There are nearly five million dog bite injuries recorded annually in the USA, half of which are children.
Children are more prone to dog bite injuries due to low height proximity to the dog, unfamiliarity with the dog or its behavior, poor adult supervision, and insufficient anticipatory guidance and protection regarding dog-in-residence relationship.
Biting or attack-breed dogs render more serious and complex bite wounds in children and often chase children off-property without provocation.
Most wounds require thorough washout under gentle pressure (<10 psi) and meticulous primary closure.
Puncture wounds should not be closed but rather thoroughly irrigated and left open for several days prior to definitive repair.
Bite wounds from a larger dog to the head of a young child (<5 years) should prompt CT screening to rule out calvarial penetrance.
5.1 Introduction: Scope of the Problem
Evidence of association between humans and dogs dates back approximately 12,000 years as the two species learned to be companions and people trained dogs for tracking, herding, guarding, and retrieving [1]. Approximately 70 million dogs are owned in the USA; the canine population has grown faster than the human population [2–4]. Half of US households have one or more dogs [5].
The increase of dog breeds, especially “guard” or “attack” breeds, has resulted in a worldwide increase in dog bites [6]. Some bites or attacks are vicious maulings resulting in severe avulsion injuries and death, which has led to attempts at legislation to address this burgeoning problem. Some countries view dog bite problems as a public health and safety issue [7–9].
It has been noted in many dog bite studies that children are vulnerable to and involved in most dog bites requiring medical attention [3]. Many of these wounds involve the head and facial regions, as face height is often at dog level [4]. As children have become more exposed to danger in our society (firearms, abuse, recreational hazards, less supervision, etc.), dog bites and attacks have alarmingly increased, particularly with the advent of more dangerous dog breeds (e.g., pit bull terrier).
Management of the child with a dog bite is twofold—proper care of the wounds and holistic care of the child. Care of children with a dog bite of the head, facial, and neck regions requires an understanding of bite wound characteristics (timing, puncture vs. avulsion, etc.), dog breed features and bite forces generated, home safety and well-being initiatives for children, and emotional-psychological “fallout” from a terrifying traumatic event [10]. Recently, PTSD has been recognized in children who have experienced such an attack or mauling [11–13]. The attending surgeon caring for a child with a devastating injury needs to understand these components of pediatric care.
5.2 Epidemiology
The CDC reports approximately 4.7 million bites per year with almost half requiring medical attention (representing approximately 1% of all emergency department visits) [8, 14–16]. Annually, the incidence is about 13 recorded bites for every 10,000 persons or 914 ER visits for dog bites per day in the USA [14]. Gilchrist et al. noted that dog bites affect 1.5% of the US population annually (from the ICARIS-2 Injury Control and Risk Survey) and the risk of a dog bite is fivefold higher when two or more dogs live in the same household [3, 8].
Dog bite injuries requiring admission to hospital rose 86% during the time period 1993–2008. The average cost of admission was $18,200 per patient [17]. Summarily, this represents a cost of almost 250 million dollars per annum for medical management [18]. This does not take into consideration the legal fallout of dog bite injuries. The Insurance Information Institute reported that dog bites accounted for more than one-third of all homeowners’ insurance liability in 2014, costing in excess of $530 million [19].
Mortality from dog bites is low with an average of 33 fatal dog attacks in the USA per year, as reported from various media reports on dog attacks during the time period 2005–2015 [20]. Children and adults have been killed in equal numbers; many of these attacks involved large and aggressive dogs [20]. Schalamon et al. found increased incidence during summer months and even distribution across days of the week [21].
One out of every 20 dogs will bite a human during the dog’s lifetime, and multiple breeds (pit bull terrier, German shepherd, Rottweiler, and Doberman) have been implicated as higher risk for bites and assaults [3, 4, 21–27]. Pit bull terriers, Rottweilers, and German shepherds are most often involved in severe dog bites or attacks [12, 18]. Schalamon et al. noted a relative risk of a bite by a German shepherd or Doberman as five times higher than by a Labrador or golden retriever or mixed breeds in their Austrian study population. Bites from these two breeds occurred in 37% of the recorded cases despite accounting for only 13% of the dog population [21].
In a large retrospective review of 1616 dog bites recorded over a 4-year period at the Children’s Hospital of Atlanta, ED, it was noted that pit bulls (as recorded) were implicated in over half of the severe wounds requiring surgical management in the OR, and were responsible for multiple wounds [28]. Further, multiple bite wounds were 2 ½ times more likely from pit bulls than other breeds. More than half of the wounds (57%) were in the head and neck region. Almost 88% were either identified as family pets or as known to the victim.
A study by the University of Colorado-Denver identified 58 breeds responsible for dog bites [29]. Most common were mixed breeds (23.0%) followed by Labrador retriever (13.7%), Rottweiler (4.9%), and German shepherd (4.4%). It was noted that Labrador retrievers were the most popular dog in numbers both in the USA and in Denver during the study period; further, pit bull terriers, the leading perpetrators of severe wounds in most studies, had been banned from the county for the preceding decade, accounting for their absence from the study [30].
5.3 Provocation
Why a dog bite is difficult to ascertain is because either many events are unwitnessed or a dog’s behavior is not readily or reliably determined just prior to biting; provocation leading to a single bite, however, is often dismissed as a “natural” animal response. Aggressive bites rarely follow in “play” activity between a child and his or her pet dog; rather, such a case represents a response or instinct to attack. “Triggers” including surprise, guarding or protecting behavior, pack mentality, and prey targeting all may provoke a powered or sustained attack, especially in the young or naïve [10]. Gershman et al. observed increased aggressive behavior in unneutered male dogs, compared to female and neutered dogs [24]. They suggest that the likelihood of a dog biting is multifactorial with heredity/breed, early training experience, late or confined socialization, and victim behavior all playing a role [31].
More bites have been recorded involving unlicensed, non-vaccinated, non-neutered, or chained and restricted male dogs [24]. These characteristics would indicate that the owner’s behavior and interaction with his or her dog may come into consideration for “provocateur” or “scienter” dynamics in responsibility. The owner’s intent is often trained into the dog for conditioned responses to stimuli, protection or guarding or threatening behaviors, though instinct often trumps training in some breeds.
Familiarity may be a risk factor for bites because a young child may not understand a dog’s behavior pattern (easily excitable), thus readily placing themselves at risk during teasing or playful activities. Triggers of a bite—playing with, startling, teasing, or feeding the dog at the time of injury—have been noted in dogs well known to the child. Most bites are considered to be provoked using these loose definitions; thus, provocation may be difficult to always or precisely determine. Adolescents are more likely to be bitten by unknown dogs whereas younger children by dogs with which there is some familiarity. Children with ADHD were also noted by Mitchell et al. to have a greater risk for injuries than children without ADHD, suggesting that behavioral aspects of the victim come into play to trigger a bite [26].
Dog owners who accept that aggression is a normal response for a breed and do not take steps to control such behavior are contributing to a dangerous public health environment and intensification of the problem. Further, veterinary medicine now includes anticipatory guidance for owners of certain breeds, taking into consideration the possible inherent dangers of mixing some breeds and vulnerable persons in the home environment [10].
5.4 Children at Risk
Children are commonly affected with many children experiencing or witnessing a dog bite at some point [32, 33]. The dog is typically known to the victim (either a family pet or owned by a neighbor) and the attack usually occurs in a familiar environment such as the home. Bites from stray dogs, though problematic for rabies exposure, are less common [25]. The CDC estimated greater than 133,000 dog bite injuries for children less than 18 years of age in 2013 in the USA [34]. American studies indicate that young children are most at risk for a dog bite, followed by infants and toddlers [4, 13, 22, 31]. For every age group and gender, the highest incidence of bites occurs in 5–9-year-old boys [21]. Mitchell et al. describe the prototypical child as a 5-year-old male bitten by a familiar dog in the neighborhood or at home [26]. At the Denver Children’s Hospital they noted an average age of 4.6 ± 3.4 years with boys more at risk for bites (52%). Elsewhere, Schalamon et al. in a study of Austrian children noted on average about 1 bite per 2000 children up to 16 years of age and the highest incidence of bites in toddlers and infants [21]. Dog bite rates are significantly higher in developing countries where children and mongrel-type dogs interface more often without careful supervision or protection [9].
5.5 Bacteriology of Dog Bites
Infection rate following a dog bite is variably reported at 2–20% [15]. Animal saliva is generally the major source of bacteria obtained from culture versus the bite victim’s resident skin flora. The oral flora of dogs includes Pasteurella, Streptococci, and Staphylococci. Anaerobes grow in more than 50% of late-onset infected dog bites with Bacteroides, Porphyromonas, Prevotella, and Fusobacteria predominant [35]. Capnocytophaga has also been identified in immunocompromised and asplenic septic patients [36]. Pasteurella sp. have many strains in a single animal though with variable virulence.
Pasteurella multocida is a small aerobic, facultative anaerobic, gram-negative coccobacillus, which can be difficult to culture and is present in about 25% of dog bite wounds [35, 37]. It is responsible for early onset of infections, within 12–24 h after a bite [38, 39]. Although the risk of infection is low, prophylactic antibiotics is indicated in higher risk wounds (i.e., greater than 8 h old, wound needing surgical repair, deep puncture wounds, hand and joint wounds, and bites in medically compromised patients) [35, 40].
Ordot et al. in 1986 cultured wounds from 420 open dog bite patients and noted Staphylococcus epidermidis as the most common isolate and the majority of infections were polymicrobial [41]. Staphylococcus sp., Streptococcus sp., and Corynebacterium sp. are the most commonly isolated aerobic organisms from infected dog bites [42]. The most frequently isolated anaerobes include Bacteroides fragilis, Prevotella, Porphyromonas, Peptostreptococcus, and Fusobacteria [43].
5.6 Rabies
Rabies is caused by a neurotropic RNA rhabdovirus that results in an acute encephalomyelitis with retrograde neurotropic assent to the brain. It is transmitted to human beings by the inoculation of saliva into bite wounds or scratches. Worldwide, dogs are the primary animal reservoir. In the USA, however, the main vectors vary by region with skunks, raccoons, bats, and foxes being the greatest carriers of rabies [44]. The exposed person must be treated with rabies immunoglobulin and vaccine soon after exposure before the virus reaches the brain. With the onset of encephalitis, the infection is invariably fatal.
The CDC recommends a quarantine period of 10 days following bite by a known dog and immediate victim vaccination in cases of a suspected rabid animal. In 2014 the total number of rabid dogs reported to the CDC was 59 (13.3% of which were “domesticated”) [45]. In France, if a dog is vaccinated it will be placed in quarantine after a bite for 15 days and no prophylaxis is given to the patient. If the dog cannot be retrieved or verified despite owner’s warranty, then prophylaxis is administered. If the dog is not vaccinated, it is placed in quarantine for 15 days. If it begins to show signs of rabies, vaccination is given to the patient and the dog sacrificed to confirm diagnosis by microscopic brain examination [36].
Therapy following exposure involves passive immunization with human rabies immune globulin (HRJG) and active immunization with the human diploid cell vaccine (HDCV) or the rabies vaccine adsorbed (RVA) [46]. Rabies immune globulin is administered at 20 IU/kg, with half of the dose injected around and deep to the bite wound, and in children the other half in a muscle region proximal to the bite, e.g., thigh or deltoid. Rabies vaccine offers active immunity and is administered one (1.0) mL IM only on days 0, 3, 7, and 14 [47].
Tetanus prophylaxis is given if a booster has not been administered in the last 5 years. If the bite victim’s prophylaxis history is not known or less than three boosters have been received, then tetanus immunoglobulin is administered in the dirty wound.
5.7 Initial Management
Although taking care of the wound is primary, consideration must be given to the social implications leading to the bite, especially an infant or a young child. Safety and a healthy home environment are cornerstones to “child well-being” in pediatric care. Negligence on behalf of caregivers leading to serious injury of a child from a dog attack in the home should be documented. It may necessitate social work involvement if other children are at risk in the home environment, just as it would for abuse or violence. Inconsistency of story and bite marks not matching dog description should also prompt further investigation. This is also the time to think about emotional health of the child and the potential for emerging signs of PTSD [11, 12].
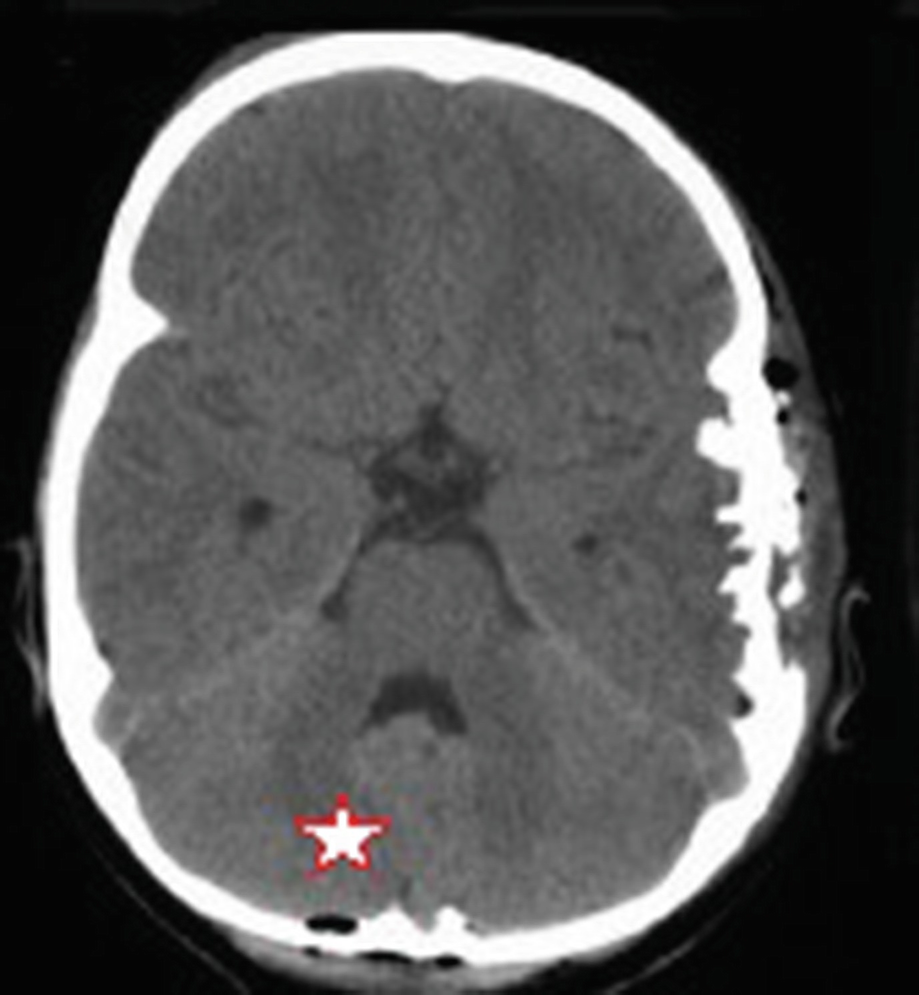
CT axial image of the skull with calvarial penetration (intracranial air noted by star) after dog bite of a young child
Brogan et al. in a review of 40 attacks noted facial fractures in about 25% of the cases, and of these, 22% had orbital injuries [25]. Mitchell et al. reported that scalp and cranial injuries were common in younger children; therefore naso-orbital skeletal injuries and fractures are possible necessitating appropriate radiologic survey [50, 51]. In a study of 143 isolated facial bite wounds in children, Mcheik noted that the majority of wounds involved the cheek 24% followed by the lip 19%, orbit 16%, forehead 15%, chin 8%, nose 7%, ear 6%, and scalp 4% [36].
In an unpublished series at the authors’ institution, dog bite-related injuries of the head and neck (n = 98) treated by the Section of Maxillofacial Surgery over the last 10 years were as follows: lips 43%; cheeks/jaws 40%; scalp/forehead 20%; orbit 17%; ears 17%; nasal 15%; jaw/nasal fractures 10%; neck 9%; facial nerve 7%; and ductal 7%. Many of the wounds were multiple bites or regions involved in the same victim, accounting for the respective percentages. Some children were bitten multiple times with injuries to the back and extremities including four limb fractures. Many of the victims were children under 10 years of age; therefore operative management was carried out in theatre under anesthesia. Obviously, many simple wounds are seen and managed by the emergency services; thus this sample does not accurately reflect correct total numbers and percentages of anatomical region involvement.
Thorough assessment of a dog bite wound in a young, frightened child is difficult. Evaluation may have to take place in theatre under anesthesia. Initial cleansing of a wound in the ED is vital (or in the prehospital setting by the family or paramedics). Normal saline is adequate (or even tap water in the home) and better for fragile and injured tissues than toxic agents like peroxide or iodine solutions [49, 52]. Dog bite wounds to the facial region are managed as any other contaminated wounds. Vigorous but gentle washout of the wound to its depths and extent is important in order to dislodge gross contaminants and reduce the bacterial load in the damaged tissues.
Irrigation with a syringe and 16–18-gauge catheter is adequate for most bite wounds in children. Pressures more than 15–20 psi are not easily generated and will generally be kinder to the fragile tissues and not extend the zone of injury [53]. Surface film, bacteria, and foreign bodies are dislodged, and irrigation lessens the intensity of the inflammatory phase of wound healing leading to optimal progression to the proliferative phase of healing. Sustained high pressure (commercial irrigators) in pediatric wounds may be more damaging to the tissues plus the force may actually propel microorganisms deeper into the tissue bed [54].
5.8 Antibiotics
Antibiotic coverage is prescribed to cover typical oral flora of dogs including Pasteurella (e.g., amoxicillin-clavulanate, moxifloxacin, cefuroxime axetil; azithromycin, clarithromycin, or doxycycline) [35, 55]. For the penicillin-allergic patient, clindamycin in combination with ciprofloxacin (for adults) and Bactrim (trimethoprim sulfamethoxazole) is the regimen of choice. IV antibiotic combinations for more established or progressive infections include ampicillin-sulbactam, ticarcillin-clavulanate, and cefoxitin with clindamycin plus ciprofloxacin for the penicillin-allergic patient. The course is 3–5 days for prophylactic treatment, 7–14 days for therapeutic treatment, and 3 weeks or more in the setting of bone involvement [35].
5.9 Wound Care in the ER

Puncture wounds of the periorbital region with secondary mixed aerobe-anaerobe infection

Washout of puncture wounds with syringe and catheter
5.10 Operative Management
5.10.1 Principles
Initial management is prioritized by urgency of the injury. A savage attack with multiple bites to the head, neck, and extremities will necessitate a thorough clinical and radiographic evaluation to identify all injuries, especially deeper or life- and limb-threatening injuries. Urgent surgical intervention is predicated on these positive findings.
Bites sustained more than 12 h prior to initial presentation should be treated with either delayed primary closure or healing by secondary intention [56]. Macerated wounds or those with ischemic elements should be delayed for several days or until the wound clinically appears clean without signs of infection. Established infections warrant frequent (daily or every 2 days) washouts and resolution of the infection prior to definitive repair. Obviously in young children this may require sedation or anesthesia for large wounds, making a daily routine a challenge. Daily wound checks, however, should be done to confirm resolution of the infection.

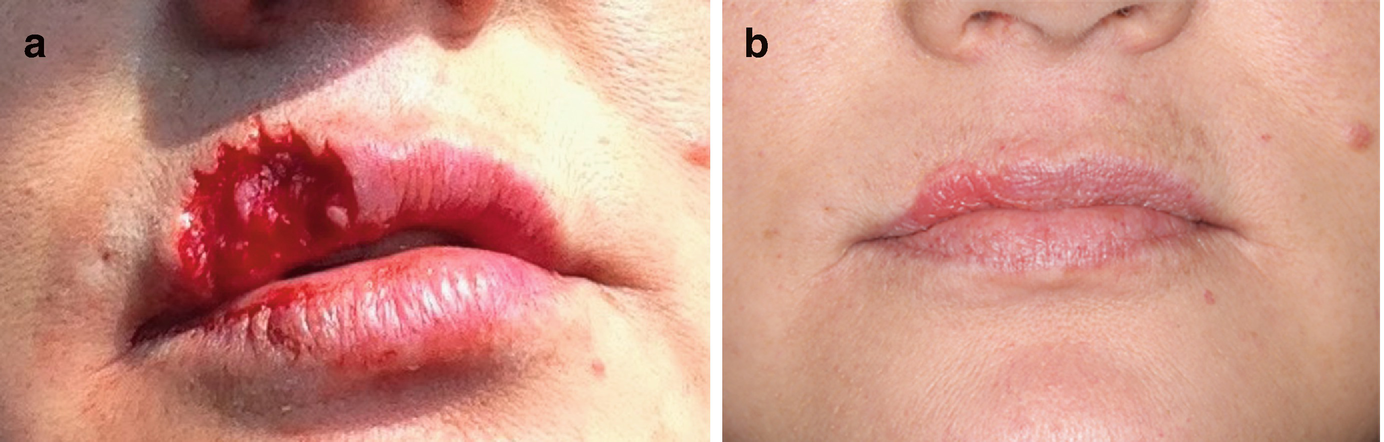
(a) Missing central upper (philtrum) dermis and muscle. (b) Primary closure of lip wound after tissue undermining and advancement
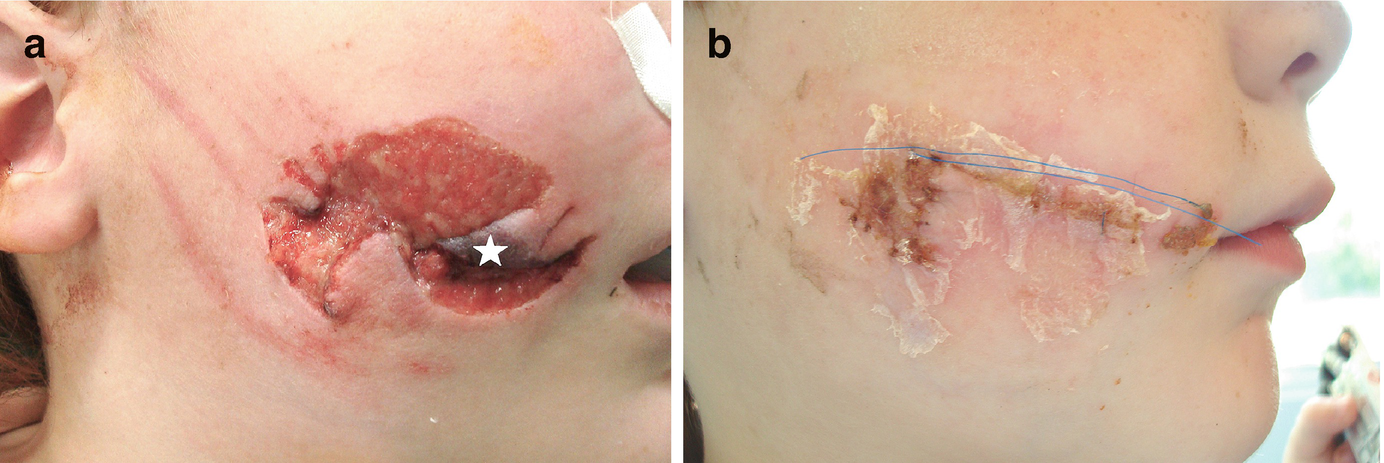
(a) Right cheek avulsion injury with necrotic tissue (star). (b) 10 days after sharp debridement, tissue undermining, and subcuticular closure with dermal glue

(a) Avulsion wound to deep fat with anterior pedicle. (b) Immediate repair of cheek wound and obvious venous stasis. (c) 3 months post-op and daily silastic pressure dressings
5.10.2 Avulsion Defects
Dog bite wounds that result in tissue loss are a challenge in the pediatric patient due to limited tissue reserve for local flaps. Some tissue rearrangement can be gained in the scalp, cheek, or neck; but generally, most surgeons are reluctant to create new incisions for local flaps on a child’s face. The scarring is already a concern and new incisional limbs contribute to that parental concern.
Waiting for tissue and scar maturity in order to provide enough tissue laxity for later scar revision may mean deferral; thus, the surgeon may have to counsel the parent and child during this waiting time period. During this waiting period, measures can be taken to enhance scar maturity and the ultimate tissue health—steroid preparations, silastic dressings, massage, and time [58].
Avulsive wounds require dead space elimination with a few deeply placed sutures, consideration for a small Penrose drain if it is a deep wound, and a protective pressure dressing. The wound should be inspected in 2–3 days to confirm vascularity, no hematoma formation, and satisfactory tissue approximation. Prolonged lymphedema should be expected in these wounds and may necessitate gentle pressure dressings (elastic) for weeks to months, especially whilst at home or sleeping [59].

Scalp reconstruction with tissue expansion. (a) Necrotic, infected scalp bite wound. (b) 4 weeks after tissue expansion (note external ports) and wound bed preparation. (c) Immediate expander removal and scalp reconstruction with primary closure
Special facial anatomical units deserve attention in dog bites where tissue is missing or transected. Focus on each of these unique regions follows with reconstructive options presented with a view toward application and limitation in children.
5.10.3 Nerves and Ducts

(a) Left eyelid and canalicular injury. (b) Canalicular intubation with skin stabilization. (c) 2 months post-canalicular repair (stent was removed 2 weeks previously)

Right cheek avulsion wound with exposure of deep fat and facial nerve (arrow)

Right facial nerve injury after deep bite to orbit and mandible. (a) 2 weeks after bite and initial repair. Note right mandibular branch weakness. (b) Wound distal to line dropped from lateral canthus indicating no need for facial nerve repair. (c) Spontaneous nerve recovery 3 months after injury

Bite to right lateral orbit with frontal-temporal branch transection and microscopic epineural repair (circle)
5.10.4 Lips
Missing portions of the lip and cheek are common in dog bites. Reconstruction is dictated by the location and amount of tissue missing. Upper lip avulsions cannot be primarily closed as readily as the lower lip due to tissue depot availability and anatomical distinctions (philtrum, cupid’s bow, more distinct vermilion, and white roll). Lower lip avulsions up to 1/3 can be closed primarily and in time the lip will attain some laxity and acceptable form and function without risk of microstomia [59]. Lower lip reconstruction or revision should only follow after several months of tissue maturation and preparation. Time, massage with aloe/lanolin/vitamin E preparations for a short period (1–2 months), steroid administration, and function with help prepare the tissues for revision, if at all necessary.
(a) Avulsion of upper lip skin including vermilion and white roll. (b) Reconstruction with dermal and mucosal advancement flaps

(a) Pit bull attack with large avulsion wounds to left face with missing left commissure, lips, and cheek tissue. (b) 3 week post-op of initial repair of avulsion wounds after debridement and primary closure. (c) 6 months after initial repair with demonstration of some tissue laxity and less commissure obliteration. There is significant hypertrophic scar formation due to tension across the areas of tissue loss which will require revision
5.10.5 Nasal
Creation or maintenance of a healthy recipient wound site
Prevention of stenosis and progressive cicatrization
Replacement tissue of similar features
Long-term tissue support
These steps in surgical management are demanding and require patient and caregiver commitment over a long period of time.
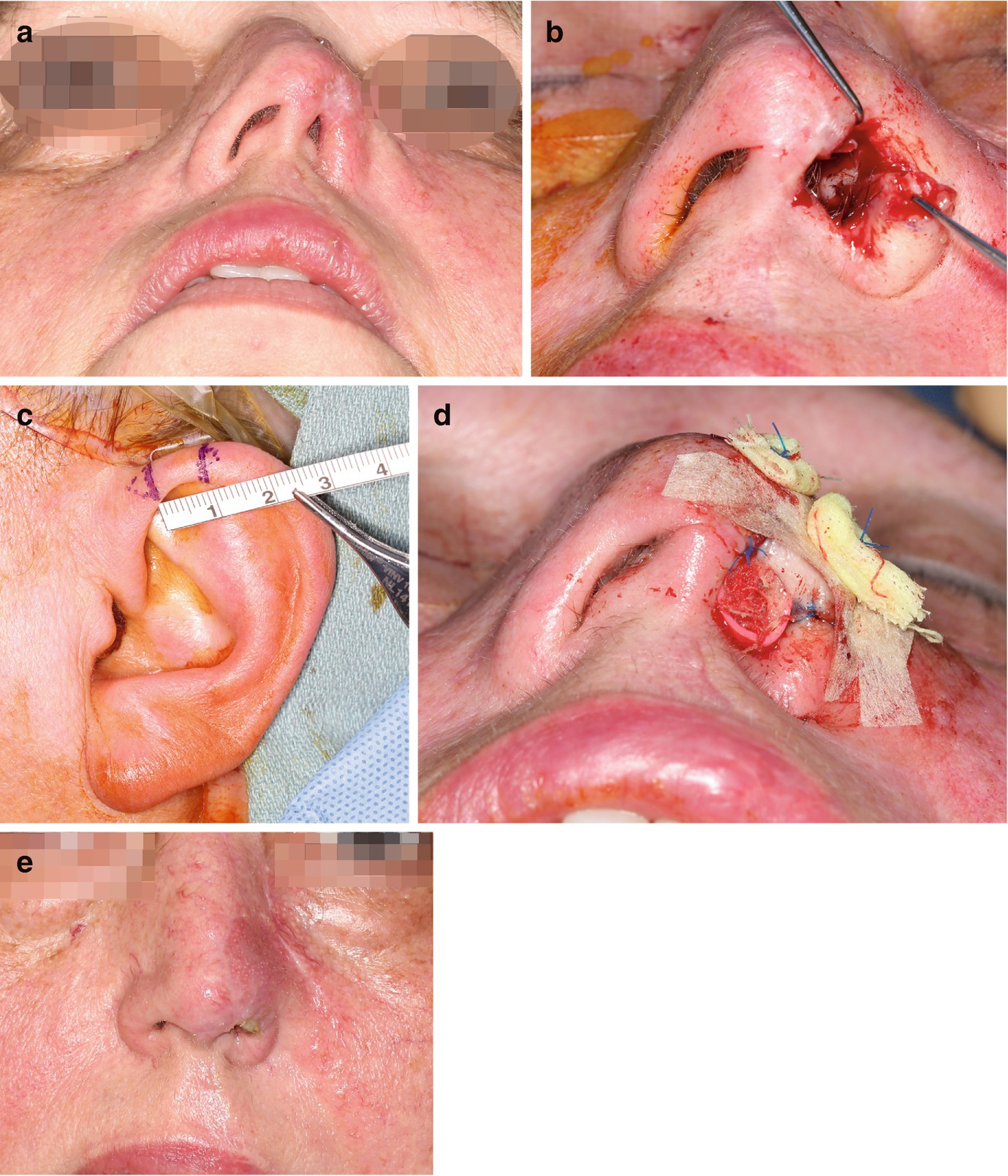
(a) Post-bite avulsion of left nasal side wall and alar rim with attendant nasal stenosis. (b) Preparation of alar site for composite graft by excision of nasal vestibular and dermal scar. Measurement of the defect is then carried out for determining the composite graft dimensions. (c) Composite graft donor site with attendant measurement. Grafts less than 1 cm will not require v-excision or releasing incisions to obtain donor-site primary closure. (d) Composite graft in place with respective bolster dressings. (e) 1 month post-graft and 2 weeks after bolsters removed. Note restoration of alar width, alar contour, and relief of stenosis

(a) Partial alar rim defect with loss of skin and cartilage. (b) Alar rim defect with cartilage strut sutured in place. (c) Advancement skin flap advanced from nasal sidewall and dorsum to cover strut. (d) 3 months post-graft
Central total nasal defects can be reconstructed with turned-down forehead flaps based on the supratrochlear artery. Tissue donor color and texture are approximate though not identical, plus a forehead donor site scar is inherited—all considerations to be reviewed with the parents prior to reconstruction. Partial nasal skin defects can be grafted with free skin grafts harvested from the postauricular (thinner), supraclavicular, and periumbilical (thicker) regions, though ultimate color, hypopigmentation, and texture betray the graft from native tissue [57].
5.10.6 Ears
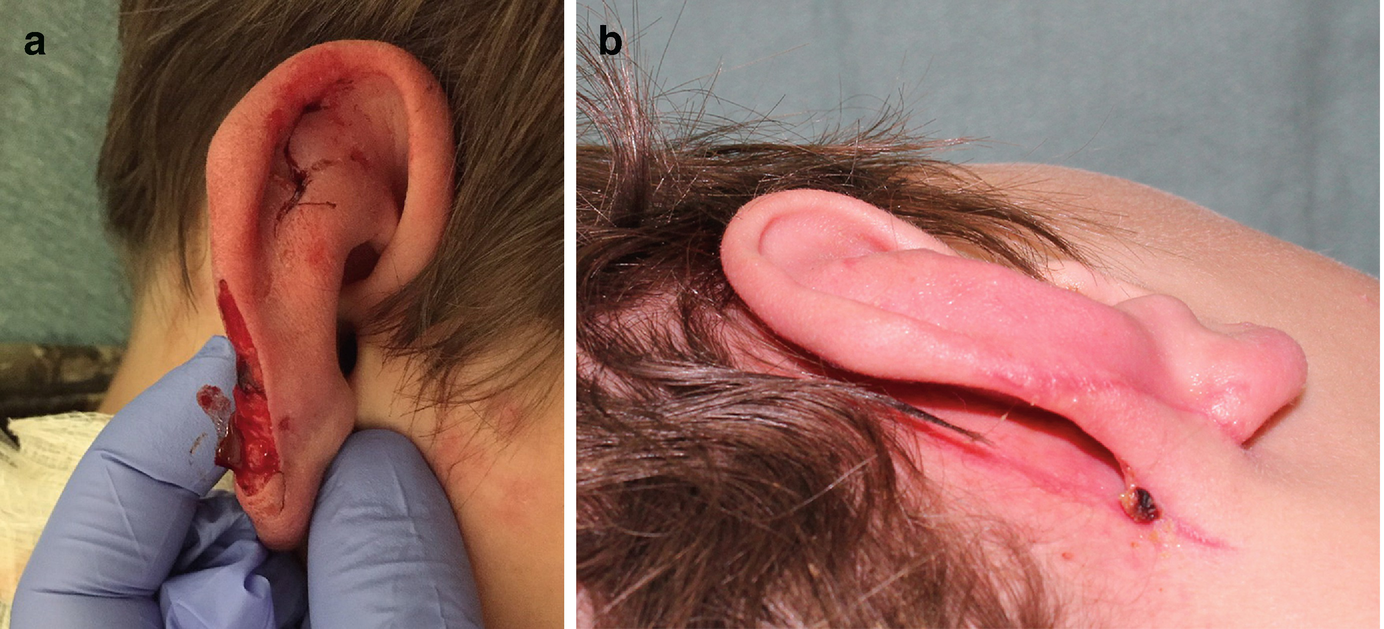
(a) Helical rim defect, soft tissue only. (b) Postauricular skin flap prior to division at 3 weeks

(a) Large skin, cartilaginous helical defect. (b) Raised postauricular flap to cover native defect. Note xeroform™ wick dressing under pedicle. (c) Reconstructed helix 6 weeks after division
Near-total ear avulsions require a staged approach through first preparing the wound bed for skin flaps or grafts. After adequate healing time of several weeks, tissue expanders are placed to provide enough space and tissue laxity to cover a fabricated cartilaginous framework harvested from the ribs. These steps are akin to that in congenital microtia reconstruction. Preservation of the external meatus is necessary through this entire process [57].
5.10.7 Neck
Dog bites from either a large breed or sustained aggressive bites to the head and neck regions should alert the surgeon to possible airway damage or vascular compromise. A child’s airway can be compromised by a deep bite to the airway itself, crushing the cartilaginous support, or through attendant edema and hematoma formation. Laryngeal fracture has been reported to respond to conservative therapy but early awareness of resulting edema and need for airway support in the period following injury is crucial [62]. If either is suspected, then airway preservation (consider very early in the process for endotracheal intubation) and vascular study (CTA) should be undertaken immediately, as for any penetrating injury to zone 2 of the neck [59].
Bites to the back of the neck of a child by a large dog can result in paraspinal, cervical, or laryngotracheal damage. These injuries ensue when a child is running away from the dog and the child is knocked to the ground in an aggressive and sustained attack [26]. Neurologic assessment is mandatory followed by CT examination if there are noted deficits.
5.11 Psychological Implications
Children exposed to or who have experienced significant traumatic events may develop emotional and psychological ramifications which may impact future health. Many studies have addressed this increasing problem of post-traumatic psychological damage which has been observed in a variety of multicultural pediatric populations, and in dog bites specifically [12]. From a seemingly innocent bite to a savage mauling, children (and families) respond differently to the event. Schmitt notes “A child attacked by a dog and bitten above the shoulders is equivalent to an unarmed adult sustaining a bear bite. The human emotional coping is overwhelmed.” [63] Peters et al. noted that over half of 22 children studied had symptoms of post-traumatic stress disorder (PTSD) following a dog bite, especially in those suffering from deep or multiple bites [13]. The treating surgeon needs to be aware of this dynamic and be able to identify signs of emerging emotional “fallout” or PTSD.
PTSD is a potentially crippling condition in children. The reserve, coping mechanisms and “plasticity” of children during development cannot be summarily applied as the rule when recovering from a dog attack. Children exhibit stress differently than adults and symptoms may include undue anxiety and fear, spontaneous crying, withdrawal, enuresis, insomnias, and nightmares [62]. Simple tasks that previously were simple now are difficult or ignored. Somatic disorders—headaches, chronic pain, and GI irritability—may develop. School absenteeism, relational disruption or withdrawal, and avoidance of anything perceived as threatening by the child begin to dominate the psyche.
In the postoperative period, the surgeon should be aware of this potential. Simple queries made at the bedside or chair which are related to a sense of well-being will gain the trust of the child and parent. Facial and body language responses may suggest some difficulties at hand during this visitation period. If so, referral to a child psychologist or counselor should be offered (most children’s hospitals offer such services) and followed up on.
Going forward, any revision procedures should be planned and discussed with these emotional and psychological conditions in mind. Having a pediatric mental health professional on board is helpful in delivering holistic care to children who have suffered a devastating dog bite injury.
5.12 Legislation
Attempts at legislation to control certain dog breeds in response to the increasing numbers and severity of dog bites have met considerable resistance due to cost, privacy, enforcement difficulties, and dog breed lobbies. In the USA, breed-specific legislation is specifically banned in some states, leaving municipalities or counties to independently enact their own policies and statutes [64, 65]. Over 700 US municipalities have statutes addressing primarily pit bull ownership [66].
In some countries, legislation has been enacted which specifically addresses particular breeds through “dangerous dog” laws and bans against owning certain breeds (as reported in US News and World Report April 20, 1987:24; Time July 27, 1987:60; Los Angeles Times July 29, 2011; Philadelphia Inquirer July 15, 2011) [3]. In Ontario, for example, the Dog Owners Liability Act was amended in 2006 to prevent free transport and breeding of pit bull terriers, making it mandatory to muzzle and leash dogs whilst in public, wearing government-issued warning collars in public places and posting warning signs on any property where the dog is confined. Heavy fines or imprisonment is imposed for owners of dangerous breeds of dogs who fail to comply with the attendant legislation.
The Dangerous Dogs Act (DDA) enacted in the United Kingdom and similarly in Australia (amended in 2013) in response to well-published pit bull-related maulings and deaths bans unauthorized ownership, breeding, or transfer of dangerous breeds (pit bull terrier, Japanese Tosa, Dogo Argentino, Fila Brasileiro, bullmastiff). These breeds must be confined, have government-issued warning signs and collars, and be muzzled and leashed when in public. Court exemptions must be obtained to own the dog and owner liability certification and insurance must be similarly obtained. Germany in the early 2000s similarly banned “fighting breeds” including mastiff, bullmastiff, bulldog, bull terrier, and Tosa [21, 67, 68].
Unfortunately, the impact of such bans and regulations on the incidence and severity of dog bite injuries is difficult to study for efficacy. Multifaceted approaches to dog owner education and awareness of aggressive behavior in certain breeds and physical state of the animal (injured, sick, or in pain), discouraging the breeding of aggressive dogs, and mandating training and early socialization of young dogs are seen as better alternatives to outright restriction and bans [69].
5.13 Prevention
It appears that in the USA, prevention of some dog bites through legislation which focuses on control or bans of certain breeds is very difficult due to the emotional components and strong lobby efforts involved on both sides of the issues. It remains, therefore, as in many potential public health hazards (e.g., alcohol, sexual promiscuity, firearms, violent video games, recreational vehicles for children) for children, a necessity for healthcare professionals to address these hazards in the holistic care of children. And this goes for the interface of dogs and young children. The prudent approach is to educate parents about exposure of their children to certain conditions or agents of harm in the home or neighborhood environment. For children and dogs, this means education about certain breeds of dogs, their behavior, avoidance of triggers for a bite or attack, and what to do in the event of a dog attack. Dog ownership must be taken responsibly and accountably in each community.
The American Veterinary Medical Association has made some recommendations along these lines, which can be accessed at https://www.avma.org/public/Pages/Dog-Bite-Prevention. Anticipatory guidance should include review of these elements in prevention of dog bites with parents and children, both by primary care providers and, to some extent, those surgeons who care for an injured child.
5.14 Summary
Dog bites represent an often underreported and recently ascendant healthcare problem for children in the USA. Managing the child with a dog bite has two key components—care for the wound in its entirety and holistic care for the child and family that have experienced a severe dog bite wound. The majority of bites occur from family-owned dogs or those known to the child. Early intervention for repair and appropriate antibiotic administration are important to optimize aesthetic, functional, and psychological outcomes. Many specialized regions of the face—nose, eyes, ears, and lips—are a challenge to reconstruct when tissue is missing or significantly distorted by scar. The attending surgeon must be verse with several reconstructive options when restoring form and function in these unique regions. The emotional fallout with PTSD is a concern for any child who has suffered a dog bite attack. Prevention of dog bites requires a multifaceted approach as the tendency of a dog to bite is affected by genetic predisposition, intrinsic aggressive behavior, socialization, training, maltreatment and care issues, adult supervision, and victim behavior.