Chapter 2
Eczema + diet: 60 years of research
Eczema is a unique skin disease with many factors associated with its appearance. The last 60 years of research offer some fascinating clues into how your diet (or the diet of your parents) can contribute to the appearance of eczema. While some aspects of eczema and genetic health cannot be explained, this chapter is devoted to the scientific research on how diet can affect eczema-related gene function and (most importantly) what you can do about it. Included in this chapter are eight factors associated with eczema (there are more factors discussed in Chapters 3, 6 and 8). If you are not keen on reading the scientific information presented in Chapter 2, you can skip these paragraphs, if desired, and focus on the Recommendations, which are listed in dot points in shaded boxes, and the Questionnaires, which can help you to identify problem areas in your diet and health.
• Genetic defects
Eczema is not contagious, so you can’t catch it from someone if you touch their skin, but chances are you inherited it from your parents. If you have one parent with eczema, you have a 20 per cent risk of developing eczema yourself. If both parents suffer from eczema, hay fever or asthma, your chances of developing it jumps to between 50 and 80 per cent. According to the research, eczema is regulated by approximately four or five major genes; some affect the immune system while others weaken the skin barrier.[1] For example, all genes come in pairs and some eczema sufferers can have one or two defective copies of the filaggrin genes (the protein that binds keratin fibres in the epithelial cells in human tissue).[2] Approximately 10 per cent of the British population have a single defective copy, so they suffer from dry, flaking skin.[3]
Genetics and dietary factors
Your diet affects your genetic health in a variety of ways. In the American Journal of Clinical Nutrition, Professor Loren Cordain and her colleagues say that our dietary changes, which began with the introduction of agriculture and animal farming about ten thousand years ago, may have occurred too recently for our human genetics to adapt.[4]
There are various problems with today’s diets, which include the following:
- The glycaemic load has increased. Processed foods usually have a higher glycaemic index (GI), which elevates blood glucose and insulin levels.
- We consume the wrong ratios of fats: our diets are low in omega-3 and rich in saturated fat, and processed vegetable oils and margarines cause the overconsumption of omega-6.
- We have fewer micronutrients in our diet. Processed foods often contain sugar and white flour, which are low in vitamins and minerals. Deficiency in just a single nutrient can cause genetic defects that can lead to the appearance of eczema.[5]
- Acid–alkaline balance has been altered. Western diets can cause low-grade metabolic acidosis that worsens with age.
- Sodium–potassium ratio has altered. There has been a 400 per cent increase in salt ingestion, while potassium-rich fruit and vegetable consumption has plummeted.
- Fibre content has decreased. Refined sugars, vegetable oils, alcohol and dairy products are devoid of fibre, and refined grains contain much less fibre than wholegrains.[6][7]
Over the last 200 years, food manufacturers have introduced highly processed foods containing artificial colours, preservatives, sweeteners and flavour enhancers. Our biological make-up hasn’t had enough time to become accustomed to this barrage of artificial additives.[8] According to the Food Intolerance Network in Australia, in 2009 there were 1154 food products containing problematic colour additives in Australia and in the United Kingdom there were more than 1000 products containing problematic food colourings that can worsen eczema symptoms and cause a range of side effects. And population studies confirm that acne and eczema are rare in traditional cultures where processed foods are not a regular part of the diet.[9][10]
Your genes can be modified by your diet
As mentioned in the introduction, American researchers claim that our dietary habits are the most important environmental factor modulating gene expression during one’s life span.’[11] According to German researchers, essential fatty acids in the diet can modify gene expression, T-cell function, cell membrane fluidity and cell signalling.[12] In experimental studies, dietary carotenoids modulate gene activity to protect against inflammatory damage and tumour growth.[13] And in one of the largest gene – diet interaction studies ever conducted, involving analysis of more than 27,000 people from five ethic groups (European, South Asian, Chinese, Latin American and Arab), the effect of diet on genetic health was confirmed yet again. Researchers reported that a healthy diet rich in raw vegetables and fruit modified the gene variants located on chromosome 9p21, which is the strongest marker for heart disease. A healthy diet significantly weakened this gene’s damaging effects.[14]
Your diet greatly affects your genetic health, and this chapter covers the research and the dietary ways to improve your genetic health and ultimately prevent eczema.
• Allergies
An allergy is an abnormal immune response triggered by a normally harmless substance. In eczema sufferers, allergic reactions can cause a worsening of eczema symptoms, coughing, sneezing, wheezing and, in severe instances, anaphylaxis (a difficulty in breathing caused by a life-threatening swelling of the tongue and/or throat). Allergic reactions can be measured as allergy sufferers have raised levels of immunoglobulin E (IgE), the antibody found in your blood and tissues that mediates allergy. Allergy tests include the skin prick test, measuring serum-specific IgE, and for children under the age of three there is a skin application food test. IgE-dependent, food-allergic reactions cause a sharp rise in the blood histamine level (this is a vital piece of information) and histamine toxicity occurs, which causes the negative symptoms you experience when you’re having an allergic reaction.[15][16][17] Histamine toxicity and diet solutions are covered shortly.
Common food allergies in eczema sufferers | Percentage with allergy |
|---|---|
| egg (hen’s) | 71 |
| peanut | 65 |
| dairy products, cow’s milk | 38 |
| other nuts | 34 |
| sesame seeds | 18 |
| wheat | 13 |
| soy | 4 |
Allergy tests are useful but keep in mind they only identify a limited number of possible food allergies and even if you’ve been allergy tested you may still be exposing yourself to foods you are sensitive to. Do the following questionnaire to see if you have food or environmental allergy symptoms.
Questionnaire 1: Allergy symptoms
Circle any symptom/s you experience on a regular basis, then circle the corresponding answer (YES/SOMETIMES/NO) that best describes the frequency of that symptom or collection of symptoms. YES = weekly or daily; SOMETIMES = monthly or occasionally; NO = never or rarely.
- itchy nose
- sneezing
- wheezing
- nasal drip
- blocked or ‘stuffy’ nose
- and/or a crease at the end of the nose from frequent rubbing/itching/wiping of drips
- hives
- skin rash
- itchy skin
- eczema
- facial flushing
- rosacea
- acne
- foul or abnormal body odour
- excess perspiration
- and/or swelling (lips, tongue, eyes, throat...)
Note: If you experience swelling, see your doctor or go to a hospital as you may be having an anaphylactic reaction.
- dark rings under the eyes (allergic shiners)
- puffy eyes
- itchy eyes
- conjunctivitis
- eye pain and/or
- temporary blurred vision
- low blood pressure
- high blood pressure
- heart palpitations
- and/or a quickened pulse after consuming a particular food
- muscle aches/pains
- joint pain
- and/or muscle weakness
- anxiety
- hyperactivity (ADD/ADHD)
- temporary confusion
- intense cravings (often for the food you are allergic to)
- mood changes after eating
- and/or sleep problems (excessive need for sleep or insomnia)
If you experience three or more allergy symptoms you could have undiagnosed allergies or food/chemical/environmental sensitivities. Other health factors may also be involved so if you have any concerns speak to your doctor for a formal diagnosis. In the meantime, keep a diet diary to help you identify what you ate preceding an attack (for a sample diet diary refer to ‘Diet diary’).
If you have an allergy are you stuck with it for life?
Over the past twenty years, researchers have found that of the 40 per cent of infants and young children with moderate to severe eczema and food allergy, most of their food allergies resolve in early childhood.[18] There is, however, an increased risk of ‘atopic march’, also known as the ‘allergic march’. The atopic march is associated with eczema in early childhood, where the form of allergic response changes over the years. For example, children under the age of three with eczema and allergies grow out of their allergies, then the more serious symptoms of asthma—wheezing and difficulty of breathing—develop. In the adolescent years, when asthma begins to subside, hay fever symptoms occur. Later in life at about the age of 40, just as allergic rhinitis is settling down, asthma and eczema return.[19] Research shows that antihistamine drugs, which are often prescribed to eczema sufferers, fail to prevent the atopic march.[20] The next section details how diet can alleviate allergy/histamine symptoms and reduce the risk of atopic march.
Recommendations
Eczema sufferers with allergies, especially those with life-threatening anaphylactic reactions, should continue to avoid the offending foods until given clearance by your doctor.
• Histamine toxicity
Your body not only makes histamine in response to an allergic reaction, your food also supplies histamines and other amines. According to several research papers, eczema sufferers have elevated histamine levels in the blood combined with a reduced capacity to detoxify these histamines.[21][22][23] And 36 per cent of eczema sufferers experience a worsening of eczema symptoms when they eat amine-rich foods.[24]
Symptoms of histamine toxicity are the same as an allergic reaction: a runny nose or nasal obstruction can be the first signs. Other symptoms include skin rash, a worsening of eczema symptoms, headaches, diarrhoea, stomach ache, colic, flatulence, sneezing, asthma and facial flushing.[25] Histamine toxicity occurs when the blood histamine level elevates beyond what the liver is capable of detoxifying. Therefore, the health of your liver is an important part of managing allergic reactions and eczema.
The next body of research gives us clues as to how to manage and prevent allergic reactions and reduce the risk of atopic march. In the body, diamine oxidase (DAO) is the main enzyme that breaks down histamine. Monoaminoxidase (MAO) also plays a role in histamine breakdown. According to German researchers, MAO and DAO activity are significantly decreased in patients with atopic eczema, compared with people without eczema.[26] According to research published in the American Journal of Clinical Nutrition, DAO activity can be blocked by the consumption of alcohol, food additives, nicotine and heavy metals such as mercury. MAO activity can be blocked by drugs, including some types of antidepressants.[27] Now this is where the research gets interesting: antihistamine medications, which are often prescribed to eczema sufferers, do not improve DAO activity (and antihistamine drugs suppress the liver’s ability to detoxify histamines). So while antihistamine drugs mask the symptoms when an allergic reaction occurs, they fail to treat the cause.
While antihistamine drugs can be useful in emergencies, there is a healthy alternative to the daily use of antihistamine drugs, and it comes packaged in the form of papaya. According to research published in the American Journal of Clinical Nutrition, vitamin C and vitamin B6 increase DAO activity and break down histamine.[28] Laboratory experiments show the flavonoid quercetin, which is present in onions and available as a supplement, also breaks down histamine.[29][30] (Refer to Table 4, ‘Nutrients for liver detoxification’, and Chapter 6, ‘Eczema supplements’.)
Recommendations
• Take natural antihistamines—vitamin C, vitamin B6 and quercetin—on a daily basis to reduce the risk of histamine toxicity and allergic reactions.
• Eat papaya, pawpaw and brussels sprouts, as they are rich in vitamin C.
• Gastrointestinal tract dysfunction
Like your skin barrier, your gastrointestinal tract is your ‘gut barrier’—a vital part of your body’s defence system against food-borne bacteria, toxins and allergenic substances.[31] According to Italian researchers, children with eczema often have abnormalities in the gastrointestinal tract, including increased intestinal permeability. A clinical trial revealed 44 per cent of children with atopic eczema have gastrointestinal symptoms after ingesting food (compared with 22 per cent of children without eczema).[32] The most common gastrointestinal symptoms in children with eczema are diarrhoea, regurgitation and vomiting. It’s interesting to note that gastrointestinal symptoms were, in most cases, reported to have been present before the appearance of eczema.[33] This research suggests that poor gastrointestinal health can contribute to the appearance of eczema.
According to research published in the Journal of Investigative Dermatology and The Lancet, eczema sufferers can have increased intestinal permeability, which allows larger food particles, pathogens and toxic substances to enter the body.[34][35] When microbes and toxins pass into your bloodstream, they can block or interfere with biochemical pathways and cause genetic mutations and allergic reactions.
Like a vicious cycle, intestinal permeability can also occur after you’ve had an allergic response to food. When a food allergy triggers histamine to be released from mast cells, inflammation and increased vascular permeability occurs. Research shows that the intestinal mucosal defect in eczema sufferers can also exist in eczema patients who don’t have food allergies.[36] The following table lists the factors that can cause gastrointestinal damage.
| alcohol consumption (also damages stomach lining)[37] | consumption of milk and other dairy products (can cause gastrointestinal bleeding in infants) |
| allergic reactions (histamine release) | frequent chilli consumption (stomach lining damage) |
| toxic bile | fungal infestation e.g. candidiasis, or parasite infestation |
| consumption of wheat | consumption of artificial additives (such as preservatives) |
| excess consumption of salicylates | taking aspirin or non-steroidal anti-inflammatory drugs (NSAIDs)[38] |
As you can see, your diet plays a major role in your gastrointestinal health. What happens when you ignore your diet and fail to protect the gut lining from damage? Intestinal permeability creates a heavy workload for the liver, which can lead to damaged liver cells (hepatocytes) and increased free radicals in the bile. In experimental studies, the antioxidant quercetin protects the stomach lining from alcohol-induced damage, if taken during or prior to exposure.[39] The liver is designed to detoxify substances, such as alcohol, and it makes bile to transport toxins to the colon for removal via the faeces. Your diet directly affects how adequately your body eliminates toxin-loaded bile from the colon. The liver produces up to 1 litre of bile salts every day and to do this it needs lecithin from your diet. Your body also needs plenty of dietary fibre to push chemical-loaded bile through the colon and to cleanse the colon of toxic substances, microbes and carcinogens (substances that can cause cancer).
Candida albicans infestation
Another gastrointestinal problem common in eczema sufferers is fungal infestation. Research shows that 70 per cent of patients with atopic eczema have candida albicans overgrowth in the gastrointestinal tract.[40] Furthermore, 69 per cent of infants with seborrhoeic eczema, which affects the scalp, are infected with candida albicans overgrowth at one or more external areas of the skin (including the inside of the mouth).[41] Researchers suggest this may be linked to the use of topical steroid creams (which is another reason why cortisone creams should only be used short-term, if at all). Overgrowth of pathogenic fungus, particularly Malassezia and candida albicans, can trigger skin inflammation and increase the incidence of atopic eczema.[42]
What exactly is candida albicans? Candida albicans is usually present in the digestive tract and it’s a harmless yeast while the immune system keeps it under control. If it proliferates, candida albicans can cause a visible skin infection and it can affect your gastrointestinal tract (infestation can be referred to as candidiasis, yeast infection or thrush). Candida albicans overgrowth triggers the production of IgE antibodies (remember how IgE is implicated in allergic reactions? See section entitled “Allergies”). According to research published in Clinical & Experimental Allergy, people with atopic eczema and candidiasis are exposed to continuous IgE antibodies, which worsens their eczema symptoms.[43] Unbalanced gut microflora and the proliferation of fungus often come before the development of eczema so it is important to treat candida infestation immediately.[44]
Questionnaire 2: Candida albicans
Circle any symptom/s you experience on a regular basis, then circle the corresponding answer (YES/SOMETIMES/NO) that best describes the frequency of that symptom or collection of symptoms. YES = weekly or daily; SOMETIMES = monthly or occasionally; NO = never or rarely.
- red, itchy skin
- tiny yellow pustules
- white patches on the skin that show improvement with anti-fungal treatment
- genital itching/burning
- white or chalky discharge or appearance
- stinging while urinating
[space left intentionally blank in the original book]
If you answered yes to any of the physical symptoms (questions 1 to 4) or if you have four or more YES or SOMETIMES answers to questions 5 to 17 then you could have a fungal overgrowth requiring medical treatment. When you have candida overgrowth, eczema symptoms cannot improve, even with a healthy diet, so it is essential to treat the fungal problem. Speak to a pharmacist or doctor about taking a powdered oral anti-fungal and a topical anti-fungal (one that is suitable for eczema). If you are sexually active, your partner should also take an oral anti-fungal (if he has signs of jock itch or if she has signs of thrush, he/she needs to apply a topical anti-fungal for fourteen days and avoid sex during this time). If you have repeatedly suffered from thrush, speak to your doctor about stronger anti-fungal treatments. After you have treated your fungal infection, the Eczema Diet is designed to minimise the risk of further infestations and if you have regular bouts of candidiasis you’ll also need to avoid sweet foods like muffins during the Eczema Diet, as fungus proliferates when sugar is in the diet. Also avoid common triggers such as alcohol and tea.
Anti-fungal foods
There are a range of foods that kill fungus in the gastrointestinal tract and these foods include garlic and the onion family, including eczema-safe leeks and spring onions (scallions).
Do you have worms?
Signs of worm infestation include:
• grinding your teeth at night
• itchy bottom, nose or ears
• children who regularly wet the bed
• frequent nose bleeds
• disturbed sleep (and/or itchy bottom at night)
If you or your child are experiencing signs of worm infestation then speak to your doctor or a pharmacist about oral worming treatments—they are simple, painless and pleasant tasting.
Tip: Remember to always wash your hands before eating to reduce the risk of worms.
Recommendations
• Take a suitable probiotic supplement (for probiotic information see section entitled “Probiotics”).
• Ensure you are consuming dietary fibre from pears, rolled oats (porridge, Omega Muesli), rice, linseeds, buckwheat and root vegetables, and eat two to three serves of eczema-safe grains daily (see section entitled “Eczema-safe grains”).
• Drink five to eight glasses of filtered water daily.
• Add garlic, spring onions (scallions), leeks, pawpaw and papaya to your diet.
• Take digestive enzymes, if required.
• Chew your food properly.
• Avoid sugar.
• Avoid milk and other dairy products.
• Avoid drinking alcohol while you have eczema; if you have a rare special occasion when you’d like to have a drink, choose eczema-safe varieties (listed on section entitled “Occasional treats”) and limit intake to two glasses per fortnight.
• Avoid wheat products for three months.
• If you have signs of intestinal permeability, the amino acid glutamine can help to heal the gut lining, along with probiotics, B-group vitamins, vitamin E and magnesium. Keep in mind that supplement therapy can fail if you continue to consume gut irritants.
• Abnormal fat metabolism
The fats you consume can affect your eczema, so it’s important to know a bit about the different types of fats in your diet. Essential fatty acids (EFAs) are polyunsaturated fats and include linoleic acid (commonly known as omega-6) and linolenic acid (which we call omega-3). In general, western diets are far too low in omega-3 and very high in omega-6, thanks to high intakes of margarine and vegetable oils. It’s been estimated that the present western diet has a ratio of omega-6 to omega-3 of 15:1 (instead of 1:1) and this increases the risk of inflammation.
In the 1930s researchers initially thought that omega-6 was deficient in eczema sufferers. However, research published in the 1980s confirmed the opposite: eczema sufferers tend to have elevated omega-6 in their blood and adipose tissue, in conjunction with a decrease in omega-6 metabolites such as DGLA (dihomogamma-linolenic acid).[45] When the milk of nursing mothers was tested, those with elevated levels of omega-6 and low levels of DGLA in their milk had children who later went on to develop eczema.[46]
What came first, the eczema or the fat abnormality? A large, carefully designed study by Italian researcher Galli and colleagues demonstrated that the elevated omega-6 and other EFA abnormalities appear before the eczema manifests.[47][48] This suggests that abnormal ratios of essential fatty acids in the diet and/or enzyme blockages caused by diet or stress could be involved in the appearance of eczema.
To promote proper functioning of the enzyme that converts omega-6 (via the FADS2 gene), consume the nutrients biotin, vitamin B6, magnesium and zinc. To promote the conversion of DGLA into skin-smoothing prostaglandins, reduce stress if necessary and avoid consuming trans fats, alcohol and limit high GI foods such as white bread. The mineral chromium helps to reduce high insulin levels after the consumption of carbohydrates.
What are trans fats?
Trans fats are partially or fully hydrogenated fats that act like saturated fats and block some enzyme reactions in the body. For good health, avoid trans fats (check product packaging for phrases like ‘trans fats’, ‘partially hydrogenated oil’ or ‘hydrogenated oil’). Trans fats are found in cheap vegetable cooking oils, canola oil, doughnuts, pastries, biscuits, Nutella®, chicken nuggets, some margarines, deep fried foods such as fried chicken and chips/French fries, imitation cheese, confectionery fats, pizza dough and many fast foods.
What are prostaglandins?
Prostaglandins are hormone-like substances that your body produces to moderate your hormones, your heart, your blood vessels, your cells and they can cause or prevent skin inflammation such as eczema. Prostaglandins are grouped into three families called Series 1, 2 and 3 prostaglandins. Which series a prostaglandin falls into depends on what type of fats you eat—omega-3, omega-6 or saturated fats. See Diagram 3, ‘How prostaglandins control inflammation’.
Recommendations
• To increase omega-3 intake, eat eczema-safe fish once or twice a week and eat linseeds/flaxseeds or use flaxseed oil five times a week.
• It is optional to take a fish oil supplement (EPA and DHA) if you are eating fish and linseeds.
• Reduce saturated fat intake—you can enjoy lean cuts of lamb, veal, turkey and chicken (cut the fat off meats and eat red meat no more than twice a week).
• Avoid trans fats, sausages, deli meats, beef, pork and roast crackling.
• Reduce stress, worry and anxiety, or seek counselling for ways to cope with stress, grief or trauma.
• Greatly reduce omega-6 in the diet (see ‘Margarine and vegetable oil’, below).
• Don’t bother taking an evening primrose oil supplement unless you find it significantly helps your skin (instead, focus on promoting DGLA conversion).
• Take a supplement containing biotin, vitamin B6, zinc and magnesium for delta-6-desaturase enzyme reactions (so the FADS2 gene is more likely to work).
• Take a supplement containing vitamin C and vitamin B3 for delta-5desaturase enzyme reactions (so the FADS1 gene is more likely to work).
• Take supplements containing quercetin and vitamin E, and eat garlic, leeks and spring onions (scallions). Ginger is allowed in Stage 2 of the diet but not Stage 1.
• Take a supplement containing chromium (see section entitled “Chromium”) and favour low GI foods to reduce insulin production and promote DGLA conversion.
• Margarine and vegetable oil
Margarines are made from vegetable oils and have been touted as a healthy alternative to butter, but research is emerging to suggest otherwise. According to a large cross-sectional study in Germany, families who predominantly use margarine (as opposed to butter) are more likely to have children with eczema.[49][50] And frequent consumption of vegetable oils, margarine or frying fats during the last four weeks of pregnancy increases the risk of having a child with eczema.[51] So are these products as healthy as they seem? If you have a look at the ingredient panel of most margarine tubs and refined vegetable oils, you’ll see they contain chemical additives such as preservative 202 and research shows food preservatives cause a worsening of eczema symptoms in more than 50 per cent of eczema sufferers.[52] Margarines usually contain artificial colours, which 40 per cent of you will react to, and antioxidants BHA/320 or 319, which can worsen symptoms in 21 per cent of eczema sufferers.[53] Furthermore, margarines and vegetable oils contain large quantities of omega-6. And despite the marketing hype about the health benefits of margarine and vegetable oils, the fact is the typical western diet is far too rich in omega-6. Our diets are virtually devoid of omega-3 (from seafood, wild/game meats, linseeds/flaxseeds and walnuts) and this disrupts essential fatty acid balance and may partly explain why margarines and vegetable oils increase the risk of eczema.
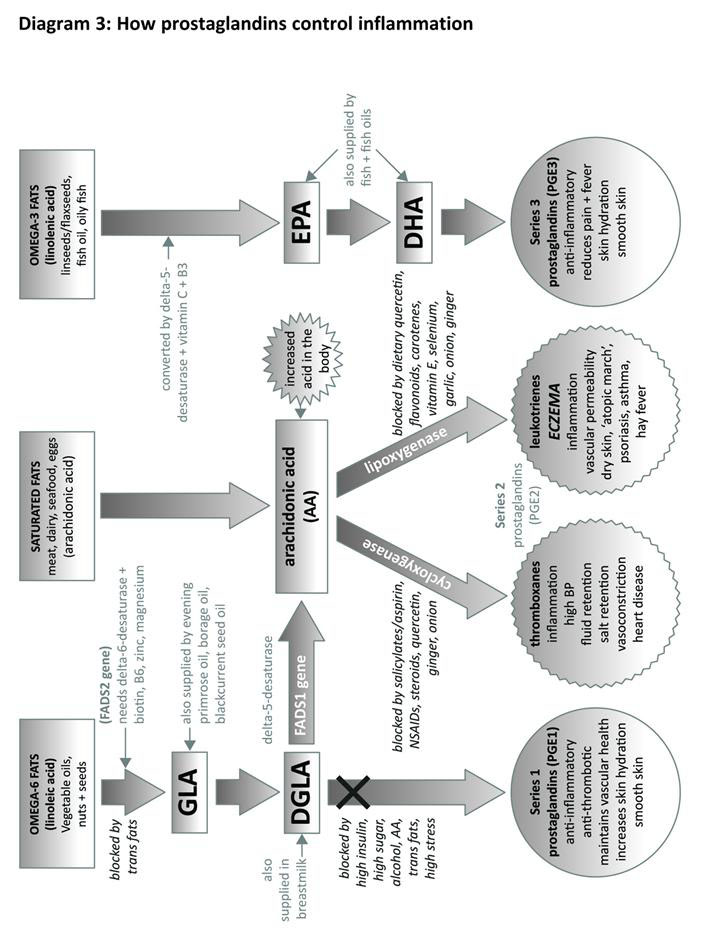
AA (arachidonic acid), DGLA (dihomo-gamma-linolenic acid), EPA (eicosapentaenoic acid), DHA (docosahexaenoic acid), GLA (gamma-linolenic acid), BP (blood pressure), X = blockage of this pathway can contribute to eczema.
Recommendations
• Avoid margarine and pastry or baked goods containing margarine.
• Avoid butter in Stage 1 of the Eczema Diet (pure butter is allowed in Stage 2 if you are not allergic to dairy products).
• Limit the amount and types of vegetable oils in the diet (refer to eczema-safe cooking oils).
• Chemical sensitivity
Chemical sensitivity is an adverse reaction which can occur within 3 hours or up to several days after coming into contact with the offending chemical. How do you know if you have a sensitivity to chemicals? Symptoms are varied and they can be mild to severe depending on the individual and include skin rashes, migraines, headaches, depression, irritability, unfocused behaviour, hyperactivity, flu-like symptoms and a worsening of eczema symptoms. In severe cases, some sensitivities can trigger strong feelings of anger, aggression, suicidal thoughts and physical pain.1
Your diet plays a major role in the appearance of chemical sensitivity, but first let’s look at the range of problematic chemicals, which includes natural chemicals such as salicylates, and artificial ones like preservatives, colourings and flavour enhancers.
Salicylates
Salicylates are chemicals found in many fruits and vegetables, herbs, nuts, teas, coffee, wine, beer and spices. Salicylates are also in many skin creams and perfumes. According to research by Loblay and Swain from the RPA Hospital Allergy Unit in Sydney, Australia, salicylate sensitivity is the most common chemical sensitivity in eczema sufferers and ingesting salicylate-rich foods can cause a worsening of eczema symptoms.[54] A high dose of salicylates (especially if taking aspirin, which contains salicylates) can cause temporary damage to the stomach lining, especially in children and sensitive individuals.
Salicylates are often touted as an eczema sufferer’s worst enemy, but are they to be permanently avoided? Maybe not. Salicylates are often found in the most nutritious foods such as dark leafy green vegetables and blueberries so you want to do all you can to prevent or decrease salicylate sensitivity. Here is the key: your liver is designed to detoxify salicylates and other chemicals so they can be safely removed from the body. In order for this to occur, your diet (or the maternal diet if your eczema-prone baby is being breastfed), needs to supply all the nutrients the liver requires for salicylate detoxification. These nutrients are glycine[55], vitamin B6 and magnesium.
Although it is not essential, you can test to see how well your liver is processing salicylates by using a liver function test home kit (where you take aspirin, so if you are allergic to aspirin this test is not suitable for you). See ‘Resources’, for more information. There is more information on salicylates and liver detoxification of chemicals coming up shortly.
Recommendations
• It’s essential for eczema sufferers to supplement with the correct doses of glycine, magnesium and vitamin B6 (see Chapter 6, ‘Eczema supplements’).
• Greatly reduce salicylate intake (some healthy salicylate foods are essential in the diet and these include carrots, sweet potato and fresh beetroot as they supply carotenoids for skin protection).
• Avoid aspirin* and baby teething gels as they are rich in salicylates (for alternatives to teething gel refer to section entitled “Teething gel”). (*If you have been prescribed aspirin for heart disease, do not stop taking aspirin, and talk to your doctor about your options. Do not take glycine if you are on blood thinning medications such as aspirin.)
Nitrates
Nitrates are chemicals used to preserve meats such as bacon, sausages and ham. In the 1970s it was discovered that during the cooking of nitrate-containing meats, harmful nitrosamines form which can cause cancer and liver damage.[56][57][58] It is for this reason government health authorities in Australia recommend we don’t eat deli meats or sausages. Carcinogenic nitrosamines are present in tobacco smoke and in the nettings wrapped around deli meats such as ham, which can contaminate the meat.[59][60] According to research by Loblay and Swain, eczema sufferers are sensitive to nitrates and nitrate consumption can worsen eczema symptoms in 43 per cent of eczema sufferers.[61]
Your diet can help to reduce the damaging effects of nitrates. According to laboratory studies, the antioxidants quercetin, vitamin C and vitamin E help to reverse the liver damage caused by nitrate consumption.[62][63][64]
Recommendations
• Avoid nitrate-containing meats as they increase cancer risk and eczema symptoms.
• Ensure your diet contains the antioxidants quercetin, vitamin C and vitamin E (see Chapter 6, ‘Eczema supplements’).
Food colourings
If you’ve ever eaten food at a children’s party, chances are you have ingested dozens of artificial food colourings known to exacerbate eczema. And it’s not just brightly coloured party food, either. Regular breakfast cereal, yoghurt and margarines contain colourings that can trigger a range of adverse reactions, including a worsening of eczema symptoms.[65]
Tartrazine (102), one of several yellow food colourings, worsens eczema symptoms in 40 per cent of eczema sufferers and it can trigger asthma attacks, runny nose, purplish skin bruising and in severe cases anaphylactic shock. How can eating a yellow lolly cause such problems? Tartrazine stimulates the production of pro-inflammatory leukotrienes. A team of researchers at Southampton University in the United Kingdom also found that artificial colourings could hamper a child’s intelligence by up to five IQ points and cause behavioural problems such as inattention and hyperactivity.[66]
Artificial colourings are not the only additives eczema sufferers should avoid. There is a natural food colouring that is problematic for eczema-prone people and most children are consuming it on a daily basis. Annatto (160b), used to colour many brands of butter, yoghurt and fish fingers to name a few, can cause eczema flare-ups in sensitive individuals. Adverse reactions to annatto include obsessive head banging, irritable bowel syndrome, headaches, learning difficulties and (surprisingly) some children may obsessively favour yellow: for example, they only want yellow food/pencils/clothes, which ceases when annatto is removed from the diet.[67] In Europe, annatto has been banned from use in foods and a safe alternative, beta-carotene (160a), is used. A range of problematic colourants are listed in ‘Additives to avoid’.
Additive | Number/s | Food sources |
|---|---|---|
| flavour enhancers: glutamates, monosodium glutamate (MSG) | 620–635 | flavoured noodles, chicken-salted chips, flavoured crackers and crisps, sauces, stock cubes, gravies, fast foods, traditional Chinese cooking (natural sources of MSG include tomato, soy sauce, broccoli, mushrooms, spinach, grapes, plums, deli meats, miso, tempeh, wine, rum, sherry, brandy, liqueur) |
| artificial colourings: tartrazine (yellow), red, blue, green, black, brown | 102, 104, 107, 110, 122–129, 132, 133, 142, 151, 155 | confectionery/lollies/candy, jelly, breakfast cereals, glacé cherries, salmon, hot dogs, soft drinks, flavoured mineral water, chocolate, potato crisps, corn chips, toppings, ice-cream, iceblocks (popsicles/ice lollies), fruit drinks, cordials, flavoured milks, meat pies, cupcakes, cakes, liqueur, yoghurt and dairy snacks |
| (US: blue 1 and 2, green 3, red 2, 3, 4 and 40, yellow 5 and 6) | ||
| natural colouring | 160b (annatto) | in many yoghurts, butter, fish fingers, custard and commercial desserts (160a is a safe alternative) |
| preservatives | sorbates 200–203 | used in some processed fruits and vegetables, wines, beer, most soft drinks (sodas), diet drinks, cordials, juices, processed meats, sausages, dried fruit, processed deli meats (e.g. sausages, devon, ham, salami); 282 in some breads, buns and wraps |
| benzoates 210–213 | ||
| sulfites 220–228 | ||
| nitrates, nitrites 249–252 | ||
| propionates 280–283 | ||
| antioxidant preservatives | 310–321 | in oils, margarines, chips, fried snack foods, fast foods |
| artificial sweeteners: aspartame, saccharin | 951, 954 | NutraSweet®, Equal®, Sweet N’Low®, diet and ‘sugar-free’ products, diet soft drinks (sodas), ‘zero’ soft drinks, cakes, cookies, sweet pies, muffins, ice-creams |
[Sources: McCann, D. et al., 2007, ‘Food additives and hyperactive behaviour in 3-year-old and 8/9-year-old children in the community: a randomised, double-blinded, placebo-controlled trial’, The Lancet, vol.370, pp.1560–7; Dengate, S., Food Intolerance Network fact sheet, retrieved 12 May 2011: www.fedupwithfoodadditives.com]
Recommendations
• Avoid artificial chemicals, especially food colourings, preservatives and flavour enhancers.
• Avoid natural colour annatto (160b).
• Refer to the handy shopping guides in Part 3 for a list of additives to avoid when you are grocery shopping (Eczema-safe shopping guide: Stage 1).
Brewer’s yeast
Approximately 31 per cent of eczema sufferers have a worsening of eczema symptoms after consuming brewer’s yeast.[68] Brewer’s yeast is a fungal micro-organism used to ferment carbohydrates in beer and it is available as a nutrition supplement.
Sulfites
Sulfites, such as sulphur dioxide, are food preservatives which are commonly used to preserve wines, deli meats, dried fruits and dried vegetables, to name a few. Sulfites destroy vitamin B1 and folic acid in foods so they can be considered an ‘anti-nutrient’ (anti-nutrients are discussed in section entitled “Reduce anti-nutrients”). While dried fruits might be touted as a healthy snack for children, one dried apricot can contain 16mg of sulphur dioxide which can cause a worsening of eczema symptoms in susceptible individuals and/or a range of adverse reactions such as diarrhoea, unfocused behaviour, hyperactivity, smelly gas and it could trigger an asthma attack in susceptible individuals.[69]
If you’ve ever experienced facial flushing after drinking a glass of red wine or consuming vinegar you may be sensitive to sulfites, and highly sensitive people may react to sulphur-rich garlic and onions.
Monosodium glutamate (MSG)
A study conducted by Loblay and Swain found that 35 per cent of eczema sufferers have adverse reactions to monosodium glutamate, a flavour enhancer that is both natural (present in tomato) and artificial (in products such as flavoured potato chips). Dietary MSG can not only worsen eczema symptoms, it may increase the risk of premature wrinkles because it reduces stores of glutathione, an anti-ageing antioxidant enzyme needed for liver detoxification of chemicals.[70] In animal studies, MSG ingestion promotes liver inflammation, which significantly increases the size of the liver and promotes liver damage.[71]
Can modifying your diet make up for previous dietary sins? Clinical studies show MSG-induced liver damage can be reversed with antioxidant supplementation.[72]
Reduce your chemical load
Consuming soy sauce, fermented soybeans, chocolate, cheese, coffee and yoghurt causes a worsening of eczema symptoms, according to a Japanese study published in the Journal of Dermatology. After the avoidance of these foods for three months all the participating eczema sufferers had reduced eczema symptoms.[73]
Recommendations
• Avoid consuming artificial additives in your diet.
• Wash fruits and vegetables in water, soaking them for several minutes. Use a soft scrubbing brush on hardy fruits and vegetables and peel the skin where possible.
• For more information on avoiding chemicals, read Chapter 8, ‘General recommendations for eczema’.
• Additives to avoid are listed in the handy shopping guides.
• While you have eczema, avoid natural MSG sources such as soy sauce, tomato and grapes (for a list of foods containing MSG refer to ‘Additives to avoid’).
• Avoid artificial MSG and other flavour enhancers.
• Avoid sulfite-rich foods and drinks, including dried fruits and alcohol (sulfite-rich foods are listed in Table 3, ‘Additives to avoid’).
• Supplement with the antioxidants vitamin C, vitamin E and alpha-lipoic acid (supplement details are in Chapter 6).
• Lactose + dairy products
Lactose is the sugar portion of dairy products such as cow’s milk, yoghurt, butter and cheese. In order for your body to break down lactose, you require the enzyme lactase in your digestive tract. If you are sensitive to dairy products it is likely that your body does not adequately produce this enzyme. Lactose intolerance can cause diarrhoea, gas, cramps and bloating. More than 40 per cent of eczema sufferers are sensitive to lactose and they experience a worsening of eczema symptoms when they consume lactose.[74]
It’s not only lactose intolerance that can occur. A total of 38 per cent of eczema sufferers are allergic to cow’s milk and dairy products.[75] Aside from diagnosed allergies, dairy products can cause damage to the lining of the gastrointestinal tract. Research shows the consumption of cow’s milk causes gastrointestinal bleeding in 50 per cent of American infants who present with iron deficiency (frequent milk consumption can also cause iron-deficiency anaemia). When the gut lining is damaged from eating dairy products, tiny holes allow larger food particles to enter the body and allergic reactions can result. Naturopaths often refer to this as leakygut syndrome and the medical term is increased intestinal permeability. A dairy-free diet is one of the most effective ways to decrease the appearance of eczema, even when dairy allergy or lactose intolerance is not present.
Recommendations
• Avoid all dairy products while you have eczema and refer to the calcium information in section entitled “Calcium”.
Questionnaire 3: Eczema + diet
The following questionnaire is suitable for adults and children with eczema, and if you have a baby with eczema you can use this questionnaire to assess maternal diet (the diet of the mother during pregnancy and/or the diet of both parents before conception).
Circle the foods you consume and then circle the corresponding answer (YES/SOMETIMES/NO) that best describes the frequency of consumption. YES = weekly or daily; SOMETIMES = monthly or occasionally; NO = never.
Part 1. Do you...
- eat raw egg or raw egg whites?
- have whole-egg mayonnaise in your fridge?
- eat mayonnaise, coleslaw or creamy salad dressings?
- drink protein shakes containing powdered/fresh egg or egg whites?
- eat hollandaise sauce or eggs Benedict?
- eat the icing on traditional wedding cakes?
- have mood disturbances such as depression, moodiness or anxiety?
- eat traditional chocolate mousse? (store-bought varieties may not contain egg but they have lots of artificial additives)
- have dermatitis plus any of the following symptoms: greyish pallor of the skin, scaly lips, nausea, loss of appetite, muscle pain, raised cholesterol or localised numbness?
- eat store-bought dips containing egg (e.g. baba ganoush/tuna/beetroot)? (not including hummus, tahini or pesto-type dips)
Part 2. Do you...
- use margarine?
- consume store-bought pastry or softened butter (containing vegetable oil and additives)?
- use canola oil, plain vegetable oil, olive oil or ‘light’ cooking oil?
- eat fried foods (e.g. takeaway/takeout foods cooked in oil, or fish and chips)?
Part 3. Do you...
- eat a lot of fruit? (3 pieces/1 1/2 cups or more per day)
- frequently eat broad beans, broccoli, cauliflower, eggplant (aubergine), gherkins, olives, mushrooms, silver beet or spinach?
- frequently eat tomato, oranges, lemon, kiwi fruit or strawberries?
- drink tea, herbal tea or coffee?
- drink tomato juice, flavoured soft drink/sodas or cordial?
- drink beer, wine, cider, brandy, liqueur, port, rum or sherry?
- eat cornflakes or consume corn products?
- have adverse reactions to aspirin?
- use teething gel (babies and toddlers)
Part 4. Do you...
- eat grapes, plums, prunes, raisins, sultanas, tomato and/or tomato products such as sauces and juice?
- eat broccoli, mushrooms, silver beet or spinach?
- eat deli meats such as devon, turkey, chicken, salami and sausages?
- consume gravy, soy sauce, flavoured potato chips/crisps or flavoured rice crackers?
- drink wine, brandy, liqueur, port, rum or sherry?
Part 5. Do you...
- chew gum or use mouth wash?
- consume flavoured potato chips/crisps, diet soft drink/soda, cordial, flavoured rice crackers, coloured iceblocks/popsicles/ice lollies, flavoured corn chips or sweets?
Analysis of Questionnaire 3
Let’s take a look at the results of Questionnaire 3 to identify where you might need to alter your diet.
Part 1: egg white injury
Assess your total intake of raw egg whites. If you consume whole-egg mayonnaise once a week, tuna dip once a week and hollandaise sauce once a week, this is classified as frequent consumption of raw egg white and egg white injury may result. Egg white injury and biotin information is in section entitled “Biotin”.
Part 2: vegetable oil
If you consume margarine, products containing margarine, or vegetable oils, discontinue use and refer to the rice bran oil information in section entitled “Cooking oil: rice bran oil”.
Part 3: salicylates
This section highlights foods and drinks rich in salicylates. Do not consume these products while on the Eczema Diet as doing so may affect your results (if you have been prescribed aspirin for heart disease do not stop taking aspirin, and talk to your doctor about your options).
Part 4: MSG and flavour enhancers
This section highlights foods and drinks rich in natural MSG and foods containing artificial flavour enhancers. Do not consume these products while on the Eczema Diet as doing so may affect your results.
Part 5: artificial chemicals (general)
Do not consume these products while on the Eczema Diet.