CHAPTER 22
QUICK FIXES FOR RUNNING′S “BIG 6” INJURIES
A Run for Life runner isn’t supposed to get IT band syndrome, Achilles Tendonitis, Runner’s Knee, tendonitis and chrondomalacia, shin splints, plantar fasciitis, and hamstring strains. Theoretically, if you build a strong, balanced body, running form, and workout program, you won’t get injured bad enough to have to pay a physical therapist like Bob Forster to repair you. But we’re all human, subject to overtraining and biomechanical inefficiencies. “If you have pain in the same place for two workouts in a row or over the course of a week or two, consider yourself injured,” says Forster. “For every two days you train in pain, it will take two to get better.” Below are the 6 big runners’ injuries and—besides swimming, cycling and other logical cross-training options—what you can do yourself to rehab them.
1. IT BAND SYNDROME
What it is / Symptoms : Iliotibial (IT) Band Syndrome, one of the leading causes of lateral knee pain in runners, includes extreme pain on the outside of the knee, pelvis, or hip, while running, squatting, and doing knee-bending exercises. The pain, often worse while walking or running downhill, is caused by the continual rubbing of the IT Band (the thick sheath of tissue on the outer thigh running from the outside of the pelvis, over the hip, down to the knee, attached to the tibia) against and over the lateral femoral epicondyle (the outside hump of the end of the thigh bone). The IT is crucial to stabilizing the knee during running, shifting from behind the femur to the front during the gait cycle.
Causes: Tight muscles in lower extremity and pelvis; structural or functional leg length inequalities (a short or long leg); excessive foot pronation from poor shoe choices or faulty running mechanics.
Treatment: Fix incorrect running mechanics and keep the IT and outer thigh muscles loose with stretches, deep tissue massage, foam rollers, and The Stick. Also, stretch the glutes, strengthen the hip abductors (especially the gluteus medius), which control ITB tightness, and strengthen the quads to lessen the load on the IT bands.
2. ACHILLES TENDONITIS
What it is/Symptoms: Dull or sharp pain above the back of the heel due to inflammation of the Achilles—the tendon that connects the two major calf muscles, the soleus and the gastrocs—to the heel bone. Over time, it gets covered with scar tissue and, in extreme cases, can tear or rupture.
Causes: Running too far, too fast, or too steep on tight, fatigued, or untrained calves, which transfer the burden to the Achilles. Natural overpronators are at highest risk.
Treatment: Stop running and avoid weight-bearing activities until the pain disappears; be patient—it could be weeks.
Stretch and massage the both the gastroc and soleus (see Chapter 12, stretches #3 and 4), gently at first, then more rigorously and frequently. Use The Stick (see photo). Don’t run until heel raise and jumping are pain-free.
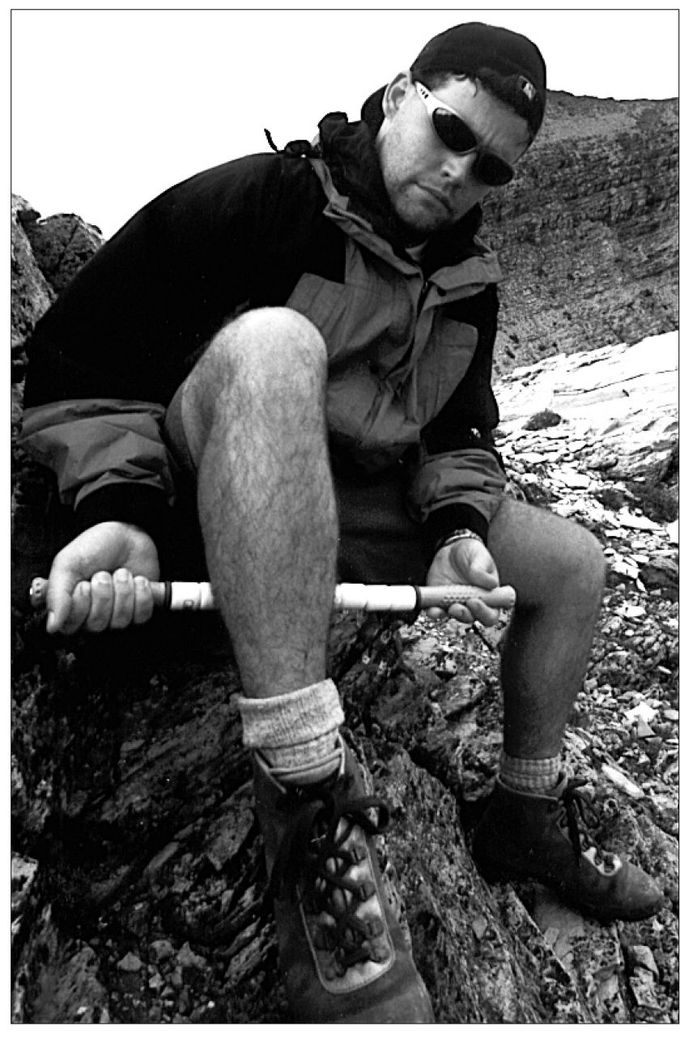
The Stick
3. RUNNER′S KNEE
What it is / Symptoms: Any pain in the kneecap. The two most common forms of runner’s knee are patellar tendonitis, a tendon strain, and something much worse and permanent: chondromalacia, a fraying and deterioration of the cartilage that coats the end of the femur and the backside of the kneecap.
Causes: Overtraining, poor biomechanics, overpronation, and tight, imbalanced leg muscles. In chondro, the culprit is “lateral tracking,” in which the V-shaped backside of the kneecap no longer rides in the center of the groove in the end of the femur, but high on the groove’s lateral side, scraping off cartilage in the process. It will not grow back.
Treatment: For tendonitis, rest and cross-train until pain disappears. For chrondro, cut your loses by stretching the IT bands and outer part of the quadriceps, the vastus lateralis (VL) to loosen their lateral pull on the kneecap. At the same time, strengthen the inner part of the quad, the vastus medialis oblique (VMO). This will realign the kneecap back into the groove between the two condyles (humps) of the femur. Do pool running until pain disappears. For overpronation, try motion control shoes.
4. SHIN SPLINTS
What it is / Symptoms: Razor-sharp pain on the inside of the shin bone from knee to ankle, technically called Medial Tibial Stress Syndrome (MTSS), caused by any of a half a dozen problems. The most common is trauma to tendons and muscles where they attach to the front of tibia. While trying to stabilize the foot, ankle, and lower leg, the muscles exert great force at this point, often causing strains and microtears.
Causes: The sudden shock of hard running after a long layoff, a too-big increase in mileage, tight Achilles and calves, excessive forward lean, worn-out shoes, sudden change in running venue from soft to hard surfaces; lack of warm-up and stretching.
Treatment: Stretch the calves three times daily and before and after activity. Warm up the area before running; ice it after cooldown. Cut back to half your current mileage and stop all hills and speed work. Water-run. “Do not wait,” says Forster. “This injury can lead to stress factures in your tibia, which will keep you off your feet for a longer time.”
5. PLANTAR FASCIITIS
What it is / Symptoms: Pain in the bottom of the heel due to inflammation of the plantar fascia—a thick, tough, fibrous band of connective tissue that runs along the bottom of the foot in a fanlike manner from heel to the base of each toe. During running and walking, it acts to stabilize the metatarsal joints (the joints associated with the long bones of the foot) during impact with the ground, acts as a shock absorber for the entire leg, and helps to lift the longitudinal arch of the foot to prepare it for the takeoff phase of the gait cycle. The fascia is thinnest near the heel, which is why the pain occurs there.
Causes: Inflexible calves, especially the tibialis posterior (a muscle located underneath the soleus and gastrocnemius that connects from the arch of the foot up to the back of the knee) that limits the tibia’s ability to move forward at the ankle joint. This lifts the heel early and increases the tension in the plantar fascia. Also, a sudden increase in hill training or general volume, and large weight gain or pregnancy.
Treatment: Stretching or deep massage to relax calf muscles to allow less stressful bending at the ankle. Putting about a small lift under your heel will reduce the ankle bend a bit. Strengthening the fascia with toe-grasping drills and barefoot running will help, too.
6. HAMSTRING STRAIN AND ISCHIOGLUTEAL BURSITIS
What it is / Symptoms: These are two similar conditions caused by biomechanical imbalances. Both can cause persistent or growing pain and tenderness in the back of the thigh during and after workouts; loss of flexibility and pain when stretching; bruising; and pain during sitting. It is caused by a sudden tear (you may hear a “popping” or “snapping”) or accumulated microtrauma (from overuse) in the hamstring group, the three large rear-thigh muscles that extend from the pelvis at the “sit bones” (the ischium) to the top of lower leg bone (tibia), below the knee. These “two-joint” muscles are very active in running and biking. Ischiogluteal Bursitis refers to inflammation of a fluid-filled sack (bursa) that lies between the sit bone (ischium) and the butt’s huge gluteus maximus.
Causes: All causes are biomechanical and may be exacerbated by: overuse (too much work with too little recovery); leg length discrepancy; tight glutes, hamstrings, hip flexor, and quadriceps; poor running mechanics; improper bike fit.
Treatment: Rest from all painful activities; cross-training if it produces no pain; cross-fiber massage to break up the scar tissue that makes the muscle unable to contract in that area, causing weakness, pain, and frequent reinjury, restrengthening the muscle; stretch associated muscles but avoid directly stretching the injured muscle before scar tissue is resolved, as the scar tightens with aggressive stretching. Physical therapists like Forster use ultrasound, electric stimulation, and icing to fight inflammation and swelling.