TO FULLY UNDERSTAND the central importance of the role of the gut in your health and wellness, and how it is of key importance to the Mind Body Cleanse ethos, we must first explore how it works. Then, in Part 2, we show you how the 12-Day Plan can help you if you are struggling with sluggish intestines and other gut-related conditions.
The strength of a tree does not lie in its limbs or branches, but in its roots. And the root system of the human body is not found in the hand or in the feet, but in the digestive organs. Like the roots of a tree, the digestive organs process food, extract vital nutrients and deliver them to the rest of the organism. They also excrete the rubbish generated by metabolism.
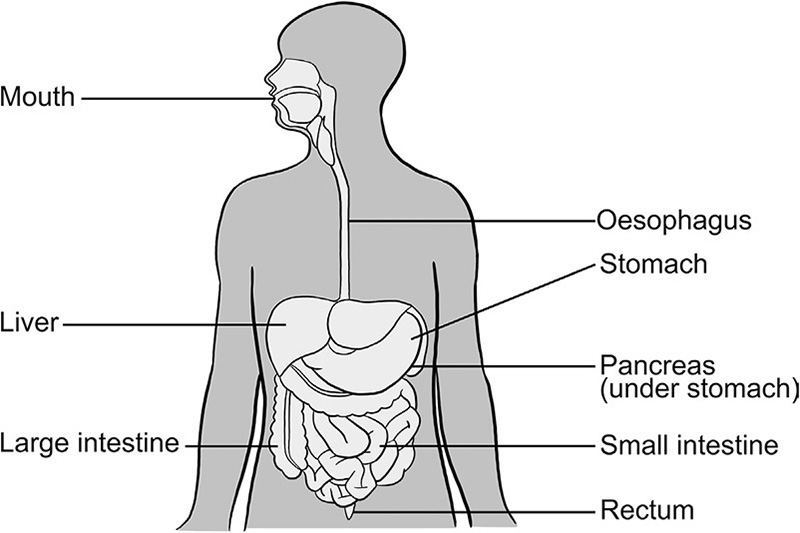
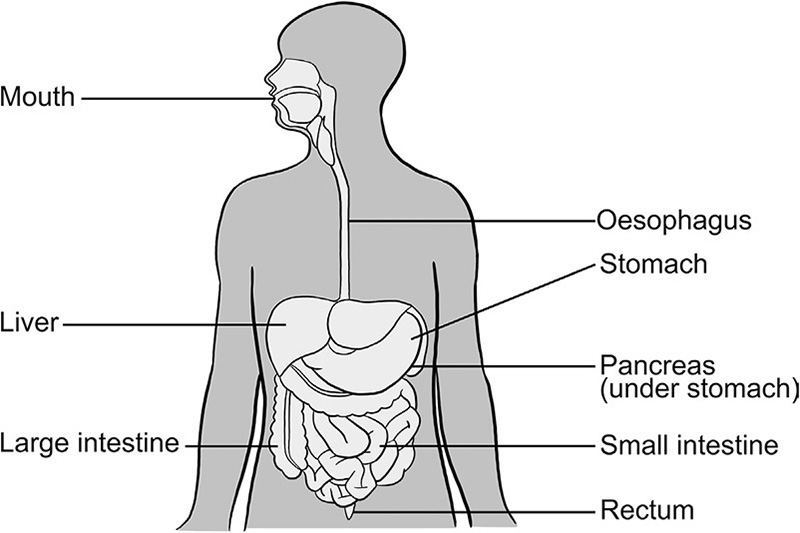
The digestive system is a tube-shaped canal, which is up to 27 feet long in adults. The surface area of the gut is 200 times greater than the skin, making it the largest surface of interaction with the world. It begins at the mouth and ends at the anus and includes the oesophagus, stomach, and small and large intestines. The liver, the gall bladder, the pancreas, as well as billions of mucus glands in the stomach and intestines, are each a part of it. Just as the roots of a plant absorb nourishment from the earth, producing branches, leaves and blossoms, millions of intestinal villi take root in the chyme, absorbing food that has broken down in the gut and supply it to the bloodstream, which in turn carries it to the 60 trillion cells of the human body.
‘The intestines are the Father of all suffering.’
OLD ARABIC SAYING
Digestion begins in the mouth with the production of ptyalin, a digestive enzyme secreted at the very first sight, smell or even thought of food.
Masticating your food thoroughly is key to good digestion and food should enter the stomach as a thick liquid, not hastily swallowed, unchewed chunks or lumps. The papillae in your cheeks and beneath your tongue secrete around 0.7 litres of saliva every day, which starts off the digestive process.
If you explore the root of the tongue with your finger, you will notice bumpy nodules. This area, known as the lingual tonsils, contains immune tissue. The job of these nodules is to analyse tiny particles of everything that you eat. Before we reach about seven years of age, our tonsils are still an important training camp for our immune cells. Building a strong immune system is key to keeping the heart healthy and in controlling body weight. It is worth noting that removing the tonsils of a child younger than age seven can lead to an increased risk of obesity.
On the arrival of the bolus of food, the oesophagus choreographs a wave-like action to draw the food downwards towards the stomach. This propulsive peristalsis is so much a part of our physiology that it even works if you are standing on your head. In this first part of the digestive journey, the conscious peripheral nervous system and the autonomic nervous system – or that part of the nervous system that we can influence – work in harmony.
The position of the stomach is much higher in the upper body than we realise. It begins at the left nipple and ends below the bottom of the ribcage, on the right-hand side, behaving a bit like a washing machine, slapping and turning, churning and walloping food against its back wall to ensure that it can be absorbed in the small and large intestines. From here, food particles are ground into tiny particles that then pass into the small intestine.
Liquid travels down the shorter right-hand side of the stomach to end up at the entrance to the small intestine. Food, on the other hand, travels against the larger side of the stomach and gets smashed to the sides.
Immediately before food arrives in the stomach, the latter relaxes so that it can stretch and extend for as long as it needs to. Emotions such as anxiety or fear inhibit the stomach from relaxing, which can stop us feeling hungry or make us feel nauseous. If you have difficulty winding down and relaxing before eating, I recommend a few different short breathing practices before eating, which influence the rest and relaxation response. These simple practices ensure that everything in the stomach is working in the way that it should before you eat (see Three-part breath and complete breath, here).
Stress not only affects your mental state but can also take its toll on your physical wellbeing. It can negatively affect every part of your digestive system, causing your gut, and especially your colon, to spasm or even increase the acid in your stomach, causing indigestion.
The pH of the stomach is very acidic and activates peptidases that begin to break down proteins. While simple carbohydrates, such as pasta or rice, pass into the small intestine quite quickly, proteins and fats need a great deal more work to process them, which requires greater energy. This is why I recommend not eating animal protein during the 12-Day Plan. A piece of steak, for example, may easily be churned around in the stomach for between five and seven hours and therefore consumes too much energy.
The acidic environment of the stomach is also a first line of defence against harmful bacteria in our food. In the stomach, carbohydrates break down into glucose. Protein is broken down into amino acids, the building blocks of muscle and tissue.
Ninety per cent of all foodstuffs are absorbed through the wall of the small intestine, where bacteria that naturally live in our gut begin fermenting and feeding off our food. The small intestine is between 3 and 6 metres long. As food moves into the small intestine, the pH changes from being acidic to more alkaline. The small intestine absorbs, through billions of finger-like projections called villi, the nutrients derived from the combination of mono-saccharide carbohydrates, which come from vegetables and fruits are easy to digest – with proteins from animal sources and essential fats found in fish, nuts and seeds. In the final stages of food breakdown in the small intestine, our digestive enzymes work like tiny scissors and break down food to the same basic ingredients: sugar molecules, amino acids and fats. The villi help to move the chyme down the digestive line, where everything is moving forwards. The action of peristalsis is greatly enhanced by Mind Body Cleanse twisting movements, which you will find in Part 2 (see here, here and here). These yogic twisting poses bring intelligence into the gut and the action of pushing and pulling with the breath in turn speeds metabolism and digestion.
The health of the large intestine is dependent on the smooth functioning of all the digestive functions in harmony.
The large intestine is the home of our gut flora, dealing with anything that gets swept into the large intestine undigested, and it needs time to complete this action. Water is absorbed and any remaining nutrients, including energy-rich fatty acids, vitamin K, vitamin B12, B1 and B2. The colon takes its time with all the leftovers and digests them thoroughly. During this time it processes calcium, which can only be absorbed properly in the colon. Everything is then screened by the liver before entering the main blood system.
The large intestine, unlike other parts of the gut, also has to deal with the brain directly: it is the brain that decides when it wants to make the colon evacuate its contents, not the large intestine. Sometimes, when we are anxious, the brain orders the large intestine into evacuation, without sufficient time to reabsorb all the water the body lent it. The result is diarrhoea. This is why engaging with the parasympathetic branch of the autonomic nervous system (R&R response) before eating as described in Part 2 (see three-part breath and complete breath, here) is key if you are prone to runny tummies.
On average, food movement from fork to toilet can take one day, while those who provide the intestine with sufficient bulk may have to go to the toilet two or three times a day. Slower guts can take as many as three to four days for the food to pass through. Generally speaking, women’s large intestines are slightly slower than men’s.
ARE YOU SITTING COMFORTABLY?
Even in our modern world, most people, globally, still defecate in the squatting position – especially in Asia, the Middle East and Africa. It is only in the industrialised West, where the modern toilet, or ‘throne’, was invented, that people sit on something in order to defecate, using the same posture as when they sit down on a chair to eat.
Anatomically speaking, the ‘throne’ is a device of considerable torture to the bowels. When sitting on a ‘throne’, the lower end of the descending colon is bent, requiring a major muscular effort to evacuate the bowels. The intense effort required can lead to clogging the minute capillaries that feed the anal sphincter, and this may lead to the formation of haemorrhoids and bleeding piles.
When squatting, however, the colon naturally aligns itself with the rectum and anus, and no, or very little, effort is required for evacuation. In fact, you will evacuate so much more in a single, efficient squatting than you will in a single sitting. No wonder so many in the Western world suffer from chronic constipation!
In southern India, nearly 20 years ago, I was in a place called Patnem. I rented a beach hut and on the first night I was given a pig. I couldn’t quite work out what this pig was for until the following morning, when I went to perform my ablutions. There are no Western-style toilets in that part of India, and I had become quite used to squatting to eliminate waste. It had even begun to feel quite comfortable – until I saw the pig’s snout and two eyes peering up at me expectedly through the hole in the toilet bowl!
LET’S GET THINGS MOVING
Increasing fibre
Unless you are attempting to target a specific health goal, such as lowering your cholesterol, which requires more soluble fibre, in general focus on eating foods that span the colours of the rainbow. This way you will be getting all the soluble and insoluble fibres required for a healthy diet in the phytonutrient spectrum. The best way to increase your fibre intake is to gradually incorporate more foods in this list (see here). If you are increasing the intake of fibre in your diet, make sure you increase your water intake too. Not drinking enough water when increasing fibre intake can lead to constipation.
The issue of constipation
The best barometer for assessing constipation is not how often you need to go to the toilet, but how difficult it is. Temporary constipation can be due to stress, travelling or illness. Prolonged symptoms can point to more serious conditions.
You can try the following to get things moving:
> Take psyllium husks and/or prune fibre. Both contain fibre and also draw extra fluids into the gut. Be patient – it can take three days to take effect.
> Drink more fluids – this may be very helpful. Air travel can cause the body to lose water, without even sweating, so it’s vital to drink plenty of water before, during and after flights.
> Try not to put yourself under pressure to go to the loo; your gut likes to work according to plan so if you need to go, just go!
The most common effect of sluggish bowels is the formation of toxins from decomposition. Just as butter goes rancid and fruit begins to ferment, and while meat goes bad, likewise a sluggish intestine forms poisons. This may lead to gastritis and gastroptosis, intestinal ulcers and various diseases of the intestines. Fasting and cleansing should be done as a preventative measure.
The pancreas secretes pancreatic juice, which is alkaline, to neutralise the acid from the stomach. It performs two major tasks. It produces:
 Enzymes (for digestion); protease (for proteins); amylase (for carbohydrates); and lipase (for fats) to aid digestion in the small intestine
Enzymes (for digestion); protease (for proteins); amylase (for carbohydrates); and lipase (for fats) to aid digestion in the small intestine
 Hormones: insulin to help regulate blood-sugar levels by transporting glucose to the brain and muscles for energy, and leptin to tell your brain when you are full.
Hormones: insulin to help regulate blood-sugar levels by transporting glucose to the brain and muscles for energy, and leptin to tell your brain when you are full.
In the liver, bile salts serve to emulsify fats from the food we eat. Eating the right kind of fat feeds the body with nutrient-dense compounds that are vital for the brain and nervous system and helps to produce hormones. The liver is also the primary organ of detoxification, processing all toxins that we absorb from the environment.
COLONIC HYDROTHERAPY
Colonic irrigation cleanses the entire colon from the ascending portion across the transverse portion to the descending portion of the colon. The procedure must not be confused with enemas (at best, enemas flush out the rectum and a small part of the descending colon, but they do not reach the transverse and ascending portions).
Colonic hydrotherapy should work entirely by gravity rather than via pumping and it is vital that it is administered by a professional. You can use ARCH, which is registered in the UK and Europe.
Russian physicians realise that no cure for any ailment can be properly administered to an ‘unclean’, highly toxic, body, which simply cannot assimilate medication.
So in Russia it remains standard procedure in all hospitals and clinics to administer a thorough colonic cleansing to all patients, regardless of their ailments, immediately upon arrival.
The multiple functions of the gut interact with each other and with the food you eat to regulate your nutrition, metabolism, mental function, weight, energy and your susceptibility to illness.
 Your gut has its own nervous system, the enteric nervous system (ENS), which has as many nerve cells as your spinal column and has constant contact with your brain. This has a direct impact on your mood and mental function.
Your gut has its own nervous system, the enteric nervous system (ENS), which has as many nerve cells as your spinal column and has constant contact with your brain. This has a direct impact on your mood and mental function.
 Your gut is also home to about 100 trillion microbes and lives in a symbiotic relationship with favourable bacteria, yeast and fungi, viruses and an occasional worm. This is called the ‘microbiome’.
Your gut is also home to about 100 trillion microbes and lives in a symbiotic relationship with favourable bacteria, yeast and fungi, viruses and an occasional worm. This is called the ‘microbiome’.
 Over two-thirds of your body’s immune system is found in the lining of the small intestine. Thus your gut is the largest immune barrier to the outside world.
Over two-thirds of your body’s immune system is found in the lining of the small intestine. Thus your gut is the largest immune barrier to the outside world.
 The gut is also an organ of detoxification. Much of this responsibility rests with the liver, but the intestinal lining cells are themselves rich in detoxifying enzymes.
The gut is also an organ of detoxification. Much of this responsibility rests with the liver, but the intestinal lining cells are themselves rich in detoxifying enzymes.
The state of your guts affects how you feel in your mind. It can be either a source of suffering or of extraordinary wellness. The gut is home to an unimaginable number of nerves and it commands fleets of signalling substances and connections.
Just as the brain has its own nervous system, the central nervous system (CNS), the gut has its own nervous system called the enteric nervous system (ENS). Both systems originate from the same embryonic tissues and in life share a certain synchronicity.
The ENS has a number of key functions. It:
 Controls the immune system in the gut
Controls the immune system in the gut
 Coordinates the release of hormones as food arrives
Coordinates the release of hormones as food arrives
 Helps to open up the gut to circulation after you eat, which help absorption of nutrients
Helps to open up the gut to circulation after you eat, which help absorption of nutrients
 Choreographs and coordinates the contraction of the muscle cells that line the intestines to keep everything moving in the right direction (i.e. out of the body).
Choreographs and coordinates the contraction of the muscle cells that line the intestines to keep everything moving in the right direction (i.e. out of the body).
The ENS is autonomous. If the connection between the enteric nervous system and the brain is severed at the vagus nerve, the gut will continue to function as if nothing has happened. It will even continue to digest food! This is unique to the ENS and is found nowhere else in the body.
The gut is affectionately referred to as the ‘second brain’ and the conversation that takes place between the first brain and the second brain is actually a two-way-highway conversation, although it has to be said that 90 per cent of the conversation is from the gut to the brain.
‘The state of your guts affects how you feel in your mind.’
The insular cortex part of the brain needs information from the vagus to form a picture of how the body is doing. So, while the vagus nerve works like a telephone cable between the switchboard, or brain, the ENS gathers information from the gut. This makes the gut the largest sensory organ to the outside world. The information that the ENS gathers is used by the conscious mind.
A healthy gut does not transmit unimportant signals from the gut to the brain via the vagus nerve. However, if the gut thinks that something is important, it may require the brain’s input rather than process it with its own brain.
The gut is not only the seat of your health, it is also the seat of your intuition; a huge matrix that senses our inner life working on the subconscious mind.
Human beings have an innate ability to process information about what’s going on around them and put a response into action separate from the brain and the central nervous system.
Listening to your gut is a very visceral activity; it is like having a sixth sense. In fact, listening to gut feelings is the most powerful guiding ally we have – ignoring them often leads to suffering. Cooperation between the gut and brain begins very early in life. When we are children we have not yet evolved the analytical brain to override what we are truly feeling and are adept at responding to the impulses from the gut, but as we get older we experience the world more through our senses.
BUTTERFLY FEELINGS
Have you ever felt ‘butterflies’ in your tummy? Underlying this sensation is an often-overlooked network of neurons lining the gut.
You don’t have to be a gastroenterologist to be aware of the more subtle feelings in your stomach that accompany emotions such as excitement, fear and stress. The second brain consists of sheaths of neurons embedded in the walls of the long tube of our gut, or alimentary canal. The second brain contains some 100 million neurons, more than in either the spinal cord or the peripheral nervous system. It is this multitude of neurons in the enteric nervous system that enables us to ‘feel’ the inner world of our gut.
You can become more sensitive to the mind – gut connection. The Mind Body Cleanse techniques that we look at in Part 2 will help you to explore and strengthen this vital connection.
As adults we have to practise letting go of the analytical and over-thinking mind and trust in our intuition, especially when it comes to assessing potentially threatening situations. The process of making decisions based on gut feeling may involve the gut recalling how it felt in similar situations in the past. This is why yoga and meditation are such good, effective practices – because they allow us to step back, drop the analytical mind and tune in to our intuition. Therefore developing our intuition, with the help of techniques described in the second half of this book, allows us to have more control over our own health.
‘Listening to your gut is a very visceral response; it is like having a sixth sense.’
I was recently delivering a presentation on Mind Body Cleanse techniques, in leafy south-west London. A top fashion designer was in the audience and needed encouragement to sit still. I said to the lady: ‘You are 90 per cent bacteria, and 10 per cent human.’ As you would imagine, this did not go down too well. Most people do not like to think of themselves as consisting mostly of bacteria, and for this reason the fashion designer looked aghast, but at last started to pay attention to the presentation!
Viewed at great magnification, bacteria resemble bright little spots against a black background. The microbiome and its role in maintaining health and healing disease is one of the greatest medical discoveries in modern science. It comprises all the microorganisms inhabiting us.
‘You are 90 per cent bacteria, and 10 per cent human.’
There is an inconceivable number of microbes in the gut and, according to recent research, humans are made up primarily of bacterial cells that control virtually every aspect of our physiology. It is vital to our wellness that we shatter the myth that bacteria are the ‘enemy’. The bacteria of the microbiome are actually our greatest allies when it comes to improving health.
If you lifted out your gut, you would find that your microbiome weighed up to two kilos and contain about 100 trillion bacteria. One gram of faeces contains more bacteria than there are people on earth.
Some scientists now support the theory that our gut microbiota can be considered an organ in its own right. It has an origin, develops with us, is made up of trillions of cells, and is in constant contact with its fellow organs.
Bacteria help to:
 Break down foodstuffs
Break down foodstuffs
 Supply the gut with energy
Supply the gut with energy
 Manufacture vitamins
Manufacture vitamins
 Train our immune system.
Train our immune system.
The precise nature of the creatures that colonise us makes a difference to our wellbeing. Varying proportions of different bacteria in our gut have been detected in those suffering from obesity, nervous disorders, depression and even malnutrition. So, when something is wrong with our microbiome, something is wrong with us!
Science is just beginning to understand that we are all individual ecosystems:
 The numbers of bacteria are greater in the colon and rectum, rather than higher up in the gut.
The numbers of bacteria are greater in the colon and rectum, rather than higher up in the gut.
 Bacteria do not like to be removed from their own world and it is very difficult to observe them.
Bacteria do not like to be removed from their own world and it is very difficult to observe them.
 Our gastrointestinal tract is home to more than a thousand species of bacteria – plus populations of viruses and yeasts and fungi.
Our gastrointestinal tract is home to more than a thousand species of bacteria – plus populations of viruses and yeasts and fungi.
 If we allow the wrong bacteria to colonise our gut, which produces a variety of different toxins, we may end up with all sorts of behavioural and emotional problems. Our brain chemistry can be changed for the worse.
If we allow the wrong bacteria to colonise our gut, which produces a variety of different toxins, we may end up with all sorts of behavioural and emotional problems. Our brain chemistry can be changed for the worse.
 If you add this deteriorating condition to the immune response, which includes the effects of inflammation, this can affect the brain too, with the result that your central nervous system becomes inflamed.
If you add this deteriorating condition to the immune response, which includes the effects of inflammation, this can affect the brain too, with the result that your central nervous system becomes inflamed.
The brain cannot work effectively unless it is working in an environment that is anti-inflammatory. And to work on the brain you have to start with the gut.
The moment each of us passes through the birth canal, a unique combination of microbes from our mother’s vagina initiates the process of colonising our bodies, both inside our airways and digestive tract, and outside on our skin. Up until this point we live in an environment that is germ-free inside our mother’s womb. At the age of three our gut flora develops to the right level and then stabilises, after our bacterium has gone through the wars, so to speak. And so begins the long process of bacterial colonisation, the composition of which depends upon our own actions – largely due to what we put in our mouths!
One-third of all children in the Western, industrialised, world are born via Caesarean section. And these children, including myself, have to garner bacteria from somewhere, since their population will not develop from the mother’s vagina. Children born by Caesarean section take much longer to develop a normal population of gut bacteria. They also have an increased risk of developing allergies or asthma.
Breastfeeding promotes specific members of our gut microbiotica, such as bifidobacteria. These bacteria are integral to the development of the immune system in later life. Interestingly, children with insufficient bifidobacteria have an increased risk of developing obesity in later life.
While our genes help to design our bodies, they do not design our microbial home. Taken together, our gut bacteria have 150 times more genes than a human being. This massive collection of genes is called a ‘biome’. And their genes represent a huge pool of borrowed abilities.
Our bacterial colonies change with lifestyle, diet and our exposure to antibiotics. This microbiome of 100 trillion tiny creatures dictates how our bodies feel, how our immune systems behave, and how we digest foods. However, we are only at the beginning of learning how the bacteria of the gut can have an effect on an adult human.
The idea that the bacteria in our gut might influence our overall metabolism, and therefore our weight, is only a recent phenomenon. A hypothesis postulated in 2013 suggests that gut bacteria can affect the appetite of the host. It is our bacteria that reward us when we send them a decent delivery of food. They do this by cranking up the body’s production of certain transmitters. This principle applies to the feeling of satiety.
When we consider the range of functions carried out by our microbiome, it is not surprising that these microbes are able to express their wishes too. We do, after all, live symbiotically with our bacteria.
The nutrition we receive from bacteria is not only important for fighting flab, it also affects the levels of fats, such as cholesterol, in our blood.
Obesity and high cholesterol are connected with the greatest health issues of our time: hypertension, arteriosclerosis and diabetes.
CHOLESTEROL-LOWERING BACTERIA?
The early indications are that the bacterium Lactobacillus plantarum can significantly lower high cholesterol and other blood lipid levels, increase ‘good’ HDL cholesterol and lead to significantly lower rates of arteriosclerosis.
Follow-up research still needs to be carried out to verify these promising indications. Lactobacillus plantarum is already recommended as a pain treatment for patients with IBS.
Our bacteria do not take anything from us when they share food. Remember that 90 per cent of our digestion takes place in the small intestine, where we absorb most of our nutrients, whereas the highest concentration of bacteria is found where digestion has nearly finished. If this equilibrium is disturbed and bacteria migrate to the small intestine, we may come across what doctors call ‘bacterial overgrowth’. This can cause severe bloating, abdominal pain, joint pain, nutrient deficiencies and anaemia.
Bacteria do more than just break down food. They also produce completely new substances. Fresh cabbage, for example, is less rich in vitamins than the sauerkraut it can be turned into. Extra vitamins are made by our bacteria.
Unfortunately, over the years our modern diet, full of sugar, processed foods and additives, promotes the growth of harmful bacteria and yeast. It also turns on genes that are unfavourable to our wellbeing. With the right amount of healthy bacteria, our guts can promote happy minds. However, if the wrong yeast and bacteria start to colonise the gut, toxins are produced which in the long run can create problems.
Your gut and your brain will function optimally when their signals are not jammed by toxins, food allergens and stress. I am always amazed at how lucid my thinking becomes after completing the 12-Day Plan. My problem-solving skills are also greatly improved.
‘With the right amount of healthy bacteria, our guts can promote happy brains.’
Several times a day our lives are saved by our immune system. Mutated cells are destroyed, bacteria are peppered with holes and viruses are sliced in two. The immune system has to tread delicately in the gut; while it permits peaceful co-existence with the many bacteria that live there, it must also be able to recognise enemies. Our immune system must also be able to differentiate between its own cells and the body’s own human cells. It doesn’t always. Type 1 diabetes results from the autoimmune destruction of the cells that produce insulin.
The gut is the training camp for the immune system. And immune cells with a tendency to attack the body’s own tissue are weeded out before they leave the camp.
When it comes to the immune system, much of what bacteria tends to do is ‘fine-tuning’. Each kind of bacterium has its own way of affecting the immune system. Some species of bacteria have been observed to make our immune system more tolerant by producing mediatory immune cells, while others have been found to provoke the immune system by imitating the behaviour of more harmful pathogens. For example, these provocateurs might dock in the villi of the small intestine. When a dangerous pathogen passes by, the provocateur has already docked in their favourite spot and it will move on. This phenomenon is known as ‘colonisation resistance’. The majority of the microbes in our gut protect us simply by occupying spaces that would otherwise be free for harmful bacteria to colonise.
Antibiotics kill bacteria by filling them with holes, by poisoning bacteria, or by destroying bacteria’s ability to reproduce. However, antibiotics are oversubscribed and often prescribed as if they were ordinary sweets from a sweetshop – this is a huge problem. Antibiotics decimate the microbiome and this can eventually lead to serious health problems.
The main reason for taking antibiotics is to cure ‘colds’. However, as any family doctor will tell you, most infections are viral, whereas antibiotics only kill bacteria. Except for a select few, viruses are unaffected by antibiotics. Most colds are caused by viruses and will resolve with some simple rest and immune support. So, taking antibiotics for a cold is a complete waste of time and will negatively affect your delicate microbiome.
When medically necessary, for example in cases of severe pneumonia, or for helping children recover from an acute infection, taking antibiotics can be justified. The cost is high in terms of the price you pay for the destruction of good bacteria in your gut, which could take many years to recover, but overall, in this situation, the risk is worth taking.
Antibiotics can alter gut flora. Our microbe collection becomes less diverse and their ability to produce vitamins is affected, likewise the amount of cholesterol they can absorb and the type of foodstuffs they can help us digest. Most of all, antibiotics can be a problem for old people and children.
However, the over-subscription of antibiotics is leading to more antibiotic-resistant bacteria that are difficult to treat and can kill. Many thousands of people die in the West because they are infected with bacteria that have developed resistances that no drug can counter. And every time you take a course of antibiotics your gut flora is changed.
After a course of antibiotics it is essential to repopulate the gut with good bacteria. This can be achieved through eating fermented foods or by taking a multi-strain probiotic. If you do not take care of yourself after a course of antibiotics, you can suffer from an imbalance between good bacteria and bad bacteria, as your gut flora changes.
HOW TO KEEP OUT OF THE ANTIBIOTIC WARS
> Do not take antibiotics unless it is 100 per cent necessary to do so
> Always complete your course of antibiotics
> Buy organically farmed meat
> Wash your fruit and vegetables
> Take care when travelling and follow this advice: ‘If you can’t peel it, cook it or boil it, don’t touch it.’
The overuse of antibiotics is the root cause for the overgrowth of yeast in the gut. Eating high-sugar foods feeds the yeast and creates neurotoxins, which are responsible for fatigue, mental fog, mood swings, poor memory, insomnia, anxiety, muscle and joint pains and depression. Accompanying the yeast overgrowth is usually a ‘leaky’ gut. The yeast passes through the cheesecloth-like gut lining, causing all sorts of problems such as body pain and fibromyalgia. Many students have come to me over the years complaining of doctors who are unable to resolve their issues and they have asked me if yoga can help soothe their painful muscles. And after a few months of practice, which often includes the 12-Day Plan, their symptoms start to slowly dissipate.
Dysbiosis is a microbial imbalance inside the gut, characterised by increased levels of harmful bacteria, yeast and parasites, and reduced levels of beneficial bacteria.
Between the antibiotics, poor dietary habits and the toxins that you are exposed to in your environment, and the resulting dysbiosis, you put yourself at risk to processes in the body such as a leaky gut.
Other common causes of dysbiosis include:
 Chronic indigestion
Chronic indigestion
 Constipation
Constipation
 Stress.
Stress.
The symptoms of dysbiosis are non-specific and can be seen if you suffer from the following:
 Gas
Gas
 Bloating
Bloating
 Indigestion
Indigestion
 Constipation.
Constipation.
Symptoms outside your gut include:
 Asthma
Asthma
 Eczema
Eczema
 Rashes
Rashes
 Nerve pain
Nerve pain
 Joint swelling.
Joint swelling.
Yeast overgrowth is a form of yeast dysbiosis. Your best protection against this is a normal acidic stomach pH, but any acid-blocking medication may lead to yeast overgrowth. If yeast overgrowth establishes itself, toxins produced by it will create problems in the body and may lead to further conditions, which may seem unrelated at first. A diet rich in sugar and simple carbohydrates is usually the culprit.
Common symptoms of yeast overgrowth:
 Fatigue
Fatigue
 Mental fog
Mental fog
 Anxiety
Anxiety
 Joint pains
Joint pains
 Itchiness
Itchiness
 Bloating.
Bloating.
As we have seen, every time you take antibiotics your gut flora is disrupted. That’s trillions (more than there are stars in the Milky Way) of microbes, whose delicate balance influences our overall health. A disruption here allows pathogenic bacteria to step in and it can take over. Probiotics help the gut to return to a state of healthy equilibrium.
People have been taking probiotics since ancient times; our ancestors used bacteria to preserve food. Every culture in the world uses microbes in food preparation. Germany has its sauerkraut, the French have their crème fraîche and the Turks have their ayran. And in Asian cultures we have miso soup, lassi, etc. All these foods rely on fermentation.
Friendly bacteria help us to maintain proper intestinal permeability. They help to stabilise the villi in the gut, which is likely to grow bigger because of their presence. The more stable they are the less waste they will allow through the gut wall.
One of their most important jobs is to defend the gut, and outnumber and antagonise unwelcome pathogens in it. These unwelcome pathogens could be parasites, yeast or bacteria. This activity known as ‘colonisation resistance’ prevents colonisation of our guts by unfavourable pathogens.
Probiotics are really our silent heroes of health and have been shown to decrease the frequency of sinus, ear and upper-respiratory infections in children. And not only do they protect us against pathogens but they also help to reduce ‘leakiness’ of the gut and bolster our immune system as well.
A number of fermented foods can support the growth and proliferation of your ‘good’ bacteria.
Try to incorporate:
 Cultured foods, such as yoghurts and kefir
Cultured foods, such as yoghurts and kefir
 Fermented foods
Fermented foods
 Coconut water kefir.
Coconut water kefir.
However, when completing the 12-Day Plan, it is best to avoid dairy foods for 12 days.
Normally probiotics require refrigeration. There are several supplements on the market; however, I find the best ones to use are those that have at least 16 viable strains that have been subjected to rigorous scientific study and are proven to be effective. Strain-level research is key, and you can be sure that the strains are of the highest quality and backed by solid scientific research. I selected 16 key strains in my product ‘Brilliant Biotic’ (see here) because science has demonstrated that to be an optimum amount for the vast majority of people to attain and maintain a healthy gut. The sicker your gut is, the more imbalanced it is, the higher the dose will be needed to create a positive effect. Brilliant Biotic can also guarantee 30 billion live microorganisms at the time of expiration, rather than just at the time of manufacture. See here for a list of the active ingredients included in Brilliant Biotic.
Take Brilliant Biotic on an empty stomach at least twice a day for at least three months to:
 Regulate local and systemic immune function
Regulate local and systemic immune function
 Regulate inflammation
Regulate inflammation
 Regulate bowel motility
Regulate bowel motility
 Support mucosal barrier
Support mucosal barrier
 Support resistance to pathogens.
Support resistance to pathogens.
Lactobacillus and bifidobacterium Some of the most beneficial Lactobacillus probiotics are L. acidophilus, L. plantarum and L. paracasei. They help to repopulate the small intestine with friendly organisms that will help support digestion and the performance of the immune system.
Bifidobacteria (Bifidus) predominantly live in the colon or large intestine. Bifidobacteria lactis helps support intestinal motility, promotes immune balance and relieves IBS symptoms. They produce butyrate, which is essential for the health of the cells that line the colon.
Whereas probiotics are live microorganisms and are responsible for boosting your digestion and reducing bad levels of ‘bad’ gut bacteria and strengthening the immune system, prebiotics are non-digestible ingredients that pass undigested into the large intestine, where they feed our beneficial bacteria. Nothing influences our gut as much as the food we eat. And we should feed our microbes well so they can populate as much of the large intestine as possible. We need to include real roughage, made of real fibre in fruit and vegetables.
Prebiotics can:
 Influence the composition of the gut microbiome
Influence the composition of the gut microbiome
 Prevent infections
Prevent infections
 Regulate appetite
Regulate appetite
 Prevent neoplastic changes
Prevent neoplastic changes
 Increase nutrient utilisation.
Increase nutrient utilisation.
The best way to take prebiotics is to eat them. But introduce them slowly into your diet, otherwise things can get a little gassy.
Top foods containing prebiotics (all raw):
 Chicory root
Chicory root
 Jerusalem artichoke
Jerusalem artichoke
 Dandelion greens
Dandelion greens
 Garlic
Garlic
 Leeks
Leeks
 Onions
Onions
 Asparagus
Asparagus
 Banana (not during the 12-Day Plan).
Banana (not during the 12-Day Plan).
Prebiotics support our good gut bacteria by eating certain foods. This results in a reduction of toxins produced in the gut. In fact, prebiotics are much more suitable for daily use than probiotics. And they only require one condition: beneficial bacteria must already be present in the gut.
If your gut is not as healthy as it could be, your stomach will always be fat. Probiotics help you to lose weight around your stomach because they help ensure that your digestive system is working to the best of its ability. They also help your body absorb health-boosting nutrients from your food better.
For hundreds of years, people have believed that the gut interacts with the brain to influence health and disease. However, the brain also interacts with, and affects, the gut. Depression treatments that target the mind can unintentionally impact the gut and medics, intending to cause chemical changes in the mind, often provoke gastro-intestinal issues, such as irritable bowel syndrome, as a side effect. Antidepressant medications (SSRIs), initially believed to be the cure for depression, change brain chemistry and contributed to chaos in the gut. As serotonin also plays a key role in moving food down the gut, altering the gut function will create side effects such as nausea, diarrhoea and constipation. The reason for this is that the gut-brain possesses the same neural receptors as the brain in our head. Anti-depressants treat both brains so it is clear that improving gut health will positively affect brain health. So, if people have both psychiatric and behavioural disturbances, one of the first places to look is the gut.
SEROTONIN AND THE GUT
Serotonin is a neurotransmitter, primarily found in the gastrointestinal tract (GI tract), blood platelets and the central nervous system. It is popularly thought to be a contributor to feelings of wellbeing and happiness. Approximately 90 per cent of the human body’s total serotonin is located in the GI tract, where it is used to regulate intestinal movements.
It always comes as a surprise when I ask my students in Mind Body Cleanse masterclasses where they believe serotonin to be manufactured in the body. They always reply, ‘In the brain, of course!’ It always amazes everybody when I state that in fact 95 per cent of serotonin is produced in the gut’s enteric nervous system. The gut is responsible for producing about 30 neurotransmitters along with this important ‘happy chemical’ and it shows why the gut is so central to feeling happy.
In coming years psychiatry will need to expand its scope to treat the second brain in addition to the one on the shoulders. And in some cases, it would be more effective if the gut had a session on the therapist’s couch, rather than the brain. We should not always blame depression in the brain on our life circumstances.
Stress is thought to be among the most important stimuli monitored through the gut – brain axis (see also here). When the brain senses a major issue, such as anger or fear, or that it is late for an appointment, it naturally wants to solve the problem. In order to solve the issue the brain needs energy, which it mainly borrows from the gut. Through the sympathetic nerve fibres the gut is instructed to obey the brain. The gut reduces blood supply and saves energy from temporarily digesting food because of this perceived emergency situation.
This system is not designed for over-use forever. However, if the brain thinks that it is in an emergency for the long term, the overworked gut will respond with negative stimulus, which may include diarrhoea, loss of appetite and fatigue. And if this situation is not checked over time, the health of the gut will eventually suffer. A reduced blood supply and a thinner layer of mucus will weaken the gut walls. The immune cells that live in the gut wall begin to secrete large amounts of signal substances that make the gut brain increasingly sensitive and eventually may influence behaviour and lead to illness down the line.
Over the years I have been amazed at how simple lifestyle and eating habits have influenced behavioural, psychiatric and emotional issues with my one-on-one clients. Often clients have been so toxic that it has been a struggle to make real positive health changes, which require modifications in lifestyle and eating habits, and it is often the smaller incremental changes that make all the difference.
Marcus was a case like this:
I am 45 now, and have been morbidly overweight for most of my life.
After several months of yoga and plenty of water to flush out my system Chris finally let me go on to his 12-Day Plan. I was reluctant because I didn’t think I’d make it 12 days without meat, cheese, pasta or fried food. I cheated on Day 1 and had some salmon. Day 2, I craved meat or fish, but resisted. Day 3, no cravings and in fact I started enjoying my outrageously delicious and varied salads, my sprouting beans and lentils, my hummus, olive oil, raw garlic, lime, coriander and a slew of spices and other herbs. I completed each stage of the Cleanse looking forward to the next day of my adventure with healthy eating. Days 7, 8 and 9 I felt amazing and had no symptoms to cause me concern, and then back to a gentle weaning off liquid for the last three days.
I have so far lost 55lb from my highest weight last year. I wake up without back pain and have a spring in my step. I do my yoga and I feel euphoric all day. I can’t even look at the food I used to love without my stomach turning. And the quality of my life at home and at work has improved considerably.
My goal is to lose another 110lb in five years, though at this rate I’ll do that long before my birthday in 2018.
Marcus is one of hundreds of clients I have seen undergo a remarkable transformation in wellness after rebalancing their gut and following the 12-Day Plan. An important realisation for Marcus is that you are far more in control of how you feel by how you eat and lifestyle factors than you realise.
While the Mind Body Cleanse method and 12-Day Plan are suited to those who want to optimise their health and wellness, it is also good for people who want to recover from gut-related conditions. Over the years I have been amazed at the increase in cases of gut-related problems among clients.
Irritable-bowel syndrome is often characterised by a bloating or gurgling sensation in the gut – unpleasant. There is also an increased susceptibility to constipation and diarrhoea-like symptoms. Sufferers of IBS who seek out yoga and meditation speak of anxiety and depression as often being linked to their symptoms. Sadly, the medical profession can still dismiss patients with IBS all too easily because tests often show no visible damage to the gut.
Other diseases affecting the bowel include conditions such as Crohn’s disease or ulcerative colitis. Sufferers also show increased rates of depression and anxiety.
A bloated tummy is often a warning sign of a sluggish intestine. You may be able to mitigate against the effects of sluggish bowels by:
 Eating slowly.
Eating slowly.
 Chewing your food thoroughly. Poorly chewed food will sit and ferment in your gut. Chew each mouthful at least 30 times and never eat when you are stressed, as Gandhi said: ‘Chew your liquid and drink your solids.’
Chewing your food thoroughly. Poorly chewed food will sit and ferment in your gut. Chew each mouthful at least 30 times and never eat when you are stressed, as Gandhi said: ‘Chew your liquid and drink your solids.’
 Drinking plenty of water between meals. Dehydration will cause fluid retention and this will lead to bloating. Drink a minimum of 2.5 litres of fresh filtered water every day.
Drinking plenty of water between meals. Dehydration will cause fluid retention and this will lead to bloating. Drink a minimum of 2.5 litres of fresh filtered water every day.
 Trying not to drink and eat simultaneously as this will dilute the gastric medium and make your digestive process less efficacious. Rather, drink water 30 minutes before or 30 minutes after eating.
Trying not to drink and eat simultaneously as this will dilute the gastric medium and make your digestive process less efficacious. Rather, drink water 30 minutes before or 30 minutes after eating.
 Eating too many acidic foods. Rather, eat more alkaline foods. Aim to make 80 per cent of what you eat alkaline.
Eating too many acidic foods. Rather, eat more alkaline foods. Aim to make 80 per cent of what you eat alkaline.
 Eating early in the evening. Digestion is at its peak in the morning and thereafter slows down. Badly digested food will sit in your gut. Avoid eating before bedtime and make breakfast your biggest meal of the day.
Eating early in the evening. Digestion is at its peak in the morning and thereafter slows down. Badly digested food will sit in your gut. Avoid eating before bedtime and make breakfast your biggest meal of the day.
At a professional level I have been surprised at the number of clients who count allergies and food intolerances and sensitivities as serious issues.
There are two different types of reactions to food. One is delayed and the other is immediate. And while some are immune-related, not all reactions are immune-related.
Food intolerances A food intolerance is the result of a deficiency in a digestive enzyme that makes it difficult to break down a food nutrient, like the lactose in dairy products. It is not the same as a food allergy, and you may experience the following symptoms:
 Indigestion
Indigestion
 Gas
Gas
 Bloating
Bloating
 Cramping
Cramping
 Flatulence
Flatulence
 Loose stools.
Loose stools.
Food allergies cause an immediate response after contact with the substance. A food allergy may be characterised by the following symptoms:
 Anaphylaxis
Anaphylaxis
 Shortness of breath or asthma
Shortness of breath or asthma
 Skin rash
Skin rash
 Itching of the skin
Itching of the skin
 Hives.
Hives.
Food sensitivities are characterised by a delayed response to a food substance. Often a common healthy food may be at the root of this problem. Symptoms may include:
 Migraines
Migraines
 Mental fog and fatigue
Mental fog and fatigue
 Delayed onset of symptoms – this makes it difficult to identify the food sources responsible
Delayed onset of symptoms – this makes it difficult to identify the food sources responsible
 Skin rashes
Skin rashes
 Irritable bowel syndrome (IBS).
Irritable bowel syndrome (IBS).
The best way to identify whether you are food-sensitive or intolerant is to keep a diary and keep track of your symptoms and eliminate specific foods as part of your 12-Day Plan.
A healthy gut works in a very similar way to cheesecloth. While it keeps the larger food particles, parasites, pathogenic gut bacteria and yeasts out, it allows all of the good nutrients through. Problems occur when these pathogens and larger food particles slip through the cheesecloth-like membrane and trigger an immune response. As the immune system hunts along the gut border for anything it does not recognise, it attacks these pathogens and larger food particles. In individuals with a predisposition to autoimmune diseases, the increased work for the immune system leads to a type of deregulation that eventually becomes an autoimmune disease. This causes inflammation and sensitivities.
Why do people develop a leaky gut? This could occur for one or more of the following reasons:
 Stress
Stress
 Dietary choices
Dietary choices
 Infections
Infections
 Low stomach acid
Low stomach acid
 Toxic exposure to preservatives and pesticides
Toxic exposure to preservatives and pesticides
 Antibiotics.
Antibiotics.
Leaky gut is one of the most controversial and significant conditions when we are looking at gut imbalances. It is the description of the underlying pathology of numerous diseases that we treat yet have failed to find a cure for. Gut ‘hypermeability’ or ‘leaky gut’ is a process that has only begun to be accepted as a real syndrome in medicine comparatively recently. Often the symptoms are very similar to those of food-sensitivity reactions.
IBS and migraines can both be activated by immune reactions to food that a person may be consuming on a daily basis. If not treated, leaky gut can lead to serious inflammatory disorders and malnutrition.
Common symptoms may include:
 Fatigue
Fatigue
 Indigestion
Indigestion
 Constipation
Constipation
 Weight gain.
Weight gain.
The 12-Day Plan will certainly help many of the issues related to a leaky gut; however, you may require a longer bespoke approach to cure your unique imbalances from your health-care practitioner if symptoms persist.
If you have coeliac disease, eating wheat can damage the villi in the gut wall and can cause serious infections. It can also damage the nervous system. For children it can be more serious and can cause diarrhoea and stunted growth. Symptoms may range from nausea to anaemia. The most effective treatment is a gluten-free diet.
Those with non-coeliac gluten sensitivity (NCGS) can eat wheat without serious risk to their small intestine, but should eat wheat in moderation. This is because you can become sensitive to gluten without developing autoimmune coeliac disease. Many people who do the 12-Day Plan, which is gluten-free, notice their sensitivity when they cut out gluten for 12 days and note a general improvement in their wellbeing. Digestive problems, flatulence, painful joints and headaches clear up, while energy levels and the ability to concentrate generally improves.
Gluten is a sticky protein that gives bread products their fluffiness and chewiness and it is omitted from the 12-Day Plan. It is a mixture of proteins found in wheat and related grains, including barley, rye and oats.
The incidence of NCGS, wheat allergy and gluten ataxia is increasing in most areas of the Western world. This is due mainly to the higher content of gluten in bread and bakery products, due to the reduction of dough fermentation time.
People with NCGS may develop gastrointestinal symptoms, which resemble those of irritable bowel syndrome or wheat allergy, and a wide variety of non-gastrointestinal symptoms, such as headache, chronic fatigue, fibromyalgia, atopic diseases, allergies, neurological diseases or even psychiatric disorders.
FEELING FOGGY?
A protein from gluten, gliadorphin, interacts with opiate receptors in the brain, mimicking opiate drugs such as heroin and morphine. These compounds affect the temporal lobe – an area of the brain that is associated with speech and hearing comprehension. That is why you can feel fogged up after a sandwich, for example.
In the same way that gluten metabolises into an opiate-like substance, so does the protein casein found in milk and other dairy products. Just like morphine, it makes you feel happier, calmer and sleepier.
Gastro-oesophageal reflux disease is a common condition where acid from the stomach leaks out of the stomach and up into the oesophagus (gullet). The oesophagus is a long tube of muscle that runs from the mouth to the stomach.
Common symptoms include:
 Heartburn – burning chest pain or discomfort that occurs after eating
Heartburn – burning chest pain or discomfort that occurs after eating
 Acid reflux – you may have an unpleasant taste in the mouth caused by stomach acid coming back up into your mouth
Acid reflux – you may have an unpleasant taste in the mouth caused by stomach acid coming back up into your mouth
 Pain when swallowing (odynophagia).
Pain when swallowing (odynophagia).
The answer to curing heartburn and acid indigestion is to restore your natural gastric balance and function. Eating large amounts of processed foods and sugars will exacerbate acid reflux as it will upset the bacterial balance in your stomach and intestine. So, before you turn to medication, you need to look at your lifestyle and diet. Instead, eat a lot of vegetables and other high-quality, ideally organic, whole foods. Eliminate caffeine, alcohol and nicotine products, which can trigger symptoms.
Acid reflux can also be a mechanical issue, as the pressure from too much food, incompletely digested and sitting in the stomach, especially if consumed too soon before bedtime, pushes stomach acid up the gullet. This leads to a burning sensation and inflammation.
Medications that suppress stomach acid may make your immediate symptoms better, but they should never be used long term to manage your indigestion or reflux because they may have serious long-term negative health effects.
Wellness depends on the breakdown and absorption of nutrients from the foods we eat, and enzymes are responsible for breaking down the foods into small absorbable units.
Digestive enzyme deficiency causes may include:
 Stress
Stress
 Toxicity
Toxicity
 Imbalanced stomach pH
Imbalanced stomach pH
 Infection and inflammation
Infection and inflammation
 Free-radical damage.
Free-radical damage.
You can see how serious this condition can become. If you cannot digest food properly, you may suffer from nutrient deficiencies and dysbiosis, and your potential to develop leaky-gut syndrome and food sensitivities is high.
If your symptoms get better with supplementation, with ‘Gorgeous Greens’ for example (see here), you can assume that you had a deficiency to begin with.
Symptoms of digestive enzyme deficiency:
 Fullness after a meal
Fullness after a meal
 Gas and flatulence about one hour after eating
Gas and flatulence about one hour after eating
 Undigested food in stool
Undigested food in stool
 Weight loss or weight gain
Weight loss or weight gain
 Deficiency of fat-soluble vitamins.
Deficiency of fat-soluble vitamins.