CHAPTER FIFTEEN
THE 1918 INFLUENZA PANDEMIC, like many other influenza pandemics, came in waves. The first spring wave killed few, but the second wave would be lethal. Three hypotheses can explain this phenomenon.
One is that the mild and deadly diseases were caused by two entirely different viruses. This is highly unlikely. Many victims of the first wave demonstrated significant resistance to the second wave, which provides strong evidence that the deadly virus was a variant of the mild one.
The second possibility is that a mild virus caused the spring epidemic, and that in Europe it encountered a second influenza virus. The two viruses infected the same cells, “reassorted” their genes, and created a new and lethal virus. This could have occurred and might also explain the partial immunity some victims of the first wave acquired, but at least some scientific evidence directly contradicts this hypothesis, and most influenza experts today do not believe this happened.
The third explanation involves the adaptation of the virus to man.
In 1872 the French scientist C. J. Davaine was examining a specimen of blood swarming with anthrax. To determine the lethal dose he measured out various amounts of this blood and injected it into rabbits. He found it required ten drops to kill a rabbit within forty hours. He drew blood from this rabbit and infected a second rabbit, which also died. He repeated the process, infecting a third rabbit with blood from the second, and so on, passing the infection through five rabbits.
Each time he determined the minimum amount of blood necessary to kill. He discovered that the bacteria increased in virulence each time, and after going through five rabbits a lethal dose fell from 10 drops of blood to 1/100 of a drop. At the fifteenth passage, the lethal dose fell to 1/40,000 of a drop of blood. After twenty-five passages, the bacteria in the blood had become so virulent that less than 1/1,000,000 of a drop killed.
This virulence disappeared when the culture was stored. It was also specific to a species. Rats and birds survived large doses of the same blood that killed rabbits in infinitesimal amounts.
Davaine’s series of experiments marked the first demonstration of a phenomenon that became known as “passage.” This phenomenon reflects an organism’s ability to adapt to its environment. When an organism of weak pathogenicity passes from living animal to living animal, it reproduces more proficiently, growing and spreading more efficiently. This often increases virulence.
In other words, it becomes a better and more efficient killer.
Changing the environment even in a test tube can have the same effect. As one investigator noted, a strain of bacteria he was working with turned deadly when the medium used to grow the organism changed from beef broth to veal broth.
But the phenomenon is complex. The increase in killing efficiency does not continue indefinitely. If a pathogen kills too efficiently, it will run out of hosts and destroy itself. Eventually its virulence stabilizes and even recedes. Especially when jumping species, it can become less dangerous instead of more dangerous. This happens with the Ebola virus, which does not normally infect humans. Initially Ebola has extremely high mortality rates, but after it goes through several generations of human passages, it becomes far milder and not particularly threatening.
So passage can also weaken a pathogen. When Pasteur was trying to weaken or, to use his word, “attenuate” the pathogen of swine erysipelas, he succeeded only by passing it through rabbits. As the bacteria adapted to rabbits, it lost some of its ability to grow in swine. He then inoculated pigs with the rabbit-bred bacteria, and their immune systems easily destroyed it. Since the antigens on the weak strain were the same as those on normal strains, the pigs’ immune systems learned to recognize—and destroy—normal strains as well. They became immune to the disease. By 1894, veterinarians used Pasteur’s vaccine to protect 100,000 pigs in France; in Hungary over 1 million pigs were vaccinated.
The influenza virus is no different in its behavior from any other pathogen, and it faces the same evolutionary pressures. When the 1918 virus jumped from animals to people and began to spread, it may have suffered a shock of its own as it adapted to a new species. Although it always retained hints of virulence, this shock may well have weakened it, making it relatively mild; then, as it became better and better at infecting its new host, it turned lethal.
Macfarlane Burnet won his Nobel Prize for work on the immune system, but he spent the bulk of his career investigating influenza, including its epidemiological history. He noted an occasion when passage turned a harmless influenza virus into a lethal one. A ship carrying people sick with influenza visited an isolated settlement in east Greenland. Two months after the ship’s departure, a severe influenza epidemic erupted, with a 10 percent mortality rate; 10 percent of those with the disease died. Burnet was “reasonably certain that the epidemic was primarily virus influenza” and concluded that the virus passed through several generations—he estimated fifteen or twenty human passages—in mild form before it adapted to the new population and became virulent and lethal.
In his study of the 1918 pandemic, Burnet concluded that by late April 1918 “the essential character of the new strain seems to have been established.” He continued, “We must suppose that the ancestral virus responsible for the spring epidemics in the United States passaged and mutated…. The process continued in France.”
Lethality lay within the genetic possibilities of this virus; this particular mutant swarm always had the potential to be more pestilential than other influenza viruses. Passage was sharpening its ferocity. As it smoldered in the roots, adapting itself, becoming increasingly efficient at reproducing itself in humans, passage was forging a killing inferno.
On June 30, 1918, the British freighter City of Exeter docked at Philadelphia after a brief hold at a maritime quarantine station. She was laced with deadly disease, but Rupert Blue, the civilian surgeon general and head of the U.S. Public Health Service, had issued no instructions to the maritime service to hold influenza-ridden ships. So she was released.
Nonetheless, the condition of the crew was so frightening that the British consul had arranged in advance for the ship to be met at a wharf empty of anything except ambulances whose drivers wore surgical masks. Dozens of crew members “in a desperate condition” were taken immediately to Pennsylvania Hospital where, as a precaution against infectious disease, a ward was sealed off for them. Dr. Alfred Stengel, who had initially lost a competition for a prestigious professorship at the University of Pennsylvania to Simon Flexner but who did get it when Flexner left, had gone on to become president of the American College of Physicians. An expert on infectious diseases, he personally oversaw the sailors’ care. Despite Stengel’s old rivalry with Flexner, he even called in Flexner’s protégé Paul Lewis for advice. Nonetheless, one after another, more crew members died.
They seemed to die of pneumonia, but it was a pneumonia accompanied, according to a Penn medical student, by strange symptoms, including bleeding from the nose. A report noted, “The opinion was reached that they had influenza.”
In 1918 all infectious disease was frightening. Americans had already learned that “Spanish influenza” was serious enough that it had slowed the German offensive. Rumors now unsettled the city that these deaths too came from Spanish influenza. Those in control of the war’s propaganda machine wanted nothing printed that could hurt morale. Two physicians stated flatly to newspapers that the men had not died of influenza. They were lying.
The disease did not spread. The brief quarantine had held the ship long enough that the crew members were no longer contagious when the ship docked. This particular virulent virus, finding no fresh fuel, had burned itself out. The city had dodged a bullet.
By now the virus had undergone numerous passages through humans. Even while medical journals were commenting on the mild nature of the disease, all over the world hints of a malevolent outbreak were appearing.
In London the week of July 8, 287 people died of influenzal pneumonia, and 126 died in Birmingham. A physician who performed several autopsies noted, “The lung lesions, complex or variable, struck one as being quite different in character to anything one had met with at all commonly in the thousands of autopsies one has performed during the last twenty years. It was not like the common broncho-pneumonia of ordinary years.”
The U.S. Public Health Service’s weekly Public Health Reports finally took notice, at last deeming the disease serious enough to warn the country’s public health officials that “an outbreak of epidemic influenza…has been reported at Birmingham, England. The disease is stated to be spreading rapidly and to be present in other locations.” And it warned of “fatal cases.”
Earlier some physicians had insisted that the disease was not influenza because it was too mild. Now others also began to doubt that this disease was influenza—but this time because it seemed too deadly. Lack of oxygen was sometimes so severe that victims were becoming cyanotic—part or all of their bodies were turning blue, occasionally a very dark blue.
On August 3 a U.S. Navy intelligence officer received a telegram that he quickly stamped SECRET and CONFIDENTIAL. Noting that his source was “reliable,” he reported, “I am confidentially advised…that the disease now epidemic throughout Switzerland is what is commonly known as the black plague, although it is designated as Spanish sickness and grip.”
Photographic Insert
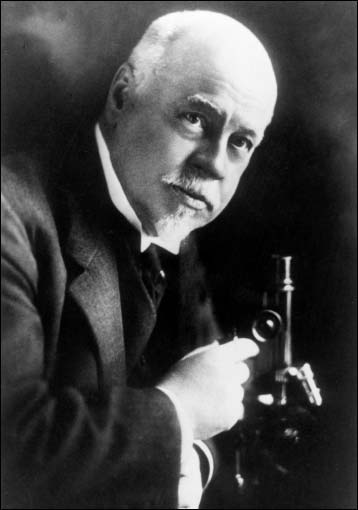
1. William Henry Welch, the single most powerful individual in the history of American medicine and one of the most knowledgeable. A wary colleague said he could “transform men’s lives almost with the flick of a wrist.” When Welch first observed autopsies of influenza victims, he worried, “This must be some new kind of infection or plague.”
2. Welch and John D. Rockefeller Jr. (on the right) together created the Rockefeller Institute for Medical Research (now Rockefeller University), arguably the best scientific research institution in the world. Simon Flexner (on the left), a Welch protégé, was the institute’s first head; he once said that no one could run an institution unless he had the capacity to be cruel.
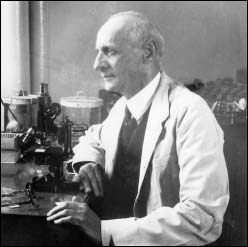
3. Flexner brought the mortality rate for the most common bacterial meningitis down to 18 percent in 1910 without antibiotics. Today, with antibiotics, the mortality rate is 25 percent.

4. A dense jungle-like growth of epithelial cells covers a healthy mouse trachea.
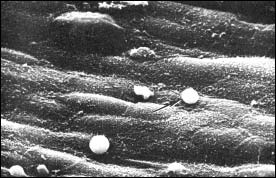
5. Only seventy-two hours after infection the influenza virus transforms the same area into a barren and lifeless desert. White blood cells are patrolling the area, too late.
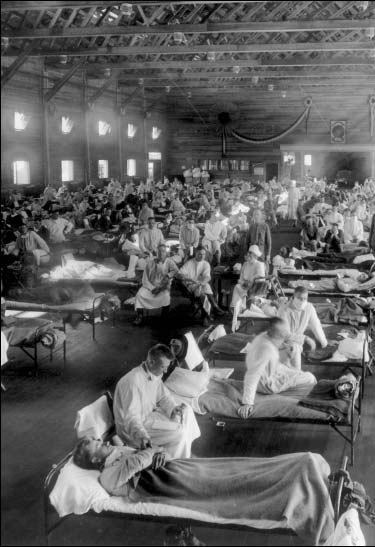
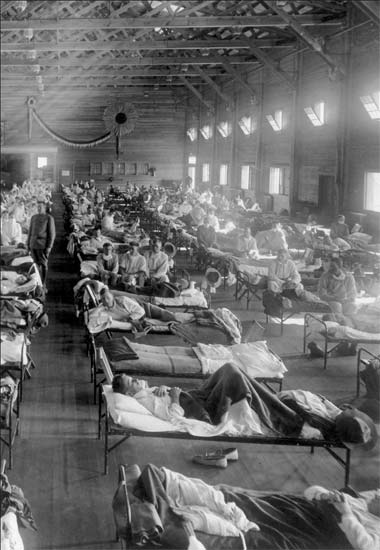
6. The virus swept first through military bases, where men were jammed together despite the objections of Welch and Army Surgeon General William Gorgas. This is an army emergency hospital, probably a ward for convalescents.
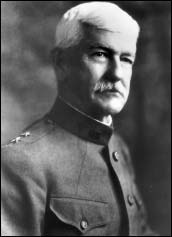
7. Army Surgeon General William Gorgas was determined that this would be the first war in which fewer American soldiers died of disease than from combat.

8. Rupert Blue, the civilian surgeon general and head of the U.S. Public Health Service, was a master bureaucrat but failed to heed warnings of, seek advance information about, or prepare for the epidemic.
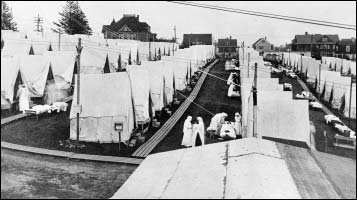
9. Massachusetts was the first state to suffer huge numbers of civilian deaths. This is a hospital in Lawrence.
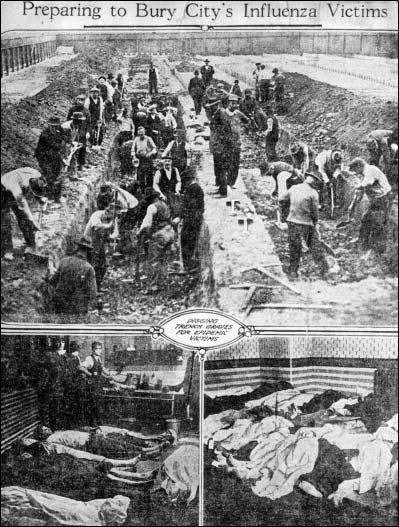
10. I n Philadelphia the number of dead quickly overwhelmed the city’s ability to handle bodies. It was forced to bury people, without coffins, in mass graves and soon began using steam shovels to dig the graves.
11.
12.
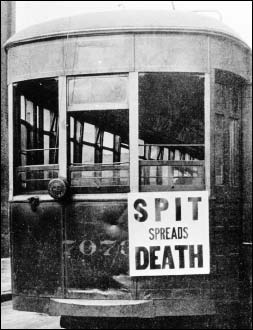
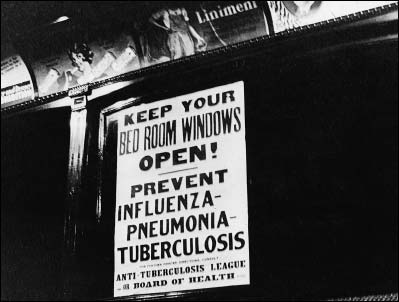
Posters and handouts spread warnings and advice. They also spread terror.

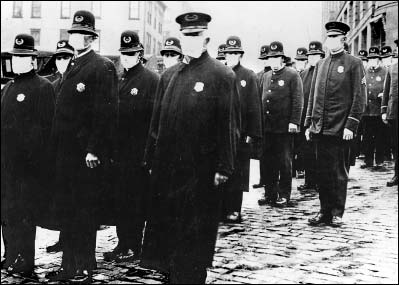
13. The two messages in this photograph—the policeman’s protective mask and patriotism—epitomized a conflict of interest in public officials.
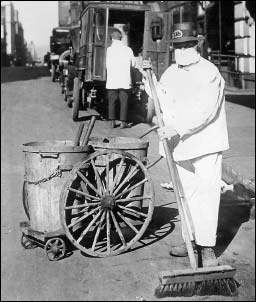
14. All New York City workers wore masks. Note the absence of traffic on the street and pedestrians on the sidewalk. The same silent streets were seen everywhere. In Philadelphia a doctor said, “The life of the city had almost stopped.”
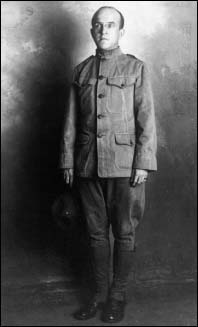
15. Oswald T. Avery as a private, when the Rockefeller Institute became Army Auxiliary Laboratory Number One.
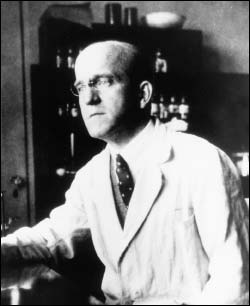
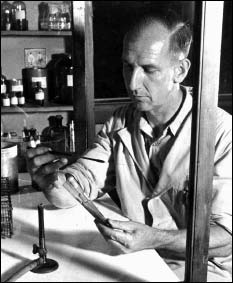
16. A very in later life. Persistent and tenacious, he said, “Disappointment is my daily bread. I thrive on it.” Welch asked him to find the cause of influenza. His work on influenza and pneumonia would ultimately lead him to one of the most important scientific discoveries of the twentieth century.

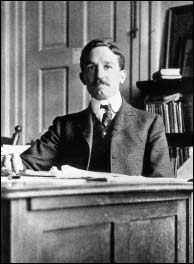
17. William Park, who made New York City’s municipal laboratories a premier research institution. His rigorous scientific discipline, when teamed with the more creative temperament of Anna Williams [below], led to dramatic advances, including the development of a diphtheria antitoxin still in use. The National Academy of Sciences hoped they could develop a serum or vaccine for influenza.

18. Anna Wessel Williams was probably the leading female bacteriologist in the world. A lonely woman who never married, she told herself she would “rather [have] discontent than happiness through lack of knowledge,” and wondered “if it would be worthwhile to make the effort to have friends and if so how I should go about it.” From her earliest memories, she dreamed “about going places. Such wild dreams were seldom conceived by any other child.”

19. The virus moved inexorably across the country. Here navy nurses and doctors await the onslaught.


20. Military commanders tried to protect healthy men; at Mare Island in San Francisco sheets were hung in barracks to screen men from each other’s breathing.

21. In most cities all public meetings were banned, all public gathering places—churches, schools, theaters, and saloons—closed. Most churches simply canceled services but this one in California met outdoors, a technical violation of the closing order but a response to the congregation’s need for prayer.
22. Rufus Cole, the Rockefeller Institute scientist who had led the successful effort to develop a pneumonia vaccine and treatment just before the outbreak of the epidemic. He also made the Rockefeller Institute Hospital a model for the way clinical research is conducted, including at the National Institutes for Health.

23.
24.

25.
Seattle, like many other places, became a masked city. Red Cross volunteers made tens of thousands of masks. All police wore them. Soldiers marched through the city’s downtown wearing them.

26. More than one scientist called Paul A. Lewis “the brightest man I ever met.” As a young investigator in 1908 he proved polio was caused by a virus and devised a vaccine that was 100 percent effective in protecting monkeys. It would be half a century before a polio vaccine could protect man. He too was one of the prime investigators searching for the cause of influenza, and a cure or preventative. Ultimately his ambition to investigate disease would cost him his life.
27. In the late 1920s Richard Shope, Lewis’s protégé, unearthed a crucial clue in the search for the cause of influenza. While Lewis went to Brazilian jungles to investigate yellow fever, Shope continued his pursuit of influenza. He was the first to prove a virus caused the disease.
Many histories of the pandemic portray the eruption of deadly disease—the hammer blow of the second wave—as sudden and simultaneous in widely separated parts of the world, and therefore deeply puzzling. In fact the second wave developed gradually.
When water comes to a boil in a pot, first an isolated bubble releases from the bottom and rises to the surface. Then another. Then two or three simultaneously. Then half a dozen. But unless the heat is turned down, soon enough all the water within the pot is in motion, the surface a roiling violent chaos.
In 1918 each initial burst of lethality, isolated though it may have seemed, was much like a first bubble rising to the surface in a pot coming to boil. The flame may have ignited in Haskell and set off the first burst. The outbreak that killed 5 percent of all French recruits at one small base was another. Louisville was still another, as were the deaths on the City of Exeter and the outbreak in Switzerland. All these were bursts of lethal disease, violent bubbles rising to the surface.
Epidemiological studies written relatively soon after the pandemic recognized this. One noted that army cantonments in the United States saw “a progressive increase in cases reported as influenza beginning with the week ending August 4, 1918, and of the influenzal pneumonia cases beginning with the week ending August 18. If this was really the beginning of the great epidemic wave we should expect that if these series of data were plotted out on a logarithmic scale the increase from week to week would plot out as a straight line following the usual logarithmic rise of an epidemic curve…. This condition is substantially fulfilled with the curve of rise plotting out on logarithmic paper as a practically straight line.”
The report also found “definite outbreaks of increasing severity” occurring during the summer in both the United States and Europe, which “indistinguishably blend with the great Fall wave.”
In early August the crew of a steamship proceeding from France to New York was hit so hard with influenza “that all of the seamen were prostrate on it and it had to put into Halifax,” according to an epidemiologist in Gorgas’s office, where it remained until enough crew members were well enough to proceed to New York.
On August 12 the Norwegian freighter Bergensfjord arrived in Brooklyn after burying four men at sea, dead of influenza. It carried two hundred people still sick with the disease; ambulances transported many of them to a hospital.
Royal Copeland, head of the New York City health department, and the port health officer jointly stated there was “not the slightest danger of an epidemic” because the disease seldom attacks “a well-nourished people.” (Even had he been right, a study by his own health department had just concluded that 20 percent of city schoolchildren were malnourished.) He took no action whatsoever to prevent the spread of infection.
A navy bulletin warned of two steamships from Norway and one from Sweden arriving in New York City with influenza cases aboard on August 14 and 15. On August 18, New York papers described outbreaks on board the Rochambeau and Nieuw Amsterdam; men from both ships had been taken to St. Vincent’s Hospital.
On August 20 even Copeland conceded that influenza, though mild and—he claimed—certainly not in epidemic form, was present in the city. The lethal variant of the virus was finding its home in humans. Now, almost simultaneously, on three continents separated by thousands of miles of ocean—in Brest, in Freeport, Sierra Leone, and in Boston—the killing, rolling boil was about to begin.
Nearly 40 percent of the two million American troops who arrived in France—791,000 men—disembarked at Brest, a deepwater port capable of handling dozens of ships simultaneously. Troops from all over the world disembarked there. Brest had already seen a burst of influenza in the spring as had many other cities, albeit as in most of those other places that influenza had been mild. The first outbreak with high mortality occurred in July, in a replacement detachment of American troops from Camp Pike, Arkansas. They occupied an isolated camp and the outbreak initially seemed contained. It was not. By August 10, the same day the British army declared the influenza epidemic over, so many French sailors stationed at Brest were hospitalized with influenza and pneumonia that they overwhelmed the naval hospital there—forcing it to close. And the death rate among them began soaring.
The August 19 New York Times took note of another outbreak: “A considerable number of American negroes, who have gone to France on horse transports, have contracted Spanish influenza on shore and died in French hospitals of pneumonia.”
Within another few weeks all the area around Brest was in flames. American troops continued pouring into and then out of the city, mixing with French troops also training in the vicinity. When soldiers of both armies left the vicinity, they dispersed the virus en masse.
Freetown, Sierra Leone, was a major coaling center on the West African coast, servicing ships traveling from Europe to South Africa and the Orient. On August 15 the HMS Mantua arrived there with two hundred crew suffering from influenza. Sweating black men loaded tons of coal into her, guided by several crew.
When the laborers returned to their homes, they carried more than their wages. Soon influenza spread through the force of men who coaled the ships. And this influenza was not mild. On August 24, two natives died of pneumonia while many others were still sick.
On August 27, the HMS Africa pulled into port. She too needed coal, but five hundred of the six hundred laborers of the Sierra Leone Coaling Company did not report to work that day. Her crew helped coal her, working side by side with African laborers. She carried a crew of 779. Within a few weeks, nearly six hundred were sick. And fifty-one were dead—7 percent of the entire crew died.
The transport HMS Chepstow Castle, carrying troops from New Zealand to the front, coaled at Freetown on August 26 and 27; within three weeks, out of her 1,150 men, influenza struck down nine hundred of them. The death toll on her was thirty-eight.
The Tahiti coaled at the same time; sixty-eight men aboard her died before she reached England, the same day as the Chepstow Castle. After docking, crew of the two ships suffered eight hundred more cases and 115 more deaths.
In Sierra Leone itself, officials soon after estimated that influenza killed 3 percent of the entire African population, nearly all of them dying within the next few weeks. More recent evidence suggests that the death toll was most likely considerably more than that, possibly double that figure—or higher.
Across the Atlantic, at Commonwealth Pier in Boston, the navy operated a “receiving ship.” The name was a misnomer. It was actually a barracks where as many as seven thousand sailors in transit ate and slept in what the navy itself called “grossly overcrowded” quarters.
On August 27, two sailors reported to sick bay with influenza. On August 28, eight more sailors reported ill. On August 29, fifty-eight men were admitted.
As in Brest and Freetown and aboard ship, men began to die. Fifty of the men were quickly transferred to the Chelsea Naval Hospital, where Lieutenant Commander Milton Rosenau and his young assistant Lieutenant John J. Keegan, worked.
The sailors were in better than good hands. While Keegan would later become dean of the University of Nebraska Medical School, Rosenau was one of the giants of the day. Strong, solid, and thick-necked, he looked as intimidating and determined as a wrestler staring down an opponent. Yet he was uniformly polite and supportive, and people enjoyed working under him. A prime mover in creating the U.S. Public Health Service Hygienic Laboratory and later the president of the Society of American Bacteriologists, he was best known for his textbook, Preventive Medicine and Hygiene, which was referred to as “The Bible” for both army and navy medical officers. Only a few weeks earlier, he had met with Welch, Gorgas, and Vaughan to discuss how to prevent or contain any new epidemic.*
Rosenau and Keegan immediately isolated the men and did everything possible to contain the disease, working backward from each victim to trace and isolate people with whom the patients had had contact. But the disease was too explosive. They turned their attention to bacteriological analysis, seeking the pathogen so they could prepare a vaccine or serum. Their findings did not satisfy them, and within a few weeks they began using human volunteers from the navy brig in the first experiments in the world to determine if a virus caused the disease.
Long before that any hopes of containing the disease had collapsed. On September 3 a civilian suffering from influenza was admitted to the Boston City Hospital. On September 4 students at the Navy Radio School at Harvard, in Cambridge across the Charles River from Boston proper, fell ill.
And then came Devens.