chapterthree
Greening the Growing Fetus
It was only a generation ago that we thought the growing fetus was entirely protected by the placenta. At that time, we had little idea that toxins, including drugs and alcohol, could reach the growing child. We have since learned that many do.
I once read in a dusty old book that pregnancy was one of the only cures for lead poisoning. In it, they described how a pregnant mother could watch her teeth regain their normal colour as the baby-to-be absorbed the lead.
We learned the hard way that the placenta wasn’t much of a barrier at all. One of the bitterest lessons came in the form of the sedative thalidomide, marketed to help with the effects of morning sickness during pregnancy in the late 1950s and 1960s. Soon after it appeared, doctors began to notice a startling rise in severe birth defects in women who had used the drug during pregnancy. It remained available in Canada months after it was removed from use in West Germany and the U.K.
The U.S. was protected from the worst of this disaster by a Canadian woman, scientist, and medical doctor, Dr. Frances Oldham Kelsey. She had just begun working for the FDA at the time and refused to give the drug her blessing for use in the United States despite “relentless pressures” from the drug’s manufacturer. She insisted that, despite its popularity in England, there was not enough evidence to prove it was safe for use during pregnancy. This British Columbia–born doctor was tenacious in the face of pressure, in part because she had participated in research earlier in her career that demonstrated some drugs could cross the placenta and affect unborn children.
The Research
The placenta is a mother’s protective impulse turned physical. The placenta starts developing at the same time as the embryo. In the fifth week of gestation, the umbilical cord develops and attaches the embryo’s abdomen to the placenta. Inside the placenta, the baby is surrounded by amniotic fluid held within the amniotic sac. The outer layer of the amniotic sac is part of the placenta, and the placenta attaches to the uterus. The amniotic fluid is made by the mother’s blood plasma and is absorbed by the fetus’s skin.

The placenta serves two primary functions. One is to deliver nutrients from the mother’s blood to the fetus and produce hormones, including estrogen and progesterone. These hormones are used for the fetus’s development and to help prepare the mother for delivery and lactation. The other function is protective. It protects the blood of the child from the blood of the mother. This is how a child can have a different blood type from the mother. It is also how the baby is protected from certain diseases and even some toxins. The placenta also allows waste from the baby’s developing metabolism, such as carbon dioxide, to move back through the umbilical cord to the mother’s bloodstream for clean-up.
Enter into this picture of biological bliss the toxins found in the environment today and things get more complicated. Yet our basic biology still wants to protect us and our growing babies. We can help this biological impulse by reducing our exposure to toxins, minimizing drug use during pregnancy, and providing good, healthy nourishment, which helps keep our natural systems working as effectively as possible.
“Forbidden” Foods That Needn’t Be Forsaken
It isn’t that surprising to me to discover that the placenta is actually well adapted to protect the developing baby from diseases, including most viruses and food-borne illnesses. Thus, contracting E. coli from a fast-food hamburger while pregnant is likely to be very uncomfortable, but it isn’t likely to cause harm to the baby. There are exceptions, however, and these exceptions are at the root of why North Americans are relatively uptight about certain foods in pregnancy compared to their European peers. The exceptions include Listeria monocytogenes (often associated with soft, raw cheeses and lunch meats) and Salmonella enterica (associated with undercooked meat and eggs), both of which can cause harm in the unborn fetus.
The risk, however, is extremely low. A scientific paper published in the Canadian Family Physician explained that women need not avoid most of the foods we’ve come to fear, such as those soft cheeses, as long as they are from a safe and reputable source. Foods that can be enjoyed with caution include
- Runny eggs. The take-away on undercooked foods, such as runny eggs, and contracting salmonella is that the risk is minuscule — an average of 1 in 20,000 — and that pregnant women are at no greater risk than the rest of the non-pregnant population. The risk of contracting salmonella from undercooked eggs is considered even smaller from organic, pastured eggs. Cooking the egg thoroughly removes the risk.
- Raw fish and other seafood. The study authors say go ahead and eat sushi or undercooked seafood as long as it is from a reputable establishment, has been stored properly, and is consumed fresh. Any infections that might happen from seafood tend to be limited to the GI tract, so while they may be uncomfortable, they won’t harm the fetus. The authors do caution against the consumption of high-mercury fish and shellfish, including tuna.
- Raw honey. The authors also state that there is no known risk to the fetus from honey that might contain botulinum toxin and that the average healthy women need not avoid raw honey during pregnancy.
All in all, most foods are safe for women to consume during pregnancy as long as they are from safe, reputable sources. When I was pregnant, I chose to eat the way I always have: fried eggs with runny yellows; raw, non-homogenized milk; wild-caught salmon; and unpasteurized honey. I do my utmost to be sure about my sources, finding products that are organic, locally sourced, pasture-raised, or wild-caught. You can learn what to look for in healthy sources in the Organic-ize Your Diet section in the previous chapter.
Why the Placenta Doesn’t Better Protect Baby from Toxins
Just as it intuitively makes sense that the placenta would have evolved to protect a fetus from most illnesses, I’m also not surprised that the placenta is unable to better protect a baby from many of the 42 billion pounds of industrial chemicals imported or manufactured every day in North America. Perhaps one day the placenta will evolve to parse the heavy metals from the calcium before passing them on to the baby-to-be, but as of now most toxins cross into the developing fetus. Some, like mercury, concentrate in the baby-to-be. The end result is that a baby born today in Canada will be born pre-polluted with more than 130 different known or suspected toxins.
Your baby is not alone in her exposure levels: we all share the air and the water. Indeed, some of the most pristine areas of the world — like remote regions of Arctic Canada — have the highest concentrations of industrial toxins. These are areas thousands of kilometres from the nearest factory or coal-powered plant, but have nevertheless become receptacles of known poisons thanks to trade winds and ocean currents. There are things that parents can do to protect our children and that we can all do to protect our future generations from the worst of these toxins. It helps to know when a child is the most vulnerable and what toxins are of greatest concern.
The When: Critical Windows of Exposure
When I was pregnant, I had a day-by-day pregnancy journal that apprised me of what was happening in my womb. One day, near the end of the first month, the book announced, “By the end of this month, your baby will have completed a period of growth that involves the greatest size and physical changes of its lifetime. In five days, it will be 10,000 times larger than the fertilized egg, although in actuality not much bigger than a grain of rice.” And on day 140, it said, “If your baby is a female, her uterus is completely formed and has just undergone its most rapid period of growth.”
All healthy babies-to-be develop along similar lines and similar time frames (give or take a few days or weeks). The developing baby might have a bit more of a particular nutritional need or be especially affected by exposures to toxins or drugs, depending on what is happening at that moment with his development. One example of this is with thalidomide, the drug mentioned earlier that was prescribed as a treatment for morning sickness. When it was given to women in the fourth and ninth weeks of pregnancy, the drug caused severe birth defects, while women who took it outside that time experienced little risk of those same effects.
Baby teeth might also hold a key to understanding more about windows of exposure and the effects of different environmental toxins. Teeth form rings as they grow — kind of like trees — that reveal daily information about the totality of health-affecting exposures known as the “exposome.” By studying teeth, we can better understand the relationship between particular exposures at particular times and the resultant health outcomes. There are studies underway now using teeth biomarkers to understand more about causes of childhood leukemia — which is not genetic and, thus, is considered environmental — as well as adult chronic illnesses such as Alzheimer’s and heart disease. This research can help scientists, doctors, and parents-to-be figure out the human effects of the increased number of chemicals we are exposed to and how to prioritize protective actions during pregnancy.
The What: Chemicals to Be Avoided Prenatally
Industrial chemicals have made their way into nearly every aspect of modern life, from our shampoo to our sheets. Understanding what things are called, where they are lurking, and why they are bad helps us in avoiding them. It also helps parents understand why it’s worth it to buy an organic apple or avoid a ripped sofa.
- Heavy metals such as arsenic, lead, cadmium, and mercury are a problem because they can be stored in our bodies and easily pass through the placenta, where they can particularly affect the developing brain. They are found in beauty care products and in the fatty tissue of certain animals, in particular fish. Luckily there are safer options, such as greener beauty care and eating smaller, wild-caught fish.
- Persistent organic pollutants (POPs) are dangerous because they can be very toxic and long-lasting. In particular they can affect the hormones and the developing brain, and many have been linked with cancers. POPs include certain pesticides (such as DDT and hexachlorabenzene), flame retardants (including PBDEs and Tris), water- and stain-resistors (such as PFOA and PFOS), and by-products from industrial processes (such as dioxin and PCBs). These can end up in the food chain by being added directly as a pesticide or indirectly through contamination of the water and flesh of other animals. You can reduce your exposure to POPs by making those healthy food choices discussed in the last chapter, and also by greening your home and beauty care routine.
- Volatile organic compounds (VOCs) readily release into the environment and can cause a range of health concerns from headaches to organ damage after they are inhaled and make their way into your bloodstream. They are commonly found in paints, solvents, highway traffic, cigarette smoke, building materials, household cleaning products, and beauty care items. There are many ways to avoid the worst of the VOCs — for instance by avoiding cigarette smoke and greening your home. Keep reading to learn more.
- Pesticides aren’t always so persistent, but can still be harmful because of their pervasiveness. Their residues can be found in most conventionally grown foods and most of our drinking water, and they can be added to products such as antibacterial hand soaps and cleaning products. Learning to read labels can help you avoid these unwanted ingredients.
- • Plastics in almost all cases have the ability to interfere with developing hormones. The worst of the plasticizers, including phthalates, BPA, melamine, PVC, and polystyrene, can largely be avoided by keeping them away from your kitchen and not using them in food preparation or storage.
Learn more about these chemicals and where they are found in the Green Mama-to-Beware appendix.
More What: Drugs and Exposures to Approach with Caution During Pregnancy
When my grandmother was pregnant, it was possible that a doctor would enter the room smoking a cigarette, and women were even allowed to smoke in some maternity wards. Indeed, a stiff drink to wash down the diet pills prescribed by the doctor wasn’t uncommon then either.
We’ve come a long way from those times, but many of the substances we encounter in our daily living can still harm a baby-to-be. Some of these, like tobacco, are better understood, but others, like acetaminophen, we are just beginning to understand. We do know enough to be cautious about the following commonly used drugs.
The chemicals in cigarettes are among the most studied prenatal toxins, and e-cigarettes may be just as bad. As recently as 2007, it was reported that up to 15 percent of pregnant women smoke, and many millions more are exposed to secondhand smoke, which may be just as dangerous. Its detrimental effects to a growing baby-to-be and even future grand-babies-to-be include miscarriage, reduced birth weight, and an increased risk for chronic diseases, respiratory disease, asthma, allergies, cancer, cognitive impairment, and behavioural disorders, including aggression, ADHD, major depression disorder, substance abuse, and other externalizing disorders. Cigarette smoke contains more than 4,000 chemicals, of which more than 40 are known carcinogens and at least some of which — such as nicotine — do cross the placenta, where they can show up in higher concentrations in the baby than in the mother.
A number of my friends and family members have finally kicked their smoking habits with the help of e-cigarettes. While less is known about the effects of e-cigarettes on health because there has not been time to do adequate research, early studies suggest that they may not be much healthier than regular old cigarettes. The FDA published a review in 2014 cautioning against the many known and potential toxins that they contain and can release in their vapours, including nitrosamines, aldehydes, metals, VOCs, nanoparticles, and nicotine. Indeed, the class one — known human carcinogen — formaldehyde can be up to 15 times higher in e-cig vapour than in cigarette smoke. Researchers and health organizations caution that even the second-hand vapours should not be considered safe for fetuses, babies, or children.
As with many toxins, some researchers say there is no safe level of alcohol when it comes to protecting the fetus. Your doctor will likely say this as well, for two reasons. One, it is known that fetal alcohol spectrum disorder (FASD) can cause irreparable harm to a baby, including physical deformities, mental handicaps, learning disabilities, and behavioural disorders. Two, because there is simply no ethical way to do controlled experiments involving alcohol and pregnant women.
We don’t know much about what a moderate alcohol level does to the fetus. It is during the first trimester that alcohol consumption is most likely to lead to physical deformities. We also know from sibling comparison studies that even light to moderate drinking can lead to some behavioural problems.
Can You Tox-Out Toxins?
Can we detoxify ourselves? That’s the question behind ToxIn ToxOut, the sequel to Bruce Lourie and Rick Smith’s bestselling book Slow Death by Rubber Duck. In it, the intrepid authors exposed themselves to numerous everyday items: BPA and pesticides in foods, phthalates and fire retardants found in furniture, and triclosan and phthalates in skincare products. All the while, they tested their blood and urine and found, yup, the levels of toxins in their bodies increased noticeably. Then they tried to figure out if it was possible to get these toxins out of their bodies, and how.
In short, “A lot of detox therapies just aren’t that effective,” warns Smith. Chelation was one of the “big hitter” techniques they tested and found could work to reduce some of those longer-lasting toxins such as aluminum, mercury, and lead. Chelation involves using an intravenous agent that travels through the bloodstream, grabbing onto minerals and metals and binding with them. These bound minerals and metals then move through the digestive system and out of the body through the urine. Doctors have used chelation to help treat diseases including arthritis, autism, fibromyalgia, and Parkinson’s, and even as an alternative to heart bypass surgery. It can be risky, though, because chelation binds with minerals as well as heavy metals. Chelation might be something to consider if you are having trouble conceiving or when preparing for a pregnancy (in consultation with a medical professional) about a year before trying to get pregnant. Chelation is not on the menu for someone who is already pregnant, within the few months leading up to conception, or breastfeeding.
Everyday detoxification methods for children and mamas-to-be that were proven to work include sweating, pooping, peeing, and all of the things tied to creating “beautiful pathways of elimination,” as nutritionist Margaret Floyd Barry puts it. They also tested and confirmed that you could successfully limit and lower toxin levels in children by doing all those great Green Mama things, like feeding them fresh organic food, improving indoor air quality, getting children outside more, and encouraging them to exercise. The best thing, of course, “is [to] try to shield them from these chemicals in the first place,” says Smith.
There is another complexity in all of this: FASD seems to be affected by genetics. That’s right; alcohol consumption of the mother affects some babies more than others. The genetics of both mother and child seem to play a part in this.
Over-the-counter products for pain relief can also be toxic to the fetus. For many years, the go-to medicine for pregnant women was acetaminophen, better known as Tylenol. That changed in 2014, when the Danish National Cohort Study looked at 64,322 live births and found that mothers who used acetaminophen during pregnancy were more likely to have children with ADHD, ADHD-like behaviours, and hyperkinetic disorders. The more frequent the use, the higher the chance of the outcome. No trimesters were safe, and exposure in more trimesters also increased risk.
Other over-the-counter pain relievers seem to be no safer. Doctors and midwives have warned against the use of painkillers such as ibuprofen, diclofenac, and other non-steroid anti-inflammatory drugs (NSAIDs) because they more than double the risk of miscarriage in the first 20 weeks and are associated with low birth weights when used in the second trimester and asthma when used in the second or third trimester. You can find other more natural remedies to help with occasional pain in the Natural Pregnancy Handbook following this chapter.
Caffeine is one of the most popular mood-altering drugs. It can help a person feel more awake and energetic by stimulating a number of hormones in the brain, including dopamine, and it blocks adenosine, a brain chemical associated with feelings of drowsiness. The more caffeine a person drinks, the more a person requires. Unfortunately, caffeine is not so good for your baby. It’s been shown to cross the placenta to the baby-to-be, where the baby’s developing metabolism is ill-equipped to handle the effects, which include keeping him awake. Caffeine has been linked to reduced fertility in men and women, an increased chance of miscarriage, and low birth weights, and it may even be linked to preterm birth and some birth defects. In short, scientists say there is no proven safe limit of caffeine use during pregnancy.
Most healthcare practitioners advise that you reduce your levels to below 200 mg a day while pregnant. That equals one cup of organic coffee, up to a few cups of black or green tea, or a couple of pieces of dark chocolate. I’d suggest going decaf (but read about the importance of going organic when you do that, or try decaffeinating your own organic tea at home). Don’t drink your tea or coffee on an empty stomach either; it’s far better for your blood sugar (and your baby) to drink it after one of those healthy, blood-sugar-smart meals discussed in the previous chapter.
Avoid unnecessary ultrasounds. Ninety-nine percent of women in Canada will have an ultrasound during their pregnancy. While the procedure is considered safe for mother and baby, there are some risks. A growing number of studies are showing that ultrasound may cause harm in the growing fetus because of the relatively high amount of heat and sound that they produce. While heat and sound don’t seem particularly disturbing, the research suggests we may have underestimated their effects on the fetus, for which high heat can lead to central nervous system damage. (This is why we aren’t supposed to submerge for long periods of time in super-hot tubs or saunas, particularly in early pregnancy when the organs and central nervous system are forming.) The sound inside the woman’s uterus during an ultrasound was compared to a “subway train coming into a station,” according to a 2011 study in which the researchers put a microphone that detects sound waves underwater into a woman’s uterus during an ultrasound.
Dr. Bethany Hays, an obstetrician with more than 30 years of experience, says she sees ultrasounds being over-prescribed. Guidelines indicate that they should be limited to one or two per pregnancy when medically indicated. But what is meant by medically indicated? Hays says situations when a woman might want an ultrasound include early in the pregnancy if there is pain or bleeding (to ensure the pregnancy is forming in the uterus); if the mother doesn’t have clear menstrual dates before 12 weeks to nail down a delivery date; as an alternative to other genetic screening at 18 to 20 weeks (she cautions it cannot be used effectively for genetic screening if done any earlier); in cases where fundal height or fetal growth are in question; or if you are concerned about amniotic fluid in a high-risk pregnancy. The Society of Obstetricians and Gynecologists of Canada have guidelines around the use of ultrasound in pregnancy. They caution that ultrasounds should not be used to just determine the sex of the baby and that “if your health-care provider recommends that you have an ultrasound, make sure you know why it is needed, the risks that may be involved, and how it will be done.”
Little Things Matter
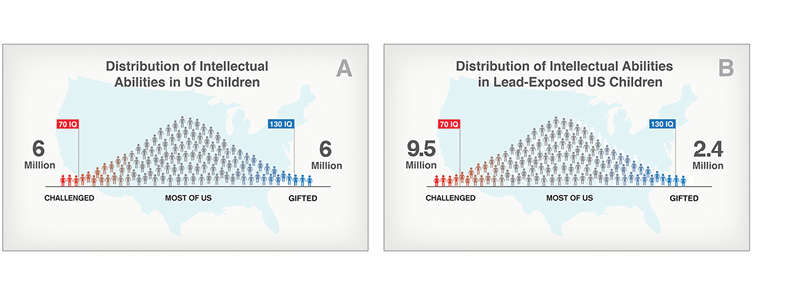
Dr. Bruce Lanphear — toxin scientist, medical doctor, and dad — reminds us that “not all chemicals are bad.” Yet it only takes a tiny dose of the bad chemicals to “have a lifelong impact on children.” The amounts seen in children today, though so minuscule they are measured in parts per billion (ppb), are causing serious effects, including loss of IQ points. The combined total can be substantial in one child and even more substantial in the population as a whole. “Children with more exposure to toxins won’t reach the same cognitive abilities as those exposed to less,” says Lanphear. “Little shifts in children’s IQ scores [have] a big impact on the number of children challenged.”
The Beautiful, Vulnerable Brain
“[The brain] makes us who we are,” says Dr. Bruce Lanphear. It’s so important that it has its own built-in biological protection system: the blood-brain barrier. Like the placenta, however, the blood-brain barrier is really more like a porous protection system. Large molecules, molecules that have a high electrical charge, and molecules with low lipid (fat) content do not pass readily through the blood-brain barrier. This means that it can help create a more consistent environment for the brain, protecting it from many foreign substances and hormones and neurotransmitters that travel through the rest of the body. The blood-brain barrier is not fully developed at birth and does not function as well when coupled with high blood pressure, infection, or inflammation or when exposed to high concentrations of chemicals in the blood, microwaves, or radiation.
The brain is particularly vulnerable to the effects of toxin exposure. It is susceptible for two reasons. The brain develops over such an extended period of time (in other words, it has many windows of exposure) beginning soon after conception and continuing for at least two years after birth. The brain is also susceptible because of the rapid rate at which it develops. Rapid growth creates added vulnerability. “This is why chemotherapy works on cancer,” Lanphear explains. The chemotherapy drugs kill the rapidly growing cancer cells, but they don’t affect the slow-developing cells of healthy tissue. Toxins can target the nervous system and brain because they are particularly drawn to the rapidly developing brain tissue.
If contributing factors of conditions such as ADHD and autism spectrum disorders can be removed, says Lanphear, “then which and why some children are more susceptible ceases to matter.” The key to prevention, then, is to identify any environmental risk factor and remove it. And there have been successes. Lead has been removed from gasoline and paints and children’s products. In turn, levels of lead (and also banned substances such as DDT, PBDEs, and PCBs) are diminishing in our children as those chemicals are phased out of use.
And while our science and government regulations may be lacking in North America, there is a silver lining. Citizens, many of them parents, are increasingly demanding safer products and getting companies to change. This citizen pressure has led to victories from Johnson & Johnson’s promise to phase out formaldehyde-releasing ingredients from its baby products to Whole Foods leading the charge on removing the worst cosmetics and food additives from its shelves. Similar to what happened with the consumer outrage over BPA, these are victories for citizen action.
Canadians can make a difference by asking better questions of the research that is presented on all chemicals and consumer products, avoiding products with unproven ingredients, asking companies to change their formulations, and asking their elected officials and governing bodies to take greater action on protecting human health from everyday toxins.
It all starts here. A new baby is a new opportunity to mother not just this new life, but also life in general. That instinct you have that things aren’t quite what they say they are is probably right. Your parenting instincts will only grow stronger, fuelled by a better understanding of the science, your own observations, and a power to ask more of those who represent you and market to you.
How to Get Everyday Toxins Out of Your Pregnancy
Babies, especially while still in utero, are unable to adequately eliminate the toxins to which they are exposed. However, it is possible to reduce their exposure to potentially harmful chemicals by taking greater care in what you eat, drink, breath in, and rub on; avoiding or lessening your exposure to everyday chemicals that have the potential to cross the placenta and provide additional stress on the growing baby; and enhancing your own natural pathways of elimination. Here are a series of action steps listed from ♥♥♥ (biggest impact, and possibly more work) to ♥ (quick and easy) to help you get those nasty toxins out of your pregnancy.
- ♥♥♥ Eliminate the big-hitter chemicals and drugs. If you are reading this book, then you certainly care about growing the healthiest child possible. If you are still smoking cigarettes (or even using e-cigarettes) or drinking in excess, then it is clearly because it is out of your control. For the health of your child and your grandchildren, this is the most important battle you can take on. No amount of organic food and skincare will undo the negative effects of these routine exposures. That doesn’t mean these other things don’t matter; it’s just that as you now know from everything else you have read, two goods can’t undo one bad when it comes to toxin exposure and a growing fetus.
Nearly everybody in my family of origin has been a smoker and tried everything to quit. When nothing else worked, they found help through acupuncture, hypnotism, and diet. Try everything; the stakes are high. Similarly, alcohol addiction is not something most people want to discuss, especially when pregnant. Guilt is not a good motivator, according to my research and experience. Hope, however, is a great motivator. You should know, then, that it isn’t too late for your child to benefit from you tackling your addictions. As I have mentioned, my family of origin has suffered greatly through all kinds of drug addictions, and I have seen the healing power ripple down through the generations when a person — even if that person is a grandparent — faces their addictions, whether to alcohol, tobacco, caffeine, work, or even cellphones.
- ♥♥♥ Organic-ize your diet and your kitchen. A nutrient-rich diet is the most important tool in supporting your body’s natural ability to eliminate toxins. Eating organic (see the previous chapter for more on this) has also been shown to significantly reduce your exposure to pesticide residue. Continue the good work by keeping plasticizers (including BPA, phthalates, and more) and water-resistant and non-stick coatings out of your storage containers, food packaging, pots, and cooking utensils.
While it is not possible for most of us to completely eliminate plastics from our lives, we can certainly reduce our exposure where it matters the most. All plastics have the potential to release hormone-mimicking chemicals into our food. This includes those items labelled BPA-free, which can still leach other compounds.
Eating and drinking food from cans is thought to be the largest contributor to our body burden of BPA. I would especially avoid fatty or acidic foods packed in cans, because they can leach more of the chemical into themselves. Instead of buying foods in cans, fresh and frozen foods are a far better option, both from a nutrient perspective as well as from a toxin perspective (and most often a cost perspective).
When storing food or buying take-out, use glass or stainless steel. Avoid plastics, including plastic wrap, especially for hot foods or foods that will be heated. When this isn’t possible, such as when getting take-out, I’d choose just about anything over Styrofoam, especially if the item is hot or acidic.
Get rid of non-stick and water-resistant cups, wrap, and cookware. You can save money and potential chemical exposure by going with cast iron, ceramic, stainless steel, titanium, or glass pots and pans. For all those water-resistant slick packages, follow the plastic guidelines: the hotter, more fatty, or more acidic, the more nasty chemicals can leach out of the packaging and into the food. I’d ditch the microwave popcorn or the cook-in-bag rice at all costs, but might still buy parsnip chips in a bag with a similar glossy mix of chemicals.
- ♥♥♥ Get toxins out of your skincare regime and indoor air. Learn more about doing this in the next two chapters!
- ♥♥︎ If you are getting the flu shot while pregnant, ensure it is the preservative-free version. Preservative-free (mercury-free) inactivated flu shots are available for pregnant women. These are packaged and sold as a single-use injection (hence no need for a preservative). Press the point! No amount of mercury exposure is proven safe for pregnant mothers and babies.
- ♥♥ When getting dental work, avoid amalgam fillings. Pregnant women and children in Canada are still routinely exposed to mercury in amalgam dental fillings — despite warnings about its being “extremely toxic” issued by the American Society of Dental Surgeons as early as 1845. Mercury is released from amalgam fillings as vapour, through chewing, brushing, and steady wear and tear. Much of the developed world, including much of the European Union, has entirely or partially restricted the use of amalgam fillings, particularly in pregnant women and in children. Health Canada has issued warnings that it may not be advisable to use amalgam fillings in children and pregnant women, but they continue to be the most common type of filling used in Canada today and are also routinely used in the United States.
- ♥♥ Get your pathways of natural elimination working. The previous chapter had a lot of tips on getting your digestion moving. You can get yourself sweating through gentle exercise and warm baths, pee out more toxins by drinking more water, and ensure you’re getting good nutrition.
Nutritionist Margaret Floyd Barry recommends oil pulling, and while there is no proof that it removes toxins, there is evidence to show it reduces gingivitis. So pull away! Oil pulling is the process of taking edible oil and swishing it around your mouth and teeth for about 20 minutes or so and then spitting it out along with anything it “pulls” from your body. I used to do this in the car on the way to work, and besides being a safe way to gently detox while pregnant, it can also make your teeth brighter and your breath fresher.
- ♥♥ Decrease your caffeine intake. Caffeine is a drug, and there is no proven safe level for a fetus. If you are in the habit of drinking sodas or energy drinks, try replacing them with the probiotic-rich homemade ginger beer (see page 67), or substitute with drinks that contain less caffeine and sugar and more probiotics, such as kefir, water kefir, or kombucha. If you have a habit of drinking coffee, try replacing it with certified organic decaffeinated coffee. The organic certification will protect you from the worst of the chemicals found in the coffee and from the chemically intensive decaffeination process as well. Or replace it with a cup of black or green tea that you decaffeinate at home (learn how in the previous chapter) or with a cup of herbal pregnancy tea (recipes to follow).
- ♥♥ Filter your water. I recommend a more involved system than a Brita pitcher filter, but even it is far less expensive and far better for you and the environment than bottled water. A really good water filtration system will cost more upfront but will last longer and filter more toxins, and most can be tailored to filter fluoride. There is a growing body of research to suggest that fluoride, a chemical added to the public water supply in much of the U.S. and Canada, may interfere with healthy body functioning and interfere with brain function. Fluoride accumulates in the body, particularly in the bones and pineal gland and the amount in bones increases over a lifetime, with children taking more into their bones than adults. Fluoride also crosses the placenta. Its linked with slowing down the time it takes for teeth to appear, which increases risk of decay. It is also associated with the tooth discolouration called dental fluorosis, now estimated to affect 41 percent of American children.
- ♥ Save the ultrasound for when it is medically necessary. I know; I loved the security I felt from seeing the baby growing inside me and having the doctor say, “Everything looks great!” Just remember that those ultrasounds come with a risk, and it’s equally satisfying to minimize that risk. Always ask your healthcare provider why an ultrasound is needed, and then do your own research to see how legitimate that need is and if you can wait. If you were to get just one ultrasound, I’d recommend doing it during that 18- to 20-week window, when the ultrasound can be used in lieu of a number of other tests often prescribed in early pregnancy, many with high rates of error.
- ♥ Stop dry cleaning. The dry-cleaning process exposes workers, those who live nearby, and you when you wear the clothes to one of the nastiest, most persistent toxins there is: perchlorates (PERC). PERCs can affect the endocrine system and is linked with breast cancer. If you wear dry-clean-only clothes for work (or because you are Princess Kate), then you will be happy to know there is a safe alternative to dry cleaning called wet cleaning, and there is almost certainly a wet cleaner in your town.
- ♥ Avoid over-the-counter medicines such as painkillers in pregnancy. As the new research on acetaminophen shows, substances long assumed to be safe are often under-researched. I advise trying the natural, food-based, or time-tested remedies first. If something is largely food-based (such as herbal tea), then our bodies are usually able to handle it through normal systems of detoxification. Synthesized chemicals — whether in the form of drugs or chemicals or super-concentrated herbal oils — can “outsmart” the body’s ability to properly and safely handle them, so it is more likely to make it across the placenta to your baby. That’s great if you are trying to treat the baby chemically, but not so great if you are trying to treat the mother without experimenting on the baby-to-be as well. Use natural remedies instead of pharmaceuticals for treating normal pregnancy-related issues such as nausea, swelling, and varicose veins. Read on for suggestions for gentle herbal teas, homeopathic remedies, and aromatherapy solutions.
- ♥ Develop a gentle exercise routine, such as yoga, water aerobics (preferably not in a chlorinated pool), Pilates, or walking or hiking, all of which help to keep your natural pathways of detoxification working perfectly while providing the other positive benefits of exercise. Read on to learn a yoga routine you can do during pregnancy.
The Natural Pregnancy Handbook
The Phases of Pregnancy
The way women experience pregnancy is as varied as women themselves, says Kate Koyote, midwife and co-founder of the Matraea midwifery practice, alternative health centre, and line of organic teas, herbal balms, and birth kits. Her midwifery practice does about 50 percent of births in the Cowichan Valley of British Columbia. She herself has five children, and each pregnancy was also varied. When she first meets with pregnant women, they come with all sorts of emotions that range from excited to scared, or the woman may be laid-back and her partner extremely anxious. During the first visits, Koyote works with her clients to make sure they understand the midwifery model of care, which is based on being the woman’s partner in creating a healthy pregnancy and birth, as well as establishing how they are feeling both mentally and physically. Women who work with midwives in Canada usually have more access to and longer visits with their care provider, and in most provinces, such as B.C., they also have a choice about where they want to birth, whether at home or in a hospital.
Pre-Embryonic Phase (First Two Weeks)
Pregnancy begins with conception when that lucky sperm and its corresponding genetic and epigenetic material unites with the woman’s egg and her genetic and epigenetic material and begins its journey of great influence inside the environment of the mother. Most women are as unaware of the moment of conception as they are of all the other cellular events that make up life. The first two weeks are a time of rapid cell division as the embryo-to-be moves from the fallopian tube, where fertilization generally occurs, to the uterus, where the growing cluster of cells implants into the uterine lining around day ten. By the end of the first two weeks, the placenta has begun forming, and levels of Early Pregnancy Factor, an immunosuppressant protein, is already being manufactured.
First Trimester (Embryonic Phase)
The overwhelming experience for most pregnant women during the first trimester is one of nausea, vomiting, and lack of appetite, which affects 60 to 75 percent of pregnant women the world over. Indeed, it seems to transcend race, ethnicity, region, class, and lifestyle. It also transcends the morning and can affect women day and night, and while it often passes with the first trimester, sometimes it doesn’t (as I discovered in my second pregnancy). The other common experience in the first trimester is fatigue. Elevated levels of progesterone are one of the culprits. Progesterone helps build up the uterine lining and slightly suppress the mother’s immune response so that her body doesn’t fight off the baby as a foreign invader (having suffered from parasites, I can confirm there is nothing as similar to that experience as the first trimester of pregnancy). The progesterone, combined with the relaxin (which helps relax the joints and widen the pelvis), work together to slow digestion, so that your body has the most opportunity to get nutrients out of food.
If you have just read the last chapter on nutrition, you may be cursing my name as you struggle to eat anything, let alone everything important for growing that baby. For most women, including myself, eating everything supposedly necessary was impossible. If this is the case for you, focus on bone broths, lightly-steeped pregnancy teas (such as from ginger or red raspberry leaf), and try your best to get your cod liver oil and folate supplements down to aid in the massive brain development during this time. Your body will likely guide you in avoiding many airborne toxins and even alcohol, coffee, and that kind of thing, which so many pregnant women report make them feel nauseated in their first trimester that a number of my friends say this is how they knew they were pregnant. As well, work your best to avoid junk food, indoor air pollution, and skincare pollutants. Indeed, because I more than once stopped to vomit while passing a leaf blower or when opening a new bottle of skin cream, I am convinced that the purpose of morning sickness is in part to help us avoid the very toxins to which we are most vulnerable, especially during this early period. Unfortunately, it also makes it hard to stomach that prenatal vitamin and liver. Koyote, the midwife, says that she counsels her patients that if they just can’t stomach their prenatal vitamin, to skip it during this period because it’s more important to focus on food sources of nutrition, stay hydrated, and avoid potential toxins. Most women want to avoid pharmaceutical medicines for morning sickness, and she encourages her patients to try all of the natural options first, including acupuncture and acupressure, ginger, herbal teas, and B vitamins. (See the next section for more ideas.) As well, eating protein-rich snacks at regular intervals can help keep the blood sugar stabilized, which can also prevent nausea.
Weeks Three Through Seven
During this period, the baby-to-be is called an embryo and begins to develop all of its essential parts and organs: the heart begins to beat, the head and brain begin to form, and the baby’s first movements and reflexes begin. At the end of this time, the embryo looks like a miniature baby and is about half an inch long. Drug, alcohol, and toxin exposure during this period are the most correlated with abnormalities of structure or form, such as to the shape or function of the heart, eyes, arms, legs, ears, palate, teeth, and, near the end of that time, external genitals.
De-Stress the Thyroid
Bethany Hays, MD, has spent 34 years in obstetrics, founded a non-profit holistic healthcare centre called True North, and serves on the board of the Institute for Functional Medicine. Hays also knows a lot about the importance of the thyroid gland. She lost her own thyroid as a young woman between her first and second babies when she developed cancer that was likely caused by childhood irradiation.
The thyroid gland, which sits near the neck, is responsible for energy production and metabolism of all the cells in the body, including the brain. It works closely with the adrenal glands, found near the kidneys, on issues related to hormones, using and conserving energy, and the stress response. If the adrenals are under chronic stress — from daily life, diet, or environmental factors — they will tell the thyroid to slow down to help keep from over-drawing the adrenal bank account. Numerous environmental toxins directly affect the thyroid, as well, including most of the POPs (PERC, dioxins, PCBs, chemical flame retardants, and PFOAs), heavy metals, pesticides, plastics, soy, and fluoride. “Thyroid is the sentinel gland for the environment,” says Hays.
All of these stresses can lead to autoimmune hypothyroidism, which is responsible for the vast majority of all thyroid problems in North America. Hypothyroidism can result in fatigue, weight gain, thinning hair, digestive problems, constipation, and hormonal issues, and has even been linked to issues of the developing brain, such as developmental delays, ADHD, and autism. It is also a cause of infertility and miscarriage. “The machinery has to be very carefully balanced to create sperm [and] ova, and having thyroid far enough out of the range it is supposed to be in adds to the problems of getting those things to happen and in the right order.
“I think Mother Nature’s approach is that if life is too stressful, there is no need to be making babies. If they don’t, they may get pregnant, but will they stay pregnant? Does the baby’s brain form normally?” If a person is able to improve their environment and reduce stress, then their thyroid will work better. Hays says that to really address the issues of the thyroid, we need to “upstream”to focus on the causes, rather than the symptoms. The tips in this chapter will help. Learn more about Dr. Hays and reducing stress in Chapter 7.
Weeks 8 Through 12 to 14
During this period the baby-to-be begins to grow hair and fingernails. It is possible to determine a boy from a girl, and the embryo is able to make facial expressions and even sucking motions with the lips. The eyes are almost completely developed, but they remain closed. The baby is able to drink amniotic fluid and pee it out. Weeks 8 to 14 are particularly sensitive for the developing sperm in a baby boy.
Second Trimester (Fetal Stage)
Weeks 13 Through 27
For me, as for many women, the second trimester was the golden time of pregnancy. I was finally able to pick myself up out of bed in the morning and avoid that afternoon nap, and by the end I was even able to return to my favourite pastime of freshwater swimming. The nausea eased up, and while I was still sensitive to smells, I could again walk into the kitchen and open the dishwasher without retching. Perhaps just as rewarding during this trimester is being able to finally feel the baby growing and moving inside. As well, the changes of pregnancy are in full swing: likely your breasts have grown, your body is filling with extra fluid and blood, and a bit of extra fat is being stored all over (remember, you need that for growing the baby and creating milk, so don’t worry about it as long as it is from high-quality, organic sources, in which case it will build great milk and disappear quickly).
This is likely the time of pregnancy you will be feeling the best, so it’s important to eat particularly well during this period. The second trimester is the time to consume plenty of protein and calcium to aid in building the baby’s muscle, skin, fingernails (from protein), skeletal system (from calcium), and brain (from fats). During the fifth and sixth months, the baby-to-be’s milk teeth start to develop in the uterus. The second trimester is also a time of rapid brain growth. At every opportunity, you want to eat high-quality, fat-rich protein because your body cannot store it and the baby uses it daily. If you restrict your calories at this point, your body will use the protein you eat as fuel and rob the baby of the nutrients it needs to build muscles, skin, and fingernails. As well, eat super-clean, calcium-rich foods so that the baby does not need to rob your stores to build her bones. Calcium is more viable in fermented dairy than plain old milk (remember: organic, whole). It’s also in leafy greens, legumes, and seafood. You may find that you benefit tremendously during this time from frequent fat- and protein-rich snacks in order to maintain healthy blood sugar levels.
Many women also return to an exercise program. Gentle exercise such as yoga and water aerobics can be low impact and protect the joints. Women who are more physically active need to be aware of their changing centres of gravity and their bodies’ different needs. Koyote says this is also when she starts discussing gestational diabetes with her clients. The treatment of gestational diabetes is diet and exercise, and thus prevention is the same. Pregnancy itself is considered a bit of a diabetic state because the placenta releases hormones that slow down the sugar to direct it through the mother and into the baby. The fundal height measurements — the measurement between the pubic bone and the belly button — is one indicator at this point that the baby’s development is progressing normally. Typically the fundal height measurement equals the number of weeks pregnant.
Because of the importance of protein during the second trimester, particular attention should be given to finding sources that are of the highest quality possible and to avoiding soy, which has been shown to be able to affect the developing hormone system and sex organs of the baby-to-be.
Third Trimester (Fetal Stage)
Week 27 to the End of Pregnancy
I found the beginning of the third trimester a relief because I could regularly feel the baby move and I knew that the baby could survive if born early. By the end of the third trimester, the magic of pregnancy had worn off. My first baby was nearly two weeks past her due date — which, while being totally normal, was causing me a great deal of anticipation. I had gotten the room ready, folded all the baby clothes, and set up the birthing tub. I could barely sleep. Nothing was comfortable. My belly was enormous: it felt like a creature all its own. As well, by this time, my emotions were running high, and if I got particularly upset, my nose would spring a bloody leak: the blood vessels in the nose expand during pregnancy and that, with the increased blood supply, puts more pressure on those delicate vessels. In terms of appetite and brain fog, it felt like the first trimester all over again. Indeed, the pregnant body and brain are flooded with hormones, in particular estrogen and progesterone, and a mother-to-be can be more irritable, weepy, and anxious than she would be otherwise.
As a midwife, Koyote says that in this trimester she encourages women to focus on the positioning of the baby. By about 32 to 34 weeks, the baby is of the size and weight that positioning makes a difference. Optimal fetal positioning is the concept of getting the baby positioned for ease of birth, which means having the baby’s head down and facing the spine of the mother, with chin tucked. Ideally, the baby’s back will be on the mother’s left. When the baby is in this position, the natural shape of the pelvis helps the baby wind its way out with the crown of the baby’s head, which is the smallest part, in the lead. This helps to prevent back labour, which is when the baby’s back is to the mother’s back, a situation that can increase the duration of labour and the chance of a C-section being required.

If women focus on their posture — not letting the curve of their back get too exaggerated and their bellies pulling forward and down — and their position while sitting, driving, and lying, they can help encourage optimal fetal positioning. When a pregnant mom sits on a couch with her feet up, her pelvis becomes a hammock and the baby will lie with his back in the curve of that hammock. That’s the opposite of what’s ideal. The heaviest parts of the baby — the crown of the head laterally or the back horizontally — will naturally want to move to the bottom. To use gravity to your advantage, sit on the couch sideways and lean forward a bit on the armrest, put a rolled-up towel under your sitting bones while driving a car, and lie on your left side at night. As well, exercises where you are on all fours — knees and hands — and gently tilt your pelvis, or where you lie across or sit on a large exercise ball, can help with ideal positioning.
This trimester is also when Koyote speaks with her clients about the benefits of perineal massage. “It’s really a perineal stretch,” says Koyote. “For a lot of women, the fear of childbirth is the fear of tearing,” and gently stretching and preparing the perineum can help. “You will never do a stretch that will feel as intense as when you have the actual baby,” she says, but perineal massage creates a body memory so that in the moment of birth a woman is more able to breathe into the stretch and relax.
By the end of the third trimester, fluid and blood volume have expanded significantly, and there is a naturally occurring anemia at this point. Koyote likes to check iron and hemoglobin levels at this time to ensure it stays in the normal range. She also recommends taking herbal teas with red raspberry leaf and nettle, traditional herbs used throughout time for uterus toning and support. They can also help with anemia. “If you were going to sign yourself up for the Boston marathon, you would train. You wouldn’t just sign up and then go the next day. The uterus is the same thing.” Braxton Hicks contractions are one way the uterus practises for its big work, and those will also often start by the end of the third trimester.
The third trimester for the baby is one of continued rapid brain development, with the weight of the brain tripling. The rapid development means more vulnerability to drugs, nutritional deficits, and toxins. It’s a great time to keep eating that protein and essential fatty acids, especially from fish and fish oils.
Natural Pregnancy Remedies for Common Concerns
Need I even say it? Home remedies are not the same as having a midwife or medical professional who knows you, your body, and your growing baby-to-be. The home remedies below are merely a sample of recipes and old wives’ cures, some used for many hundreds of years, to help get women and baby safely and comfortably through pregnancy. The aromatherapy suggestions are made with the guidance of aromatherapist Heather Gibson and the homeopathy suggestions are thanks to classical homeopath Sonya MacLeod. You can learn more about them in the sidebars in this section. There is a wealth of information out there to help you on your journey to becoming the expert on caring for yourself and your growing baby; some of it is listed in the resource section at the end of the book. Becoming that expert means becoming a better observer of your own needs as well as your baby’s and knowing when you need more help. A good healthcare provider will be your partner in helping find natural remedies where appropriate and helping you determine when more emergency intervention is needed. Dr. Aviva Romm — medical doctor, midwife, herbalist, and author — says this about using herbs in pregnancy: “Overall, most herbs have a high safety profile with little evidence of harm. Pregnant [mamas] commonly experience minor symptoms and discomforts for which the use of natural remedies may be gentler and safer than over-the-counter and prescription pharmaceuticals.”
Remember, the remedies below are a guideline only, and while homeopathy, particularly the kind taken as “sugar pills,” is unlikely to cause direct harm, herbal remedies can be more potent and should be used with caution and guidance during pregnancy. There are some herbs better not consumed internally at all during pregnancy, according to Romm: these include the abortificants (tansy, safflower, rue, mugwort, yarrow, scotch broom, angelica, wormwood, and pennyroyal), stimulating laxatives (castor oil, buckthorn, and aloes), phytoestrogens (hops, isoflavone extracts, and red clover), and other herbs such as comfrey, borage, barberry, goldenseal, and Oregon grape. If you are in an acute situation of any kind during pregnancy — such as a prolonged headache, extreme dehydration, or severe swelling — these are signs that you need to seek immediate medical help from a professional.
Herbal Pregnancy Tea Recipe
Red raspberry leaf is the herb for pregnancy: it can help calm first trimester symptoms like nausea and third trimester symptoms like anemia. It’s mineral-rich and helps tone the uterus. Other herbs that are generally agreed to be safe for use as tea in pregnancy include mint, chamomile, lemon balm, nettles, rose hips, ginger, and small amounts of echinacea to treat cold symptoms. Always use organic herbs to minimize pesticide exposures.
Ingredients:
2 tablespoons organic, dried red raspberry leaf (uterine tonic that provides vitamins A, B, C, and E, and calcium, iron, and potassium; also helpful for increasing fertility in men and women)
1 tablespoon organic, dried nettle leaves (uterine tonic that provides vitamins A, C, D, and K, and calcium and potassium)
You can also add any one or a combination of the following:
- 2 teaspoons lemon balm to support nervous system, digestion, and provide iron, calcium, and potassium
- 2 teaspoons oat straw to nourish nervous system and provide vitamins A, C, E, and B, and calcium, zinc, iron, and magnesium
- 2 teaspoons rose hips to add flavour and vitamin C
- 2 teaspoons mint to add flavour and enhance digestion (Caution: used postpartum, mint can reduce production of breast milk)
- 2 teaspoons chamomile for relaxation and to enhance sleep
- 1 teaspoon shaved ginger can help in the first trimester with nausea (if you can stomach it)
Directions:
Use 1 tablespoon of the mixed tea leaves of your choice (see above) per 2 cups (500ml) of boiling water. Steep for 20 to 30 minutes, strain, and then discard the herbs. Drink a cup 2 to 3 times a day.
Morning Sickness
In the section on nutrition I talked about the importance of magnesium. Another one of the things magnesium does is help balance blood sugar. Extreme highs and lows are part of what causes morning sickness. Pregnancy hormones can interfere with the absorption of magnesium, and since 80 percent of people are already magnesium deficient, you probably need more. I recommend using a magnesium spray: it’s effectively absorbed through the skin, and you can take it this way even when you are too sick to stomach it. The first few times you use it, it can sting a bit, but that quickly passes as you get used to it. Magnesium deficiency can also cause body odour, so try using your spray on your armpits, where it’s readily absorbed and can be part of a healthier deodorizing option than conventional deodorants. Other sources include magnesium supplements and magnesium drinks such as Natural Calm. Because our soils have become increasingly depleted in magnesium, it’s nearly impossible to get enough through food alone, but eating seeds and nuts can also help.
Other natural morning sickness cures include vitamin B6 (typically three doses of 25 mg three times a day), or, for greater effect, vitamin B injections under the care of a naturopath or physician. Ginger has also been shown to be effective and safe during pregnancy. Try ginger candies or homemade naturally fermented ginger beer (see page 67 in the Green Eating Recipe Handbook). I also enjoyed and found relief from homemade bone broth, which can be made with the addition of ginger and nutritional yeast to make it a source of all of Grandma’s nutritional cures at once, although for truly bad cases of nausea, it might be wise to do additional supplementation, as well.
Acupuncture and acupressure can help relieve the nausea of pregnancy. You can work with a TCM to receive acupuncture or use acupressure at home. I used acupressure bands to help my morning sickness. These are also sold as motion sickness bands and are meant to be worn so that they press against the acupressure point just a finger’s width above the inside of the wrist.
Homeopathy can help, as well, with the most common remedy being Nux Vomica 30c taken two to three times a day. Aromatherapy may also help, so try a drop of ginger essential oil on the palms of your hands and inhale. Or put a few drops of pure essential oils with citrus scents like orange or lemon on a bandana or scarf around your neck, or put a few in a vaporizer or in some water on the stove. Citrus scents can also help with fatigue; put a few drops on your hands and inhale and massage on the back of your neck.
Varicose Veins
The blood volume increases during pregnancy, and increased progesterone can cause varicose veins, which commonly appear in the legs, but can also appear as hemorrhoids or vulvar varicosities, when blood pools inside the pelvic veins deeper inside the body. The good news is that all forms of varicose veins typically diminish or disappear in the year after birth. The bad news is that they can become more likely in subsequent pregnancies. During pregnancy you can help prevent them by eating a healthy diet with plentiful good fats and by avoiding foods that promote constipation, such as refined flour, sugar, and processed foods. As well, avoid wearing high heels and sitting or standing in the same position — especially crossing your legs while sitting — for long periods. Natural treatment options include chiropractic and acupuncture care to help with circulation and the general health of the pelvic area and nerves. It can also help to partake in gentle exercise, wear maternity support hose, sleep on your left side to relieve pressure on the inferior vena cava, drink plenty of water, and elevate your legs (see the Legs up the Wall pose instructions on page 177 in the Prenatal Yoga Handbook). Try drinking pregnancy herbal teas with nettle leaf or oat straw. The homeopathic remedies that can help include Hamamelis for varicose veins and Sepia for hemorrhoids; both can be safely used during pregnancy in the potency of 30c two to three times a day. Witch hazel compresses (see below) can help with varicose veins in the anus and vulva area.
How to Make Witch Hazel Compresses
Witch hazel has anti-inflammatory properties and is a natural antibacterial. Pour 1 to 2 tablespoons (15–30ml) on a reusable menstrual pad and freeze it before using to help ease pain associated with vulvar varicoses, hemorrhoids, or healing after giving birth.
Swelling, High Blood Pressure, and Preeclampsia Prevention
Preeclampsia is a serious medical condition and the second leading cause of maternal death in the U.S. It’s marked by sudden and severe swelling, hypertension, and protein in the urine, and it typically occurs in late pregnancy. Swelling in itself is uncomfortable at best.
Obstetrician Tom Brewer established a link between preeclampsia and protein deficiency in the 1970s. The Brewer Diet is based on preventing the ravages of preeclampsia by eating 100 grams of high-quality protein from meat, poultry, fish, eggs, and milk. That’s four or five small servings of meat or fish every day. A can of wild salmon is two servings that equal 45 grams of total protein, 100 grams of steak or chicken breast both have about 20 grams, an egg yolk has 12 grams, a glass of whole milk has 8 grams, and just ten almonds has 2.5 grams. You can further enhance this diet by avoiding fried and processed foods and increasing your potassium, calcium, and magnesium levels.
Meditative practices, gentle exercise, fresh air, and anything that helps reduce stress — even reading — can help prevent high blood pressure. And the discomfort of swelling is further helped by getting the legs or arms above the heart. The most common homeopathic remedy prescribed to bring down swelling and edema is Apis 30c taken two to three times a day.
Avoiding Gestational Diabetes
Gestational diabetes affects up to 9 percent of pregnant women, and while its symptoms usually disappear soon after giving birth, both mother and child are at greater risk of developing Type 2 diabetes. Researchers have been using the data from the Nurses’ Health Study, the same one that has given so much information on fertility and diet, and followed more than 6,000 women to understand why gestational diabetes is such a strong indicator of future diabetes. The conclusion is that epigenetics play a role and that environmental factors are turning on and off genes that make diabetes more likely. For instance, researchers found that drinking soda was more likely to flip the switch for the obesity gene. While much is left to be studied, gestational diabetes is an early indicator that environmental factors such as diet, sleep, and stress have already begun to affect you and your child. It also means that you might be predisposed to gestational diabetes through no fault of your own.
Prevention in this case is the same as the cure: better diet and exercise. In particular, the advice of nutritionist Margaret Floyd Barry is relevant: always consume carbohydrates with a healthy, fatty protein; skip refined sugars and carbohydrates; front load your day and your meals with those good fatty proteins; and partake in gentle exercise. As well, try sipping on a mix of apple cider vinegar with water before meals. Vitamin D, in conjunction with vitamins A and K, can also be helpful in preventing gestational diabetes. Anti-inflammatory foods like omega-3 oils, olive oil, fatty fish, and leafy greens can help, and so can reducing stress and getting at least eight hours of sleep. If you develop full-blown gestational diabetes, then what might be fine in other pregnancies — such as eating a piece of cake every so often or starting the day with a bowl of cereal — can put you and your baby at risk because, in short, your body and the baby’s body while inside you can’t handle sugars, including simple carbohydrates, even the natural kind. Besides diet and lifestyle changes, homeopathic phosphoric acid can be tried at 30c two to three times a day.
Inspiring Mamas: Adopting Aromatherapy for Families
Heather Gibson is a clinical aromatherapist and a mother extraordinaire: she also has three biological children and four adopted children, and she has fostered more than 20 kids. Gibson has turned to aromatherapy to help her manage her own health as well as many of the more difficult behavioural issues that she encounters as a parent. Gibson has used aromatherapy clinically to help clients relax during therapy. “It’s a tool, not a cure-all,” she says about using essential oils for health.
Essential oils can be used topically as a cosmetic or breathed in as aromatherapy, or some can even be taken internally. “Aromatic use is the safest way to use essentials oils and also the best way to use them for the emotions,” says Gibson. “It goes straight to your limbic system and affects you more powerfully.” She cautions that not all essential oils are made the same, and there isn’t true oversight of essential oil claims such as “pure.” When looking for a good brand, be wary of grocery store brands, many of which aren’t pure and can even have added petroleum by-products or fragrance oils. You can learn more about aromatherapy and essential oils for pregnancy and parenting at Gibson’s website www.MyHealthEmpowered.com and try many of her recommendations in this section.

Heartburn Help
Heartburn is common in later pregnancy and is caused by the pressure the growing uterus puts on the digestive system and the relaxation of the esophageal sphincter by the rise in progesterone.

The midwives at Matraea recommend watermelon (if you like it) and almonds, and eating small meals, not eating right before bed, and propping yourself up on pillows in bed. Aromatherapy can also help: try peppermint essential oil or a mix of equal amounts of lemon, mandarin, and sweet orange essential oil. Put a few drops of either blend on a tissue or on a scarf that you wear around your head. Or mix a few drops with an edible oil (such as olive or sesame oil) and use it on your chest. The homeopathic remedy Pulsatilla 30c, in two to three doses a day, can help a woman who has heartburn as well as other symptoms of indigestion during pregnancy.
Ease Those Leg Cramps
I was prone to leg and foot cramps, otherwise known as charley horses, in my pregnancy. Yikes! I found that a diet rich in magnesium, yoga stretches, and flexing the leg during the cramp could all help. You can also try a warm bath with half a cup of Epsom salts with essential oils added: 3 drops geranium, 10 drops lavender, and 2 drops cypress.
Treating Yeast Infections with Garlic
Vaginal yeast infections can be more common during pregnancy, perhaps because of fluctuating hormones. And while you don’t have to worry about the infection hurting the baby, if you still have it during labour, the baby may be more likely to develop thrush. Vaginal application of garlic is a cure I have used myself for treating yeast infections. Some midwives also say vaginal garlic suppositories used regularly at the end of pregnancy may be able to rid a woman of Group B strep (GBS).
Take a clove of garlic and peel it, being very careful not to nick the clove. Wrap the clove in a small rectangle of clean gauze and then tie closed the ends with a bit of equally clean, thin string, leaving a tail. In the end, the whole thing ought to look like a DIY tampon. Dip the cloth into organic, food-grade olive oil or coconut oil to help with insertion. Insert into the vagina and leave in overnight. Expect a bit of discharge. Change every twelve hours and use for three to five days. If the infection is more advanced, then you can purposely create a small nick in the garlic, or even cut the clove in half, significantly increasing your exposure to the garlic’s antibacterial and antifungal properties. Beware: this increased exposure comes with quite a sting.
Treating Headaches in Pregnancy
Headaches can occur during pregnancy for a variety of reasons, including low blood sugar, stress, and hormonal changes, as well as all the regular headache triggers, such as not getting enough water or suffering from constipation. If headaches during pregnancy are frequent or more intense than usual, talk with your doctor or midwife, because they can be a sign of much more serious problems, such as the onset of preeclampsia. For routine headache, tea may help. See the recipe that follows. Aromatherapy using lavender, lemon, peppermint, spearmint, sweet orange, or tea tree oil might help, as may acupressure. There is a pressure point on the hand in the fleshy part between the thumb and the pointer finger; if you try probing around in there, you will often find a more sensitive spot. Press on this with the thumb and forefinger of your other hand for as long as possible.
Inspiring Mamas: Homeopathy to the Rescue
Sonya McLeod, B.A., DCH, R.Hom., found her way to studying homeopathy after she had her second daughter and found herself plagued by health problems with which her doctors couldn’t help.
Classical homeopathy originated in Germany more than 200 years ago, and it is based on the idea that the body can be taught to heal itself and works on the energetic level. To do this, homeopathic doctors operate under the principle that “like cures like.” To make homeopathic remedies, they use nano amounts of a natural material — such as a mineral or a plant or, say, a bit of bee — and dilute it many times. In homeopathy, the more diluted something is, the stronger it is. For example, a homeopathic remedy given to a person suffering from insomnia is coffea, a remedy made from coffee. The final homeopathic remedy is so dilute that there isn’t more than a nanoparticle of the original substance, in this case coffee, left within. Rather, an energetic imprint has been made on the substance in which it is diluted — such as sugar water or alcohol — and that imprint is what stimulates the body to heal itself.
Homeopathy is so different from our usual understanding of chemistry and pharmaceutical medicines that it has garnered very vocal skeptics — from medical doctors to journalists — who say it isn’t conceivable that homeopathy works. Nevertheless, in many places, such as England, France, Switzerland, Italy, the Netherlands, and India, it is so popular that it has been incorporated into mainstream medicine. It’s called the leading “alternative” treatment used by physicians in Europe. At the very least, what skeptics and homeopaths alike agree upon is that homeopathy is so gentle that it is virtually impossible to cause harm from its use.
McLeod recommends that pregnant women look into cell salts — very gentle, mineral-based homeopathic remedies — which can be used to help balance or provide minerals during key times of pregnancy. To learn more about cell salts and what remedies might be an addition to your pregnancy, visit a homeopath or try out McLeod’s website at www.littlemountainhomeopathy.com, or try some of her general recommendations in this section. McLeod cautions, “If after a few doses there is no improvement, a person is advised to move on to another remedy or seek the help of a trained homeopath.”
Headache Tea Recipe
Ingredients:
1⁄2 cup dried lemon balm leaves
1⁄2 cup nettles
1⁄2 cup rose hips
1⁄2 cup spearmint leaves
Directions:
Use 1 teaspoon of tea leaves per 2 cups (500ml) of boiling water. Steep for 20 to 30 minutes, strain, and discard the herbs. Drink a cup 2 to 3 times a day.
Moodiness and Depression
There is a lot going on during pregnancy and after, as hormones surge through the body and life changes unalterably for most women. Nutrition can help prevent some of the moodiness and mild depression that can come with pregnancy. There are a number of studies linking adequate intake of DHA, especially from fish oils, to lower rates of postpartum depression. Additional nutritional support may be necessary if you have already improved your diet but moodiness and depression continue, or if they are severe. Extreme fatigue in pregnancy can be a sign of certain nutritional deficits, especially vitamin B12 and iron, and may warrant further testing.
For common moodiness or mild depression associated with normal pregnancy, homeopathy might help. Pulsatilla is for women who are very weepy, sentimental, and all over the place emotionally during pregnancy. Ignatia is good if the predominate emotion is grief, such as from losses in the past or lots of fear. For postpartum depression, Sepia is recommended. Take 30c two to three times a day.
Stretch Mark Prevention
It’s not really possible to cure stretch marks, only to reduce their appearance and try to prevent them. You will know if you are more susceptible if you already have stretch marks from a previous pregnancy or growth spurt. Fortunately, genetics or having previous stretch marks does not mean you can’t try to prevent future stretch marks, and diet is the key. Stretch marks are actually a tearing of the tissue in the dermis or middle layer of the skin that occurs when it is stretched beyond its capacity. That capacity can be somewhat increased through diet. Great foods that help include gelatin, which you can get through high-quality, natural supplements or by eating that ever-so-wonderful homemade bone broth (consider adding chicken feet for extra gelatin). Fish oil is another great food supplement that is high in vitamin A and anti-inflammatory omega-3 oils and can help with elasticity. Butter, olive oil, and coconut oil can also help with this. Eat antioxidant-rich fruits and vegetables, especially those high in vitamin C, which helps make the collagen necessary for skin elasticity. Foods rich in vitamins A, E, K, and B-complex will also help with the suppleness of the skin. The good news about preventing stretch marks through diet is that these same foods will help the perineum to stay soft and supple, thus making tearing during birth less likely. Skin-based prevention for stretch marks is not likely enough on its own because it is the middle layer of the skin where the tearing occurs, but nevertheless, having skin that feels rich and hydrated at the very least helps prevent the discomfort of growing larger and the itchy-dry skin feeling that may accompany it. Try the belly balm that follows for stretch marks. As well, you can try homeopathic Calc Fluor 6X cell salts one to two times per day.
Blossoming Belly Balm
Most apothecaries I work with recommend a base of cocoa butter and coconut oil. I personally find coconut oil a bit drying, so I will often supplement with unrefined sesame oil or olive oil, which can make the final product a bit runnier, but I like the feel. Try using two parts cocoa butter to one part other oil. Experiment to find your favourite!
Then add other oils for additional nourishment, such as rose hip oil, vitamin E oil, or sweet almond oil. Try any of these at about 1⁄2 part ratio to the oil. See the recipe below for clarification.
Ingredients:
1⁄2 cup (109g) cocoa butter
1⁄4 cup (52g) coconut oil
2 tablespoons (30ml) rose hip seed oil, vitamin E oil, and/or sweet almond oil
5–10 drops lavender essential oil
5–10 drops helichrysum essential oil
5–10 drops of myrrh
Directions:
Warm cocoa butter and coconut (or other) oil in a double boiler until both are melted. Then add the rose hip seed oil, vitamin E oil, and/or sweet almond oil. Stir. Remove from heat. Add essential oils. Pour into jar. Apply regularly.
Labour Help
There are a lot of old wives’ tales about how best to bring on labour. Most midwives, however, will caution that the baby will come when the time is right. That being said, the information on proper positioning and gentle exercise leading up to the birth can help with a speedier labour. Perineal massage, water birth, and diets rich in omega-3 fatty acids, fish oils, and vitamins A, E, K, and B-complex will help to avoid tearing. Taking adequate amounts of fish oils can help soften the perineum. And drinking pregnancy tea with red raspberry leaves can help prepare the uterus.
Homeopathy offers a few helpers as well, including Pulsatilla 30c to turn a breech baby and Caulophyllum and Cimicifuga 30c. The latter two can be alternated (one in the morning, one in the evening) for overdue labours, and for a non-progessive labour alternate 200c potency of Caulophyllum with Cimicifuga every half hour or so. (Never take Cimicifuga or Caulophyllum during the first or second trimesters.) And for panicked fathers or grandparents during labour, a dose or two of Aconitum 200c will help. Arnica 30c pellets can help with healing and bruising after the labour.
Aromatherapy can help a person relax more into the labour. Try any of these out beforehand to find your favourite: lavender, wild orange, and peppermint, or bergamot. Use a diffuser for best results.