Chapter 1
Development of the Epidemic
Overview
The commonest mode of transmission of the virus is through sexual intercourse
The growth of the epidemic has appeared to stabilize
HIV continues to exhort a huge public health and economic burden
In 2009, there were 33.3 million people living with HIV worldwide
Sub-Saharan Africa has experienced a disproportionate burden of the global HIV epidemic
10 million people who are eligible for treatment under World Health Organization guidelines are still in need of treatment
The first recognized cases of the acquired immune deficiency syndrome (AIDS) occurred in the summer of 1981 in the USA. Reports began to appear of Pneumocystis carinii (now known as jirovecii) pneumonia and Kaposi sarcoma in young men, who it was subsequently realized were both homosexual and immunocompromised. Even though the condition became known early on as AIDS, its cause and modes of transmission were not immediately obvious. The virus, human immunodeficiency virus (HIV), now known to cause AIDS in a proportion of those infected, was discovered in 1983. Subsequently a new variant has been isolated in patients with West African connections, HIV-2.
Thirty years on and with the introduction of combination antiretroviral therapy (cART), where it is widely available, the clinical picture of HIV has changed from a fatal illness to that of a chronic condition. There has been an increase in the number of people living with diagnosed HIV as a result of fewer deaths from AIDS and ongoing high rates of HIV diagnosis. In developed countries, where cART has been available from its inception, an ageing cohort is now seen, and people with HIV are living near-normal life expectancies. Consequent to this has arisen the challenges of managing the co-morbidities associated with age and the long-term consequences of cART. Despite this, more than 10 million people worldwide who require cART are not able to access it, and HIV continues to exhort a huge public health and economic burden. The last decade has seen consistent global efforts to address health, development and the HIV epidemic, starting with the United Nations (UN) Millennium Development Goals (MDGs). Despite extensive progress, many countries have failed to achieve MDG Six, which is in part to halt and reverse the spread of HIV (Box 1.2)
HIV has been isolated from semen, cervical secretions, lymphocytes, cell-free plasma, cerebrospinal fluid, tears, saliva, urine and breast milk. This does not mean, however, that these fluids all transmit infection, as the concentration of virus in them varies considerably.
Particularly infectious are semen, blood and possibly cervical secretions. Infection can occur after mucosal exposure to infected blood or body fluids.
The commonest mode of transmission of the virus throughout the world is through sexual intercourse. Unprotected anal and vaginal intercourse carry the highest risk of transmission, and the promotion of condom use has been the focus of prevention efforts.
Transmission also occurs through the sharing or reuse of contaminated needles by injecting drug users, which continues to drive the epidemic in Eastern Europe.
Transmission from mother to child occurs in utero, during labour and through breastfeeding. Transmission rates can be between 15% and 45% without intervention, and less than 5% with effective interventions. Mother-to-child transmission (MTCT) of HIV still significantly contributes to child mortality worldwide. However, the increase in access to services for preventing MTCT has led to fewer children being born with HIV. Use of cART during pregnancy, and at the time of birth, has been the mainstay of intervention strategies (see Chapters 17 and 18). In the UK, universal antenatal screening and access to cART have virtually eliminated MTCT. Globally, an estimated 370 000 children were newly infected with HIV in 2007, a fall of 24% from 5 years previously. UNAIDS called for the elimination of new paediatric HIV infections by 2015. It recommends that countries adopt a policy that HIV-positive mothers or their infants take ART while breastfeeding to prevent HIV transmission.
Contaminated blood products have previously contributed to the transmission of HIV, but universal screening has almost eliminated this mode of transmission in developed countries. Healthcare workers can rarely be infected through needlestick injuries and skin and mucosal exposure to infected blood or body fluids.
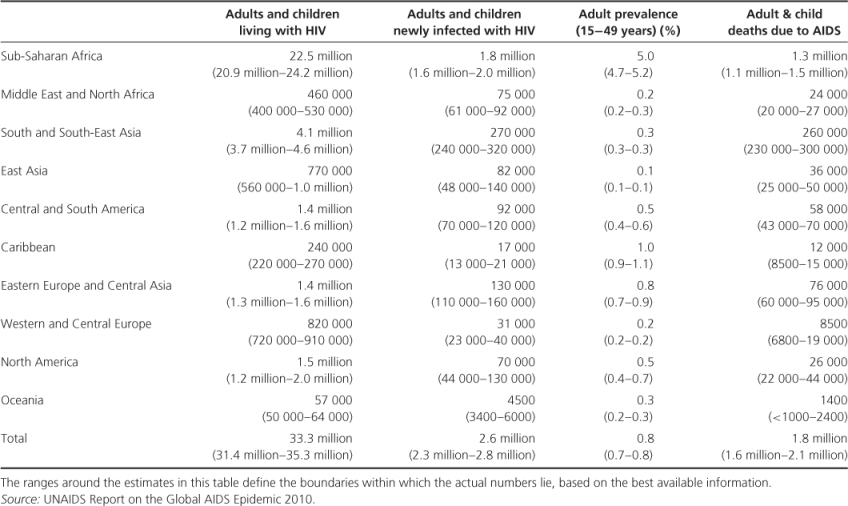
The growth of the epidemic has appeared to stabilize. Globally, there are fewer AIDS-related deaths and a steady decline in the number of new HIV infections since the late 1990s. In 2009, there were 33.3 million people living with HIV. There were 2.6 million new infections, which is 21% fewer than in 1997 (3.2 million) when the number of new infections reached its peak. HIV remains undiagnosed in 40% of people. The HIV incidence in 33 countries has fallen by 25% between 2001 and 2009, with 22 of these countries being in sub-Saharan Africa. However, in seven countries there has been an increase of more than 25% in the same time period. These include five countries in Eastern Europe and Central Asia.
Table 1.1 Regional HIV and AIDS statistics 2009.
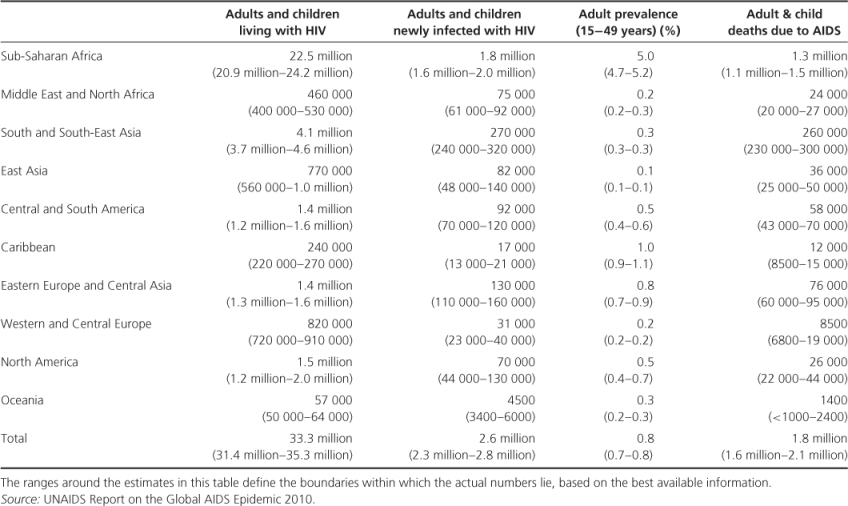
Figure 1.1 Estimated adult and child deaths from AIDS, 2009.
Even though North America and Europe experienced the first impact of the epidemic, infections with HIV are now seen throughout the world, and the major focus of the epidemic is in resource-poor countries.
The number of people living with HIV in North America and Western and Central Europe has increased, with a 30% rise since 2001, and reached an estimated 2.3 million people in 2009. Heterosexual transmission represents about 50% of new HIV infections. In 2007, almost 17% of these new infections were among people from countries with generalized epidemics. The data are indicative of a resurgence of the HIV epidemic among men who have sex with men (MSM) in North America and Western Europe. Between 2000 and 2006 there was an 86% rise in the annual number of new HIV diagnoses in this risk group.
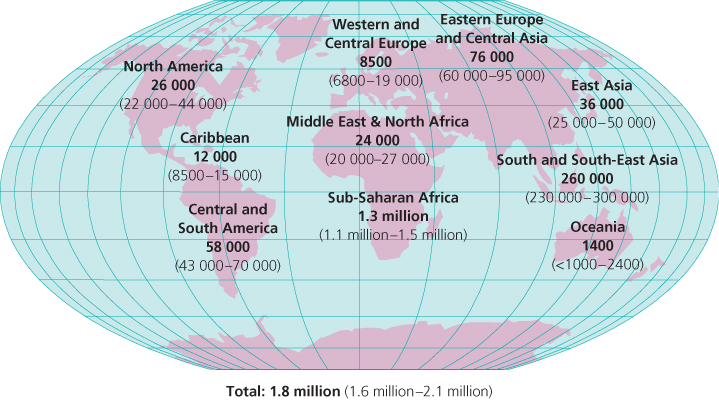
In the UK, the Health protection Agency (HPA) predicts that by 2012 the number of people living with HIV will continue to rise and reach 100 000. In 2009 there was an estimated 86 500 people thought to be living with HIV, 26% of these with undiagnosed infections. Among those with diagnosed HIV, 43% are MSM, 51% are heterosexuals and 2% are injecting drug users (Table 1.2).
Table 1.2 Cumulative reported cases of diagnosed HIV by exposure category in the USA and UK, 2009.
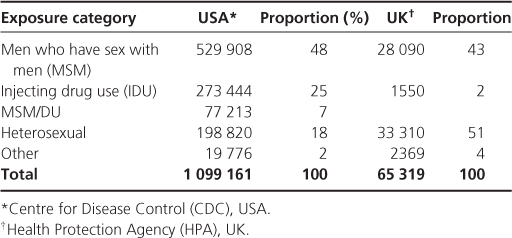
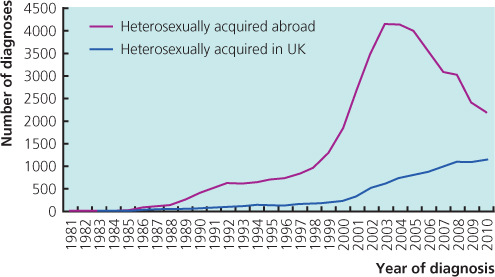
In 2010, the largest number of new diagnoses of HIV in the UK was recorded among MSM (Figure 1.2). Most infections among heterosexuals were acquired abroad, the majority from sub-Saharan Africa. There is a downward trend in the numbers of infections acquired abroad, thought to be due in part to changes in immigration policies (Figure 1.3).
Figure 1.2 Annual New HIV diagnoses among men who have sex with men, UK, 1981–2010.
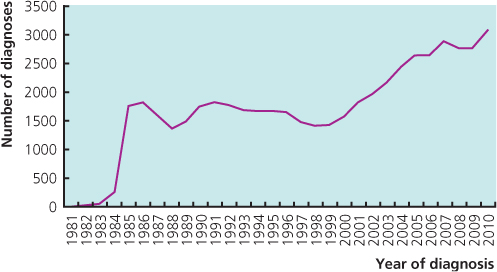
Figure 1.3 Annual New HIV diagnoses acquired heterosexually, UK, 1981–2010.
In the USA there were an estimated 1,099,161 people living with HIV by the end of 2009 (Table 1.2), 48% among MSM, 25% in injecting drug users and 18% in heterosexuals. HIV disproportionately affects racial and ethnic minorities, with 45% of newly infected people in 2006 arising from the African-American population.
In the developing world, HIV is spread mainly through heterosexual intercourse. The epidemic in this region has been driven by a combination of poor economies and an absence of functioning health systems leading to lack of access to early diagnosis and cART.
Sub-Saharan Africa has experienced a disproportionate burden of the global HIV epidemic (Box 1.4). In 2009, 22.5 million people were living with HIV in this region, accounting for 68% of the global total. Swaziland has the highest adult prevalence of HIV in the world, with an estimate of 25.9%. Southern Africa is still the most affected by the HIV epidemic, with an estimated 11.3 million people living with HIV in 2009, an increase of more than 30% in 10 years. South Africa's epidemic remains the largest in the world (Box 1.5). However, there is an indication of slowing of HIV incidence in Southern Africa as well as in East Africa. The HIV prevalence in Kenya fell from 14% in the mid-1990s to 5% in 2006.
There has been little change in the HIV epidemic in Central and South America, with an estimated 1.4 million people living with HIV. One third of those affected live in Brazil. The HIV rates in this region have been contained largely by the availability of cART and early HIV prevention and treatment strategies.
The epidemic in Asia is stable, with an estimated 4.9 million persons living with HIV in 2009. Thailand has the highest prevalence in the region, with a prevalence of 1%. The HIV prevalence is increasing in Pakistan, Bangladesh and the Philippines, but still remains low in these countries. There was a 25% decrease in HIV incidence in India and Nepal between 2001 and 2009. There are wide variations in the epidemic in Asia, both within and between countries and risk groups. For example, in China, five out of 22 provinces account for more than 50% of people living with HIV.
There has been an almost threefold increase between 2001 and 2009 in the number of people living with HIV in Eastern Europe and Central Asia, with an estimate of 1.4 million in 2009. The Russian Federation and the Ukraine account for 90% of these people with new HIV diagnoses. The epidemic in this region has been driven mostly by infections among injecting drug users, sex workers and their partners. An estimated 37% of people who inject drugs in the Russian Federation are thought to have HIV, with estimates in the Ukraine ranging from 39% to 50%. The upward trend continues, and the interaction between injecting drug use and sex work is fuelling the epidemic in this region.
National policies have influenced the HIV epidemic in certain regions. Needle exchange programmes are an effective strategy to prevent onward transmission of HIV among injecting drug users and have been adopted in many countries. However, in others, such as the Russian Federation, there is a lack of political will to implement these programmes, with only an estimated 7% of injecting drug users able to access needle exchange programmes, which are mostly run by non-governmental organizations. This situation is reflected across most of Eastern Europe and Central Asia, and has contributed to the rise in the number of HIV infections in this region.
Immigration policy can also influence the nature of regional epidemics. In the UK, for example, the fall in the number of new HIV infections acquired abroad amongst heterosexuals since 2002 has been in part due to the change in UK immigration policy to immigrants from sub-Saharan Africa.
The HIV epidemic has had a profound influence on the economic and political structures of many developing countries, particularly in sub-Saharan Africa (Box 1.6). The UNAIDS estimates that in 2010 there were approximately 20 million children in sub-Saharan Africa who had lost at least one parent to AIDS. This not only represents a breakdown in family structure but also the loss of a whole generation of young working adults, resulting in devastating consequences for already struggling economies. Population growth and death rates are increasingly affected. Countries with an adult prevalence of over 10% are expected to see an average reduction in life expectancy of 17 years by 2015.
Source: World Health Organization (WHO) Trade, foreign policy, diplomacy and health: HIV and AIDS. http://www.who.int/trade/glossary/story051/en/index.htm.
Despite these large numbers there has been a decline in people with new HIV infections, in large part due to public health efforts of health promotion and education strategies, such as condom use and addressing the issue of concurrent partners, as well as the availability of cART. In South Africa there are indications of a paradigm shift towards safer sex among young people. In Zimbabwe there are proportionally fewer men with casual partners and there is higher condom use between regular partners.
Treatment 2.0 (Box 1.7) is a new approach from UNAIDS and its partners to simplify the way HIV treatment is provided and to scale-up access to medicines. Mathematical modelling suggests that Treatment 2.0 could avert an additional 10 million deaths by 2025, compared to current strategies.
Globally, more than 5 million people are receiving HIV treatment. Since 2004 there has been a 13-fold increase in the number of people receiving cART, representing more than 5 million people. Access to cART is thought to have contributed to a 19% decrease in deaths among those with HIV. However, 10 million people who are eligible for treatment under WHO guidelines are still in need of treatment, the majority of whom are in developing countries. Forty per cent of people with HIV are undiagnosed, resulting in presentation at a late stage in the disease course and poorer outcomes. This is in part due to inadequate healthcare systems and persistent stigma in many countries, particularly those in Africa.
National and international policy efforts need to be redoubled to ensure there is access to early diagnosis and treatment. Political and health infrastructures need to be strengthened to deliver public health messages and much needed healthcare. These are essential to controlling and reversing the trend of the current HIV epidemic.
The data on AIDS/HIV is reproduced with permission from the Health Protection Agency and the United Nations AIDS Programme.
UNAIDS. UNAIDS Report on the Global AIDS Epidemic 2010. (www.unaids.org/globalreport/Global_report.htm).
UNAIDS. UNAIDS in 2011. (www.unaids.org/en/resources/presscentre/featurestories/2010/december/20101230unaidsin2011).
WHO. HIV/AIDS. (www.who.int/topics/hiv_aids/en).
Centre for Disease Control and Prevention (CDC). HIV/AIDS Statistics and Surveillance. (www.cdc.gov/hiv/topics/surveillance/index.htm).
Health Protection Agency (HPA). HIV in the United Kingdom, Report 2010. (www.hpa.org.uk/web/HPAweb&HPAwebStandard/HPAweb_C/1287145264558).
Mathers BM, Degenhardt L, Ali H, et al. for the 2009 Reference Group to the UN on HIV and Injecting Drug Use. HIV prevention, treatment and care services for people who inject drugs: a systematic review of global, regional, and national coverage. Lancet 2010;375:1014–1028.