There is, as has been suggested, a seductive familiarity in the symmetrical manner with which The New Genetics and The Social Theory sought to explain the causes of disease, evoking the separate contributions of nature (the gene) and nurture (upbringing) in human development.
The great appeal of The Social Theory is that it both provides an explanation for disease and opens the way to preventing it. The major significance of Bradford Hill’s demonstration in 1950 of the causative role of smoking in lung cancer is that it held out the possibility of the dramatically different and potent alternative of ‘mass prevention’ to the problem of illness. Self-evidently, public health campaigns to discourage people from smoking were likely to have a greater practical benefit, by orders of magnitude, by preventing lung cancer than seeking, not very successfully, to treat it with surgery or drugs. Prevention, as everyone knows, is better than cure. Indeed, the many great achievements of the therapeutic revolution, the ‘cornucopia of new drugs’ and the ‘triumphs of technology’, could simply be dispensed with were it possible to identify modifiable causes of common diseases in people’s everyday lives. The problem was that up until the mid-1970s the precise causes of these diseases remained quite unknown. And then, suddenly it seemed as if this ignorance was being swept away as, with increasing certainty, it was asserted that, in precisely the same way as abjuring smoking prevents lung cancer, so most cancers together with heart disease and strokes were similarly preventable were people to change their social habits. The rise in the scope and ambition of The Social Theory is really quite extraordinary. Thus a booklet published by the British Medical Association in the late 1960s with the old-fashioned title ‘Doctor’s Orders’ advised readers of the dangers of smoking, the merits of a ‘sensible balanced diet’, and particularly to avoid becoming overweight. It warned that drinking more than a bottle of wine a day (or its equivalent) could damage the liver. But that was all. By the 1990s, this sensible – if rather obvious – advice had escalated to encompass every aspect of people’s lives. The advice on a ‘sensible balanced diet’ had metamorphosed into the claim that the serious diseases are quite simply the outcome of specific foods people consume: salt overloads the circulation, pushing up the blood pressure to cause paralysis or death from stroke; saturated fats in dairy foods and meat fur up the arteries to cause untimely death from a heart attack, as well as being ‘implicated’ in causing many common cancers including those of the breast and bowel.
Meanwhile scientific investigations revealed that numerous other unsuspected hazards in people’s lives, including the minuscule quantities of chemicals and pollutants in air and water, were similarly implicated in a whole range of serious illnesses such as leukaemia, stomach cancer, infertility and much else besides. This was medicine on the grand scale of the great sanitary reforms of the nineteenth century when civil engineering, by providing a clean water supply, eradicated water-borne infectious diseases such as cholera. Now social engineering, by encouraging people to adopt healthy lifestyles, together with a serious assault on the environmental cause of disease, would have a comparably beneficial effect.
While it is very difficult to evaluate all the relevant evidence for such assertions, their origin undoubtedly can be traced to a powerful and persuasive critique by Professor Thomas McKeown in 1976 of the prevailing view that the progress of medical science could take the credit for the prodigious improvements in health over the preceding 100 years. On the contrary, he argued, doctors might pride themselves on the modern drugs and technology they deployed in their shiny new palaces of disease, but in reality they had played only a minor role in the precipitous fall in infant and maternal mortality and the substantial increase in life expectancy. These achievements could more readily be attributed to social changes: ‘Medical science and its services are misdirected,’ he said, ‘because they rest on an indifference to the external influences and personal behaviour which are the predominant determinants of health.’
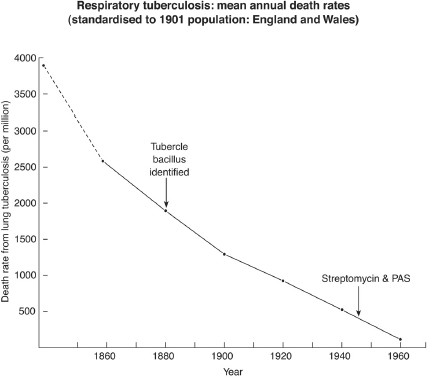
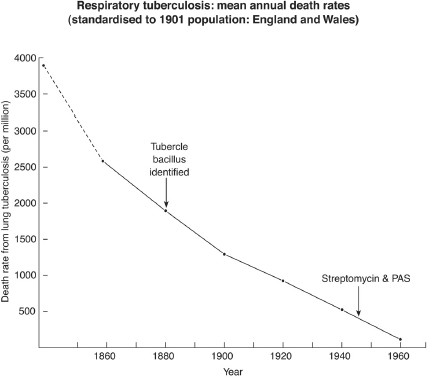
The essence of McKeown’s argument is encompassed in a single graph (see page 354) showing the decline in mortality from tuberculosis of the lungs in England and Wales, from a peak of 4,000 per million of the population in 1838, down to 350 per million in 1945 when the drugs streptomycin and PAS were introduced, and then almost to zero by 1960. Thus 92 per cent of the decline in tuberculosis could be attributed to ‘social factors’ and only 8 per cent to the great miracle of twentieth-century medicine, antibiotics. From this McKeown concluded that ‘medical intervention can be expected to make a relatively small contribution to the prevention of sickness and health’. He conceded that there was ‘no direct evidence’ that social factors were primarily responsible; nonetheless it seemed plausible enough that better nutrition, improved hygiene and housing (and particularly the decline in overcrowding) could account for this massive decline of tuberculosis.1
Similar sentiments had been expressed before. If McKeown had merely limited his observations to the past, they would have had little impact, but he used this example of the apparently limited contribution of antibiotics (such as streptomycin) to the decline of tuberculosis to infer that the same principles applied to contemporary medical problems in the 1970s. And certainly the parallel was compelling enough. There were, he claimed, two broad categories of preventable illness: the ‘Diseases of Poverty’, which obviously included infectious diseases like tuberculosis, but also the ‘Diseases of Affluence’ which had become more prevalent with growing prosperity – cancer, strokes and heart disease. So, just as the Diseases of Poverty had declined as society had become wealthier, the Diseases of Affluence would diminish by adopting a more rigorous and ascetic lifestyle: ‘The diseases associated with affluence are determined by personal behaviour, for example refined foods became widely available from the early nineteenth century . . . sedentary living dates from the introduction of mechanised transport, cigarette smoking on a significant scale has occurred only in recent decades.’
(Adapted from Thomas McKeown, The Role of Medicine, Oxford: Blackwell, 1979.)
The characterisation of these preventable Diseases of Affluence struck a most resonant chord. Thus the following year, in 1977, the Assistant Secretary of Health to the US Government told a Congressional Subcommittee: ‘There is general agreement that the kinds and amounts of food we consume may be the major factor associated with the causes of cancer, circulatory disorders (heart disease and strokes) and other chronic disorders.’ Soon afterwards Sir Richard Doll, former colleague of Sir Austin Bradford Hill and now Professor of Medicine at Oxford, provided his authoritative support. Following an extensive review of the relevant evidence, he had discovered that, leaving aside smoking, patterns of food consumption accounted for 70 per cent of all cancers in the Western world.2 And there was more. Professor Samuel Epstein of the University of Illinois, writing in the journal Nature in 1980, argued that a further 20 per cent of cancers were caused by minute quantities of chemical pollutants in the air and water and were thus also theoretically preventable.3 So, within four years of McKeown propounding his Social Theory, it seemed that he had been well and truly vindicated, and if attention were paid to modifying these ‘social factors’ then more deaths would be prevented every year than there were people dying.4
It cannot be sufficiently stressed what a radical departure this Social Theory of disease was from the preceding thirty years. The achievements of the previous three decades had been hard-won; the pursuit of the cure for leukaemia had taken the best part of twenty-five years, drawing on specialist scientific expertise from many disciplines and requiring the accidental discovery of no less than four different types of anti-cancer drugs. But now here were distinguished doctors and scientists arguing that the future of medicine lay in a completely different direction: get people to change their diets, control pollution, and many diseases would evaporate like snow on a sunny day. Could it be that simple? Why had no one conceived of the problems of disease in this way before? Certainly, had they done so, much time and energy would have been saved trying to discover treatments for common diseases that now could so easily be prevented.
It might sound almost too good to be true, but The Social Theory was enthusiastically taken up by many. Politicians and policy-makers, alarmed at the escalating costs of modern medicine, were impressed by McKeown’s arguments that the emphasis on expensive hospital-oriented medical services was misdirected and that, were the emphasis to be shifted towards ‘prevention’, the health services would be not only much more effective but also a lot cheaper into the bargain. Such sentiments were echoed by intelligent observers, as reflected in the BBC’s prestigious Reith Lectures for 1980, given by a young lawyer, Ian Kennedy, committed to the ‘unmasking of medicine’. ‘The elimination of the major infections has served as a star witness for the triumphs of modern medicine over illness,’ he observed, ‘but this has had the unfortunate consequence of creating a “mythology” where the doctor is portrayed as a crusader engaging in holy wars against the enemy of disease . . . The promise of more and more money to wage this war will not improve the quality of health care.’ Rather ‘the whole project’ had to be reoriented towards ‘prevention and health promotion’ – and who could argue with that?5 Since the war, ‘the public health’ had been very much the poor relation of medicine, marginalised by the glamorous successes of open-heart surgery and transplanting kidneys. Here now was the opportunity to change all this and reassert the priority of preventive measures in the finest tradition of the nineteenth-century sanitary reformers. This ‘new’ public health movement, as it styled itself, was to move forward relentlessly from the early 1980s, warning people of the dangers lurking in their food supply and in the air and water. And it was a dynamic process that every year brought evidence of yet further unanticipated hazards of everyday life, while those responsible for health policy felt it necessary to proffer ever more precise advice on how the public should lead their lives.
And how much of it was true? It is necessary to bear a few general points in mind. First, the radicalism of The Social Theory is that, as suggested, it goes far beyond the self-evident truism that those who pursue a ‘sober lifestyle’ – drinking sensibly, abjuring tobacco, avoiding obesity and staying fit – are likely to live longer and healthier lives. Rather, contentiously, it makes specific claims about the causative role of commonly consumed foods and environmental pollution as a major factor in common illnesses. Next, we are citizens of a society in which, utterly uniquely for the first time in history, most people now live out their natural lifespan to die from diseases strongly determined by ageing. Thus the putative gains from ‘prevention’ (if real) are likely to be quite small. Further, the human organism could not survive if its physiological functions such as blood pressure (implicated in stroke) or level of cholesterol (implicated in heart disease) varied widely in response to changes in the amount and type of food consumed. These functions rather are protected by a ‘milieu intérieur’, a multiplicity of different feedback mechanisms that combine to ensure a ‘steady state’. Hence truly substantial changes in the pattern of food consumption are required to change them and to influence the types of disease in which they have been implicated.
Finally, man, as the end product of hundreds of millions of years of evolution, is highly successful as a species by virtue of this phenomenal adaptability. Humans can and do live and prosper in a bewildering variety of different habitats, from the plains of Africa to the Arctic wastes. No other species has the same facility, so it might seem improbable that for some reason right at the end of the twentieth century subtle changes in the pattern of food consumption should cause lethal diseases.
Finally, the evidence for The Social Theory is overwhelmingly statistical, based on the inference that the lives we lead and the food we eat cause disease in the same way that smoking causes lung cancer. Throughout this discussion it will be necessary to bear in mind Sir Austin Bradford Hill’s insistence that such statistical inferences by themselves have no meaning unless they are internally coherent, that is to say, when the several different types of evidence for an association between an environmental factor and disease (such as tobacco and lung cancer) are examined, they all point to the same conclusion. Put another way, no matter how plausible the link between dietary fat and heart disease might seem, just one substantial inconsistency in the statistical evidence effectively undermines it.
We now turn to examine The Social Theory in more detail, but not before noting that McKeown’s central argument – that medical intervention could not take the credit for the decline in tuberculosis – is much less compelling than it might appear. The bacillus that causes tuberculosis spreads itself around by the simple expedient of irritating the airways of the lungs of those infected, causing them to cough and sneeze. Thus millions of droplets of lung secretions are scattered into the atmosphere every time a patient with tuberculosis coughs, some of which will contain tubercle bacilli which, if inhaled by those nearby, will spread the infection. This dissemination of infection will clearly be interrupted if patients with tuberculosis are isolated in a sanatorium with others similarly infected until they either die, or, as happened to Bradford Hill, are cured by the admittedly crude methods available prior to the introduction of streptomycin. McKeown, it seems, overlooked, presumably deliberately, this important point, for as a historian subsequently observed:
McKeown mis-stated, or failed to understand, the point demonstrated with brilliant clarity in the classic book The Prevention of Tuberculosis published in 1908, namely that the effect of placing consumptive patients in poor law infirmaries was to separate them from the general populace and to restrict the spread of the disease – the proportion of consumptive patients thus segregated corresponded closely to the progressive rate of decline of tuberculosis in England and Wales.
Certainly, rising living standards and particularly improvements in housing would have contributed to tuberculosis’s decline, but ‘medical intervention’ – the identification of those with tuberculosis by examining their sputum and their subsequent incarceration in a sanatorium – was also very important. This might not be a conventional view of ‘medical intervention’, but it was instigated and co-ordinated by doctors with the clear intention of reducing the spread of the disease, so medical intervention it must be.6
When the slightest breath of scepticism is sufficient to undermine McKeown’s argument, perhaps a similar attitude will prove just as damaging to The Social Theory he instigated. We start with ‘The Rise and Fall of Heart Disease’, the bitterest intellectual controversy of post-war medicine.