CHAPTER 5
Hypertension, High Cholesterol, Spastic Heart, Angina, Arrhythmia, Arteriosclerosis, and Heart Attack
THREE THINGS YOU NEED TO KNOW ABOUT MAGNESIUM AND HEART DISEASE
Magnesium prevents muscle spasms of the heart blood vessels, which can lead to heart attack.
Magnesium prevents muscle spasms of the peripheral blood vessels, which can lead to high blood pressure.
Magnesium prevents calcium buildup in cholesterol plaque in arteries, which leads to clogged arteries.
Annette was tired of people’s shocked reaction when they learned that she was recovering from a heart attack. She knew that the common image of heart disease was that it targeted aggressive, overweight men who smoked and ate too much. Annette, on the other hand, was slim, reserved, and a vegetarian who ate a low-fat diet. She chuckled when friends tried to tell her about the Dr. Dean Ornish vegetarian diet for reversing heart disease, because she’d lived according to that diet.
She was only fifty-six, a nonsmoker, with exemplary cholesterol, but she did have slightly elevated blood pressure, her only risk factor. Yet she had had a mild heart attack. Now she suffered from daily palpitations and was on several medications that seemed to drain her energy more with every passing day. She was also simply too afraid to exert herself for fear of bringing on another heart attack.
Annette was becoming an invalid, and at her next appointment her cardiologist was shocked at her worn-out appearance. He decided to run some blood tests and was urged by a student doctor to order the new ionized magnesium test. The results of that test were so low that the lab rushed the results to him the next morning. His nurse immediately called Annette to come in, saying the doctor had found something that would help her feel better. Annette was prescribed a magnesium preparation that she mixed with water (Slow-Mag) that began to work within twenty-four hours. She was amazed that her muscle aches, insomnia, palpitations, and fatigue all but disappeared. She was even able to cut back on her other medications. Her doctor vowed to test all his patients’ magnesium ion levels from then on, and wondered aloud if it had been
AN IMPORTANT REMINDER ABOUT TAKING MAGNESIUM WITH PRESCRIPTION DRUGS
You may experience a decreased need for your drugs as magnesium deficiency is corrected or as magnesium treats your symptoms or reverses your condition. In other words, the symptoms for which the drug was prescribed may clear up due to the magnesium, making the drug unnecessary or toxic and causing new symptoms. Patients and doctors should be on the alert for a shift in symptoms. Be sure to work with your doctor to lower your medication doses safely.
low magnesium in the first place that had led to Annette’s heart attack.
As we will learn in Chapter 7, obstetricians are quite familiar with the use of magnesium for hypertension in women about to deliver. Unfortunately, they aren’t talking to cardiologists or even to family doctors about the importance of magnesium in treating general hypertension, one of the main risk factors for heart disease.
Heart disease is the number one killer of both American women and men, accounting for half of all U.S. deaths (52.3 percent of the total deaths occurring in women compared to 47.7 percent in men). According to the American Heart Association, every thirty-three seconds someone in the United States dies of cardiovascular disease; that’s approaching one million deaths annually. Hypertension occurs in fifty million Americans and accounts for an estimated 29.3 million office visits a year to allopathic doctors (M.D.’s)1 Antihypertensive drug prescriptions are given at most of these appointments, even though magnesium has been used successfully for over half a century by medical doctors, osteopaths, and naturopathic doctors.2,3
THE SLIPPERY ROAD TO HEART ATTACK
STEP ONE: LOSS OF ARTERIAL ELASTICITY
The coronary arteries bringing oxygen-filled blood from inside the heart through the aorta to the heart muscle are very, very small, only about 3 mm across (a nickel is 2 mm thick). It doesn’t take much to plug them up with a tiny blood clot or to imagine them collapsing when in spasm. Magnesium prevents blood clot formation and artery spasm. These coronary arteries get even smaller as they split into two, then four, then eight and so on as they descend toward the bottom of the heart. Each of these splits is called a bifurcation. According to cardiologists, about 85 percent of sclerotic plaques initially form near bifurcations. It is widely believed that the development of these plaques is a response to injury. This means that something, such as an infection, may be damaging the arteries, rather than just fat and calcium building up like silt in a river.
Endothelial cells are a single layer of specialized cells that form the inside membrane of an artery. The subendothelial layer (the next layer in) is a very thin connective tissue that contains elastin. As its name implies, this is the layer responsible for providing much of the elasticity in your arteries. It is important to note that your body requires magnesium to maintain healthy elastin.
Smooth muscle cells are the next layer. Smooth muscle cells provide integrity and control the dilation of the arterial cavity, triggered by the calcium/magnesium ratio in the body. Calcium causes contraction and magnesium causes relaxation, which together control the blood pressure and flow in the artery. A final messenger for the dilation response is nitric oxide, which is dependent on magnesium.
One of the earliest signs of magnesium deficiency is degeneration of elastin in the subendothelium. Animals on low-magnesium diets lose the elasticity of their arterial system. Coronary arteries require even more elasticity than other arteries because they must stretch and flex as the heart expands and contracts. Loss of elasticity results in inflammation of the endothelial and subendothelial layers at points that are most mechanically challenged by stretching the bifurcations. Imagine a small rubber-band-like tube shaped like a Y. In your mind’s eye-grasp the two legs of the Y in one hand. With your other hand, grip the single leg. Begin pulling them apart just as though they were stretching on the surface of the heart. Stretch it as far as you can. Where is the shape weakest? If we left the rubber tube out in the sun for a week or so, what would happen if you slowly stretched it again? Where might you expect the first crack to appear? Most of the time it would happen at or near where one tube becomes two—at the bifurcation. If your artery loses elasticity, it makes sense that the problem might show up at or near the bifurcation.
STEP TWO: THE INFLAMMATORY RESPONSE
Inflammation begins with injury of the artery wall, leading to white blood cells and cholesterol hovering around trying to heal the damage. At this stage in the process, if there is too much calcium and not enough magnesium in the bloodstream, excess calcium precipitates around the area of inflammation in the artery wall. The area becomes rigid and interferes with blood flow.
STEP THREE: HEART ATTACK
Over time, the above steps weaken and plug the coronary arteries and slowly kill small areas of the heart muscle. The final result is severe chest pain, damage to a larger portion of heart muscle, and heart attack. 4
Some of the first evidence for the use of magnesium against heart disease came from epidemiological studies in Wales, Taiwan, Sweden, Finland, and Japan showing that death rates from coronary heart disease are higher in communities with magnesium-deficient water and magnesiumdeficient diets. 5 Areas where calcium in the water is much higher than magnesium or where dietary intake of calcium is higher than magnesium showed even more coronary heart disease. A U.S. study done over a seven-year period followed fourteen thousand men and women and concluded that low magnesium in the diet may contribute to the origin of coronary atherosclerosis and acute heart attack.6
The Centers for Disease Control and Prevention in Atlanta followed twelve thousand people for nineteen years, at the end of which 4,282 people had died, 1,005 from heart disease. Risk of dying from heart disease was highest in those with magnesium deficiency. Researchers made a conservative estimate that 11 percent of the half a million people dying of heart disease in 1993 could have been directly related to magnesium deficiency.7 If more accurate measurements for magnesium deficiency were used, such as ionic magnesium testing, we would find the numbers to be even higher and the need for magnesium even greater.
The evidence has been mounting for decades that magnesium plays a crucial role in the prevention of both atherosclerosis and arteriosclerosis. 8,9 It maintains the elasticity of the artery wall, dilates blood vessels, prevents calcium deposits, and is necessary for the maintenance of healthy muscles, including the heart muscle itself. For all these reasons, magnesium is critical to the maintenance of a healthy heart. 10 One of the pivotal metabolic chemicals in the body is nitric oxide (NO). It is a very simple compound made from nitrogen and oxygen, but it packs a powerful punch. Nitric oxide controls vasodilation, but this activity is under the direction of magnesium.11
HIGH CHOLESTEROL
The upper limit of normal cholesterol is 200 mg/dl, but it appears that over time, with the average cholesterol in the general population becoming more elevated, the values that medicine accepts as normal have risen. Some doctors are taking a stand and revising the upper limit of normal down to 180 mg/dl. As with hypertension, the actual cause of most cases of high cholesterol is said to be unknown. High cholesterol tends to run in families and occurs in association with low thyroid hormone production or hypothyroidism, liver disease, and pregnancy.
There are several types of cholesterol with different functions, some of which we label good and some bad. Cholesterol associated with high-density lipoprotein, HDL, is generally considered to be beneficial to the body. It apparently functions to remove other cholesterol or fatty deposits from blood vessel walls and the blood itself, bringing it to the liver for processing and excretion. Low-density lipoprotein, LDL, is commonly thought to be harmful to the body because it carries cholesterol into the bloodstream, promoting the buildup of cholesterol plaque on the arterial walls. Very-low-density lipoproteins, VLDLs, are made into LDLs in the liver and are also thought to be harmful.
But all of these cholesterols are normally found in the body. What’s not normal is the high amounts of oxidized cholesterol (cholesterol abnormally bound with oxygen) that we eat in processed foods, fast foods, and fried foods. In addition, chlorine, fluoride in water, pesticides, and other environmental pollutants can also oxidize cholesterol in the body. It is this oxidized cholesterol that researchers are concerned about when it comes to heart disease. 12 Regular use of antioxidants such as magnesium, vitamin E, vitamin A, vitamin C, and green tea can lower oxidized cholesterol levels. There is compelling evidence that magnesium therapy reduces cholesterol levels, 13,14,15 even when there is a genetic risk factor present for hypercholesterolemia. 16
There are no visible symptoms of high cholesterol beyond the associated signs of a bad diet, sedentary lifestyle, smoking, alcohol intake, and stress. A poor diet with a high intake of saturated and polyunsaturated fats, hydrogenated oils, fried foods, meat, sugar, coffee, and alcohol will elevate cholesterol levels, especially when a person lacks fiber from whole grains and vegetables. Add a sedentary lifestyle, and cholesterol increases. The very diet that promotes elevated cholesterol also causes magnesium deficiency. Unfortunately, many doctors do not have the time or inclination to educate patients about correct eating habits that could reduce their cholesterol, instead using medication to treat the problem. To be fair, many patients don’t have the inclination to comply even if their doctor recommends a diet, exercise, and weight loss. Adding magnesium supplementation to lifestyle changes, however, gives patients more dramatic improvement, making compliance easier.
Many of us have been conditioned to believe that elevated cholesterol is the only cause of heart disease; that is why marketers have been so successful in getting us to replace the saturated fat of butter with hydrogenated vegetable oils. Yet epidemiologists and dental anthropologists proved long ago that various world cultures that ate high-cholesterol diets for thousands of years (including meat, lard, cream, butter, and eggs) suffered very little, if any, heart disease.17 Almost all the long-lived, healthy communities where degenerative disease and heart disease were unknown included significant amounts of natural, unprocessed meat or dairy in their diets. And it is also clear that once a country is exposed to refined and processed food, or
A major disadvantage of low-fat products is that they contain extra sugar in order to capture the taste buds. Even worse is aspartame, a synthetic sweetener with a daunting list of ninety-two side effects to its name. To maintain your health, avoid both.
“altered” meat and “altered” dairy, health declines in a number of ways.18,19,20 Hydrogenated oils are unsaturated oils and for that reason were thought to be healthier than saturated fats such as butter. But the processing of liquid vegetable oil by heat, pressure, and chemicals to change it into a solid fat creates an unhealthy synthetic product called a trans fatty acid (as opposed to the natural cis fatty acid). Only in the late 1990s did we find out that these highly refined hydrogenated oils themselves promote atherosclerotic plaque much more than butter. In fact, some scientists say that the rise of myocardial infarctions, and heart disease in general, can be traced back to the 1930s, when hydrogenated oils were first introduced. We now know that trans fatty acids cause arterial damage and cancer. Be sure to read labels to avoid this substance.
HOMOCYSTEINURIA
Dr. Kilmer McCully was the first researcher, back in 1969, to identify a condition of increased levels of an amino acid, homocysteine, in the urine of patients with heart disease, which could be reversed with certain nutrients. 21,22 Homocysteine is a normal by-product of protein digestion, which in elevated amounts causes oxidized cholesterol, which damages blood vessels. (See page 89 for a definition of oxidized cholesterol.) For certain individuals who lack specific enzymes for protein digestion, homocysteine can become a real problem.
NORMAL LIPID VALUES
Cholesterol: 180 mg/dl
HDL cholesterol: greater than 45 mg/dl
LDL cholesterol: less than 130 mg/dl
VLDL cholesterol: less than 35 mg/dl
Total-cholesterol-to-HDL ratio: in men the optimal ratio is less than 3.43 (average = 4.97); in women the optimal ratio is less than 3.27 (average = 4.44)
A healthy level of homocysteine is below 12 micro-moles per liter of blood (12 μmol/L). Homocysteine levels greater than 12 μmol/L are considered high. Twenty to 40 percent of the general population have elevated levels of homocysteine. Individuals with high levels have almost four times the risk of suffering a heart attack compared to people with normal levels.23 Elevated homocysteine is high on the list of risk factors for heart disease and serves as an even stronger marker than high cholesterol for heart disease and blood clotting disorders.24,25
The more relevant marker, in my opinion, is low magnesium, since the major enzymes involved in homocysteine metabolism are magnesium-dependent. 26 McCully blames too much protein in the diet for elevated homocysteine. However, when magnesium, vitamin B6, vitamin B12, and folic acid are deficient, the body is not able to properly digest protein. The B vitamins were readily available in the typical diet a hundred years ago; now that they’re absent from the diet, homocysteine becomes elevated and heart disease results. When these metabolic nutrients are reintroduced through diet or supplements, the high homocysteine levels are reversed and the symptoms of heart disease diminish. Ongoing research confirms that B6, B12, and folic acid together with magnesium are necessary to prevent blood vessel damage induced by high levels of homocysteine in the blood.27 In short, the successful treatment of homocysteinemia relies on dietary changes that include B vitamins and magnesium.28,29,30
It must be remembered, however, that high homocysteine is also a marker for all causes of mortality and signifies that a deficiency in essential nutrients has a far-reaching effect on the body beyond heart disease. 31
ATHEROSCLEROSIS
It is easy to confuse the terms arteriosclerosis and atherosclerosis ; in fact, many people use them interchangeably. Arteriosclerosis is the overall term for sclerosis or scarring of the arteries. Atherosclerosis is scarring or thickening specifically due to fatty plaques. When the diameter of an artery is narrowed by fat deposits, a blood clot or an arterial spasm can be the final straw that results in angina, heart attack, or stroke. Complications of this preventable condition cause over a third of all deaths in the United States.
SUPPLEMENT AND DRUG INTERACTIONS IN HEART DISEASE
Calcium interacts with verapamil (Calan, Isoptin, Verelan). This is a calcium channel blocker, and calcium interferes with the hypotensive effect of this drug. Avoid calcium until your doctor weans you off this drug.
Vitamin B1 (thiamine) interacts with furosemide (Lasix). Lasix causes increased urinary excretion of B1 so supplements of this vitamin may be necessary.
Vitamin B6 interacts with hydralazine (Alazine, Apresazide, Apresoline, Unipres). Hydralazine causes increased excretion of vitamin B6; supplements of the nutrient may be necessary.
Calcium, magnesium, and potassium interact with furosemide, which causes urinary excretion of these minerals. Monitor levels of these nutrients and replace as necessary.
Grapefruit juice makes felodipine and nifepidine (Adalat, Procardia) more powerful; it increases the action of these drugs by temporarily blocking the enzyme that clears them from the body. You may have to avoid grapefruit juice while on these medications.
Magnesium, calcium, potassium, and sodium interact with thiazide diuretics such as chlorthiazide (Diuril, Aldoril, Diachlor) and hydrochlorthiazide (Hydrodiuril). Thiazides work by increasing urinary excretion of sodium, which presumably lowers blood pressure. However, significant amounts of calcium, potassium, and magnesium are also excreted. Magnesium at 600 mg per day may have to be increased to 900 mg if you are on thiazide diuretics or digitalis because both drugs cause excretion of magnesium. Your doctor should do an ionized magnesium test to determine your needs.
Potassium and magnesium deficiencies lead to arrhythmias in patients on digoxin (Lanoxin).
Small increases in plasma calcium increase digoxin (Lanoxin) toxicity. Some specialists advise avoiding high-calcium foods for two hours before and after taking this drug.
Calcium should be supplemented due to decreased absorption of vitamin D with patients using cholesterol-lowering drugs colestipol or cholestyramine.
Colestipol (Colestid) interferes with absorption of iron, folate, and vitamins A, D, E, and K.
Cholestyramine (Quesyran, Cholybar) interferes with absorption of iron, folate, and vitamins A, D, E, and K.
Heparin interferes with renal hydroxylation of vitamin D. This could lead to osteopenia; your doctor may need to check 1,25 (OH)2 D3 cholecalciferol levels.
Vitamin K inactivates coumadin (Warfarin); coumadin interferes with vitamin K synthesis.32
Researchers have identified various causes of damage to the inner wall of arteries, including homocysteine, an amino acid discussed earlier; infection by an organism called chlamydia; distorted blood flow around the mound of fat; free radicals; high blood sugar; high blood pressure; and lack of oxygen. As described previously, the damaged tissue of the artery wall initiates an inflammatory process. The inflammation then attracts bad cholesterol (LDL) and calcium, which build up into a solid scar. Magnesium has a role to play in reducing homocysteine levels, preventing free radicals, balancing blood sugar, and reducing high blood pressure.
HYPERTENSION
Hypertension is an elevation of blood pressure suffered by more than fifty million Americans. Normal blood pressure is 120–140 over 80–90. Systolic pressure is the first number and relates to the pump pressure that the heart muscle creates to push blood into the arteries. Diastolic pressure is the second number and is the pressure that the arteries maintain when the heart is relaxed, or between heartbeats, to keep the arteries open. Hypertension is either primary or secondary. Primary hypertension has no single cause and occurs in 90 percent of all hypertensive patients. Secondary hypertension is secondary to another disease. Causes of primary hypertension include high cholesterol, family history, obesity, diet, smoking, stress, and excessive salt intake. Most often, hypertension is diagnosed during a routine physical exam. It presents no distinguishing signs or symptoms unless the condition is very advanced, in which case headache, dizziness, and blurred vision can occur.
In Western medicine, the first line of drug treatment for hypertension is typically the use of diuretics, or water pills. When patients are prescribed diuretics, they are warned that the most common side effect is a deficiency of potassium, which spills out in the urine. To prevent it, they are advised to eat bananas and oranges. What they are not told is that magnesium is drained out along with potassium. Recall that magnesium deficiency leads to blood vessels that are less relaxed and more susceptible to spasm and tension, a precursor to hypertension; thus the very treatment for hypertension worsens the problem.33 (Ironically, replacing potassium doesn’t help patients who are also magnesium-deficient, because the body is unable to deliver potassium to the cells without sufficient magnesium. Also, the so-called potassium-sparing diuretics still commonly deplete other minerals, including magnesium.)34
If blood pressure is not controlled with diuretics, the next choice may be ACE inhibitors, calcium channel blockers, antiadrenergic drugs, or vasodilators. One cardiologist confided to me that if a patient’s blood pressure is still high after using five different antihypertensive drugs at one time, he then knows the problem is magnesium deficiency. Fortunately, other cardiologists know that magnesium is a physiological necessity and a pharmacological treasure to use before pharmacological intervention. They call magnesium the ideal drug: It is safe, cheap, and simple to use, with a wide therapeutic range, a short half-life, and little or no tendency toward drug interactions.35
Even before drugs, diet is the first treatment of choice for hypertension. Research shows a direct relationship between the amount of magnesium in the diet and the ability to avoid high blood pressure.36 The Alturas first demonstrated that diets deficient in magnesium will produce hypertension in experimental animals.37 Diet may lower the blood pressure successfully due to a combination of weight loss and increased intake of the vitamin and mineral cofactors necessary in blood pressure control. For example, increased levels of minerals such as potassium and magnesium in the diet have a suppressive effect on calcium-regulating hormones, which influence blood pressure. 38 The arterial blood pressure appears to go up as the levels of magnesium ions and total serum magnesium go down.39
Note: Some forms of severe high blood pressure are hereditary or due to kidney disease and do require medication. Also, if the arteries in the body are damaged from long-term atherosclerotic injury and scarring, unfortunately they may no longer respond to magnesium and you may require medications to keep your blood pressure under control.
ANGINA
Angina describes an episodic pain in the region of the chest and/or down the left arm, due to lack of oxygen to the heart muscle and a buildup of carbon dioxide and other metabolites. Usually the pain, which can be a mild ache, pressure, or fullness, or a crushing blow, comes on with exercise (especially in the cold), emotional stress, a heavy meal, or even a vivid dream, and is relieved (within five minutes) by rest and nitroglycerine.
The lack of sufficient blood flow carrying life-giving oxygen and nutrients can be due to blocked coronary arteries or spasms in these tiny vessels. Angina is labeled “unstable” when symptoms become more severe; unstable angina implies a greater risk for heart attack. Another type of angina is called Prinzmetal’s, which is angina that occurs at rest, rather than following some sort of physical stress. James B. Pierce, Ph.D., believes he has identified the cause of Prinzmetal’s, which occurs most commonly at two specific times in the day, early morning and late afternoon, when magnesium levels are at their lowest.40 Dr. Pierce estimates that up to 50 percent of sudden heart attacks may be due to magnesium deficiency. He found that magnesium worked better than nitroglycerine for his own stress-induced chest pains. In fact, Dr. Pierce could predict that he would get chest pain after a stressful day, a long drive, or an emotional upset and would increase his intake of magnesium to forestall symptoms.
Risk factors for angina include magnesium deficiency, smoking, diabetes mellitus, hyperlipidemia, type A personality, sedentary lifestyle, poor diet, and family history of coronary artery disease. Diagnosis of angina, to differentiate it from myocardial infarction and unstable angina, includes an EKG (electrocardiogram) taken during an angina attack; an exercise tolerance test, which is an EKG taken while on a treadmill; and a coronary angiogram (an X-ray view of dye in the coronary arteries) to assess whether the coronary arteries are open or blocked.
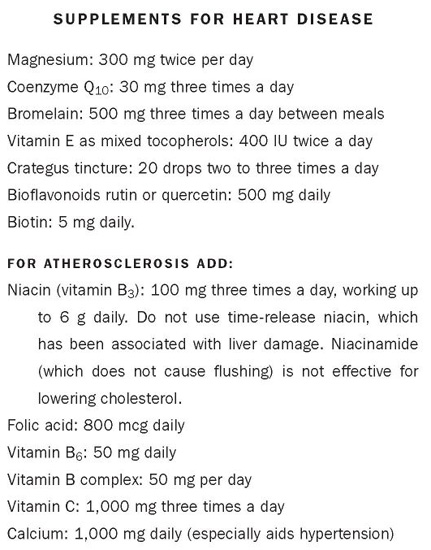
Once angina is diagnosed, the recommendations are universal: stop smoking, lose weight, get blood pressure under control (with or without drugs), and in extreme cases of arterial blockages, undergo bypass surgery to remove blocked arteries. The best treatment for angina, however, is prevention. By eliminating sugar, alcohol, and junk foods from your diet you help prevent heart disease, because these foods have no magnesium and serve only to create magnesium deficiency. When you eat a more balanced, non-processed-food diet, you have a better chance of increasing your magnesium intake. With magnesium and other heart-healthy supplements, a healthy diet and exercise regimen, you have a fighting chance of avoiding this epidemic. See page 108 for a list of supplements to cover all aspects of heart disease.
HEART ATTACKS
Myocardial infarction (MI), or heart attack, causes permanent damage to the heart muscle and requires immediate hospitalization. MI is the result of coronary artery disease due to atherosclerosis or due to spasms caused by magnesium deficiency. The artery may be damaged gradually by plaque, suddenly go into spasm, become blocked by a blood clot, or a combination of the above, often accelerated by excessive emotion. The calcified atherosclerotic plaque, the arterial spasm, and even the blood clot are all caused or worsened by magnesium deficiency.
Laboratory findings distinguish a heart attack from an episode of angina on the basis of heart muscle damage and certain heart enzyme levels that become elevated several hours after a heart attack and remain elevated for several days. The immediate treatment for an acute heart attack usually includes anticoagulant drugs in an intravenous drip. Intravenous magnesium given as soon as possible after a heart attack, however, may provide the best protection for the heart. Oral magnesium treatment also inhibits blood clots in patients with coronary artery disease whether the patient is on aspirin therapy or not.41 As more doctors read the considerable research on magnesium they are incorporating magnesium into their intravenous and oral protocols for heart patients.
Magnesium has been studied for its effects on the heart since the 1930s and used by injection for the treatment of heart conditions since the 1940s.42,43 Magnesium’s lifesaving effects have been confirmed and reconfirmed in many clinics and laboratories. For example, in an analysis of seven major clinical studies, researchers concluded that magnesium (in doses of 5–10 g by intravenous injection) reduced the odds of death by an astounding 55 percent in acute MI.44,45 Over the past decade, several large clinical trials using magnesium have shown its beneficial effects: If intravenous magnesium is given (1) before any other drugs and (2) immediately after onset of a heart attack, the incidence of high blood pressure, congestive heart failure, arrhythmia, or a subsequent heart attack is vastly reduced. One such study, called LIMIT-2, provided powerful evidence that early magnesium administration protects the heart muscle, prevents arrhythmia, and improves long-term survival.46,47,48 Magnesium might improve the aftermath of acute heart attack by preventing rhythm problems; improving blood flow to the heart by dilating blood vessels; protecting the damaged heart muscle against calcium overload; improving heart muscle function; breaking down any blood clots blocking the arteries; and reducing free-radical damage. Magnesium may also help the heart drug digoxin to be more effective in the treatment of cardiac arrhythmia;49 without enough magnesium, digoxin can become toxic.50
The suggested criteria for magnesium intervention were not followed in a very large trial called ISIS-4, and the outcome did not show the same results as the LIMIT trial.51 In the ISIS trial, magnesium was given many hours after the onset of symptoms and after blood clotting had begun. The two trials were as dissimilar as apples and oranges, yet the debate over magnesium’s efficacy still rages. Since the LIMIT and ISIS studies, several smaller trials have shown even greater recovery from heart attacks using intravenous magnesium, including a trial of two hundred people with a 74 percent lower death rate.52
Pharmaceutical companies, who want to promote their own drug therapies, cite the ISIS trial as proof that magnesium sulfate doesn’t work; supporters of magnesium cite the LIMIT trial as proof that it does. Your doctor may even be influenced by the ISIS trial and think magnesium is not an important option in your care. But cardiologists who are looking for alternatives to drug therapy and to its many side effects, and who read studies thoroughly, are using it. To help you find these doctors, there is a list in the Appendix of complementary medicine associations whose doctors study alternatives to the drug-based medicine they learned in medical school. Because one of the major side effects of heart medications, especially diuretics, is magnesium deficiency, it is vital that magnesium be tested with an ionized magnesium test and supplemented in heart patients who are on medication. The dosage ranges from 6 to 10 mg/kg/day (300–1,000 mg per day), but this should be taken only under a doctor’s supervision if you are on any other heart medications. See page 108 for magnesium dosage.
SPASTIC HEART
Between 40 and 60 percent of people who suffer sudden heart attacks may actually have no arterial blockage or history of irregular heartbeats. 53 Two suspected causes are spasms in the coronary arteries and the occurrence of a severe heart rhythm disturbance, such as atrial fibrillation. Both of these conditions can be caused by a deficiency of magnesium. Low magnesium makes the heart muscle hyperirritable, leading to the development of a rhythm disturbance that can’t be stopped without emergency medical intervention. An astute physician recognizes the possibility of magnesium deficiency and immediately gives magnesium intravenously, as in the LIMIT trial. Rapid heartbeat or atrial tachycardia, premature beats, and atrial fibrillation have all responded to treatment with IV magnesium.54,55,56
The most common time for the onset of heart attacks is around 9 A.M. on Mondays as people gird themselves for another long workweek. 57 As mentioned earlier, people who suffer from spasm-induced angina attacks most often experience them at the same time each day, usually in the morning and late afternoon, when magnesium levels are at their lowest. The morning deficiency is likely the result of overnight fasting and the loss of magnesium through the urine. Deficiency in the afternoon may be caused by depletion of magnesium induced by the stress of the day and not yet replenished by the evening meal. In view of this, it seems reasonable that people with angina, heart spasms, hypertension, or heart disease should consult with their doctors, take an ionized magnesium test, and, if it shows a deficiency, take at least 200 mg of magnesium three times each day; before breakfast, at 2 P.M., and before going to bed.
ARRHYTHMIA
Magnesium’s ability to neutralize the heart-damaging effects of catecholamines (the products of stress-induced adrenaline and cortisol) is the miracle that can prevent many of the side effects of acute heart attack such as arrhythmia. 58 Magnesium deficiency contributes to abnormal heart rhythms, possibly because magnesium is responsible for maintaining normal potassium and sodium concentrations inside heart muscle cells. A balance of potassium, sodium, calcium, and magnesium allows for normal heart muscle contraction and maintains normal heartbeat. A central pacemaker within the heart muscle creates a normal pumping action that travels across the heart; cardiac arrhythmia occurs when other, less suitable areas of the heart are forced to assume the role of the central pacemaker when it becomes damaged or irritated by lack of oxygen due to blocked blood vessels, caused by drugs (including coffee), hormonal imbalance, or deficiency of magnesium. These new pacemakers are even more sensitive to magnesium deficiency and are responsive to magnesium therapy that has been successfully used for over sixty years. 59 Magnesium is also an accepted treatment for ventricular arrhythmias, 60,61 congestive heart failure where the heart is weak and unable to empty after each heartbeat,62,63 and before and after heart surgery, including coronary bypass grafting.64,65,66 All these studies indicate that the frequency of ventricular arrhythmias is reduced by administration of intravenous magnesium and support an early high-dose administration of intravenous magnesium in the wake of myocardial infarction.
MITRAL VALVE PROLAPSE
Magnesium deficiency has been implicated in mitral valve prolapse (MVP), a disorder in which the mitral valve fails to completely close off one of the heart chambers during heart contraction. It is also called floppy valve syndrome. Blood rushing through the open valve can be heard as a heart murmur with a stethoscope. When cardiac ultrasound became more commonplace, the diagnosis of MVP escalated, especially in young women. There is no allopathic treatment for the condition, and in mild and even moderate cases it doesn’t cause any symptoms. However, patients are usually warned that they should take antibiotics when having dental work done to prevent the possibility of bacteria from the gums being picked up in the bloodstream and lodging on the prolapsed valve, causing infection. This is a very rare occurrence and some doctors disapprove of this overuse of antibiotics, but it remains a potential liability threat to dentists who don’t warn their patients.
Dr. Melvyn Werbach, author of Nutritional Influences on Disease, believes that MVP is overdiagnosed and also maintains that it is a magnesium deficiency disease that is well treated by magnesium. The valves of the heart are pulled tight by muscles, which, like any other muscle in the body, depend on magnesium for proper functioning. The mitral valve prolapses because it is not held tight. Mildred Seelig reports that low magnesium levels have been found in as many as 85 percent of MVP patients.67 Sixty percent of 141 individuals with strongly symptomatic MVP had low magnesium levels, compared to only 5 percent of the control group. Magnesium supplementation given for five weeks reduced the symptoms of chest pain, palpitation, anxiety, low energy, faintness, and difficulty breathing by about 50 percent.68
CHELATION THERAPY
Even alternative medicine can make more use of magnesium. Chelation therapy is an intravenous treatment with a chemical called EDTA that pulls out excess calcium and iron from the body to treat atherosclerosis and heart disease. It would be much more convenient to use magnesium as part of an oral chelation protocol preventively, to keep calcium from building up in the first place. When intravenous EDTA is used, however, generous amounts of magnesium are given as well.
DIET FOR HEART DISEASE
A good diet is based on chicken, fish, whole grains, legumes, fruit, and vegetables. Therapeutic foods high in magnesium should be included: garlic, onions, nuts, seeds, wheat germ, and sprouts. Don’t fall into the trap of blaming cholesterol above all else. Using margarine is not the answer to heart disease. The proper dietary fats for human consumption are butter, olive oil, flaxseed oil, and coconut oil. The diet for all forms of heart disease should exclude alcohol, coffee, white sugar, white flour, fried foods, and trans fatty acids (found in margarine, baked, fried, and processed foods).