One might have imagined that radon, issuing innocently as it does from the ground, would be difficult to politicize.
—Robert Proctor, 1995
We’ve created a statistical illness, multiplying a very small risk by very large populations to come up with the frightening figures.
—Ernest Létourneau, 1987
Radon is a colorless and odorless radioactive gas resulting from the decay of radium and ultimately from uranium, which is ubiquitous in the Earth’s crust and occurs in varying amounts in soil and rock. Normally, radon dissipates harmlessly in the air, but it can seep into homes through fissures and openings in the foundation and can accumulate to produce high levels in homes. Although radon itself is inert, it undergoes radioactive decay to polonium-218 and polonium-214 with the emission of high-energy alpha particles. These radon “progeny” or “daughters” are electrically charged and can attach to fine dust particles in the air, enabling them to be inhaled and deposited in the lining of the lungs. There they can undergo further decay emitting alpha radiation that can damage cells in the lung, leading to the development of cancer. Due to the very short range of alpha particles, radon can only affect the cells lining the lung with which it comes in direct contact, and radon is not known to cause cancer in organs other than the lung.
Geological formations in certain regions of the country have high uranium content, and homes in these regions are likely to have high radon levels. Yet even within the same geographic area, the radon concentration in homes can vary by several orders of magnitude,1 so that it is not possible to predict whether a given house has a problem without making direct measurements. This is because the radon level in a given home is dependent on soil permeability, building construction, air pressure within the house, as well as other factors, such as barometric pressure and temperature. However, other things being equal, houses in areas with high uranium content are more likely to have high residential radon levels than houses in other areas. In addition to its presence in the air, radon can also be present in water, but only about 5 percent of exposure in the United States is believed to derive from exposure to water through activities like showering and cooking.2
Extensive evidence for the carcinogenicity of radon comes from studies of underground miners exposed to extremely high levels and from animal and molecular studies.3 However, the effects of exposure at the much lower levels typical of exposure in homes are unknown. Furthermore, the question of the effects of domestic radon exposure is fraught with complexities, paradoxes, and imponderables that were often lost sight of when radon became a focus of intense public and government concern in the mid-1980s. The gap between what the science indicated and the message that was orchestrated by the federal government, politicians, and the media is perhaps nowhere greater than on the subject of radon. In addition, there is disagreement within the scientific community about the extent of the hazard to the general population from exposure to radon in homes and elsewhere in daily life. However, not all points of view have been given equal weight in the regulatory and political arenas and in the media. Consequently, there has been a slanting of the science, and we will have to examine how this takes place.
FROM OCCUPATIONAL CARCINOGEN TO DOMESTIC THREAT
Although radon itself was not discovered until 1898, the earliest observations of its effects on health date from the sixteenth-century physician Georgius Agricola, who noted the frequent occurrence of a mysterious “mountain sickness” (Bergkrankheit) among silver miners in the Erz Mountains straddling present-day Germany and the Czech Republic. Agricola observed that some women were widowed as many as seven times due to the miners’ high mortality rate. In 1879, based on autopsies and clinical examinations, the physicians F. H. Harting and W. Hesse identified the miners’ malady as pulmonary malignancy,4 and by the early twentieth century the condition was demonstrated to be primary cancer of the lung.5 Over the next thirty years, additional reports suggested that roughly half of the Erz miners eventually succumbed to lung cancer.6 Following the discovery of radioactivity in the late 1890s and the subsequent recognition of radiation-induced cancer, by the 1930s it was hypothesized that high levels of radon gas emanating from the uranium-rich ores in the mines was the culprit. However, this explanation was not universally accepted, and some physicians attributed the miners’ high rate of lung cancer to inbreeding within the population or to other compounds present in the mines.
It was only with the increased demand for uranium following World War II and the expansion of uranium mining that radon was firmly linked to the increased rates of lung cancer among miners. In the 1950s the Public Health Service and the Colorado State Department of Health began sampling radon progeny levels in mines on the Colorado Plateau, and later the first epidemiologic cohort study of Colorado Plateau uranium miners was initiated.7 Analyses of the mortality experience of this cohort, which first appeared in the 1960s and 1970s, demonstrated that miners suffered from an excess of lung cancer and that the risk of disease increased with increasing exposure.8 The results of the Colorado Plateau study were supported by the findings from other cohorts of miners in North America, Europe, and China, and collectively these studies provided the major source of data on the long-term effects of heavy exposure to radon progeny.
Attention to radon as a potential health hazard in homes first arose in the 1970s from the identification of “hot spots” like Grand Junction, Colorado, and central Florida, where homes had been built on the uranium-rich “tailings” left over from the milling of uranium and phospho-gypsum. (Tailings are the huge quantities of fine, grey radioactive sand left over from the milling uranium ore to produce “yellowcake,” which after further refining can be used to fuel nuclear reactors or in making nuclear weapons.) It was also recognized, based on the Swedish experience, that certain building materials, such as alum shale, could contain significant amounts of uranium, producing elevated radon levels in homes. In response to these findings, both the Department of Energy and the Environmental Protection Agency (EPA) established programs to evaluate radon as an “indoor air pollutant.” Prompted by concern about a hazard to homeowners living above mill tailings, Congress passed the Uranium Mill Tailings Radiation Control Act in 1978, and, to comply with the act, in 1983, the EPA set a mandatory “action level” of 4 pCi/L of air as a goal, with an upper limit of 6 pCi, for these homes.9 [The two units most commonly used to measure radon levels in homes are picocuries per liter of air and becquerels per cubic meter (Bq/m3). A picocurie is a trillionth of a curie; 1 Ci is the amount of radiation emitted by 1 g of uranium. One picocurie per liter of air is equivalent to 37 Bq/m3]. As pointed out by several observers, it is ironic that the agency was well aware that many homes had “natural” radon levels that exceeded those found in homes built over tailings but made no effort to address this more common situation.10
In spite of the focus on high radon levels arising from landfills contaminated with radioactive wastes, before the mid-1980s, there were indications that the problem might be of much wider scope. During the 1970s and early 1980s, scientists at Lawrence Berkeley Laboratories and Argonne National Laboratories conducting research into the effects of energy conservation standards on indoor air quality were surprised to find high radon levels in some model homes.11 And following the accidental release of radioactive material from the Three Mile Island nuclear power plant in 1979, measurements in nearby homes showed the presence of high radon levels (20–100 pCi) that were not due to the accident.12
While these developments were of great interest to health physicists and epidemiologists concerned with the biological effects of ionizing radiation, there was no widespread concern about radon in homes and, hence, no pressure for a national policy regarding radon. This was to change as a result of the fortuitous discovery of extraordinarily high radon levels in a home in Boyertown, in eastern Pennsylvania. In December 1984, Stanley Watras, an engineer working on the construction of Philadelphia Electric Company’s Limerick nuclear power plant outside of Pottstown, Pennsylvania, set off radiation detectors on his way into the plant. The source of his contamination was traced to his home, which had levels of 2,800 pCi/L, or 700 times higher than the recommended standard.13 Boyertown is located near the southwestern end of the Reading Prong, a geologic formation rich in uranium ore that stretches from eastern Pennsylvania through north central New Jersey and into southern New York. In the months following the Watras incident, a survey of more than 1,600 homes in Berks County found that nearly 40 percent had elevated radon levels.14
One of the many paradoxes surrounding the question of the effects of exposure to indoor radon is that radon contamination of homes, except for rare instances involving contaminated landfills, is due to naturally occurring uranium in soil and rock and thus did not fit the pattern of man-made industrial pollution. For this reason, it did not clearly come under the EPA’s jurisdiction, and the agency was slow to set policy regarding radon. According to Richard Guimond, who became head of EPA’s newly formed radon division in 1986, the Watras incident was responsible for galvanizing the agency into action.15 In May 1985, on the basis of very limited survey data, the EPA estimated that one million homes around the country might be contaminated at levels posing a serious lung cancer hazard and that from 5,000 to 20,000 lung cancer deaths per year could be caused by residential radon.16 However, by mid-1986 the agency had increased its estimate of the number of affected homes to 8 million,17 and it later revised its estimate of the number of lung cancer deaths attributable to radon to 7,000 to 30,000.18
Federal and state officials, politicians, and the media were quick to characterize the newly discovered problem in the most extreme terms. A front-page article in the May 19, 1985, edition of the New York Times carried the headline “Major Peril is Declared by U.S.,” while an Atlanta Constitution story was titled “Radon in Homes Could Kill 30,000 Yearly.”19 Newsweek reported the EPA’s estimate of the number of affected homes under the headline “Radon Gas: A Deadly Threat—A Natural Hazard is Seeping into 8 Million Homes.”20 According to Robert Yuhnke, the Environmental Defense Fund’s regional counsel in Denver who had been active on radon issues, the situation in the Reading Prong area of Pennsylvania represented the “early stages of a cancer time-bomb waiting to go off.”21 EPA labeled radon “probably the biggest public health problem we have,”22 and the Assistant Surgeon General of the Public Health Service, Vernon Houk, termed radon-induced lung cancer “one of today’s most serious public health issues.”23 Media coverage devoted to radon gas in homes surged in the mid-1980s following the publicity surrounding the Watras home and the ensuing attention to testing of homes. For example, the number of articles on indoor radon published in the New York Times went from zero in 1983 to twenty-two in 1985, to forty-seven in 1986, and to forty in 1987, after which it began to taper off.24
Although EPA officials acknowledged that there was virtually no epidemiologic evidence available regarding the health effects of exposure to radon at residential levels (as opposed to data on exposure to much higher levels in the confined and dusty environment of mines), the agency proceeded to make strong claims about the threat from radon in homes—claims that often had little scientific basis. In addition, the EPA chose to downplay certain aspects of the radon issue, and this led to a national radon policy that many scientists and other observers judged to be misguided. In keeping with its philosophy that there is no safe level of exposure to a carcinogen, the EPA adopted a “conservative” approach to radon. This led it to set what some radon authorities considered to be an overly stringent threshold for remediation of 4 pCi/L of air and to recommend further reducing levels to 2 pCi/L.
The administrators and scientists at EPA who shaped the agency’s radon policy undoubtedly believed that their guidelines were justified by what the agency considered to be a major public health threat. EPA officials argued that indoor radon posed a much more serious hazard than other substances that it had regulated in the past, such as formaldehyde and asbestos. However, a number of factors in the political landscape appear to have played an important role in shaping the agency’s radon policy. First, radon, which had been a localized issue limited to communities contaminated with radioactive debris, quickly became an issue of national concern following the Watras incident. Throughout the second half of the 1980s, a number of powerful members of Congress took up the issue and made radon the focus of congressional hearings. These included Senator Frank Lautenberg of New Jersey (whose home happened to be in Montclair, the site of a bungled and protracted clean-up of a radon-contaminated residential landfill), Senator George Mitchell of Maine, and Representatives Edward Markey and Henry Waxman—the last was chairman of the House Subcommittee on Health and the Environment. Many of the most vocal politicians urging government action on radon were Democrats and liberals, and the radon question quickly took on a political coloration. Early on, the Reagan administration was open to the charge of not addressing the radon problem with sufficient vigor, and politicians like Lautenberg and Waxman exerted powerful political pressure on the government to act aggressively to control radon in homes, schools, and other buildings.25 EPA responded to this pressure by taking a hard line on radon, and, in return, the agency was given sole responsibility for articulating a national radon policy.26 Second, it has been suggested that EPA’s radon policy was also influenced by the agency’s need to distinguish itself from the Department of Energy, which had a long-standing radon program but which, owing in part to its roots in the nuclear power industry, took a more cautious and less activist approach, acknowledging the many uncertainties pertaining to radon.27 Finally, it has been pointed out that, in the antiregulatory climate prevailing during the Reagan years, radon provided the administration with the perfect opportunity to demonstrate its concern for public health without having to confront industry, since the culprit in this case was Mother Nature. Some have characterized the EPA’s radon campaign as “environmentalism on the cheap.”28
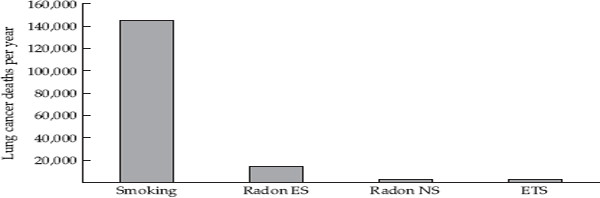
THE EPA’S RADON CAMPAIGN
In August 1986 the EPA published two widely circulated brochures spelling out the main elements of its radon policy: Radon Reduction Methods: A Homeowner’s Guide and Citizen’s Guide to Radon: What It Is and What to Do About It.29 The first publication acknowledged that techniques for remediating home radon levels were poorly understood, but it provided guidelines for those with a serious problem. The second booklet was less tempered and made no attempt to put the radon issue in perspective or to acknowledge the considerable uncertainties. On its first page it stated, without elaboration, that “scientists estimate that from about 5,000 to about 20,000 lung cancer deaths a year in the United States may be attributed to radon.”30 It went on to note that roughly 85 percent of the 130,000 expected lung cancer deaths in the United States in 1986 were attributable to cigarette smoking. But no explicit mention was made of the phenomenon of synergism between smoking and radon exposure, which means that most of the lung cancer deaths ascribed to radon would not have occurred in the absence of smoking. There is only a vague statement on the penultimate page (page 12) of the brochure to the effect that “smoking may increase the risk of exposure to radon.” However, the off-hand nature of the statement and its relegation to the end of the pamphlet suggested that it was an afterthought of little importance. Thus, the brochure conveys the erroneous impression that radon must be responsible for a substantial proportion of the remaining 15 percent of lung cancer that is not explained by smoking.
The Citizen’s Guide also included a chart designed to convey the magnitude of the lung cancer risk due to different levels of home radon in terms of equivalence to the risks from smoking and exposure to chest X-rays. For example, a level of 15 pCi/L of air was equated to the risk of lung cancer of a pack-a-day smoker. The clear message from this chart is that even low levels of indoor radon are something to be concerned about. But these supposed equivalences are meaningless because they fail to distinguish between the effects of radon in smokers and never smokers.
The cornerstone of the EPA’s radon policy was the setting of a recommended “action level” for homes of 4 pCi of radon per liter of air, with the further recommendation that, if possible, indoor levels should be reduced to 2 pCi. In order to identify homes exceeding 4 pCi, the agency urged that all homes below the third floor be tested, since there was no valid method of predicting which homes had a problem. Beyond the decision to set a relatively stringent action level, in its pronouncements on radon the EPA tended to overstate the number of homes with high levels, as well as the magnitude of the risk associated with a given radon exposure. In doing so, it created a great deal of needless anxiety and confusion both about the extent of a health hazard and about the need for testing and the benefits of testing.
Responding to increased concern about radon, in 1986, Congress passed the Radon Gas and Indoor Air Quality Research Act, which essentially made the EPA responsible for determining the magnitude of the indoor radon hazard and the appropriate response. It is significant that the Department of Energy, which had a long-standing research program on radon, was not even mentioned in the bill.31 Two years later, Congress enacted a more ambitious bill, the Indoor Radon Abatement Act, which further delineated EPA’s responsibility to provide updated information regarding the health risk posed by radon and techniques for testing and mitigation, as well providing assistance to state and regional radon programs.32 But, without doubt, the act’s most striking provision, contained in its opening paragraph, was its espousal of the “national long-term goal of the United States” of reducing radon levels in buildings to the level of outdoor air.33 (The median radon level in outdoor air is about 0.5 pCi/L). While such a goal was far from being technologically feasible and would have been prohibitively expensive, supporters argued that it represented a valid long-term objective.
In spite of its wide distribution (one million copies were printed), the Citizen’s Guide to Radon was unsuccessful in motivating large numbers of homeowners to test for radon, and the EPA soon escalated its efforts to gain the public’s attention.34 In the fall of 1988, appearing on national television, EPA Administrator Lee Thomas claimed that up to one third of U.S. homes had radon concentrations exceeding the agency’s action level of 4 pCi/L of air.35 The agency also equated the lung cancer risk due to a daily radon exposure of 4 pCi to that from smoking up to half a pack of cigarettes per day, although there was no scientific basis for this equivalence.36 Again, as pointed out by Philip Abelson, a nuclear physicist and editor of the journal Science, what was most inexcusable about these estimates was the failure to distinguish between radon’s effects in smokers and nonsmokers.37
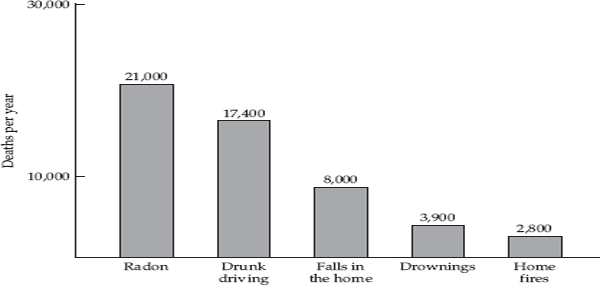
In 1989, in collaboration with the Ad Council, a private, nonprofit organization, the EPA developed an aggressive campaign to overcome the public’s apathy regarding radon, producing advertisements for print media and billboards, as well as spot television commercials. These materials featured anxiety-provoking images and alarming “statistics” to convey a sense of urgency about the lethality of the insidious, odorless gas. Many of the ads urged viewers or readers to call a hotline, 1-800-SOS-RADON, to obtain further information. One pamphlet was titled “Protect your family against Radon . . . the silent killer.” It included an image of a chest X-ray with the caption, “Having Radon in your home is like exposing your family to hundreds of chest X-rays yearly.”38 Many of the ads prominently featured the claim that radon is the “second leading cause of lung cancer in the United States—after cigarette smoking.”39 While technically correct, as we shall see, this formulation is incomplete and quite misleading.
THE PARADOXES OF RESIDENTIAL RADON
The paradoxes and uncertainties surrounding the question of the health effects of low-level radon exposure made it a challenge for scientists and regulators to present an accurate assessment of the risk to the general population. There was always the danger that certain aspects of the problem would be overstated and become the focus of attention and that other equally important aspects would be neglected. Risk assessments conducted by the National Council for Radiation Protection and Measurements and the National Research Council, which produced estimates of the number of lung cancer deaths caused by indoor radon, were careful to spell out the many qualifications and uncertainties attaching to their estimates. However, it was the number of estimated deaths—and, usually, when a range was given, the higher number—that was latched onto by the media, politicians, and the EPA, and where the estimates came from, and what the necessary qualifications and attendant uncertainties were, were lost sight of. Even in scientific papers the perspective could be skewed. But ignoring the paradoxes and the uncertainties only ensured that the resulting policy would be distorted and misguided. For this reason, it is worth pausing to summarize a number of the central paradoxes or contradictions surrounding the question of low-level radon exposure.
The fact that radon did not fit the profile of industrial environmental pollutants has already been noted. A second paradox—some would call it an irony—is that although radon is estimated to account for 55 percent of the average person’s exposure to ionizing radiation,40 other less important sources of radiation, such as nuclear power plants and food irradiation loomed much larger as concerns for most people.41 Though quantitatively more important, apparently, radon is less frightening because it is “natural.” In spite of the EPA’s aggressive ad campaign to overcome what it perceived to be the public’s apathy toward radon, only a small percentage (approximately 5 percent) of homeowners have been motivated to measure the levels in their home.42 The public’s perception of the radon hazard had its own logic and determinants, but prominent among these determinants were the confusing and incomplete public information that was disseminated by the EPA.
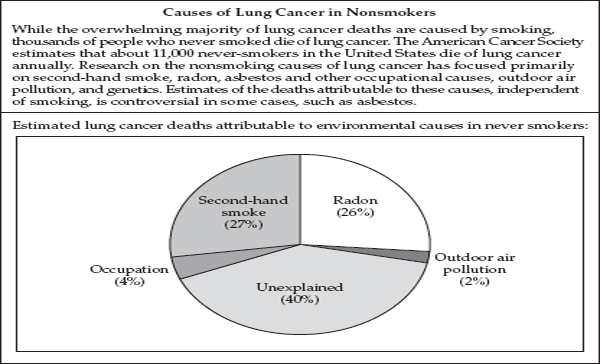
Without doubt, the greatest paradox of residential radon is the fact that the vast majority of lung cancer cases ascribable to radon occur in smokers (current and former). In an interview with the New York Times in January 1988, the chairman of the National Academy of Sciences’ Committee on the Biological Effects of Ionizing Radiation, Jacob Fabrikant, a professor of radiology and biophysics at the University of California, was quoted as saying, “Radon risk is primarily a risk of smokers unless, of course, nonsmokers spend time in a house with extremely high levels of radon. This is another reason to end cigarette smoking.”43 This clear and forceful formulation by a respected scientist should have been kept firmly in view in all discussions of the radon issue since it has profound implications both for understanding the radon issue and for formulating policy. First, it implies that the most effective way to reduce radon-induced lung cancer in the population is to motivate remaining smokers to quit. In those who have already quit, lung cancer risk declines over a number of decades, eventually approaching the risk of those who never smoked. A corollary of the overwhelming importance of smoking as the dominant cause of lung cancer is the fact that lung cancer occurring in lifetime nonsmokers is so rare that it is difficult to determine how much of a risk, if any, average levels of domestic radon pose to those who have never smoked. As we will see, this is a central problem for studies of residential radon.
The interaction between radon and smoking is so fundamental that to speak of radon without making this a central take-home message is inevitably to distort the issue. Yet, the fact that most lung cancer cases due to radon exposure are likely to occur in smokers has not gotten the attention it deserves. It is revealing that in a number of key articles, the narrow focus on radon left little room for adequate attention to, or even mention, of this central fact.44 In spite of efforts to place the radon problem in its proper perspective by keeping the much greater effect of smoking in view, all too often the linkage was lost sight of, and radon became a thing-in-itself, divorced from its crucial context. In this way, the hazard was easily misconstrued and exaggerated.
Another paradox entails the fact that, based on its extrapolation from the miner data, the National Research Council estimated that, if all homes with elevated radon levels were reduced to 4 pCi/L of air, this would only prevent one third of radon-induced lung cancer deaths. In other words, fully two thirds of these deaths were estimated to occur in homes with radon levels below the EPA “action level.” The reason for this is that the vast majority of the population has exposures in this lower range, and the lower level of exposure applied to the much larger “population at risk” contributes more deaths. However, again, it needs to be remembered that approximately 90 percent of radon-induced lung cancer deaths will occur in smokers. Furthermore, although rarely mentioned, it stands to reason that if two thirds of radon-induced lung cancer deaths occur in those with average residential exposures below 4 pCi, an even greater percentage of these lung cancers (that is, greater than 90 percent) are likely to occur in smokers. This is because, at very high exposures, radon is more likely to cause lung cancer in the absence of smoking.
CRITICISM OF THE EPA CAMPAIGN
To many in the scientific community, including health physicists who had devoted their careers to the study of radon, the EPA’s radon policy was not only objectionable on scientific grounds because it ignored many of the complexities and uncertainties pertaining to radon, but it was also bad policy. The agency’s estimate of the number of homes exceeding the action level of 4 pCi/L of air was overstated due to the fact that the early surveys were not systematic and tended to oversample regions with high radon levels and due to reliance on short-term screening measurements that were often made in basements, where radon levels are usually higher than in the lived-in areas of the home. Critics also pointed out that the action level of 4 pCi was set too low, thereby defining a much larger number of homes as requiring remediation. Both Sweden and Finland had adopted welldesigned radon programs based on sound science that had met with public acceptance, using action levels of 10 and 20 pCi/L, respectively.45 Canada had relaxed its cutoff from 4 to 20 pCi.
Largely on the basis of the 1986 analysis of available surveys of radon in homes conducted by Anthony Nero of Lawrence Berkeley Laboratory, the EPA estimated that 12 percent, or 8 million, of the nation’s seventy million homes exceeded 4 pCi/L. However, according to Nero, 7 percent, or five million, would have been a more accurate figure. And he argued that efforts should be focused on identifying the much smaller number of homes (about 1 percent) with average radon levels exceeding 10 pCi and remediating those homes.46
Others, like the physicist and Nobel laureate Rosalind Yalow of the Bronx Veterans Administration Hospital, pointed out that the fact that the rate of lung cancer in never smokers had remained low throughout the twentieth century put a very low limit on any effect of radon in the non-smoking population.47 It could also be argued that, because of the large increase over the course of the twentieth century in the proportion of the population living in apartment buildings, as opposed to single-family homes, the radon exposure of the population may actually have decreased throughout the past century. Such “ecologic” considerations and broad trends cannot resolve the issue of the effects of residential radon exposure, but they merit consideration and can help to put the issue in perspective.
In addition to its estimates of the total number of lung cancer deaths attributable to radon, the EPA also presented a range of risk estimates at various exposure levels.48 According to its figures, people spending 75 percent of their time for 70 years in a home with an average indoor level of 4 pCi/L were said to face an extra risk of dying of lung cancer of between 1.5 and 5 in a hundred. Those with an exposure level of 10 pCi/L would incur an excess risk of 3 to 12 in a hundred. At an exposure level of 200 pCi/L the projected additional lung cancer risk is shown to be between 44 and 77 in a hundred. Actually, these figures are meaningless because it is not specified whether they apply to smokers or nonsmokers, as EPA eventually did in later publications. Naomi Harley, a leading radiation expert at New York University School of Medicine, who assessed radon risks for the National Council on Radiation Protection and Measurements in the early 1980s, called the EPA estimates “outlandishly high.”49 According to her, a one-in-a-hundred excess lung cancer death rate at an exposure of 4 pCi/L should be the midpoint, not the lower bound of the range. Regarding the EPA estimates at the highest levels ranging from 44 to 77 percent for those with an average exposure of 200 pCi, Harley noted that even among the nineteenth-century miners, who had the greatest radon exposures ever recorded, fewer than half died of lung cancer. She concluded that the highest EPA estimates were “out of line with reality.”50
Another source of the EPA’s overestimates of the effects of radon was pointed out by Kenneth Warner and colleagues at the University of Michigan School of Public Health.51 They noted that the EPA’s estimates of the effects of home exposure to radon were severely overstated because the agency failed to take account of residential mobility. They cited the statistic that on average people in the United States change residences 10 to 11 times throughout their lives. Only homes that exceed the EPA’s action level of 4 pCi/L of air are targeted for remediation, and such homes represent only about 7 percent of the nation’s housing stock. Given that the average indoor radon level is 1.25 pCi, the odds are greatly in favor that a move from a high radon house will be to a lower radon house. For this reason, calculating lifetime risk due to an individual’s “current exposure level is not generally a good guide to their cumulative lifetime exposure; it is the latter that determines lung cancer risk.” “In particular, for people living in the high-radon homes the EPA targets for action, normal patterns of residential mobility mean that the vast majority will experience cumulative lifetime exposures equivalent to residing in homes having, on average, much lower radon levels.” Furthermore, the authors went on to demonstrate by use of examples that mitigation of all homes exceeding 4 pCi would reduce the typical individual’s risk by “no more than 30 percent and usually much less.”
Perhaps the most comprehensive and incisive critique of the EPA’s radon policy came from two specialists in environmental engineering, William Nazaroff of the University of California at Berkeley and Kevin Teichman of the EPA itself. Writing in the journal Environmental Science and Technology in 1990, they described what was known about the radon problem and the likely costs and benefits of the current government policy.52 Their central argument was that, when the apparent synergy between smoking and radon exposure and population mobility are taken into account, the cost of remediation of indoor radon “may be less attractive to individuals than to society as a whole.” As an illustration, they showed that for a typical family of four lifetime nonsmokers who live in a house for ten years before moving, the cost of reducing the mean indoor radon level from 260 Bq/m3, or 7 pCi/L, (the mean level of houses exceeding the 150 Bq/m3 action level) to 150 Bq/m3, or 4 pCi, would be about $3,000. The corresponding reduction in the lifetime risk of one lung cancer death in the family would be 5 percent in relative terms, or about 1 in a 1,000 in absolute terms. For a family of smokers, the reduction in absolute risk is more than ten times greater, but only one lung cancer death would be averted among 60 such households, yielding a cost of $180,000 per premature death averted. Regarding implementation of the 1988 Indoor Radon Abatement Act’s goal of reducing indoor radon to the level of “ambient air outside of buildings,” Nazaroff and Teichman determined that, “even if this were technically feasible,” the costs would be “staggering”—on the order of one trillion dollars.
As an alternative to EPA policy, like Anthony Nero, Nazaroff and Teichman proposed identifying the very small fraction of the housing stock (approximately 70,000 homes) with average radon levels greater than 800 Bq/m3, or 22 pCi. Occupants of such homes, they wrote, have an extraordinarily high lifetime risk of developing lung cancer, which should not be ignored. Because these homes tend to be clustered geographically, they can be identified more efficiently by taking into account geological information, thus avoiding the necessity of measuring every household. A focus on highly contaminated homes should be combined with efforts to improve radon measurement and mitigation techniques, foster a public consensus, and set realistic goals for dealing with the problem of domestic radon. Such an approach, Nazaroff and Teichman commented, would yield benefits that cannot be achieved “if the radon problem is treated as an epidemic that requires rapid countermeasures with little regard for scientific uncertainties and accompanying costs.”53
Finally, a number of well-informed observers criticized the agency’s motivational campaign to persuade homeowners to test their homes as gratuitously alarmist and fundamentally wrong-headed.54 Philip Abelson and Anthony Nero blasted the EPA for its “terror” campaign designed to overcome public apathy. Abelson charged that “one of the weaknesses of the EPA is that it seems unable to learn. Its basic policies were set nearly twenty years ago. Whenever a risk is identified, the EPA takes what it calls a conservative approach. This entails developing worst-case scenarios and giving credence to sloppy data if they indicate a greater risk. Experiments that later show that no risk exists are disregarded. Very rarely indeed has the EPA loosened regulations on the basis of new, valid scientific data.”55
Over the past twenty-five years, the question of the health effects of radon has received a prodigious amount of attention from scientists, professional bodies, and government agencies. Progress in delineating the hazard posed by residential radon has been incremental, and the picture that has emerged is complex, with many gaps and uncertainties, but nevertheless with certain fixed and relatively well-established points. However, within the scientific community there are differing assessments of the importance of residential radon as a health hazard, and the consensus view—the dominant interpretation as well as the message that has been put out to the public—has emphasized certain aspects of the problem and downplayed others. Even some of the most authoritative and comprehensive reports are characterized by a peculiar ambivalence and ambiguity, which has contributed to an exaggeration of radon as a public health problem. For this reason, we must now turn to an examination of some of the major documents on the health effects of domestic radon over the past twenty years and how they have been interpreted for a wider audience.
STUDIES OF UNDERGROUND MINERS
When the issue of radon in homes arose in the mid-1980s, studies of underground miners constituted the vast majority of the available evidence regarding the effects of radon exposure on humans. Reports on the mortality experience of uranium miners in the Colorado Plateau had appeared starting in the 1960s and indicated that miners experienced elevated lung cancer risks.56 In 1984, at the behest of the U.S. EPA and the Nuclear Regulatory Commission, the National Research Council of the National Academy of Sciences undertook a detailed report on the health effects of alpha-emitting radionuclides, including radon and its progeny. The report was the fourth report of the National Research Council Committee on the Biological Effects of Ionizing Radiation, or BEIR, and is referred to as BEIR IV. The specific charge to the committee was to analyze the miner data and extrapolate effects downward from the heavy exposures encountered in underground mines to the much lower levels of radon in the domestic situation. Three years in the making, the report, entitled Health Risks from Radon and Other Internally Deposited Alpha-Emitters, came out in January, 1988, immediately following the period of greatest publicity surrounding domestic radon.
BEIR IV
The core of the 1988 report consists of an analysis of the association of radon exposure and lung cancer deaths in four cohorts of underground miners and the extrapolation of risk estimates to the general population due to environmental radon exposure. The committee obtained the original data from the four cohort studies and used specially developed statistical methods to reanalyze it. In the risk model selected by the BEIR IV Committee as best describing the relationship of radon exposure and subsequent lung cancer risk among miners, the relative risk was found to increase with increasing exposure but to decrease with time since exposure and with increasing age. Radon concentrations in underground mines are expressed in terms of “working levels” (WL). (A working level is any combination of radon progeny in one liter of air that results in the emission of 1.3 × 105 million electron volts of alpha particle energy.) Exposure in the mines is expressed in terms of “working level months” (WLM), which is equivalent to one working level for a working month (170 hours). The committee’s risk projections based on the miner data to the levels pertinent to the general population yielded an estimate that lifetime exposure to 1 WLM/year increases the risk of lung cancer by a factor of about 1.5 over the current rate for both males and females, given the prevalence of smoking at the time (mid-1980s). (The average environmental exposure is equivalent to 0.2 WLM/year.57) Excess lifetime lung cancer mortality due to radon was estimated at 350 lung cancer deaths per million person-WLM/year.58 Following its estimates, the committee added a crucial sentence: “In all these cases, most of the increased risk is in smokers in whom the risk is 10 or more times greater than that in nonsmokers.”59 The report went on to list a number of sources of uncertainty affecting its estimates, acknowledging that “the committee recognizes that the differences between the risks in mining and domestic environments and the interaction between smoking and exposure to radon progeny remain incompletely resolved.”60
Although the committee acknowledged the uncertainties attaching to its estimates, some of the limitations of the available data may still have been understated. Of the four miner cohorts, only one (the Colorado Plateau cohort) had any information about smoking habits. Furthermore, of the 151 lung cancer cases used in the analysis, we are not given the number occurring in lifetime nonsmokers but are told that only 22 of the 151 consumed between 0 and 4 cigarettes per day.61 Thus, the BEIR IV analysis could say little about the effects of radon exposure in never smokers, a key question concerning the effects of radon on the general population. Furthermore, inspection of the relevant table62 of the report indicates that the number of smokers in the individual cells, particularly at lower levels of radon exposure and lower levels of smoking, are so sparse as to limit the ability to describe the interaction between radon exposure and cigarette smoking. As Richard Hornung, a radon expert at the National Institute of Occupational Safety and Health put it in 1991, “we have virtually no data on low-level exposed miners who didn’t smoke.”63
BEIR VI
Eleven years after the publication of the BEIR IV report, in 1999 a second report from the National Research Council entitled Health Effects of Exposure to Radon, provided a new, updated analysis of the miner data, this time based on 11 cohorts and including 68,000 miners and 2,700 cases of lung cancer, as compared to the 4 cohorts and 360 lung cancer deaths in BEIR IV.64 The large increase in the available data permitted a refinement of the model developed in the earlier report.
After extensive analysis, BEIR VI concluded, on the basis of what was known from studies of underground miners and an understanding of genomic damage caused by alpha particles, that exposure to residential radon is “expected to be a cause of lung cancer in the general population.”65 The analysis further indicated that there was a “synergistic effect” of radon together with smoking, although the precise nature of the interaction—whether “multiplicative” or “sub-multiplicative”—could not be determined. Most importantly, the committee estimated that between 15,400 and 21,800 lung cancer deaths per year in the United States could be attributed to domestic radon exposure, although the authors indicated that, given the uncertainties in the analysis, the actual number of deaths could be between 3,000 and 33,000. (The authors also estimated that between 2,100 and 2,900 of the lung cancer deaths caused by radon occur in never smokers.) These numbers, the committee noted, make radon “the second leading cause of lung cancer” after cigarette smoking.66
For all the sophisticated statistical modeling provided in the report, two major problems cast doubt on the ability make accurate estimates of the effects of radon at residential levels based on the miner data. These are the dearth of data on miners exposed at low radon levels and the powerful effect of smoking.
The core of the report consists of two components: (1) the extrapolation of the miner data from the 11 cohorts down to the levels encountered in homes and (2) the meta-analysis of the available case-control studies of residential radon. Each of these topics was addressed in a paper in the Journal of the National Cancer Institute published in the mid-1990s,67 and the results were presented in greater detail and in updated form in the 1999 report. I will refer both to the papers and to the report.
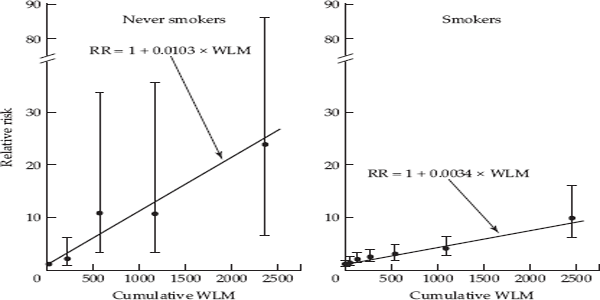
The analysis of the combined miner data from the 11 cohorts showed that cumulative radon exposure in miners was directly related to risk of lung cancer—in a linear manner—in both ever smokers and never smokers (fig. 5.1). In addition, based on theoretical considerations, the committee posited that there was no threshold, i.e., no level below which radon would not affect the risk of lung cancer, although it acknowledged that the existence of a threshold could not be ruled out. Application of the “linear no threshold model” to the miner data implied that even at the low levels encountered in most homes, radon exposure would carry some risk.68
In addition to analyzing the full range of the miner data (ranging from 0 to 2500 WLM of cumulative exposure), the committee carried out a separate analysis, restricted to cumulative exposures below 50 WLM. This level was judged to represent the upper range of residential exposure. (Living in a house with a radon level of 1 pCi/L of air for 1 year is roughly equal to 0.2 WLM of exposure. In order to accumulate 50 WLM of exposure, a resident would have live in a house with a radon level of 10.8 pCi/L for 25 years.)
In fig. 5.1, domestic exposure, in the range below 50 WLM, corresponds to the leftmost point on both graphs. This level of exposure has a relative risk that appears to be indistinguishable from 1.0 (i.e., no increased risk).
Of the eleven cohort studies analyzed, only six had any information on the smoking history of the miners, and even where there was information in some cases this was limited or was only available on a portion of the subjects. On the basis of this imperfect information, 58 percent of the miners appear to have smoked. However—and this critical fact is not directly stated—only 3 percent of lung cancer deaths in those cohorts with information on smoking history occurred in never smokers. [The 3 percent figure is obtained by dividing the number of lung cancer cases occurring among miners who never smoked (64—obtained from BEIR VI, Table C-13) by 1,814—the total number of lung cancer cases in the 6 miner cohorts that had some information on smoking history (extracted from the tables in Appendix D, BEIR VI, p. 254 ff.).] What this means is that at the very low exposure levels typical of homes, the number of lung cancer cases in miners who never smoked must be extremely small. (Lubin and Boice note that there are 358 lung cancer deaths among miners with cumulative exposure below 50 WLM.69 If 3 percent of these are never smokers, that equates to about 11 never smokers.) In other words, there is little basis for assessing the effects of radon exposure in this range on never smokers. Furthermore, it is difficult to see how it is possible to assess the interaction between radon and smoking at low levels of exposure since this depends on having a credible estimate of the effect of radon in never smokers.
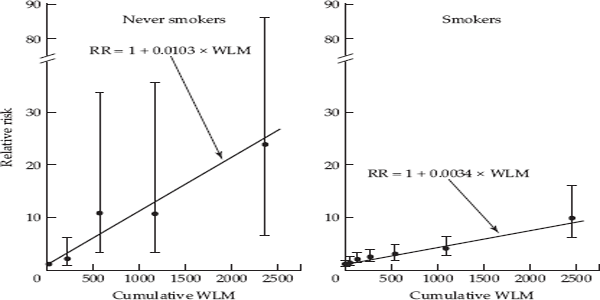
FIGURE 5.1 Relative risk of lung cancer by cumulative radon concentration for all eleven miner cohort studies combined, for reported never smokers and ever smokers. Source: Lubin et al., 1995.
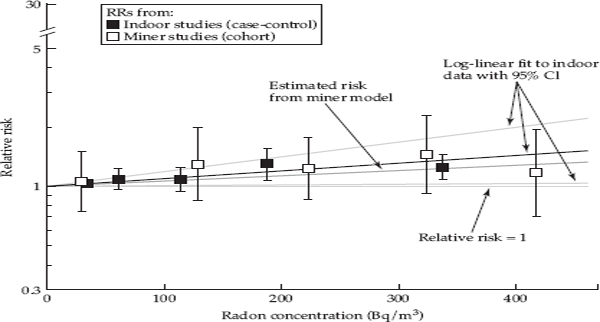
Based on a meta-analysis of the eight case-control studies published as of that time, the committee concluded that the trend in the relative risk for the combined studies was statistically significant and indicated a relative risk of 1.14 (95 percent confidence interval 1.0–1.3 at 150 Bq/m3, or 4 pCi).70 Figure 5.2 shows the results of the meta-analysis of the indoor studies (black squares) and those from the underground miner studies (open squares) restricted to exposures below 50 WLM. Both sets of estimates are in the same range, and the committee concluded that the results of the case-control studies were consistent with those seen in miners. However, the five risk estimates (open squares) based on the miner data at low exposure levels (below 50 WLM) are all between 1.0 and 1.5, and none is statistically significantly different from 1.0 (no increased risk), reflecting the paucity of data. The pooled residential data (black squares) show a small elevation in the relative risk for the two highest exposure levels, but these data include smokers.
In addition, there are a number of other problems and uncertainties acknowledged by the committee that will be mentioned in the next section. Thus, for the committee to make projections about the number of lung cancer deaths attributable to domestic radon exposure in never smokers based on the miner data appears questionable. Nevertheless, these estimates are included in the report’s Executive Summary and are widely accepted as fact, even though the many necessary qualifications enumerated in the report rarely get mentioned.
FIGURE 5.2 Summary relative risks (RR) from meta-analysis of indoor-radon studies and RRs from pooled analysis of underground miner studies, restricted to exposures under 50 WLM. Source: National Academy of Sciences, 1999.
Both the Journal of the National Cancer Institute papers and the BEIR VI report perform a fascinating balancing act. On the one hand, they present the results of careful statistical modeling of the available data and lay out the many limitations and attendant uncertainties pertaining to the analysis. On the other hand, in spite of the many intractable limitations and uncertainties, the authors feel compelled to present estimates of the effects of radon on the general population and in never smokers, and the underlying message is that radon is important as an environmental carcinogen. A reflection of this conceptual balancing act is an ambivalence and ambiguity that permeates these texts. For example, the abstract of the 1995 Journal of the National Cancer Institute paper concludes that, “In the United States, 10% of all lung cancer deaths might be due to indoor radon exposure, 11% of lung cancer deaths in smokers, and 39% of lung cancer deaths in never-smokers.”71 The final sentence adds the qualification: “These estimates should be interpreted with caution, because concomitant exposures of miners to agents such as arsenic or diesel exhaust may modify the radon effect and, when considered together with other differences between homes and mines, might reduce the generalizability of findings in miners.”72 Similarly, in the discussion section of the 1997 paper devoted to the meta-analysis of eight case-control studies of residential radon, the authors repeat no less than four times that the “results must be cautiously interpreted.”73 Finally, the closing sentences of the Executive Summary of the BEIR VI report are a consummate feat of balancing complex and competing aspects of the radon problem, as they shift back and forth between different emphases:
The qualitative and quantitative uncertainty analyses indicated that the actual number of radon-attributable lung cancer deaths could be either greater or lower than the committee’s central estimates. This uncertainty did not change the committee’s view that indoor radon should be considered as a cause of lung cancer in the general population that is amenable to reduction. However, the attributable risk for smoking, the leading cause of lung cancer, is far greater than for radon, the second leading cause. Lung cancer in the general population and in miners is related to both risk factors and is amenable to prevention.74
In this way, the authors of these reports manage to have it both ways. But, in spite of the carefully calibrated balance, in the final analysis, the message conveyed by the reports is that radon is important and that by itself it accounts for a significant proportion of lung cancer incidence. In the end, the focus is narrowed to radon alone, and estimates are given for the number of lung cancer cases “due to radon.” In order to frame broad conclusions, the carefully articulated caveats formulated by the committee needed to be shunted to the side. In the final analysis, statistical models, which include many uncertainties and assumptions, are used to make estimates based on sparse data, and these estimates are then put forward as valid descriptions of reality.
EXTRAPOLATING FROM MINERS TO DOMESTIC RADON EXPOSURE
As the BEIR VI Committee was careful to acknowledge, differences between radon exposure in underground mines and in homes were numerous and substantial and raised questions about the validity of extrapolating from the former to the latter. First, as mentioned above, levels in underground mines were orders of magnitude higher than the levels in homes. According to Lubin and colleagues,75 the lowest levels in mines were 50–100 times higher than the average level in homes of about 1 pCi/L of air. There were also important differences in the conditions of exposure in the two environments. As described by Krewski and colleagues,76 these include the relative proportion of radon to its decay products (which affects how much energy is delivered to the lung), a person’s breathing rate (which affects the rate at which radon and its progeny are inhaled and deposited in the lung), and the size of dust particles in the air (which influences the fraction of radon attached to particles and the depth of penetration and retention within the lung). As mentioned earlier, another limitation of the occupational data on miners is that most miners were smokers. In addition, other substances, some of which are carcinogens, including arsenic, silica, and diesel exhaust, were present in certain mines, complicating the identification of effects of exposure to radon alone. Furthermore, most miners worked for only a few years underground, whereas the relevant period for residential exposure is many decades.77 Finally, the miner data were limited to males and did not address possible differences in exposure and susceptibility of women and children.78
It was this awareness of the marked differences between radon exposure in the occupational setting of mines and in homes that provided the impetus for carrying out studies of residential exposure. But, from the outset, radon experts were under no illusions that these studies would be easy to conduct or that they would resolve the question definitively by detecting a strong and unambiguous effect of residential radon.79
In his critique of the EPA’s radon policy delivered in 1991, Philip Abelson had called for a large epidemiologic study of residential radon exposure as a way to resolve the question that had generated so much alarm and confusion.80 Such a study would have to be large enough to permit distinguishing the effects of exposure to low levels of radon typical of most homes from the potent effects of smoking. But Abelson argued that the millions of dollars spent on such a study would be a “better investment than spending billions of dollars on remediation that might be a waste of money.”81 Others have argued that the key group in which an effect of domestic radon needed to be demonstrated was lifelong nonsmokers, who accounted for only a small percentage of lung cancer cases.82 Female never smokers, in particular, should be focused on since historically women have spent more time in the home and typically have less exposure to occupational carcinogens. Furthermore, most lung cancer in never smokers occurs among women. An adequate sized study of this group was projected to require several thousand cases and an equal number of controls.83 However, a large national study of residential radon as envisaged by Abelson and others was never undertaken. Instead, many small case-control studies were carried out in different areas of the United States and Canada, as well as in Europe and China, and most did not focus exclusively on lifetime nonsmokers. None of these studies came even close to being of a size necessary to tease apart the effects of radon from those of smoking or to detect an effect of radon in lifetime nonsmokers.
CASE-CONTROL STUDIES OF RESIDENTIAL RADON
The cohort study design, which was used to study underground miners, was not feasible to assess the effects of indoor radon on the general population. Such a study would require very large groups of free-living subjects who would have to be followed for a long period of time in order to monitor their exposure and determine their health status.84 The case-control study offered an alternative that theoretically, at least, could address the question of the effects of residential radon exposure. In this type of study, newly diagnosed cases of lung cancer could be identified through hospitals and cancer registries, and a control group representative of the general population could be identified through random digit dialing, Medicare rosters, or population registries. Cases and controls could then be interviewed concerning their residential history and smoking habits, and radon levels could be measured in the current and former residences.
The major problem confronting case-control studies of radon is that of accurately characterizing an individual’s exposure over a period of several decades preceding his or her recruitment into the study. The average American will have lived in as many as eleven different homes during his or her lifetime, and the prospect of measuring even those homes inhabited during the two to three decades preceding recruitment posed formidable problems. Ideally, one would want to obtain long-term measurements (preferably for one year) in each of these homes. However, in practice, this was not feasible because some homes will no longer exist, some will be unoccupied, and in other cases the current owner may refuse to cooperate. Even where homes are accessible, radon measurements made in the present may not reflect past levels owing to modifications in the home or the heating system.
Some studies dealt with this problem by including only cases and controls who had lived in their current home for 10 or more years, while others attempted to obtain measurements in the previous home as well. Still other studies attempted to measure all homes lived in for at least a year within a thirty-year “time window” up to five years before recruitment into the study.
In all studies, there were homes in which measurements could not be made, either because the home was not accessible or because the radon device malfunctioned, and consequently there were gaps in some subjects’ exposure history. How one handles such missing data can influence the estimate of a person’s cumulative exposure.
Furthermore, in order to accurately characterize an individual’s exposure, one would also want to know how much time he or she spent at home during different periods and where, within the house he or she spent time, especially in multilevel homes, because radon levels can vary significantly in different parts of a home and on different floors. Most case-control studies placed one or two radon detectors in the living area and bedroom of residences, but few took measurements on upper floors, and few obtained information on the subject’s allocation of time within the house.
The challenges confronting case-control studies of domestic radon were laid out with clarity in a 1990 article entitled “Design issues in epidemiologic studies of indoor exposure to Rn and risk of lung cancer” and published in the journal Health Physics.85 The authors, Jay Lubin, Jonathan Samet, and Clarice Weinberg, were prominent epidemiologists or statisticians in the field of radon. Lubin and Samet were members of the BEIR IV and BEIR VI committees, and Samet had chaired the latter. The burden of the article was to caution researchers that, because of the many problems and biases involved in carrying out these studies and particularly in obtaining radon measurements intended to characterize an individual’s exposure over many years, studies would have reduced statistical power to test key hypotheses regarding the effects of radon. Specifically, the authors considered the impact of such factors as subject mobility (which tends to reduce lifetime exposure toward the population mean), the choice of the model used to characterize the effects of radon, and errors in calculating exposure. Errors in estimating exposure stem from a number of sources, including errors in the measuring devices, exposure to radon outside the home, “the inability to measure exposures over time in current as well as previous residences, and the unknown relation between measured concentration and lung dose of α energy from the decay of Rn and its progeny.” The authors referred to the “formidable methodological problems” that make case-control studies of radon “difficult to carry out and that may limit their interpretation.”
Appearing when it did in 1990 before the publication of all but one of the U.S. case-control studies, the paper by Lubin and colleagues provided a much needed caveat concerning what could be expected of individual case-control studies of indoor radon and lung cancer. They wrote that “realistically such studies may never be able to answer many of the subtle questions about risk patterns that burden current risk assessment with uncertainty.” And they went on to say:
Even the most carefully designed and conducted investigations are subject to substantial error in dosimetry, particularly when used to estimate temporally remote exposure. Inappropriate design assumptions with regard to the underlying effect, subject mobility, and exposure distribution also seem inevitable.86
In their conclusion, the authors “urge[d] cautious interpretation and reduced expectations for case-control studies.” They noted that some studies may fail to show any association simply due to inadequate power owing to insufficient sample size and to biases that reduce the effects toward the null. However, they also cautioned that other studies may indicate an effect that is substantially higher than that expected based on the miner data and that such results should be interpreted carefully since they could be due to small samples and the “selective publication of positive results.” The authors looked forward to the future pooling of the many small case-control studies as a way of overcoming the problem of inadequate sample size and obtaining more precise estimates. The results of such pooling efforts have begun to appear and are still in progress.
Although it is a technical paper published in a specialized journal, the points made by the authors are accessible to any interested reader. The paper should have been required reading for anyone interested in understanding the reports of individual case-control studies.
RESULTS OF THE INDIVIDUAL STUDIES
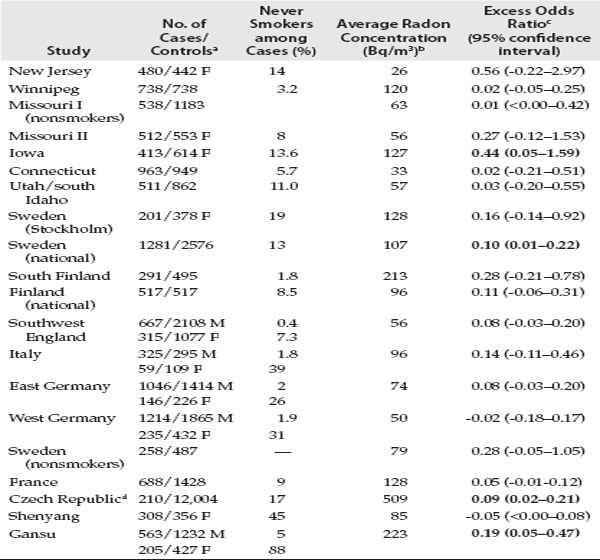
Studies of residential radon exposure using long-term direct measurements began appearing in the early 1990s, and additional studies have continued to appear up to the present. More than twenty studies have been carried out in North America, Europe, and China. Their results are summarized in table 5.1. For each study, the table presents the number of cases and controls, the percentage of never smokers among the cases, the average radon concentration, and the “excess odds ratio” at 100 Bq/m3. A value above 0 is indicative of increased risk. For example, the excess odds ratio from the Iowa study of 0.44 can be read as a 44 percent increase in the risk of lung cancer associated with an increase in radon concentration of 100 Bq/m3.
The studies differ in many respects, including their measurement protocols, the number of homes in which measurements were attempted, and whether they included all cases or were limited to nonsmokers or women. Most studies are suggestive of a small and not statistically significant increase in risk of lung cancer due to radon exposure. Of the 20 studies listed in table 5.1, only four show a statistically significant excess odds ratio associated with radon exposure. Of these four studies, one (conducted in Iowa) shows an excess risk four-and-a-half fold greater than two of the other studies. Two studies—the largest single study carried out in West Germany and a study in Shenyang, China—showed a nonsignificant inverse association between radon levels and lung cancer risk. In other words, increasing radon exposure appeared to be associated with reduced risk of lung cancer. However, no study showed a significant inverse association of radon with lung cancer risk. (A new report on a case-control study conducted in Worcester County, Massachusetts, presents results that are strikingly at variance with those in table 5.1. Thompson and colleagues found that, after controlling for smoking and other potential confounding factors, radon exposure was strongly inversely associated with lung cancer risk.87 What makes this modest-sized study of particular interest is the fact that the investigators attempted to address a number of the weaknesses of previous studies by obtaining detailed information on allocation of time within the house over different life periods and by improving quality control. The results are not included in table 5.1 because the authors did not present the excess odds ratio.)
Interestingly, studies with the highest mean radon concentrations (Czech Republic; Gansu, China; South Finland; France; Stockholm; Iowa; and Winnipeg) did not provide stronger evidence of an effect than the studies where concentrations were lower. The New Jersey study had by far the lowest mean radon concentration in homes but the highest excess odds ratio, whereas the Winnipeg study had a relatively high mean radon concentration but one of the lowest excess odds ratios. In fact, there is no correlation between the radon concentrations and excess odd ratios presented in table 5.1 (r = – 0.008, p = 0.97). This is worth mentioning because regions with higher radon levels should provide a greater opportunity to observe an association due to the wider range of exposures.
In studies that give the smoking status of men and women separately, the proportion of never smokers among male cases ranges from 0.4 percent in England to 5 percent in Gansu, China. Among female cases the proportion of never smokers ranges from 8 percent in Missouri to 88 percent in Gansu, China. Thus, male cases, who comprise the majority of cases, are almost all smokers. This means that, as is true of the miner cohorts, these studies can tell us little about the effect of radon in men who never smoked and are severely limited in their assessment of the interaction between smoking and radon, which requires adequate numbers of never smokers. Even though the proportion of never smokers is higher in female cases, because the number of cases in females is smaller, here too the power to detect an effect of radon exposure in never smokers is limited.
TABLE 5.1 Case-Control Studies of Residential Radon and Lung Cancer
Adapted from Krewski et al., 2005.
aAbbreviations: F, females; M, males.
bValues given are mean residential radon concentrations, except for the study from Italy (geometric mean) and the study from Shenyang, China (median).
c Excess odds ratio at 100 Bq/m3. Note that an excess odds ratio greater than 0 indicates potentially increased risk. Bolded numbers indicate statistically significant results.
d This study is a cohort study.
POOLING OF INDIVIDUAL STUDIES OF RESIDENTIAL RADON
By 2005, two analyses of the pooled residential radon studies had appeared, one conducted on thirteen European case-control studies, the other on seven North American case-control studies.88 By virtue of their large numbers, these analyses provided more precise estimates of the risk associated with a given level of domestic radon exposure. And the pooled estimate could then be compared with estimates based on extrapolation from the miner experience. The European analysis included a total of 7,148 lung cancer cases and 14,208 controls, while the North American analysis included 3,662 cases and 4,996 controls. There were 884 lung cancer cases among lifelong nonsmokers in the European analysis and 659 in the North American analysis, enabling a more sensitive and accurate assessment of effects in this key group than was previously possible.
Both analyses used a similar approach. Studies were included if they had used long-term detectors to measure radon concentrations in the living areas and bedrooms of homes currently or previously occupied. Time-weighted average radon exposure was calculated for each participant in terms of becquerels per cubic meter (Bq/m3) (1 Bq equals one disintegration per second, and 37 Bq/m3 are equal to 1 pCi/L). Each analysis used a time window for exposure (five to thirty-four years prior to diagnosis of lung cancer in the European analysis and five to thirty years prior to diagnosis in the North American analysis).
In the European analysis, the risk of lung cancer was found to increase by 16 percent (95% confidence interval 5 to 31 percent) per 100 Bq/m3 in usual radon exposure. This means that those exposed to 100 Bq/m3 have an odds ratio for lung cancer of 1.16, and those exposed to 200 Bq/m3 have an odds ratio of 1.32, etc. The large numbers permitted the researchers to assess the effect of radon with fine stratification for smoking history, including average number of cigarettes smoked per day, duration of smoking, and age of starting to smoke. The dose-response appeared linear with no threshold, and there was a significant dose-response relation even below the currently recommended action levels. In the North American analysis, lung cancer risk increased by 11 percent (95% confidence interval 0 to 28 percent) for each increase of 100 Bq/m3. The odds ratio for the highest exposure level (>200 Bq/m3) compared to the lowest level (<25 Bq/m3) was 1.37 (95% confidence interval 0.98 to 1.92).
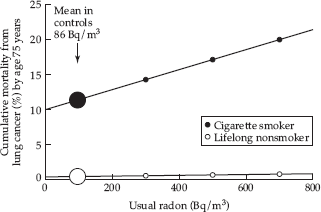
The emphasis in both analyses is on the finding of an overall association of residential radon exposure with increased lung cancer risk. In both analyses the relationship appears to be linear with no threshold. And both studies note the consistency of the findings with extrapolations from the miner data. There is, however, one striking difference in the presentation of the results of the two papers. In the discussion in the North American analysis, no attention is given to smoking and its interaction with radon. In contrast, the European analysis makes the dramatic and crucial point that, although the increase in the relative risk due to radon is comparable in smokers and never smokers, because the former have so much higher a risk of lung cancer, the absolute risk due to radon is approximately 25 times higher among smokers. This is shown in fig. 5.3 from Darby and colleagues, where in lifelong nonsmokers, the cumulative absolute risk of lung cancer by age 75 due to radon is virtually indistinguishable from zero.
Thus, in line with the BEIR VI report’s conclusion based on the miner data, Darby and colleagues’ analysis makes clear that the vast majority of excess lung cancer caused by radon occurs in smokers. Even with the greatly increased sample size, it is still unclear what the effects of radon are in never smokers. Curiously, in spite of the evidence from their analysis, Darby and colleagues keep the emphasis on radon, concluding that radon in the home “accounts for about 9% of deaths from lung cancer and about 2% of all deaths from cancer in Europe.” And the final sentence of the paper emphasizes the effectiveness of remediation of radon levels in homes, in spite of the questionable impact of remediation on lung cancer rates compared to that of quitting smoking.
At present, efforts are in progress to pool the worldwide studies from North America, Europe, and China.
A DIVERGENT VIEW
Not everyone is comfortable with the reigning consensus regarding residential radon, which could be interpreted as conveying the message that radon at any level is a significant hazard, even in those who have never smoked. We have already encountered the views of a number of scientists and observers who voiced strong criticism of what they considered to be a misrepresentation of the effects of indoor radon. Much of this criticism came from health physicists. However, a small number of epidemiologists have also expressed a divergent view and feel that the radon issue has been exaggerated and distorted. These scientists tend to emphasize the considerable difficulties posed by the studies, their methodological limitations, and the overwhelming role of smoking as the dominant cause of lung cancer. They strike a note of skepticism, whereas those who have articulated the consensus position, even while acknowledging the many uncertainties, ultimately imply that radon, even at very low levels, is an important problem.
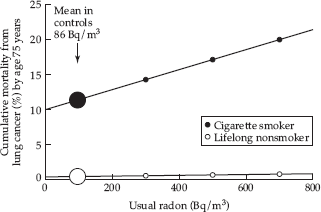
FIGURE 5.3 Cumulative absolute risk of death from lung cancer by age 75 years versus usual radon concentration at home for cigarette smokers and lifelong nonsmokers. Source: Darby et al., 2005.
But the skeptics are at a distinct disadvantage when it comes to gaining a hearing for their point of view. They tend to be isolated individuals as opposed to the shapers of the consensus, who have the backing of powerful institutions, including the EPA, the National Research Council, and the National Cancer Institute. Several of the scientists standing apart from the reigning consensus pointed out to me how small the number of individuals is that, to a large extent, controls the prevailing view on radon. These individuals, who preside over committees issuing influential reports on radon and who write prominent editorials on the topic, are also likely to review any new paper on the topic for major journals and to review grants in the area of radon. According to several scientists, these figures are unlikely to be sympathetic to researchers who take a more skeptical position. And they are unlikely to find a paper or a grant proposal that takes a critical view of the radon problem to be of sufficient interest to merit publication or funding. As Dale Sandler, who is head of the epidemiology branch of the National Institute of Environmental Health Sciences, remarked, “Conventional wisdom, especially when controlled by a small number of people, is very hard to overcome.”89
What does the alterative viewpoint look like? For one thing, there is a large area of agreement. There is no dispute that data on underground miners and experimental studies demonstrate that heavy exposure to radon causes lung cancer. The differences have to do with the uncertainty about the effects of exposure at low levels typical of most homes and distinguishing the effects of radon from those of smoking. Ultimately, the dissenters are concerned with putting risks of different magnitudes in perspective and acknowledging the limitations of the existing studies as a basis for risk assessment and policy formulation. Two recent publications articulate this more skeptical and more nuanced point of view.
In 2002, John Neuberger, an epidemiologist at the University of Kansas, and Thomas Gesell, a health physicist at Idaho State University, published a detailed and critical inventory of studies of residential radon exposure, focusing on the results in nonsmokers.90 Their rationale for concentrating on this group was that “from a public health perspective, the lung cancer risk in smokers can best be reduced through smoking cessation.” They noted that smoking rates are declining in the United States and that, if this trend continues, lung cancer rates should decrease in the future, regardless of what is done to control residential radon exposure. In contrast, it is unknown whether radon reduction by itself would provide a significant reduction in risk among smokers. They do acknowledge, however, that nonsmokers exposed to high indoor radon levels could potentially benefit from radon reduction, and this leads to the central concern of their paper—that relatively few studies of residential radon focus on the risk in nonsmokers.
Neuberger and Gesell reviewed the existing studies on residential radon describing their design, summarizing their findings, and identifying limitations. The limitations they discussed include the following: varying definitions used for smoker, ex-smoker, and nonsmoker; failure to account for other potential risk factors; use of surrogate interviews; insufficient sample size; and difficulties of reliably estimating an individual’s historical radon exposure. They concluded that a major “challenging problem” even for the better studies is the lack of focus on nonsmokers: “Major public health questions arise for non-smokers, including the effect (if any) of residential radon exposure, the existence of a threshold, and any interaction with passive smoking. The individual residential studies appear to shed little or no light on these issues, possibly because many of them were not designed, nor had the statistical power, to examine these important questions.”91
The second paper that appears to question the reigning consensus reports the results of a large case-control study carried out by Sandler of the National Institute of Environmental Health Sciences.92 The study, conducted in Connecticut, Utah, and southern Idaho, was designed in the early 1990s with the aim of improving exposure characterization compared to some of the early studies of residential radon. Specific improvements included obtaining a large sample size, taking into account residential mobility and variations in exposure levels within a home, and imputation of missing measurement data using several sources of data which can help to predict radon levels. A total of 1,474 newly diagnosed cases and 1,811 population controls were included, making this one of the largest studies of residential radon exposure.
In spite of the study’s many methodological refinements, the authors found that, “Overall, there was little association between time-weighted average radon exposures 5 to 25 years prior to diagnosis/interview and lung cancer risk.”93 Several of their initial assumptions proved incorrect. For example, actual radon levels in the two states were much lower than had been expected on the basis of surveys. Only 3 percent of homes in Connecticut and 7 percent of homes in Utah/southern Idaho had radon levels exceeding the EPA action level of 4 pCi/L of air. Also, in spite of efforts to maximize the number of nonsmoking lung cancer cases, the authors had too few nonsmoking cases for separate analyses. (“Thus, despite its large size, the study lacked sufficient power to detect main effects at the observed exposure levels and we had limited power to detect interactions.”)
In addition to the overall lack of an association between radon exposure and lung cancer, findings within subgroups failed to suggest any meaningful pattern. Sandler and colleagues concluded that, “This study provides no evidence of an increased risk for lung cancer at the exposure levels observed.”94
Beneath its measured language and careful presentation and discussion of its data, the paper has the earmarks of a corrective to what the authors imply is an overinterpretation of studies of residential radon. This makes it all the more interesting that Sandler and her coauthors note that their findings, although null, are nevertheless consistent with the pooled findings of the seven North American studies. She and three of her coauthors are also authors on that paper.95 This tension between interpretations of individual studies and of the pooled data underscores the ambiguity of findings from studies of residential radon, which was anticipated by Lubin, Samet, and Weinberg in 1990. Perhaps most provocative is Sandler’s mention at the very end of her paper that there may be a level below which radon exposure does not pose a detectable risk: “It is clear from studies of highly exposed populations that radon causes lung cancer. What is less certain is whether or not there is a threshold level below which there is no effect and what proportion of lung cancer can truly be attributed to radon—alone or in combination with cigarette smoking. Only an extremely large study can provide answers to these questions.”96
Given their assessments of studies of domestic radon, Neuberger and Sandler were less than totally enthusiastic about the undertaking of pooling the various individual studies. Neuberger, who is a co-investigator on the Iowa case-control study of radon, concedes that aggregating the individual studies is a worthwhile exercise but cautions that the results should not be taken as providing definitive answers.97 He emphasizes that the individual studies were never designed with a view to being combined. They used different methods, different inclusion criteria, different measurement protocols, different quality control, and different definitions of a never smoker and an ex-smoker. For example, Neuberger questions the definition of a never smoker used in the European pooled analysis—someone who has not smoked more than 400 cigarettes per lifetime. He believes that this allows inclusion of some people who smoked at a low level and who should not be classified as never smokers. In addition, he points out that the Darby study is suggestive of a higher risk in men than in women. Because women typically have spent more time in the home and have been less likely to be exposed to occupational carcinogens, this raises a question. Neuberger also notes that Darby’s data (fig. 5.3) show a very slight increase in risk for never smokers with increasing radon exposure. However, the graph combines both men and women. Neuberger suspects that the increase may be limited to men, and, for the reasons just mentioned, he feels that women should be analyzed separately. He concludes that the risk estimates that constitute the consensus view on radon “gloss over the fact that the risk of radon-induced lung cancer in never smokers would be minimal or none.”98 Sandler says she is “not enthusiastic about the forthcoming worldwide pooling unless the group can use the combined data to ask more thoughtful questions that deal with how complicated it is likely to be in reality.”99 Thus, the goal of isolating a true effect of indoor radon exposure through the exercise of pooling the worldwide case-control studies seems to be ever-receding.
***
How have the EPA’s pubic educational materials changed to reflect the substantial body of scientific evidence on the effects of residential radon exposure that has accumulated over the past fifteen to twenty years? The answer appears to be, hardly at all. Even when the risks associated with indoor radon have been clearly delineated and put in perspective, as was done by the National Research Council in 1999, due to the institutional agenda of the Environmental Protection Agency and the tendency to select numbers that suit its purposes, the key facts surrounding the hazard posed by radon continue to be distorted. The fact that most radon-induced lung cancer deaths will occur in smokers is nowhere explicitly stated even in the most recent EPA literature regarding radon. Instead, the agency resorts to well-intentioned but illogical comparisons, omission of key facts, and impractical proposals to convey the importance of the radon hazard. (I am referring to the recommendation that physicians counsel their patients regarding the importance of testing their homes for radon.) As recently as September 2005, in its A Citizen’s Guide to Radon, EPA cited the figure of 21,000 lung cancer deaths per year due to radon exposure and displayed a dramatic bar chart comparing deaths from radon to deaths from accidents, including drunk driving, falls in the home, drownings, and home fires.100
The arresting graphic (fig. 5.4), which appears on page 2 of the pamphlet, is apparently designed to impress the reader with the magnitude of the radon problem in order to motivate citizens to have their homes tested. However, the bar chart is misleading in two ways. First, it indicates that radon is responsible for more deaths per year than each of four causes of accidental death. But the comparison makes little sense. Unlike accidents, which are instantaneous events, lung cancer due to radon results from exposure over a period of decades. Clearly, it would not have suited EPA’s purposes to make the more logical comparison of the number of radon-induced deaths with the much larger number of deaths from chronic diseases—say, the total number of deaths from lung cancer, from all cancers, and from coronary heart disease—which would have helped to put this estimate in perspective.
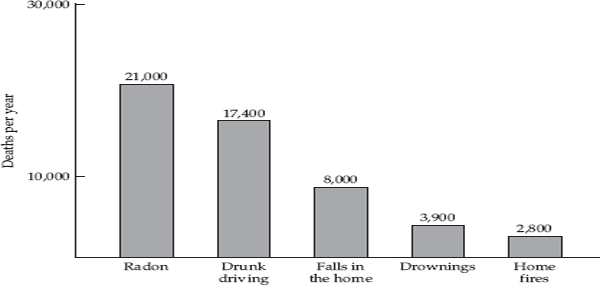
FIGURE 5.4 The U.S. Environmental Protection Agency’s estimate of the number of lung cancer deaths in the United States each year due to radon compared to the number of deaths from other causes. Source: U.S. EPA, 2005.
The second aspect of the bar chart, that is even more misleading, is the failure to mention the crucial role of smoking in radon-associated lung cancer. In the brochure’s “overview,” on page 3, the agency continues to emphasize that radon is the “second leading cause of lung cancer in the United States today,” without making any mention of the synergism between radon and smoking. It is only on page 11 that the reader is told that one’s “chances of getting lung cancer from radon” depend on “whether you are a smoker or have ever smoked.”101 And page 12 displays a table showing that the risks associated with a given level of radon exposure are roughly seven times higher in smokers compared to never smokers. Even this reference to the “synergism” between smoking and radon, while appropriate, does not really convey to the general reader the crucial fact that roughly 90 percent of radon-induced lung cancers occur in smokers. If the EPA had been concerned to give an accurate picture of the radon hazard, it would have referred to the known lung cancer risk factors and would have distinguished between the effect of radon in smokers and never smokers. The resulting bar chart would have looked like that shown in fig. 5.5, which makes clear that not only is radon-induced lung cancer a distant “second cause of lung cancer” following smoking, but that 90 percent of radon-induced lung cancer occurs in smokers. Estimated radon-induced deaths in never smokers (about 2,000–3,000) represent less than 2 percent of all lung cancers and are comparable to the number of lung cancer deaths ascribed by the EPA to environmental tobacco smoke.
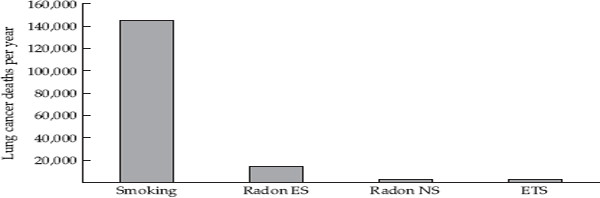
FIGURE 5.5 Estimates of lung cancer deaths from different causes. Estimates of deaths due to radon among ever smokers (ES) and never smokers (NS) come from National Research Council, 1999, p. 15. Estimate of the number of lung cancer deaths due to environmental tobacco smoke (ETS) comes from U.S. EPA, 1992.
Misinformation regarding radon is not the sole province of the EPA. The confusion surrounding the hazard posed by radon is illustrated by a pie chart purporting to show what is known about the causes of lung cancer in people who have never smoked that was published in a recent issue of the Journal of the National Cancer Institute.102 The graphic in fig. 5.6, which comes from the American Cancer Society, shows that radon and passive smoking each account for a quarter of lung cancer occurring in never smokers. (This estimate for radon is based on BEIR VI.) As we have just seen, there is really no scientific basis for this claim since studies of residential radon are acknowledged to be problematic and since extrapolation from the high levels of exposure in dusty mines in which most miners were smokers to the much lower levels in homes is also problematic. Nevertheless, owing to the tendency to overstate what is known and to want to fill in the pie chart, this “factoid” has received wide circulation. Once such an estimate is put out by an authoritative source, it will be widely cited. In contrast, careful review of the literature on risk factors for lung cancer in never smokers has led several epidemiologists to conclude that we do not know what causes the majority of lung cancers occurring in those who have never smoked.103 Here is what two prominent epidemiologists have to say in a recent textbook of cancer epidemiology: “Lung cancer among nonsmokers is not rare: it is about as common as cancer of the pancreas. Occupational factors, passive smoking, and indoor exposure due to radon do not explain more than a minor proportion of these cases, and dietary, infectious, and genetic factors are currently receiving attention.”104 And in a comprehensive review of the causes of lung cancer in nonsmokers, a group of researchers actively involved in studies of radon and lung cancer arrive at a similar conclusion: “it is clear that the largest contributors to the etiology of lung cancer in nonsmokers have not been elucidated.”105
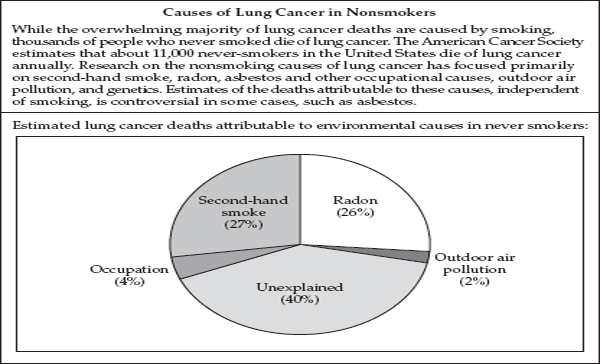
FIGURE 5.6 Causes of lung cancer in nonsmokers. Source: Stat Bite 2006:664.
***
Efforts to pin down the effects of residential radon are reminiscent of the movie Blow-up by Michelangelo Antonioni in which a photographer continually enlarges a photograph in which he may have unwittingly recorded a murder. The more he enlarges the photo, the grainier it gets, and the evidence he seeks continues to elude him. This is an apt metaphor for efforts to document effects of indoor radon exposure at what are, on average, very low levels. (The average level in U.S. homes is only slightly more than twice the concentration in outdoor air.) It should be possible to acknowledge that radon at such levels could theoretically pose some additional risk of lung cancer but that all available evidence indicates that this increment of risk is going to be small. According to the radiation expert John Boice, the average relative risk of lung cancer due to exposure to environmental radon is on the order of 1.2.106 (This includes smokers, as well as never smokers). This relative risk, which is equivalent to a 20 percent increase in risk, needs to be put in perspective by comparing it to the risk of lung cancer due to smoking—about 20-fold for a male current smoker and about tenfold for a male ex-smoker, or a 2,000 and 1,000 percent increase, respectively. The lung cancer risk of a heavy smoker (of more than two packs per day) can reach 4,000 or 6,000 percent. Instead, we have seen how strong is the tendency to make radon into a more substantial problem than it likely is. Scientists and regulators with a professional stake in radon may not be in a position to give an objective assessment of its importance. It should be possible to acknowledge that much is known about the effects of radon at high levels encountered in mines but that we cannot characterize the risk at the very much lower levels typical of homes. It should be possible to acknowledge uncertainty where this is appropriate, where everything tells us that this is an area of uncertainty, beyond the resolving power of currently available methods and data. But it is a lot easier to come up with estimates of a number of deaths (“the body count”) attributable to an agent, even if these are questionable. This satisfies a deep desire in the regulator and scientist. It provides a justification for their efforts and for large amounts of money spent on radon abatement and research. After all of the attention devoted to radon, few are going to be satisfied with a conclusion that says, “We don’t know what the effects are at these low levels. There may be a very small effect, or possibly there may be no effect.”
Box 5.1 Major Take-Home Points
Radon is a radioactive gas resulting from decay of radium and ultimately from uranium that occurs naturally in rock and soil. Radon can seep into homes through cracks in the foundation and, under certain conditions, accumulate to reach high concentrations. Radon decays to form “progeny,” which emit a type of radiation capable of being inhaled and causing cancer in the cells lining the lung.
It has been known since the early twentieth century that underground miners exposed to high levels of radon gas have an increased risk of lung cancer. However, the possibility that residential radon could pose a hazard only became a subject of widespread concern in the mid-1980s, when extraordinarily high levels were detected in a home.
In spite of the paucity of data on the effects of radon exposure at the generally low levels found in homes, in 1986 the U.S. Environmental Protection Agency set an “action level” of 4 pCi/L for single-family homes, advising that levels exceeding 4 pCi should be reduced. On the basis of early, nonsystematic surveys of radon levels, 8 million homes were estimated to be in need of remediation.
Radon was labeled “the second leading cause of lung cancer” and was estimated to cause between 6,000 and 30,000 lung cancer deaths per year in the United States. However, it was rarely made clear that roughly 90 percent of deaths attributed to radon are likely to occur in smokers and would not have occurred in the absence of smoking.
Because studies of underground miners constituted the major source of information on human exposure to radon, elaborate analyses were carried out to extrapolate downward from the effects of exposure in miners to those in the general population due to residential exposure. However, this type of extrapolation entails a number of assumptions that may not be valid. Most importantly, miners had much higher exposures and the majority of miners were smokers. Furthermore, the conditions in underground mines were very different from those in homes.
Since the early 1990s, studies of residential radon exposure have been carried out. Such studies are subject to serious problems of measuring radon exposure over a period of decades as well as detecting an effect of radon independent of the effect of smoking. The individual studies show inconsistent results, and pooling of the individual studies has been undertaken to provide a more stable estimate. Two major poolings indicate a small increase in risk associated with increased radon exposure. However, again, roughly 90 percent of the effect of radon is accounted for by smokers, and effects in never smokers remain unclear.
Efforts to assess the impact of residential radon on lung cancer continue. However, there is tendency to avoid putting the risk due to domestic radon in perspective, and, consequently, the hazard, particularly to never smokers, appears to have been greatly overblown.