3.
The Alternate-Day Advantage
Ironically, I have to thank a group of rodents that had been genetically altered to gorge for helping me find a way to overcome the gorging DNA that’s hardwired into my reptilian brain.
THE LESSON OF MATTSON’S MICE
In 2003 I read about an experiment, described briefly in the Introduction, done by Mark Mattson and his colleagues at the National Institute on Aging. That experiment had, in turn, been inspired by a previous study completed by Mattson’s colleague Donald Ingram. Ingram looked at two groups of mice from the time they were weaned until the time they died. One group was given free access to all the food they wanted on a daily basis, while the second group was also fed freely but only every other day. The group fed on alternate days was found to live an average of 30 percent longer than the group that was fed freely on a daily basis.
Based on Ingram’s findings, Mattson took the study one step further. Using three groups of the same strain of mice (which had been genetically altered to gorge when given free access to food), he and his colleagues fed two groups exactly as Ingram had fed his. The third group was fed a daily diet that was restricted to approximately 40 percent of their normal caloric intake.
More Than Just Weight Loss
At the end of the twenty-week study, the group that had been fed a restricted diet on a daily basis lost weight, and tests also showed that their glucose and insulin levels were reduced, while insulin sensitivity and “stress resistance” were increased compared with the group that was fed freely every day. Lower glucose and insulin levels are known indicators of longer lifespan and are associated with a reduction in heart disease and diabetes. This was certainly not surprising, because it replicated Ingram’s findings, and, as we’ve discussed, dietary restriction had already been shown in other studies to positively affect health and longevity. What really caught my attention, however, was that the mice who were fed only on alternate days—even though they gorged on the days they were fed freely and did not lose weight—had levels that were as good or better than those who were restricted on a daily basis.
Resistance, Resilience, and Recovery
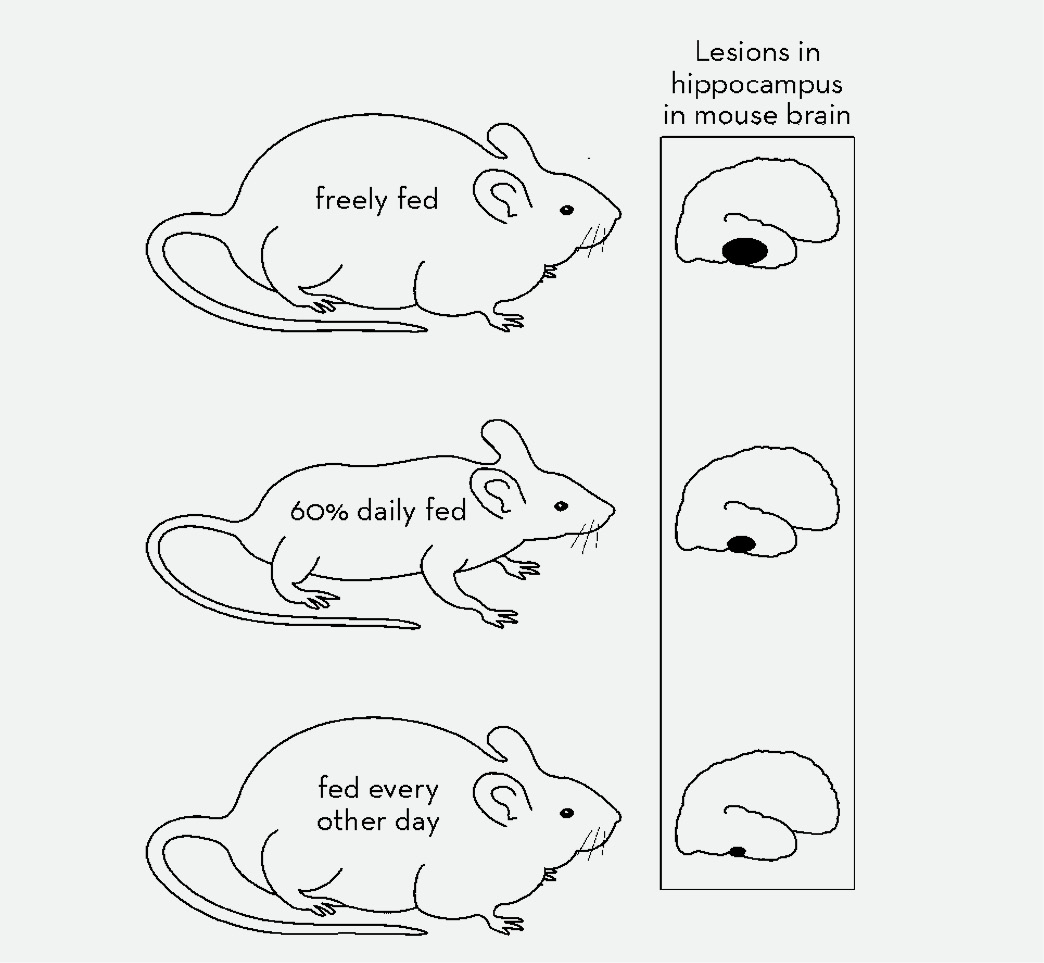
Following several weeks on one of three diets, mice were injected with an excitotoxin that would mimic the kind of neurological damage caused by diseases such as stroke, Alzheimer’s, or Parkinson’s. Mice fed every other day, while eating enough on their feeding day to maintain the same weight as the freely fed mice, showed distinctly smaller lesions in the hippocampus than either of the other groups, indicating that alternate-day feeding led to increased health and potential longevity over either free feeding or daily restriction.
Another indicator of health and longevity is the degree to which the central nervous system is able to resist and recover from the stresses to which it is subjected throughout life. In humans, the resilience of the central nervous system is an indicator of how people will react to brain disorders such as stroke and Alzheimer’s disease and their ability to resist the effects of environmental toxins. Mattson examined the ability of the central nervous system to resist stress in each of the three groups of mice. To do this he subjected the mice to an artificially created brain injury by injecting a toxic chemical (kainate) into a portion of the brain called the hippocampus, and later examined the extent of the area of damage. Once again, the amount of damage was markedly reduced in both calorie-restricted groups compared with the freely fed controls, but the every-other-day-fed mice had less damage than the mice that were restricted every day.
In other words, based on all the parameters Mattson studied, alternate-day feeding was shown to increase health and potential longevity to a greater degree than daily restriction.
Based on these results, Mattson and his colleagues concluded that intermittent fasting (feeding every other day) has “beneficial effects on glucose regulation and neuronal resistance to injury in these mice that are independent of caloric intake.”
What this groundbreaking study meant to me is that animals (and by extension, humans) do not have to restrict caloric intake on a daily basis and, further, do not have to be thin to be in good health.
HOW ELSE CAN ALTERNATE-DAY DIETING IMPROVE YOUR HEALTH?
If calorie restriction, especially every-other-day feeding, promotes good cardiac and central nervous system health, what else might it do? Might it also help prevent cancer?
Marc Hellerstein, an endocrinologist at the University of California at Berkeley, demonstrated the effect of alternate-day feeding on the rate at which the cells of various tissues divided (proliferated) in a group of mice. The rate at which cells divide and proliferate is an indicator of the likelihood of developing cancer. Dr. Hellerstein’s experiment showed that the rate at which skin cells, breast gland cells, and T-lymphocytes proliferated was markedly reduced within just two weeks in mice fed every other day, even though the total number of calories these mice received was not substantially reduced. These findings could be considered an indication of potentially profound cancer prevention benefits for human beings.
Another study conducted in France by Olivier Descamps and colleagues using a group of middle-aged mice that were genetically predisposed to be at high risk for developing lymphoma also demonstrated that alternate-day feeding protected against cancer. Over the four-month period of the study, not one of the mice being fed on alternate days developed lymphoma, while 33 percent of the control group did. In addition, the researchers found that oxidative damage to the mitochondria (the principal energy source of the cell), a basic indicator of aging, was significantly decreased in the alternate-day-fed mice. The investigators concluded that “the efficacy of alternate fasting did not really depend on calorie restriction,” and that “alternate fasting could exert a beneficial antioxidant effect and a modulation of the oxidative stress associated with aging.”
OXIDATIVE STRESS AND AGING
In 1954, a young physician named Denham Harman proposed an idea that changed the way scientists thought about how we age. His Free Radical Theory of Aging said that a side effect of oxygen metabolism in our bodies is the production of chemicals that gradually damage our cells, protein, and DNA, ultimately resulting in death. This damage, caused by so-called free radicals, is known as oxidative stress. His theory was not initially taken seriously within the medical community, but over time, medical research has caught up with Harman, and it is now widely accepted that the damage done by oxidative stress is the primary cause of aging in humans.
When apples turn brown, butter turns rancid, or iron rusts, they are “aging” and exhibiting the results of exposure to oxidative damage. Our bodies may not exhibit oxidative damage externally, but it is there just the same. Our bodies are made up of atoms and molecules, each of which contains one or more pairs of electrons. Over time, normal metabolism, mainly in the mitochondria, causes the formation of “free radicals,” which are atoms that have lost one electron. Free radicals are unstable and attempt to complete their structure and regain stability by “stealing” an electron from another, neighboring molecule. That, of course, prompts the molecule that’s been “robbed” of its electron to do the same thing, causing even further damage. The products of free-radical damage are like sludge that builds up in the cells, causing malfunctions and, ultimately, stress that is sufficient to cause the cell to die.
The same process also causes inflammation on the cellular level that, in turn, causes more oxidative damage. Both inflammation and oxidative stress have been shown to be associated with a number of chronic illnesses of aging, including atherosclerosis, arthritis, Type 2 diabetes, and Alzheimer’s disease.
Oxidative stress is reduced by both daily and alternate-day calorie restriction, possibly as a result of reduced oxygen consumption.
Oxidative Stress and Disease
Oxidative stress has been associated with some 250 diseases and with virtually all diseases of aging.
• Atherosclerosis: LDL cholesterol is deposited in the artery wall. Then free radicals “oxidize” the LDL by causing it to lose an electron, which makes the oxidized LDL irritating to the tissues and causes inflammation. This inflammation results in the formation of plaque in the wall of the artery, which obstructs the opening of the artery and eventually blocks the flow of blood.
• Arthritis is caused by oxidative damage in the joints. Inflammation causes increased oxidative damage.
• Alzheimer’s disease: The first event in Alzheimer’s disease is oxidative injury to the neuron, leading to the formation of a neurofibrillar tangle and deposits of beta-amyloid plaque.
• Cancer: An early step in the formation of cancer is often free-radical damage to the DNA that causes cells to mutate or change.
• Diabetes mellitus: Oxidative stress causes insulin resistance, the major contributor to Type 2 diabetes.
Low levels of oxidative stress are probably essential to reaching old age by preventing disease. At least two studies have shown lower levels of oxidative stress in individuals one hundred years old than in individuals seventy years old, suggesting that a low level of oxidative stress may be required to reach advanced ages.
How Free Radicals and Inflammation Cause Heart Disease and Stroke
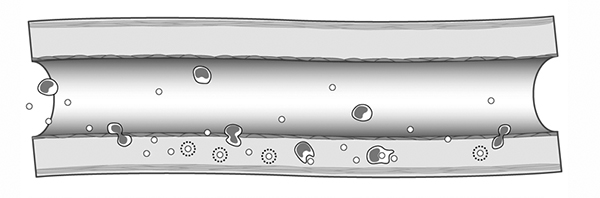
Elevated blood LDL cholesterol is deposited in the artery wall and is oxidized by free radicals, producing inflammation.
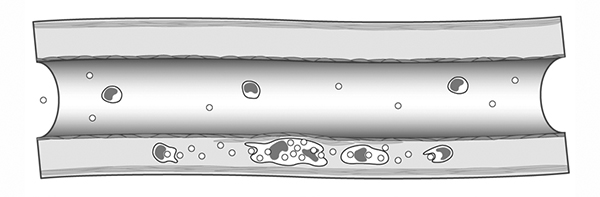
White blood cells ingest oxidized LDL, forming large foam cells. A pimple begins to form.
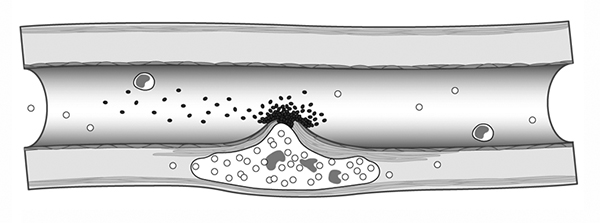
The pimple breaks, spewing inflammatory material into the bloodstream. This leads to clot formation.
By reducing inflammation and free-radical damage, Alternate-Day
dieting helps prevent heart disease and stroke.
Telomeres and Oxidative Damage
Telomeres are the ends of the chromosomes that become shorter as we age. This is because imperfect replication of the telomere occurs when cells divide, and some of the DNA is lost with each cell division. Eventually the cell cannot divide without damage to critical parts of the DNA, and it becomes senescent (not yet dead but not functioning normally), necroses (dies), or undergoes apoptosis (cell suicide).
We know that oxidative damage caused by free radicals is associated with shorter telomeres. Thus at a given age, those who undergo more oxidative stress will have shorter telomeres. People with shorter telomeres are 3 times more likely to die of heart disease and 8.5 times more likely to die of infectious disease.
Chronic inflammation means that white blood cells replicate more quickly, which, presumably, results in shorter telomeres. It seems reasonable to postulate, therefore, that people with chronic inflammation would have shorter telomeres at an earlier age, which would lead to premature cell senescence, necrosis, or apoptosis and earlier onset of chronic diseases of aging.
Because of its powerful anti-inflammatory effects, the Alternate-Day Diet will reduce the chronic oxidative damage and premature telomere shortening involved in such diseases as atherosclerosis, and would prolong life.
WHAT IF HUMANS ATE LESS OFTEN?
A number of studies suggest that it would be healthier to eat less often than most of us do—which is typically three times a day. One such study, which looked at people who were fasting for 12 to 14 hours during the thirty days of Ramadan, indicated that good cholesterol levels went up and there was a reduction in inflammatory chemicals (cytokines) in the bloodstream, with no weight loss.
Mark Mattson also performed a study of humans who were fed all their daily calories during a single four-hour period. In this case, the study subjects lost only 3 pounds over the six-month study, but they showed a 4.6-pound reduction in body fat, which meant that they had gained 1.4 pounds in lean muscle tissue. This may seem like a modest change, but reducing body fat by almost 5 pounds means a lot less inflammation is occurring. In this case, however, the study participants complained of greater hunger than when they ate regularly and did not like having to eat all their food in this limited period.
Both these studies, however, beg the question “Would we benefit from alternate-day calorie restriction?”
ALTERNATE-DAY CALORIE RESTRICTION BENEFITS PEOPLE TOO
The medical literature contains only one long-term study of humans that is described as an experiment in calorie restriction performed in a controlled setting with good nutrition. Published in a Spanish medical journal, Revista Clinica Española, in 1956, this study was conducted by Eduardo Arias Vallejo on a group of healthy male and female residents of the Residencia Geriatrica de San José, an old-age home in Madrid. At the time, Vallejo was the medical director of the residence and later became president of the Sociedad Española de Patología Digestiva (Spanish Society of Digestive Pathology).
When I read the original version of the study, however, it became clear that there was no overall calorie reduction involved. Rather, the test subjects were experiencing alternate-day restriction, eating less than their normal caloric requirement on one day and more on the next, so that on average their caloric intake was not actually restricted at all. There was also a control group who were fed “normally” every day.
Before we could analyze the study correctly, however, my colleagues and I needed to know the average daily calorie consumption of an elderly Spanish person in 1956. We consulted height and body weight data for Spaniards in the 1950s and determined that it would have been about 1,600 calories per day averaging both men and women.
On the low-calorie day the study subjects were given a liter of milk and 500 grams of fresh fruit, which we estimated to be approximately 900 to 950 calories, or 56 percent of the approximately 1,600 they would normally eat. Vallejo states that on the “up days” the diet subjects consumed 2,300 calories. Presumably, on those days they were allowed to eat as much as they wanted, and the 2,300-calorie figure was probably derived from adding up what they took on their trays at mealtime as recorded by the kitchen staff.
Based on these figures, the “restricted” study subjects were actually compensating for their 900-calorie down days by consuming 144 percent of normal daily caloric intake on their up days, so that their up and down days averaged out to a “normal” 1,600 calories per day. In other words, there was no overall reduction in calories at all.
Although others have interpreted this study to show that the diet subjects were receiving 35 percent less than their normal calorie intake, their interpretation is based on a mistranslation that led them to conclude that the control subjects (those who were not on the diet) were consuming 2,300 calories daily. But Vallejo does not state that in his article. He simply states that the control group was fed the same food as the diet group on a daily basis (meaning they would have taken food that totaled 1,600 calories on average per day).
For comparison, the most recent Dietary Guidelines for Americans produced by the U.S. Department of Health and Human Services recommend an average calorie consumption for sedentary people over age fifty-one of 1,800 calories per day (men 2,000 and women 1,600). These modern-day Americans are both taller and heavier, with a BMI of 26 to 27, than Spaniards born in the 1870s and 1880s. The point is, even by today’s standards, 2,300 calories would be much too high an estimate of average daily calorie need.
Unfortunately, Dr. Vallejo did not comment on the body weight of his subjects, presumably because it didn’t change. But if their caloric intake had been reduced by 35 percent, as suggested by some authors, these elderly people would have lost 80 pounds in the first year of the study.
Frankly, my colleague Dr. Laub and I find it impossible to imagine that Dr. Vallejo, the nuns of St. Joseph who ran the old-age home, the patients themselves, or their families would have permitted such systematic starvation to occur.
How Much Longer Would Vallejo’s
Subjects Live?
Normally, in animal studies, the lengthening of lifespan in calorie-restricted animals is expressed as a percentage increase over that of a control group. In other words, all the animals in the study die at various ages, which are plotted on a graph like the one below. All the animals are alive as shown on the y-axis at the beginning of the study, and as time passes on the x-axis all of them die eventually. The difference is that the calorie-restricted animals live about 40 percent longer—that is, they die at later ages. For example, a mouse species that lives 2 years on average would live 2.8 years when calorie restricted.
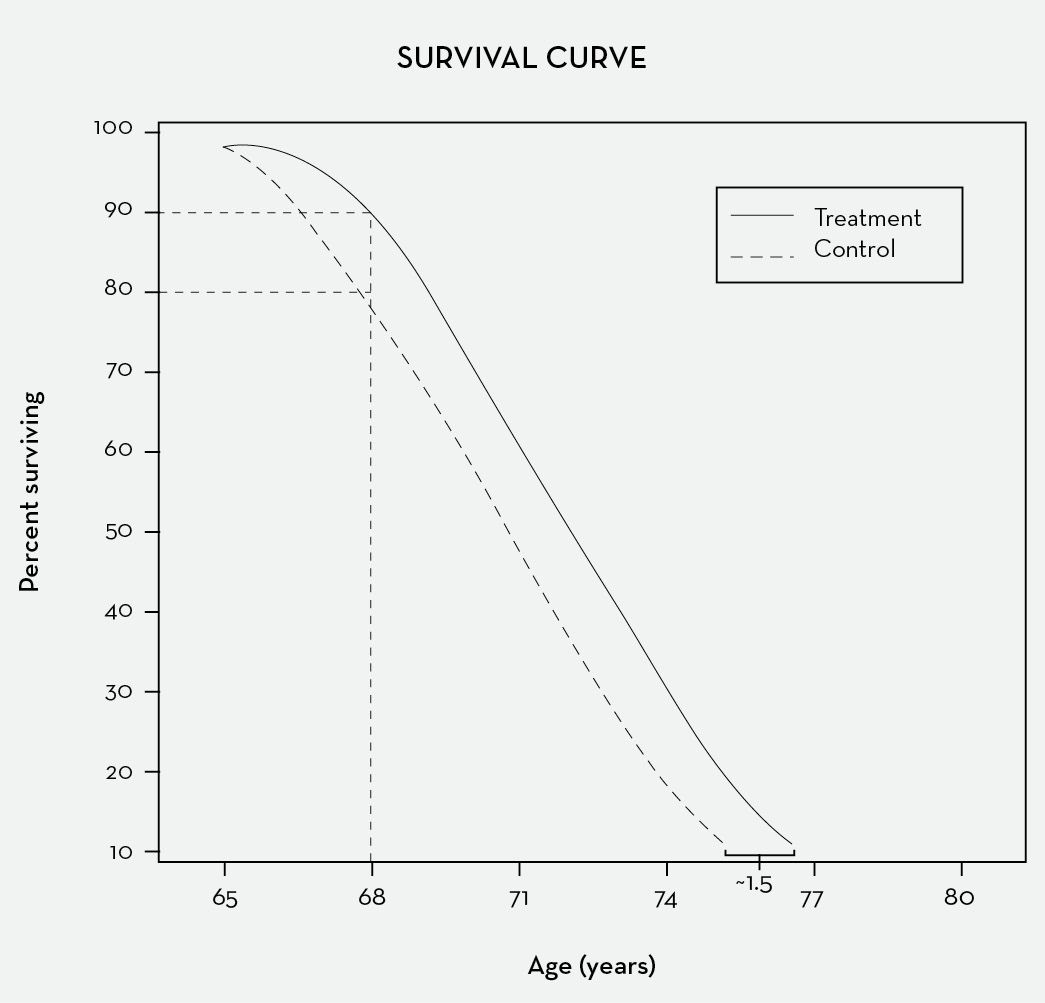
If we reconstruct the mortality curve for those in the Vallejo study, we see that these human subjects followed the same pattern. In 1957 the average life expectancy in Spain was 69.7 years. When we plot the death rate for the two groups, we see a shift to the right of approximately eighteen months for the diet group, indicating a 50 percent prolongation of life among those who followed the diet over the entire three-year period. This is only an educated guess and pertains only to the duration of the study, but it is in the same general range as the effect of calorie restriction on other species.
The study lasted three years, after which the two groups were compared. The diet group spent a total of 123 days in the hospital, while the control group spent a total of 219, and there were six deaths among the dieters as opposed to thirteen among the control group. In short, the diet reduced the likelihood of severe illness and death by half, as compared with the controls.
What Caused These Deaths?
The biggest differential between the two groups in the Vallejo study was in the number of deaths from heart disease. There were three myocardial infarctions (heart attacks) among the diet group as opposed to five among the control group. In addition, there were four cases of congestive heart failure among the control group and none in the diet group. Therefore, the total number of deaths from heart disease in the control group (9) was three times greater than those among the diet group (3).
As we’ve discussed, there have been a number of studies showing the profound ameliorative effects of intermittent feeding on the central nervous system in animals. In the heart there are specialized fibers constituting a conduction system that transmits electrical impulses to the heart muscle in an orderly way to produce a normal heart rhythm. These fibers function much like nerves, and Dr. Laub and I believe that, like nerves, they were probably affected by the up-day down-day pattern of the Vallejo study. Because many deaths from myocardial infarction are due to abnormal heart rhythms, which would be minimized if the conduction fibers were healthier, we speculate that the primary protective effect the diet had on heart attacks as well as on congestive heart failure resulted from its beneficial effect on this conduction system.
Looking at the figures for cancer deaths—two in each group—it would initially appear that the diet did not protect against cancer. But cancer is a disease that may be present in the body for years before it becomes apparent, and the three-year duration of the study might have been too short a time to have had an impact on the development of the disease. In fact, as we have seen, other studies do show a strong protective effect against cancer from calorie restriction in animals, and there is also extensive human data to show that people who eat less have lower rates of cancer.
Finally, among the nonfatal illnesses for which the subjects in the Vallejo study were treated, there were eight cases of bronchitis (an infectious disease) in the control group and three in the diet group. My own observation has been that there is a marked reduction in the incidence and severity of upper respiratory infection among people following the Alternate-Day Diet, and, in fact, members of the Calorie Restriction Society report that they have many fewer colds than they did before they began to practice Calorie Restriction.
Calorie-restricted animals have also been shown to have a reduction in infectious disease, which appears to result from a healthier immune response. For example, although the number of circulating lymphocytes (a type of white blood cell that defends against infection and tumors) in calorie-restricted animals is reduced by one-third, the lymphocytes are more effective than those in unrestricted animals.
WHAT IF YOU DON’T GORGE?
In both Mattson’s mouse study and Vallejo’s human study, test subjects ate more than their normal calorie requirement on the days when their feeding was not restricted, and yet they still showed significant health benefits as compared with their control groups. When I considered this evidence, it seemed clear to me that alternate-day feeding, even without calorie reduction or significant weight loss, could improve health and extend longevity in much the same way as daily restriction.
More recently, there has been one additional study done on humans subjected to alternate-day fasting. In this study, conducted in early 2005 by the world-renowned metabolic researcher Eric Ravussin and his associates at the Pennington Biomedical Research Center in Baton Rouge, Louisiana, sixteen people of normal weight (eight men and eight women) were put on an alternate-day fasting regimen for three weeks. On the fast day, they were allowed to consume only calorie-free soft drinks, tea, coffee, and sugar-free gum. On the alternate days they could eat whatever they wished. At the end of the study they had all lost weight, indicating, according to the researchers, “that the subjects were unable to consume enough food on the feasting days to maintain their weight.” But the researchers also noted that “a prolonged schedule of fasting and feasting would be marred by aversive subjective states (e.g., hunger and irritability), which would likely limit the ability of most individuals to sustain this eating pattern.” In other words, they were saying that no one would eat that way willingly.
When I first conceived of the Alternate-Day Diet in 2003, I had independently decided that most people would be unlikely to tolerate a down day of less than 20 percent of their normal calorie intake for any substantial period of time, so I was pleased to note that Ravussin concluded his article by saying that “adding a small meal (10 to 20 percent of caloric needs) to the fasting day may make alternate-day fasting more acceptable in all populations.”
I had asked myself, “What would happen if one severely restricted calories on alternate days without actually fasting and didn’t overeat or gorge on the up days?”
Using myself as a test group of one, I put myself on a diet of 20 percent of normal calories on alternate days, figuring that this would be restrictive enough to trigger the health benefits seen by Mattson and Vallejo without actually fasting. On the days when I wasn’t restricting, I ate as I normally would. Initially, I made little effort to follow a healthy diet. In fact, I didn’t hesitate to eat McDonald’s fries or (my personal favorite) Popeye’s spicy fried chicken.
Interestingly, I discovered that I wasn’t excessively hungry and wasn’t tempted to overeat on the up days to “make up for” the days when I was eating very little. And I found it relatively easy to muster the willpower to comply with my self-imposed regimen, because I knew that I’d never be depriving myself for more than one day at a time.
As I’ve already said, I lost 35 pounds within the first 11 weeks of my new diet, and other markers of health, including my cholesterol and triglyceride levels, improved and have remained so.
MY PERSONAL WEIGHT-LOSS EPIPHANY
What started as a personal experiment to measure the possible health benefits of an alternate-day calorie-restriction pattern became something else. I eventually realized that alternate-day dieting was the only way I had ever been able to lose weight and maintain the weight loss. Since May 2003, I have personally put many hundreds of people on the diet, and thousands of others who learned about the diet have shared their Alternate-Day experiences online in a variety of blogs.