Chapter 2
Understanding How Food Can Be Your Body’s Enemy
IN THIS CHAPTER
 Identifying links between food and inflammation
Identifying links between food and inflammation
 Knowing the difference between allergy, sensitivity, and intolerance
Knowing the difference between allergy, sensitivity, and intolerance
 Living with allergies and sensitivities
Living with allergies and sensitivities
The first obstacle to get over when making a change to an anti-inflammatory diet is realizing that yes, some foods really are your enemy. Not all food is working against you, of course. But much of the food you consider safe, the foods that you may be eating regularly, may show up on your new do-not-eat list. After you identify your food allergies, sensitivities, and intolerances, keep them in mind as you select recipes and ingredients in later chapters.
Researchers have been working for years to determine how certain types of foods react with the human body and stir up inflammatory responses. It’s no secret that fried foods, foods high in processed saturated fat, and those high in sugar are bad for you. What is surprising to many people, however, is the discovery that many of the foods that seem safe can really be hazardous to one’s health, leading to sensitivities or allergies or even contributing to cancer, heart disease, or diabetes.
Defining Toxic Foods
Food, by definition, is “any nutritious substance that people eat or drink … in order to maintain life or growth.” When you eat food, it becomes energy for your body through the process of digestion. The foods and drinks you take in aren’t in a form that your bodies can use just yet; the food has to be transformed into much smaller pieces, nutrient-filled molecules, which can be absorbed by your blood and carried throughout the body. Digestion starts in the mouth as you chew food into smaller pieces; then it continues through the body with the help of digestive fluids until it’s broken down as far as possible. Most of these molecules are absorbed into the small intestine and eventually become energy for various parts of the body.
Sometimes, however, that same food you turn to for nutrition and sustenance can turn on you. Foods that are seemingly harmless can be toxic, leading to inflammation and serving as triggers for chronic illnesses such as diabetes, cancer, arthritis, and heart disease.
We define toxic foods as any foods that are harmful to the body to any degree and can lead to inflammation and chronic disease. For some people, the nightshade family of fruits and vegetables — tomatoes, potatoes, peppers, eggplant — can be toxic in that they contain alkaloids, which can affect muscle function. Dairy products or wheat products can cause digestion problems for some people, and refined sugars can promote diabetes, obesity, and hypertension.
You can put toxic foods into three categories:
- Foods that increase inflammation in everyone, such as trans fats, refined sugars, and artificial foods
- Foods that are toxic to some individuals and not to others, such as wheat, corn, and dairy
- Foods that contain chemicals, toxins, and other harmful substances that cause inflammation and endocrine changes in the body; they may accumulate in the fat cells and liver and can be associated with cancer
- Refined sugars:
- Cookies, doughnuts, pastries
- Prepared salad dressings and condiments
- White bread
- Pasta
- Flavored oatmeal or cereal
- Soda and fruit punch
- Cereal bars
- Trans fats:
- French fries
- Margarine
- Packaged baked goods
- Potato and corn chips
- Fried foods
- Creamy salad dressings and condiments
- Bleached or enriched flour:
- Bread
- Crackers
- Cereal
- Cookies
- Pasta
- Pancakes and waffles
Looking at Allergies and Specific Sensitivities
For many people, creating a menu isn’t as simple as going with whatever they like to eat. People who have food allergies, sensitivities, or intolerances have to avoid foods and food products that many people take for granted.
- Food allergies are caused by an overreaction of the immune system toward a food or drink. Allergic reactions tend to show up almost immediately, from a rash or watery eyes to a more serious anaphylactic reaction that could be fatal.
- Food sensitivities appear in the form of a more delayed, sometimes chronic onset of symptoms, such as fatigue or even nasal congestion days after consumption. Food sensitivities are often caused by nutrient deficiencies or eating or drinking the food too often.
- Food intolerance is an adverse reaction to a food because something necessary for digestion is missing. For example, if your body is missing lactase, the enzyme needed to break down lactose, you’re likely intolerant of milk and dairy products.
It can sometimes be difficult to distinguish between a hypersensitivity and an allergy to a food, as seen in Figure 2-1. Many of the same symptoms may appear with both hypersensitivity and allergies, but the chronic effects may differ. Consult a health care professional to determine if you have food allergies, sensitivities, or intolerances.
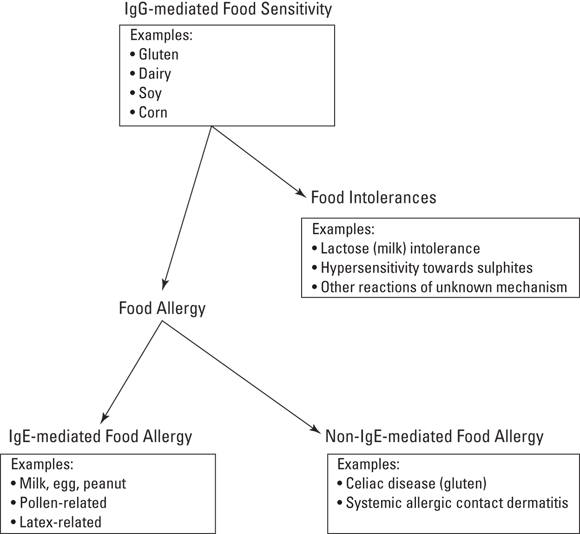
© John Wiley & Sons, Inc.
FIGURE 2-1: How food can be toxic to your body.
In this section, we take a look at various allergies, sensitivities, and intolerances; note some foods that commonly cause problems; and discuss how those food reactions can lead to chronic inflammation.
Understanding food allergies and sensitivities
Food allergies and sensitivities aren’t all that uncommon. In fact, you may have an allergy and not even realize it. Allergies of all kinds occur when a body’s immune system kicks in, attacking the irritant that it views as an invader.
Most of the time, your body doesn’t attack the food you eat because of food tolerance, which is regulated by the immune system and your gastrointestinal tract. But as you age and practice more inflammatory habits, you can develop intolerances, sensitivities, or even life-threatening allergies to specific foods. Your immune system starts attacking either because too much of a particular component of that food is present or because there’s something wrong with the way that food affects your body due to your genetic predisposition.
After the body first identifies — or rather, misidentifies — a particular food particle as an invader, the body starts mass-producing antibodies. When you eat something you’re allergic to, antibodies lock onto an antigen (the offending food particle) and trigger an inflammatory response. In most cases, the inflammation quiets down again; however, if you have a genetic predisposition to food allergies, high levels of toxicity, digestive system imbalances, or a weakened immune system, this normal immune response can kick into high gear and wreak inflammatory havoc in your body in varying degrees.
Think of a bee sting. Everyone has some level of irritation or sensitivity to the stinger, even if it’s not a full allergy. When the bee stings you, there’s a small red bump where your antibodies immediately attack the area and work to protect the rest of the body. The same thing happens with food allergies and sensitivities, only the inflammation comes in the form of arthritis, irritable bowel syndrome, or other issues.
Food allergies can be lethal. Some people must avoid not only the product itself but also anything that may contain that product in its ingredients list. People allergic to peanuts, for example, have to avoid anything made with peanut oil. In extreme cases, people must even avoid foods that have come into contact with their allergen.
Addressing lactose intolerance
Most people have some degree of sensitivity to dairy, although the majority don’t even realize it. About 65 percent of people worldwide suffer from lactose intolerance, the inability to digest lactose, which is the main sugar found in milk. Your genes influence your ability to break down lactose, with as much as 90 percent of some of the world’s ethnic groups not able to digest milk beyond infancy.
To be digested properly, the sugar lactose must be split into the smaller pieces glucose and galactose. When the lactase enzyme is either absent or inactive in the body, you can’t break down lactose, and you have lactose intolerance. The body produces less lactase as you age, and in Asian, Native American, and African American populations, lactase production drops anywhere from 70 to 100 percent from childhood.
That’s not to say everyone with a lactase deficiency is lactose intolerant; many people may go years without having any symptoms, or there may be just certain dairy products that trigger symptoms while others don’t have any affect at all. But whenever you eat or drink something your body doesn’t like, it sends out warning signals, usually in some form of inflammation. The most common symptoms of dairy sensitivity are gastrointestinal issues, but other symptoms with a potential relationship to dairy include
- Abnormal cravings for sweets
- Achy joints and muscles
- Acne
- Anxiety
- Bags under the eyes
- Chest congestion
- Chronic fatigue
- Dizziness or faintness
- Excessive sweating
- Headaches
- Mood swings
- Ulcers
Symptoms generally appear anywhere from 20 minutes to two hours after eating or drinking dairy products. Consume too much dairy, and symptoms can worsen, leading to abdominal distention and diarrhea as well as many other stomach problems.
If you suspect you may have lactose intolerance because you’re experiencing any of the symptoms listed, look for the word “lactose” listed in the ingredients of some of your favorite foods — even those you may not think have any dairy. Be sure to get a proper diagnosis so you can rule out any other conditions that may be present.
Confronting sugar and caffeine sensitivity
Refined sugar — which has been processed and stripped of all its natural nutrients — is bad for everyone. Unfortunately, that’s also the type of sugar that’s found in almost everything you eat. Refined sugar is much too easy to digest, so it quickly enters the bloodstream and raises blood sugar levels, increasing your risk of diabetes. Eat too much sugar, and you quickly see some symptoms of a suppressed immune system: fatigue, joint pain, confusion, forgetfulness. These symptoms can show up within just a day or two of eating a lot of sugar and yet may not be linked to sugar for years.
Sugar affects the body’s insulin levels and can lead to insulin resistance over time, especially when you take in too much. With insulin resistance, the cells in the body have trouble responding to insulin and taking in glucose (blood sugar); when the glucose level in your bloodstream is elevated, it becomes much harder for your body to work. Obvious symptoms of sugar sensitivity are weight gain and pain in the joints.
You know caffeine as the chemical you turn to when you need a quick pick-me-up or something to help you wake up in the morning. What you probably don’t think about is the other effects that caffeine has on your body. At the same time caffeine is alerting your senses and awakening your mind, caffeine is creating a small rise in your blood sugar. That’s not a big deal for a lot of people, but for people with diabetes, caffeine can turn a simple can of soda into a somewhat toxic cocktail. Caffeine becomes dangerous because it works to increase insulin resistance. (Note: Interestingly enough, although caffeine may have negative effects on the body’s blood sugar levels, coffee and tea have both been shown to raise insulin sensitivity and lower blood sugar levels.)
Watching wheat: Looking at celiac disease and gluten sensitivity
To many people, a piece of toast or a bagel for breakfast is a great way to start the day. For people with celiac disease and gluten sensitivity, it can be the start of a day filled with pain and discomfort. Everything made with wheat, barley, or rye is off-limits; even the smallest temptation can cause damage to the small intestine and related health problems.
Celiac disease and associated disorders
Celiac disease is an inherited autoimmune condition that affects both children and adults. It has to do with gluten, the protein found in all forms of wheat — including durum, semolina, spelt, khorasan (Kamut), einkorn, and faro — and related grains, such as rye, barley, and triticale. People with celiac disease have to avoid all foods that contain gluten.
When people with celiac disease eat gluten, it creates a reaction that damages the villi, the nutrient-absorbing projections on the lining of the small intestines. Because the body can’t absorb the nutrients, someone with celiac disease may become malnourished. Even the smallest amount of gluten can pose a threat to people with celiac disease.
Celiac disease can develop at any time, from infancy to adulthood. Although damage to the villi may heal — it takes three to six months to heal in children, two to three years for adults — people with celiac disease must continue to follow a gluten-free diet for the rest of their life.
Some of the symptoms of celiac disease are fatigue, bloating, constipation, weight loss, abdominal pain, gas, diarrhea, and weakness. It can progress to anemia, irritable bowel syndrome, and even early-onset osteoporosis.
Health problems that accompany celiac disease go well beyond the gastrointestinal tract. Damage to the bowels can lead to other autoimmune disorders (disorders that occur when the body’s immune system attacks healthy tissue). Some associated autoimmune disorders, according to the Celiac Disease Foundation (CDF), are
- Addison’s disease
- Alopecia areata
- Chronic active hepatitis
- Graves’ disease
- Insulin-dependent type 1 diabetes mellitus
- Liver diseases
- Lupus
- Raynaud’s syndrome
- Rheumatoid arthritis
- Sjögren’s syndrome
- Scleroderma
- Thyroid disease — Hashimoto’s thyroiditis
In addition, several other disorders have been associated with celiac disease:
- Chronic fatigue syndrome
- Down syndrome
- Fibromyalgia
- Williams syndrome
Nonceliac problems with gluten
Some people have sensitivities to gluten and gluten products without having celiac disease. Nonceliac gluten sensitivity may occur when a person is eating a diet with excessive gluten and gluten products or contaminated with toxins that cause leaky gut, increasing the risk that gluten protein fragments will get into the bloodstream.
Leaky gut syndrome, or increased permeability of the small intestines, is a defect in the barrier between the small intestines and the bloodstream. A little leak is normal, but when things get too leaky, it allows harmful proteins to go directly into the bloodstream without being broken down as they should. The body then looks at those escaped proteins as foreign invaders.
The same autoimmune disorders that can be traced to celiac disease have links to leaky gut syndrome. Some more minor ailments caused by leaky gut syndrome include irritability, sluggishness, tiredness, achiness, and a decline in mental acuteness.
Avoiding gluten
Shopping for a gluten-free diet has become easier thanks to increased awareness of gluten sensitivities, but it’s still a difficult task. Many grocery stores stock a gluten-free section, but that area is seldom more than a few shelves.
At the top of the list of foods to avoid are those made with wheat — which encompasses quite a lengthy list. Anything that contains flour generally contains wheat flour, even if it’s not a whole-wheat item. Wheat can even be lurking in unexpected places — it’s used as a thickening agent and is in a lot of condensed soups, gravy mixes, and sauces as well as in processed meats.
People who have gluten sensitivity or celiac disease also need to avoid foods and products made with barley and rye, which are relatives of wheat. Oats are naturally gluten-free, but they’re often farmed on land on a rotation with wheat and are processed by the same machines, so look for a brand labeled “gluten-free” — Red Mill is a good brand. For more information on celiac disease and avoiding gluten, check out the latest edition of Living Gluten-Free For Dummies by Danna Korn (John Wiley & Sons, Inc.).
Getting Tested for Allergies and Sensitivities
Although everyone’s allergy or sensitivity is different, some foods cause problems more often than others. Some of the most common food allergens are eggs, milk, soy and soy products, wheat, fish, shellfish, tree nuts, and peanuts. People with food allergies should also be cautious about eating other foods from the same evolutionary family. For example, people with wheat allergies need to be careful with other grains.
Some common food sensitivities are cow’s milk, wheat and gluten, soy and soy products, peanuts, corn, eggs, chicken, pork, corned beef, shellfish, oranges and other citrus fruits, strawberries, and tomatoes and other nightshade vegetables.
Figuring out what you’re allergic or sensitive to, and what kind of reaction you have, is an important step in regaining and maintaining health and quality of life. When talking about food allergies and sensitivities, people are most often referring to either immunoglobulin E (IgE) or immunoglobulin G (IgG) allergies/sensitivities. The differences between the two lie in reaction time and severity:
- IgE allergy: An IgE allergy triggers the IgE antibody, which causes an immediate response when the offending substance enters the body. The people who are so severely allergic to peanuts that exposure even to peanut dust can be fatal have an IgE allergy, or classic allergy. Reactions include swelling, hives, difficulty breathing, and even anaphylactic shock.
- IgG allergy/sensitivity: With IgG allergies/sensitivities, the IgG antibody response is typically much more delayed and can include headaches, nausea, fatigue, and/or other digestive symptoms and even seizures. These allergies/sensitivities can also contribute to long-term health issues such as irritable bowel syndrome, diabetes, rheumatoid arthritis, and heart disease.
Three basic types of tests, done by a health care professional, can determine whether you have a food allergy:
- Blood test: The radioallergosorbent test (RAST) is a blood test that’s generally conducted after a person has a recurring reaction to a particular food or foods. Signs of a possible allergic reaction to food are similar to other allergy signs: red or itchy eyes, hives, dermatitis (skin inflammation), coughing or sneezing, or stomach discomfort and diarrhea. A positive test doesn’t determine how severe a reaction to a certain food may be, only that you may have a reaction of some kind.
- Skin test: A skin test, in which the skin is pricked, punctured, or scratched after coming in contact with a potential allergen, may show preliminary signs of allergy.
-
Food elimination test: The elimination test is just as it sounds — a test for allergies conducted by first eliminating all possible allergens from your diet. This test takes some time, because you have to make sure you’ve adjusted to a diet without the suspect foods. You give the allergen-free diet at least a few weeks so your body gets used to the missing allergens.
To determine which foods may be triggers, they’re reintroduced one by one with three to four days between each reintroduction. After you start reintroducing the foods, you keep a log or journal of what you’ve eaten and what, if any, reactions you experienced. After a reaction occurs, you again eliminate that food to see whether the situation reverses — if you broke out in a rash, for example, you make sure the rash goes away.
Your integrative medicine doctor can also test you for food sensitivities using tests that measure IgG, protein levels in foods, or other inflammatory markers including zonulin. All these tests have different levels of accuracy, so be sure to check with you doctor first. It may be better to start with the elimination diet to get a first-hand experience of how food makes you feel.
 Be sure to replace any vitamins and other nutrients you’d be getting from a suspect food with something else, either a vitamin supplement or another food source, during the elimination period. Common food nutrient deficiencies with food allergies and leaky gut syndrome include Vitamin B12, zinc, and iron.
Be sure to replace any vitamins and other nutrients you’d be getting from a suspect food with something else, either a vitamin supplement or another food source, during the elimination period. Common food nutrient deficiencies with food allergies and leaky gut syndrome include Vitamin B12, zinc, and iron.
Working within Your Food Limits to Avoid Inflammation
The best way to avoid the inflammatory responses some foods can create is to know your limits and know what you can and can’t eat. As you discover throughout this book, many serious health issues — diabetes, heart problems, cancer — can be somewhat managed through food.
The key is knowing which foods are good, which are bad, and which are okay in moderation. Here are some tips to help you live with your sensitivities:
- Pay attention. Know which foods cause you discomfort and how you’ll react to them. Does your stomach make strange noises after you’ve had a glass of milk? Does red wine make you feel congested? If so, you likely have an intolerance or sensitivity to these items and, depending on the severity of the discomfort, you’ll want to either eliminate them from your diet or limit the amount you consume. Read labels carefully to avoid accidental ingestion of the problem food.
- Know your limits and vary your diet. Sometimes the amount of a particular food creates more problems more than the food itself. Research shows that eating the same thing three or more times in a week can cause stomach distress, so mix up your diet. Really liking salad is okay, but limit it to once or twice a week — or eat different kinds of salads — to avoid issues.
- Find an alternative. You can almost always find healthy substitutions for the foods on your do-not-eat list; you just have to be open to trying them. Does milk make you bloated or give you intestinal problems? Try almond milk. Have a hankering for some cheese but can’t handle what it does to you? Try some goat cheese, which you may tolerate better than cheese made from cow’s milk.
- Change your preparation styles. What if the problem isn’t the food but the way you prepare it? Sure, those fries are great when they come right out of the fryer, but what if you used sweet potatoes instead of white potatoes and then baked them instead of fried them? You’d consume more nutrients without adding trans fats from the oil.
Understanding the Role of Environmental Toxicity
Today’s environment may be toxic to the food supply. In fact, scientists and nutritionists have been saying it for years. But what exactly do they mean? How can the environment affect the food you eat?
As it turns out, the environment can impact the safety of your food and food sources fairly easily. What’s more, the Food and Drug Administration (FDA) considers certain levels of particular toxins acceptable, so you don’t always know when you’re eating something bad.
Truth is, a variety of substances contaminate the food supply — either before it leaves its origin or somewhere before it hits people’s plates. Some of these contaminants are due to environmental pollution; some of the toxins are from industrial agriculture, such as glyphosates, arsenic, and other heavy metals, sewer sludge, and other pesticides and fertilizers; still others are from food packaging like plastic-lined cans. Your cooking method is another way toxins can enter your food — through your pots and pans, through the additives and preservatives in your kitchen, or even in the way you cook.
Although some levels of these toxins won’t harm you, not knowing what — or where — they are can lead to real trouble. Some of them can be linked to chronic diseases like cancer, hormone deficiencies, and behavioral disorders.
Knowing where some of these dangers are hiding can help you keep your diet on track and your body healthy. Here are some common toxins found in your foods:
- Pesticides: The battle of the bugs has been at the center of the food controversy for decades. But just because you’re aware of it doesn’t mean the danger doesn’t still exist — and many pesticides leave behind residues that can lead to cancer or birth defects. Herbicides, like glyphosates, are also toxic to your food supply.
- Bisphenol A (BPA): BPA is a substance found in the coating inside most food and drink cans and has been known to leach out into the foods it’s supposed to protect. Products with a high tomato content — such as stewed tomatoes or tomato sauce — are particularly dangerous because the acid from the tomatoes increases the amount of BPA released into the food. BPA has been connected to cancer, obesity, and heart disease.
- Sodium nitrite: This preservative is used most often in deli foods, like processed meats, which you should try to avoid, anyway. Be careful when seeing “uncured” or “no added nitrites” on labels; those words may just mean the producers are substituting celery juice, which is naturally full of nitrates. Nitrites and nitrates have been linked to many cancers.
- Heterocyclic amines (HCAs): When you cook your meats and fish at too high of a temperature — think grilling — HCAs form. These toxic carcinogens form when the high heat combines with some of the natural substances of meat and fish. The best solution: Pre-cook meats and finish over a low flame.
- Brominated vegetable oil: It doesn’t sound sweet, but this oil is actually found in fruit-flavored drinks and sodas and has been linked to behavioral problems and reproductive issues in animals.
- Genetically modified organisms (GMOs): Probably one of the most common toxins in today’s food supply, these dangerous organisms —found in corn- and soy-based ingredients, among others — have been linked to organ damage and gastrointestinal disorders.
Eating Clean to Ward Off Inflammation
More than likely you’ve hear a lot about clean eating, but do you really know what cleaning eating means? Is it just a matter of making sure you scrub your fruits and vegetables before eating them?
Well, kind of. But not really. Clean eating is really about changing your eating habits to focus on fresh, whole foods and those that have been minimally processed.
Here are some tips for starting a clean eating lifestyle:
- Stock up on fresh organic fruits and veggies. Doing so is apparently harder than you may think. According to a 2018 study by the Centers for Disease Control and Prevention (CDC), just 1 in 10 Americans were eating the right amount of fruits and vegetables per day; a little more than 12 percent were getting their daily allowance of fruits and just 9 percent were getting their daily allowance of vegetables. Keeping fruits and vegetables a key part of your diet can help in the fight against heart disease, diabetes, some cancers, and obesity.
- Eliminate or minimize processed foods. When you think “processed foods,” the first things to come to mind are likely boxed meals and processed meat. Those are, of course, included, but so are things like refined sugar, white rice, and refined flour. Processed foods include those foods that go through a change so drastic from their original state that they lose many of their nutrients and replace them with sugars and chemicals.
- Eat gluten-free whole grains. If you want to eat grains, be sure to reach for the ones that are least processed, such as steel-cut oats and sprouted grain bread. Refined grains lead to better gut health and can help to reduce inflammation.
- Don’t forget the protein, fat, and carbs. Eating clean doesn’t mean eating only plant-based foods. Include some meats in your diet. Just be careful because processed red meat can actually trigger inflammation. Some good meaty protein sources include wild-caught salmon, tuna, and lean poultry.
- Be sure to read the label. Although eating clean does involve eating mostly natural items, some packaged foods like nuts, some vegetables, and some meats are good, too. Just be cautious — read the labels and look for preservatives, added sugars, or the wrong kinds of fats (refer to Chapter 6 where we discuss fats in greater detail). Some nuts are roasted in vegetable oil, for instance, and some pre-washed salads may come with processed cheese or fatty dressings.
 People who have lactose intolerance can generally tolerate yogurt or other fermented dairy products because they contain helpful live organisms (probiotics) that help with digestion and healing the gastrointestinal system and the good bacteria digest the lactose for you.
People who have lactose intolerance can generally tolerate yogurt or other fermented dairy products because they contain helpful live organisms (probiotics) that help with digestion and healing the gastrointestinal system and the good bacteria digest the lactose for you. Artificial sweeteners often aren’t a good substitute for sugar. Artificial sweeteners increase your cravings for food and increase the risk of diabetes because your brain doesn’t register the artificial sugar is different from the real thing. In many cases, you’re simply replacing one bad thing with another. Instead of using processed sugar cane or sugar beets, you’re consuming the chemicals and preservatives found in sweeteners. We discuss sugar, artificial sweeteners, and natural sweeteners in
Artificial sweeteners often aren’t a good substitute for sugar. Artificial sweeteners increase your cravings for food and increase the risk of diabetes because your brain doesn’t register the artificial sugar is different from the real thing. In many cases, you’re simply replacing one bad thing with another. Instead of using processed sugar cane or sugar beets, you’re consuming the chemicals and preservatives found in sweeteners. We discuss sugar, artificial sweeteners, and natural sweeteners in