almost all of the world’s other people.
The evolutionary explanation for the information in this illustration is simple. Most people on the planet can’t drink milk without gastrointestinal upset because their genes haven’t had enough time to adapt to this newcomer food. Milk is foreign fare that their bodies reject, as should we all, whether we can digest lactose or not. The lactose evidence is like a canary in a coal mine and hints at even greater health problems with milk and dairy consumption.
Ability to Digest Lactose
Dairy: A Nutritional Lightweight
Based on the dairy ad campaigns, cow’s milk appears to be nothing less than an extraordinary food to perk up our health and avoid illness. This milky white liquid served cold is touted as “good for everybody” and high in nine nutrients, including calcium and vitamin D.
If the truth be known, milk is a lousy source of vitamin D, as well as of the top thirteen nutrients most lacking in the U.S. diet, as shown in the following table. Let’s take a look at the facts.
In a paper published in the American Journal of Clinical Nutrition, my research group and I pointed out how dairy products were nutritional lightweights when compared to lean meats, seafood, fresh fruits, and vegetables. Based on the thirteen vitamins and minerals most lacking in the U.S. diet, our analysis showed that whole milk ended up near the bottom of the stack for all food groups.
| Nutrient | % of the U.S. Population Not Meeting 100% of the Daily Recommended Requirement |
| Zinc | 73.3% |
| Calcium | 65.1% |
| Magnesium | 61.6% |
| Vitamin A | 56.2% |
| Vitamin B6 | 53.6% |
| Iron | 39.1% |
| Vitamin C | 37.5% |
| Folate | 33.2% |
| Vitamin B1 | 30.2% |
| Vitamin B2 | 30.0% |
| Vitamin B3 | 25.9% |
| Protein | 20.5% |
| Vitamin B12 | 17.2% |
The highest sources of these thirteen nutrients are:
1. Fresh vegetables
2. Seafood
3. Lean meats
4. Fresh fruits
5. Whole milk
6. Whole grains
7. Nuts and seeds
To suggest that milk is a good source of vitamin D is a total stretch of the facts. In the last year, the official Institute of Medicine’s recommended intake for vitamin D has increased from 400 IU to 600 IU per day for most people. Although this advice represents a substantial increase, it still falls far short of human experimental evidence showing that at least 2,000 IU per day is required to keep blood levels of vitamin D at the ideal concentration of 30 ng/ml.
An 8-ounce glass of raw milk (280 calories) straight from the cow, without fortification, gives you a paltry 3.6 IU of vitamin D. At this rate, you’d have to drink 167 8-ounce glasses of milk just to achieve the 600 IU daily recommendation. Because most of the milk we drink is fortified with vitamin D, an 8-ounce glass typically yields 100 IU of this nutrient. Even with fortification, you would have to drink six 8-ounce glasses (1,680 calories or around 75 percent of your daily caloric intake) of milk to meet the daily requirement for vitamin D. If you wanted to reach the 2,000 IU level as suggested by the world’s best vitamin D researchers, you would have to drink twenty 8-ounce glasses of fortified milk, amounting to 5,600 calories. No one in his or her right mind would drink twenty glasses of milk a day, even if it was possible.
As you can see from these simple calculations, whether fortified or raw, milk is a very poor source of vitamin D. The best way to get your vitamin D is not by drinking milk, but rather by getting a little daily sun exposure as nature intended.
Milk, Ulcers, and Heart Disease
One of the more remarkable tales in recent medical history involves peptic ulcers. This is a chronic condition in which the linings of the stomach or the small intestine are eroded away, causing painful internal wounds. Complications include bleeding and perforation of the gastrointestinal tract, which are potentially life threatening.
For the better half of my adult life, peptic ulcers were routinely attributed to excessive stomach acid production caused mainly by stress, spicy foods, or too much gum chewing. Even as recently as the mid 1980s, ulcer patients were advised to take antacids, make lifestyle changes to reduce stress, cut back on spicy foods, and stop chewing gum. Yet this advice didn’t do much to alleviate symptoms or cure the problem.
One of the more unusual ideas that surfaced to treat peptic ulcers came from an early twentieth-century doctor, Betram Sippy, M.D. Dr. Sippy authored an influential paper that appeared in the Journal of the American Medical Association in 1915 suggesting that peptic ulcers could be effectively treated by feeding patients milk and cream on a regular basis throughout the day. The doctor’s advice became known as the Sippy Diet and was employed widely across the United States to care for patients with ulcers, even as recently as twenty-five to thirty years ago.
One of the downsides to the Sippy Diet, first recognized by Dr. Hartroft in 1960, was that it noticeably increased fatal heart attacks in ulcer patients. In Dr. Hartroft’s study, three groups were examined at autopsy: (1) subjects with peptic ulcers who followed the Sippy Diet, (2) subjects with peptic ulcers who didn’t follow the Sippy Diet, and (3) subjects without peptic ulcers. The fatal heart attack rate was similar between subjects without peptic ulcers and those with peptic ulcers who hadn’t been on the Sippy Diet; however, the fatal heart attack rate in ulcer patients who had adhered to the Sippy Diet was a staggering 42 percent. Close to half of all ulcer patients following the Sippy Diet had died of heart attacks! Thank goodness for us all that the medical community no longer recommends the Sippy Diet.
The reason that physicians no longer recommend the Sippy Diet or any other dietary regime for the treatment of ulcers is one of the most unlikely tales in modern medicine. For almost a hundred years, peptic ulcers were looked on as a disease of excessive stomach acid production caused by stress, spicy food—whatever. No one considered that this condition might be caused by an infectious organism until the publication of two revolutionary papers in 1983 and 1984 by two Australian scientists, Barry Marshall and Robin Warren, showing that 70 to 90 percent of peptic ulcers resulted from infection by the bacterium Helicobacter pylori. At first, these innovative publications were generally dismissed and discredited by the medical community. Yet it didn’t take long for practicing physicians to realize that ulcers could be effectively cured simply by giving their patients a good dose of antibiotics.
Unfortunately, it took about a decade for these brilliant scientists’ ideas to be accepted worldwide. Now, because of their groundbreaking insights, antibiotics are routinely used to successfully treat and cure almost all peptic ulcer cases. In 2005, Drs. Marshall and Warren were awarded the Nobel Prize in medicine for their discoveries.
The information about Sippy Diets and the risk of heart attacks has been buried in the scientific literature for nearly fifty years and is virtually lost to contemporary scientists. I would no longer necessarily hang my hat on fifty-year-old studies than I would drink a cup of milk, but the knowledge, wisdom, and insight of our parents’, grandparents’, and great-grandparents’ generations shouldn’t be swept under the rug. Is it possible that they were on to something?
Dairy and Heart Disease: Contemporary Studies
The data from the early 1960s studies on milk and heart attacks bears further scrutiny. As we move forward from the past, numerous studies support the view that milk and dairy products may not be heart healthy and good for everybody. A 1993 epidemiological study involving forty countries worldwide demonstrated that milk and its components—calcium, protein, and fat—had the highest relationship with cardiovascular death rates for any food or nutrient examined. Similar results implicating milk consumption as a cause for high mortality from heart disease were reported by Drs. Renaud and De Lorgeril in 1989, by Dr. Appleby in 1999, by Dr. Segall in 2002, and by Drs. Moss and Freed in 2003.
Milk isn’t simply a creamy white liquid that is good for everybody but rather is a complex mixture of many substances suspected of causing heart disease, including its high calcium content, saturated fats, lactose, and certain proteins. Because milk contains so many compounds that could potentially promote heart disease, it is difficult or impossible for epidemiological studies to sort out all of the facts. Let’s take a closer look at some specific elements in milk that may promote heart disease.
Most people know that milk and dairy products are one of our best sources of calcium. The dairy-manufacturing industry has pounded this message into our brains for decades—so much so, that many women fear they will develop osteoporosis if they don’t consume dairy foods. Until recently, the prevailing knowledge was that if a little calcium was good for us, then more certainly must be even better. Not necessarily so.
In 2002, I wrote a scientific paper covering this topic, and my analysis showed that modern-day Paleo diets provide us with only about 70 percent of the daily recommended calcium intake, no matter what we eat. Given this evolutionary clue, it is not surprising to find that the supra normal intake of calcium that can be achieved by milk and dairy consumption may cause unexpected health problems.
A 2010 meta analysis published in the British Journal of Medicine by Dr. Bolland from the University of Auckland confirmed the health hazards of too much calcium. His comprehensive analysis involving twenty-six separate studies and more than twenty-thousand participants revealed that calcium supplementation significantly increased the risk for heart attacks and sudden death. High blood levels of calcium from either supplementation or from excessive milk consumption are likely involved in atherosclerosis—the artery-clogging process—because too much calcium promotes the formation and fragility of the plaque that blocks our arteries.
High dietary calcium also tends to cause imbalances in magnesium, and this mineral is generally protective against heart disease for many reasons. In 1974, Dr. Varo pointed out in one study that high dietary calcium-to-magnesium ratios were a better predictor of heart disease than was high calcium intake alone. The bottom line is that if you get too much calcium and not enough magnesium in your diet, it put you at an increased risk for heart disease. Because milk’s calcium-to-magnesium ratio is quite high (about 12:1), the inclusion of dairy products in our diets can easily raise the overall calcium-to-magnesium ratio to about 5:1, thereby reducing cellular magnesium stores and promoting heart disease. Our studies of hunter-gatherers confirm that the dietary calcium-to-magnesium ratio was much lower—close to 2:1.
Supplementation studies of magnesium show that it reduces heart disease risk via multiple mechanisms. It improves our blood lipid profiles, prevents heartbeat irregularities called arrhythmias, improves insulin metabolism, and lowers markers of inflammation. When you consume dairy products, you effectively negate each of these therapeutic effects of magnesium, either fully or in part.
Let’s consider just a few other nutritional features in milk that further promote heart disease. In the 1950s and the early 1960s, when nutritional researchers were just beginning to understand how atherosclerosis and heart attacks developed, it was assumed to be a simple plumbing problem. Eat too much saturated fat and cholesterol, and your total blood cholesterol levels skyrocketed, clogging your arteries and thereby predisposing you to a heart attack or a stroke. Unfortunately, these simplistic views did not stand up well to the test of time, as hundreds of studies beginning in the 1990s showed that inflammation and immune reactions were just as important as or more important in the artery-clogging process than the consumption of either saturated fat or cholesterol.
What elements in the diet may be responsible for causing the chronic low-level inflammation that is now known to underlie not only heart disease, but also cancer and autoimmune diseases? The evolutionary template again brings us back to foods we never consumed in our ancestral past. Is there any possibility that these recent foods, such as milk and dairy, grains, and legumes, may cause chronic low-level inflammation and promote immune responses that lead to heart disease?
Milk is an amalgamation of nutrients, proteins, and hormones that have only recently been discovered and appreciated. It certainly is not the pure white liquid, high in calcium, vitamin D, and other vitamins and minerals, portrayed by milk manufacturers and their lobbyists. Milk is essentially nothing more than filtered cow’s blood. It contains almost all of the hormones, immunological factors, and body-altering proteins that are found in bovine blood.
Let’s not get too alarmed at this information; most of these compounds in milk have very short half-lives and are spontaneously degraded within minutes or hours after the manufacture of modern dairy foods, so they should not enter our bloodstream. Furthermore, a healthy human gut lining rarely allows intact large proteins such as those found in milk hormones to bypass its protective barrier.
So why should we worry? Are there proteins or hormones in cow’s milk that bypass the gut barrier and eventually get into our bloodstream to wreak havoc with our immune systems and promote atherosclerosis?
Although no smoking gun has yet been found that implicates milk in the pro-inflammatory and immune processes that underlie atherosclerosis, a suspect substance is well known. One of the more important cow’s milk proteins that may penetrate the gut barrier and get into our bloodstream is an enzyme in milk called xanthine oxidase. Numerous human studies show that our immune systems recognize this bovine enzyme as a foreign protein and produce antibodies to fight off this perceived foreign invader. Because we have a molecular duplicate of bovine xanthine oxidase located in the endothelial cells lining our arteries, it may also become a simultaneous target for the immune system’s attack and may promote atherosclerosis. Even though we don’t know for sure whether milk is involved in this process, there are no known health risks to not drinking milk, whereas the health benefits from abstaining might be enormous.
Milk, Insulin Resistance, and the Metabolic Syndrome
The glycemic index gauges how much a food raises our blood glucose concentrations. Processed foods such as white bread, candies, breakfast cereals, cookies, and potatoes have high glycemic indices because they cause rapid and marked increases in our blood glucose levels. These foods tend to promote the metabolic syndrome, a condition that includes diseases of insulin resistance such as type 2 diabetes, hypertension, cardiovascular disease, obesity, gout, and detrimental blood chemistry profiles. Natural foods such as lean meats, fish, eggs, fresh fruits, and nonstarchy veggies typically have moderate to low glycemic indices and are not associated with the metabolic syndrome.
Normally, when our blood-sugar levels soar after we consume high-glycemic-index carbohydrates, our blood insulin concentrations also rise. Shortly after the glycemic index was developed in the early 1980s, it was discovered that milk, yogurt, and most dairy foods had low glycemic responses. Presumably, these foods should be healthy and should help prevent the metabolic syndrome. About five to ten years ago, however, experiments from our laboratory and others unexpectedly revealed that low-glycemic dairy foods paradoxically caused huge rises in blood insulin levels. The table below shows that despite their low glycemic indices, dairy foods maintain high insulin responses similar to white bread.
This information posed a challenge to nutritional scientists. It was unclear whether milk’s insulin-stimulating effect but low glycemic response was healthful or harmful. To date, only one human study conducted by Dr. Hoppe in 2005 has addressed this question; it put twenty-four eight-year-old boys on either a high-milk or a high-meat diet for seven days. The high-milk diet worsened the boys’ insulin response almost 100 percent, and the entire group became insulin resistant in only a week’s time. In contrast, the high–meat eating group’s insulin levels did not change, and the boys’ overall insulin metabolism remained healthy.
The results of this experiment are alarming, particularly if future studies also demonstrate this effect in teenagers and adults. As insulin resistance is the fundamental metabolic defect underlying the metabolic syndrome, it would not be surprising to discover that drinking milk may cause other diseases of insulin resistance.
| Food | Glycemic Index | Insulin Index |
| White bread | 70 | 100 |
| Skim milk | 32 | 90 |
| Whole milk | 27 | 90 |
| Reduced-fat yogurt | 27 | 115 |
| Nonfat yogurt | 24 | 115 |
| Fermented milk (3% fat) | 11 | 90 |
Until 2002, the official party line of the mainstream dermatology community was that diet had nothing to do with acne. This viewpoint was expressed time and again in all of the major dermatology textbooks and became the doctrine taught to new dermatologists. If you didn’t know any better, you might think that this perspective was based on hundreds or even thousands of carefully controlled scientific studies.
When I first started to examine the link between diet and acne more than ten years ago, this is exactly what I had expected. How wrong I was! As it turned out, the dogma that diet didn’t cause acne was based solely on two poorly conceived experiments conducted in 1969 and 1971. In a series of papers from 2002 to 2006, I pointed out this flawed assumption to the dermatology community.
My research rekindled the entire diet/acne debate, but more important, we showed that acne was completely absent in two non-Westernized populations who didn’t drink milk or eat processed foods. We suspected that both milk and foods with high glycemic indices caused blood insulin levels to rise steeply and remain high all day long. In turn, elevated insulin levels set off a hormonal cascade that triggered the known cellular events that caused acne. My hypothesis that milk in part caused acne was verified by a series of recent epidemiological studies from scientists at the Harvard School of Public Health. Even more convincing was an experimental study carried out by Dr. Neil Mann in Australia showing that low-glycemic-index, high-protein diets improved acne symptoms.
I’m including in this book some of the many unsolicited e-mails I have received from patients whose acne symptoms were completely cured by the Paleo Diet.
Healing Adult Acne: Ray’s Story
I took antibiotics for twenty-five years to fight my acne. I also tried many changes to my diet but never saw results until I read and tried The Paleo Diet. For the last six weeks, I ate an almost entirely Paleo diet. In addition to my newfound energy, I am off my medication for the first time. I have found that if I eat any dairy (milk, cream, ice cream, or milk chocolate), it is only a matter of hours until I get pimples. It only took three or four days for me to realize that I didn’t need my medicine. It took another two weeks for me to start believing that it really worked.
I have not determined what it is exactly that causes the acne—milk, hormones, or the high glycemic load—but I know that if I eat Paleo, I don’t get acne. I will probably experiment to see if things like muffins and other grain-based foods have the same effect. But then again, I might not, because I don’t see any reason to eat those foods. Ice cream is another matter. I can stay off it most of the time, but I don’t think I am willing to say I won’t ever eat it again!
As it has been fewer than ten years since my study in the Archives of Dermatology revived the diet/acne debate, scientists worldwide have not completely worked out how milk drinking promotes acne. Some researchers share our view that milk’s exaggerated insulin response sets off a hormonal cascade that causes acne. Others suggest that hormones found in cow’s milk may be responsible, whereas some scientists believe that both mechanisms are involved.
Milk may be advertised as a squeaky-clean white liquid, high in vitamin D and calcium, but if the truth be known, it is filtered cow’s blood and as such contains almost all of the hormones and the bioactive peptides (protein building blocks) found in blood itself. Take a look at the following lists. You can see the incredible profusion of biologically active substances found in milk, even in these incomplete lists.
Growth Hormones Found in Milk
- Insulin
- Insulin-like growth factor 1 (IGF-1)
- Insulin-like growth factor 2 (IGF-2)
- Insulin-like growth factor binding proteins, 1 to 6 (IGFBP-1, 2, 3, 4, 5, 6)
- Betacellulin (BTC)
- Growth hormone (GH)
- Growth hormone releasing factor (GHRF)
- Transforming growth factor alpha (TGF α)
- Transforming growth factor beta 1 (TGF-β1)
- Transforming growth factor beta 2 (TGF-β2)
- Platelet-derived growth factor (PDGF)
Steroid Hormones Found in Milk
- Estrogens (estrone, estradiol-17β, estriol, and estrone sulfate)
- Progesterone
- 20 α-dihydropregnenolone
- 5α androstanedione
- 5 α pregnanedione
- 20α- and 20β-dihydroprogesterone
- 5α-pregnan-3β-ol-20-one
- 5α-androstene-3β17β-diol
- 5α-androstan-3β-ol-17-one
- Androstenedione
- Testosterone
- DHEA acyl ester
Bioactive Proteins and Peptides Found in Milk
- Relaxin
- Thyrotropin-releasing hormone (TRH)
- Luteinizing hormone-releasing hormone (LHRH)
- Somatostatin (SIH)
- Gastrin-releasing peptide (GRP)
- Calcitonin
- Adrenocorticotropic hormone (ACTH)
- Prolactin
- Thyroid-stimulating hormone (TSH)
- Lysozyme
- Lactoperoxidase
- Lactoferrin
- Transferrin
- Immunoglobulins (IgA, IgM, IgG)
- Proteose-peptone
- Glycomacropeptide
- Plasmin
- α Casein
- β Casein
- κ Casein
- α Lactoglobulin
- β Lactoglobulin
- Bovine serum albumen (BSA)
- Gastric inhibitory polypeptide (GIP)
- Glucagon-like peptide-1 (GLP-1)
- Antitrypsin, plasminogen activator inhibitor-1
- α(2) antiplasmin
- Butyrophilin
- Xanthine oxidase
- Mucin-1
- Mucin-15
- Adipohilin
- Fatty acid binding protein
- CD36
- Periodic acid Schiff 6/7
Bioactive Peptides Formed in the Human Gut from Milk Proteins
- Casomorphins
- α Lactorphin
- β Lactorphin
- Lactoferroxins
- Casoxins
- Casokinins
- Casoplatelins
- Immunopeptides
- Phosphopeptides
The trick for any of these elements to harm our health and well-being is for them to end up fully intact and present in our bloodstream. To accomplish this feat, these hormones, proteins, and peptides must first survive pasteurization (the quick heating of milk to destroy microorganisms), homogenization, and other processing procedures applied to dairy foods. Next, they must survive the digestion process and resist breakdown by our gut enzymes. Finally, they must cross the intestinal barrier, which normally blocks the entry of whole proteins, hormones, and large peptides into our bloodstream. It now seems quite probable that cow hormones in milk do indeed enter our bloodstream, particularly if we have a leaky gut—more about that later.
For a young suckling calf, it is a good thing for its mother’s hormones, peptides, and immune factors to cross the intestinal barrier. This process ensures that the calf will get a healthy start in life, grow rapidly, and develop resistance to disease. To ensure that mother’s hormones and peptides are not degraded in the calf’s gut by various enzymes, milk contains substances called protease inhibitors that prevent this breakdown. The downside of milk’s protease inhibitors is that they also prevent our own gut enzymes from destroying cow hormones and peptides.
Many hormones and bioactive peptides in milk do survive pasteurization and food processing. They also resist enzymatic breakdown in our guts because compounds in milk protect them. Ultimately, in order to adversely affect our health, these substances must bypass the gut barrier and enter our bloodstream.
It is apparent that this final hurdle is routinely overcome because so many people have allergies and immune reactions to milk. When intact hormones, proteins, or peptides cross the intestinal barrier, the immune system takes immediate steps to destroy any particle that is perceived as a foreign invader. Part of this process is to form antibodies against milk proteins, which later are involved in allergic and autoimmune reactions. Many of the proteins and the substances I have listed show up as specific milk allergens—meaning that they had to cross the gut barrier and interact with the immune system.
Of all of the milk hormones and the bioactive peptides listed previously, very few have been examined directly in human experiments. Nonetheless, evidence from animal, tissue, and epidemiological studies suggest that the consumption of milk and cow hormones at best may be unwise and at worst may be responsible for a number of life-threatening diseases. Let’s take a look at the most problematic of these hormones.
Bovine Insulin
The regular, everyday milk you buy at the supermarket is loaded with bovine insulin. This cow hormone not only survives your gut’s digestive enzymes, it seems to frequently cross the gut barrier and make its way into the bloodstream, as revealed by telltale signs from our immune systems. Because the structure of bovine insulin varies from the human form, if it enters circulation, it is immediately recognized as a foreign particle and flagged by the immune system. The large number of children who display immune system flags (antibodies) to bovine insulin means that it has indeed crossed the gut barrier intact and has caused an immune reaction. Although the mechanism is not entirely clear, the presence of bovine insulin antibodies in our bloodstream is associated with a greatly increased risk for type 1 diabetes.
Type 1 diabetes is an autoimmune disease in which the immune system destroys beta cells in the pancreas so that it can no longer make insulin. Type 1 diabetic patients must take insulin injections for the remainder of their lives. This devastating disease most frequently strikes children before their teen years. Epidemiological studies have time and again identified cow’s milk as a major risk factor for the disease, particularly if children are exposed to milk or milk-containing formula before the age of three. The bottom line: milk is a potentially lethal toxin for infants and young children.
Insulin-like Growth Factor 1
Another hormone found in milk that may have disastrous effects on our health and well-being is insulin-like growth factor 1 (IGF-1). As implied from its name, this hormone encourages growth. Unfortunately, it promotes growth not only in healthy tissues and organs but also in cancerous growths. Like all milk hormones, IGF-1 is a large protein molecule that normally should not breach the gut barrier and get into our bloodstream. Nevertheless, recent meta analyses of fifteen epidemiological studies and eight human dietary interventions by Dr. Qin have shown without a doubt that milk drinking robustly elevates IGF-1 in our bloodstream. This effect may result directly from the additional ingested bovine IGF-1 that crosses our gut barriers or via indirect mechanisms. Milk drinking causes our blood insulin levels to rise sharply, and whenever blood insulin concentrations increase, a series of connected hormonal events simultaneously cause IGF-1 to increase. During a twenty-four-hour period, blood insulin concentrations are a good marker for IGF-1 concentrations. When one increases, so does the other.
Whether IGF-1 in our blood is increased either directly from ingested bovine IGF-1 or indirectly from milk’s insulin-raising effects doesn’t really matter. The end result is the same—milk raises our total blood levels of IGF-1. This particular consequence of milk drinking is especially ominous because it encourages the growth of many types of cancer. Numerous worldwide meta analyses during the last forty years show that high blood levels of IGF-1 strongly increase the risk for prostate and breast cancer. If this outcome doesn’t alarm you, additional meta analyses will: these comprehensive studies show that milk drinking also increases the risk for ovarian cancer in women.
If you or any close relatives have a history of cancer, one of the best lifestyle changes you can make to reduce your risk of developing these life-threatening diseases is to wipe your upper lip clean of the milk mustache and get milk and dairy completely out of your life.
Estrogen
By now, you can see that milk isn’t simply an innocuous high-calcium food that builds strong bones, but rather is a concoction of body-altering hormones, enzymes, and proactive peptides whose wide-ranging effects promote cardiovascular disease, insulin resistance, cancers, allergies, and autoimmune diseases. Another dangerous cancer-promoting hormone in milk is the female hormone estrogen. Cow’s milk is chock full of it. It is present in bovine milk in a variety of forms, including estrone, estradiol-17β, estriol, estrone sulfate, and progesterone.
Modern dairy farmers maximize milk production from their cows. Dairy farmers are in the business to make money, and the more milk they can get from a single cow in a year, the more money they make. Female cows, like all mammals, produce milk only in the latter half of pregnancy and during the suckling period. The trick for modern dairy farmers is to get cows to make large amounts of milk during the early months of pregnancy when milk is normally not produced. Dairy farmers achieve this goal by artificially inseminating cows within three months after they have just given birth. In effect, these unfortunate cows become pregnant once again while they are still nursing the young of their previous birth. This totally contrived interference by humans causes the mother cow to produce milk 305 days out of the year. From an economic perspective, this strategy makes perfect sense—more milk means more money. From a dietary and health perspective, this practice is disastrous for us because it strikingly increases the estrogen content in the milk we drink.
The main form of estrogen in cow’s milk is estrone sulfate, which also happens to be the most frequently prescribed hormone replacement therapy for menopausal women. This pharmaceutical form of estrogen has high oral bioactivity—meaning that when you ingest it in pill form, it readily gets into your bloodstream. There is no reason to believe that estrone sulfate from cow’s milk acts any differently. So, whether you are a man, a woman, or a child, if you drink milk and eat other dairy products, your blood concentration of female hormones will be higher than if you don’t drink milk. This situation is not good.
For women, elevated blood estrogen and its metabolites increase your lifetime risk for developing breast and ovarian cancers. For men, milk’s added estrogen may increase your risk for getting prostate and testicular cancers.
Here are the eight most common food allergies in the U.S. population. These foods account for 90 percent of all food allergies. Notice that milk tops this list.
1. Milk
2. Eggs
3. Peanuts
4. Tree nuts
5. Fish
6. Shellfish
7. Soy
8. Wheat
Milk is also the most common childhood food allergy, where it afflicts from 2 to 3 percent of children between the ages of one and three. Symptoms include stomach pain, diarrhea, skin rashes, hives, wheezing, infantile colic, and anaphylactic shock, which can be life threatening. By age three, 85 to 90 percent of children grow out of their milk allergy. This change may appear to be a good thing, but the problem is that a childhood milk allergy predisposes children to other food allergies for the rest of their lives.
One study by Dr. Høst alarmingly revealed that 50 percent of all infants and young children who were allergic to milk later developed allergies to a wide variety of other foods before puberty. As was the case with type 1 diabetes, early exposure to milk proteins is the key to whether your child will develop allergies. The crucial period for restricting cow’s milk is from birth until at least age two or three.
One of the more interesting disorders related to milk allergy is infantile colic. When a healthy baby cries, screams, or fusses intensely for more than three hours a day, three days a week, it probably has colic. Continual infant crying is considerably more than just a parental annoyance. Crying and its associated exhaustion to parents and infants may lead to serious problems, including stress to your marriage, breast-feeding failure, and shaken baby syndrome, which frequently results in death.
Twenty-five to thirty years ago, it was still possible to purchase infant formula that was manufactured with cow’s milk proteins. Not so today, as it is almost universally recognized by pediatricians that infants should never consume milk or dairy products until at least age one or beyond. A series of human infant experiments carried out in the 1980s revealed that whey proteins in milk were largely responsible for colic. A powerful experiment by Drs. Lothe and Lindberg demonstrated that colic symptoms disappeared in 89 percent of all infants when they were given a cow’s milk–free diet.
You may ask why this information is relevant in 2011 when cow’s milk–based formula is no longer commercially available, and no pediatrician in his/her right mind would recommend giving cow’s milk to your infant. An often forgotten but important offshoot of these 1980s double-blind crossover experiments was that they were also repeated in milk-drinking mothers who breast-fed their infants. Not surprisingly, infants whose moms drank milk became colicky, which indicated that certain elements in cow’s milk may have caused an immunological response in the nursing mothers that was transferred to their milk, which in turn was transmitted to their babies, making them cry. Any food that causes such distress in infants should be a warning to us all. It may be possible that our babies are more in tune with their bodies than we are.
Asthma and Excessive Mucus Production
Too much milk consumption has long been associated with increased mucus production in the respiratory tract and the incidence of asthma. A few years back, I went to a high school cross-country meet and watched the young athletes cross the finish line. I noticed a few runners who were literally foaming at their mouths because they had so much mucus being produced from their respiratory system. I wondered whether milk drinking had anything to do with it, but at the time, the science hadn’t yet caught up with my observation and those of others. An intriguing 2010 hypothesis by Drs. Bartley and McGlashan from New Zealand may have found the answer.
In my list of all of the hormones and bioactive substances found in milk, you will notice under the category “Bioactive Peptides Formed in the Human Gut from Milk Proteins” (see page 92) a substance called casomorphins. These compounds are produced in our guts from the breakdown of the milk protein casein. One of these casomorphins, beta-casomorphin-7, directly stimulates mucus production from specific glands located in the gut. If the gut becomes leaky, which it invariably does on a typical Western diet, beta-casomorhin-7 can enter our bloodstream and travel to our chests, where it stimulates mucus production from MUC5AC glands located in our lungs and respiratory tracts. A final piece of this puzzle is that beta-casomorphin-7 is much more likely to trigger mucous production if the lungs and the respiratory tract are inflamed by asthma. Many people’s exercise-induced asthma symptoms disappear on the Paleo Diet.
Treating Asthma: Shannon’s Story
I’m a trainer, and I work with a very overweight woman, Jenny, who recently started my boot camp. She weighs 260 pounds at present. Until recently, she also suffered from exercise-induced asthma. For the first week of boot camp, she could not get through a class without her inhaler. Although I admired her dedication, it was painful and a bit scary to watch.
Then I put her on the Paleo Diet. This week, after doing this for a little less than two weeks, she no longer needs her inhaler. Miraculous!
Jenny’s also doing great on the diet—she’s not hungry at all, so I know the weight will be coming off soon as well.
Parkinson’s disease is a nervous system disorder that primarily affects areas of the brain that control movement. Disease symptoms include tremors, stiffness, and difficulty moving, and its two most famous victims are Muhammad Ali and Michael J. Fox. Although the cause of Parkinson’s disease isn’t known, both genetic and environmental elements seem to be involved. Like autoimmune diseases, it appears that environmental factors may be the most important triggers of this debilitating illness.
When we talk about environmental origins of any chronic disease with an unknown cause, diet is at the top of our list. The first items that we should examine are the foods that were not part of our ancestral human diet. This leads us once again to milk and dairy products.
A comprehensive 2007 meta analysis by researchers at the Harvard School of Public Health has identified a high intake of dairy foods as a prominent risk factor for Parkinson’s disease. Men who consumed the highest quantities of dairy products had an 80 percent greater risk of developing the disease than did men who ate the lowest amounts. These results are consistent with a study of Japanese men showing that people who consumed more than 16 ounces of milk daily had a 130 percent greater risk of Parkinson’s disease than non–milk drinkers. No one really knows how and why milk drinking increases the risk for this illness, but autoimmune mechanisms seem likely, particularly those directed at insulin. When you adopt the Paleo Diet, you will reduce your risk for developing Parkinson’s disease and other conditions with autoimmune components because this lifetime nutritional plan eliminates milk and all other foods that are suspected of causing autoimmune diseases.
Senile cataracts are cloudy opacities that form in the lenses of the eyes as people age and can ultimately cause blindness. The bad news is that if you live long enough, you will probably develop cataracts. The good news is that you can probably forestall their appearance until very late in life by following the Paleo Diet. For people between fifty-two and sixty-two years of age, 42 percent develop cataracts. This percentage increases to 60 percent between ages sixty-five and seventy-five and rises further to 91 percent for people between seventy-five and eighty-five years of age. In the United States and other Westernized countries, cataracts are treated by surgical removal, whereas left untreated they are the leading cause of blindness in older adults worldwide.
Milk drinking has a lot to do with cataract formation. Scientists routinely produce cataracts in rats, pigs, and guinea pigs even before they reach old age simply by feeding them high-milk and-lactose diets. As you recall, the main sugar in milk is lactose, which is broken down into its two constituent sugars, glucose and galactose, by the gut enzyme lactase. Numerous epidemiological studies show that lactose and galactose are involved in premature cataract formation. Due to the way cataracts form, we can probably never prevent them completely, but chances are good that if you adopt a dairy-free diet, you can live most of your life, even into old age, without developing cataracts.
Milk Impairs Iron and Zinc Absorption
As you saw earlier in the chapter in the list of the top thirteen missing nutrients in our diets, zinc is number one: more than 73 percent of all people in the United States don’t get enough of this essential mineral. Iron is number six, and about 40 percent of the population are deficient in this nutrient. Milk and dairy products are lousy sources of both iron and zinc, and the high concentration of calcium in cow’s milk strongly interferes with the absorption of both iron and zinc. If you were to add a slice of melted cheese to your burger, it would severely reduce the amount of iron and zinc you could absorb from the burger.
Both zinc and iron are crucial minerals for our health and well-being. Low iron stores are the most frequent cause of anemia, and in children and teens, low iron can impair mental functioning. Pregnant women with iron deficiency are at greater risk for delivering pre-term babies, and low iron may adversely affect athletic performance and work ability. The list of health problems associated with zinc deficiency includes low sperm counts, reduced libido, reduced immune function, increased susceptibility to upper respiratory infections, acne, white spots on fingernails, rough skin, lack of sexual development, stretch marks, macular degeneration, reduced collagen, and increased wrinkling. When you follow the Paleo Diet, you will be eating meat at almost every meal, and meat is a primary source of the most highly absorbable forms of both zinc and iron.
One of the biggest selling points the milk manufacturers would like us to believe is that by drinking lots of milk, we can reduce our risk of osteoporosis and future hip fractures. The foremost danger associated with osteoporosis is hip fracture in the elderly. Between 18 and 33 percent of all elderly people who suffer hip fractures die within a year after breaking their hips—not a pretty statistic. Although most people, including dairy lobbyists, believe that a low intake of calcium is a risk factor for hip and other bone fractures, the data says that’s not the case.
A 2007 meta analysis from the Harvard School of Public Health reported that high calcium intake had no therapeutic effect on hip fractures in 170,000 women and 68,000 men. In the same study, a pooled analysis of five human experimental trials showed no benefit of calcium supplementation on nonvertebrae fractures but, rather, showed that increased calcium intake actually increased the risk for hip fracture. A follow-up 2010 meta analysis specifically examining milk consumption and hip fracture risk in 195,000 women and 75,000 men also showed that low milk intakes didn’t increase fracture risk, nor did a high intake prevent it.
These studies show that we have been misled by the dairy manufacturers’ overhyped advertising and marketing campaigns. It’s clear that dairy doesn’t prevent bone fractures, and it might contribute to heart disease and cancer. I cannot come up with one single reason to drink milk or eat dairy products.
Paleo Bottom Line
Avoid dairy products.