It is imperative for facial trauma surgeons to be aware of the key anatomic and physiologic differences in children and adults. Furthermore, emergencies, such as septal hematomas and the classic “trap-door” orbital floor fracture, need to be identified as soon as possible. Treating surgeons only have one opportunity for ideal primary repair and thus when surgical intervention is required it should be completed in a timely fashion.
9.1 Pediatric Nasal Fractures
Nasal fractures have been reported to make up nearly half of all facial fractures in children [6]. However, there are several key anatomical differences in very young children that make nasal fractures generally uncommon. This is due to the underdeveloped nasal bones, which at this age are soft cartilage. Fractures are thus less likely, but septal cartilage dislocation can occur causing airway obstruction and future growth deformities [7]. However, as the patient grows and the nasal bones calcify fracture patterns tend to follow adult patterns.
Evaluation should always start with a thorough history and physical exam, but this takes place after the primary survey. A few important physical exam findings to note are presence of lacerations, crepitus, deviation, and edema. Pictures of the patient’s uninjured nose can give guidance on original position and degree of deviation. A school ID or if the patient is old enough to drive, a driver license can also help. Photographs of the injury should also be taken, as this could represent important documentation in cases resulting from non-accidental trauma. It is essential to always complete an intranasal examination with a nasal speculum. This is done to rule out the presence of a septal hematoma. The presence of a septal hematoma is an emergency and should be treated immediately. Treatment constitutes local anesthesia and aspiration with large-bore needle either for small hematomas or for larger hematoma drainage via an incision with 11 blade and packing with iodoform gauze is necessary. If missed, septal cartilage necrosis will occur resulting in a saddle-nose deformity. If complex injuries are suspected to the inferior meatus, turbinates, or posterior inferior septal junction of the perpendicular plate of the ethmoid, which cannot be evaluated with a nasal speculum, endoscopic examination can be completed by an individual trained in such techniques [8].
Considering that nasal bone fractures can occur concomitantly with orbital and nasoethmoid fractures it is appropriate to order computed tomographic imaging [9]. Three-dimensional CT scan reconstruction can be a helpful adjunct. Although imaging is helpful in diagnosis, physical exam findings take precedence when making the final decision on treatment modality.
If the nasal fracture is displaced and surgery is indicated, it is best to take the patient to the operating room and perform the procedures with general anesthesia. Pediatric nasal fractures should be reduced within 3–7 days [7]. After the patient is intubated, local anesthesia should be obtained. This can be completed with intranasal packs of cocaine, or 2% lidocaine with epinephrine. After achieving adequate anesthesia a Boies nasal fracture elevator or Asch forceps can be used. Once placed underneath the nasal bones an upward outward pressure is applied with simultaneous guiding external digital pressure. Once the surgeon is satisfied with the reduction of the external nasal bone fractures, direct pressure can be applied to the nasal septum. Bilateral intranasal packing or splinting should be kept for 2–3 days and an external splint should be in place for 10–12 days to prevent movement of nasal bones and to facilitate healing in the desired anatomical orientation. The treating surgeon should have a discussion with the patient and patient’s family to help guide expectations. Closed reduction mainly prevents a noticeable deformity, but may not achieve complete preinjury form. The patient and patient’s family should always be made aware of the option for delayed open reduction and rhinoplasty. Complications usually result from septal hematomas that are not managed appropriately. Poorly sutured nasal lacerations can result in synechia. Nasal growth disturbances have been reported when fractures involve the septovomerine sutures [10]. These issues can be corrected via secondary post-traumatic rhinoplasty; however, purely esthetic cases should not be completed until the patient is an adult and growth is completed [4].
9.2 Pediatric Orbit Fractures
There are far fewer studies describing pediatric orbital fractures when compared to adults. Most studies are relatively small retrospective case series [11–13]. Furthermore, several different specialties, such as plastic surgery, otolaryngology, oculoplastic surgery, and oral and maxillofacial surgery, often cover pediatric facial trauma at large academic institutions. Each specialty may have specific treatment preferences, which makes having a common practice algorithm difficult. In general, pediatric orbital fracture patterns are typically age dependent; for example, orbital roof fractures typically occur in younger children, whereas orbital floor fractures are more common in older children. Specifically, the probability of fracturing the lower orbits exceeds fracturing the orbital roof at age 7 [14]. Pediatric orbital injuries have been reported to make up to 20% of pediatric facial fractures [15, 16]. Indeed, in a series of 772 facial fractures in children, orbital fractures were the most common fracture type at any age group [17]. The most common cause of pediatric orbital fractures was motor vehicle accidents; however, like nasal fractures above, sports tend to increase in cause as patients age. Boys are more likely to be affected than girls [17].
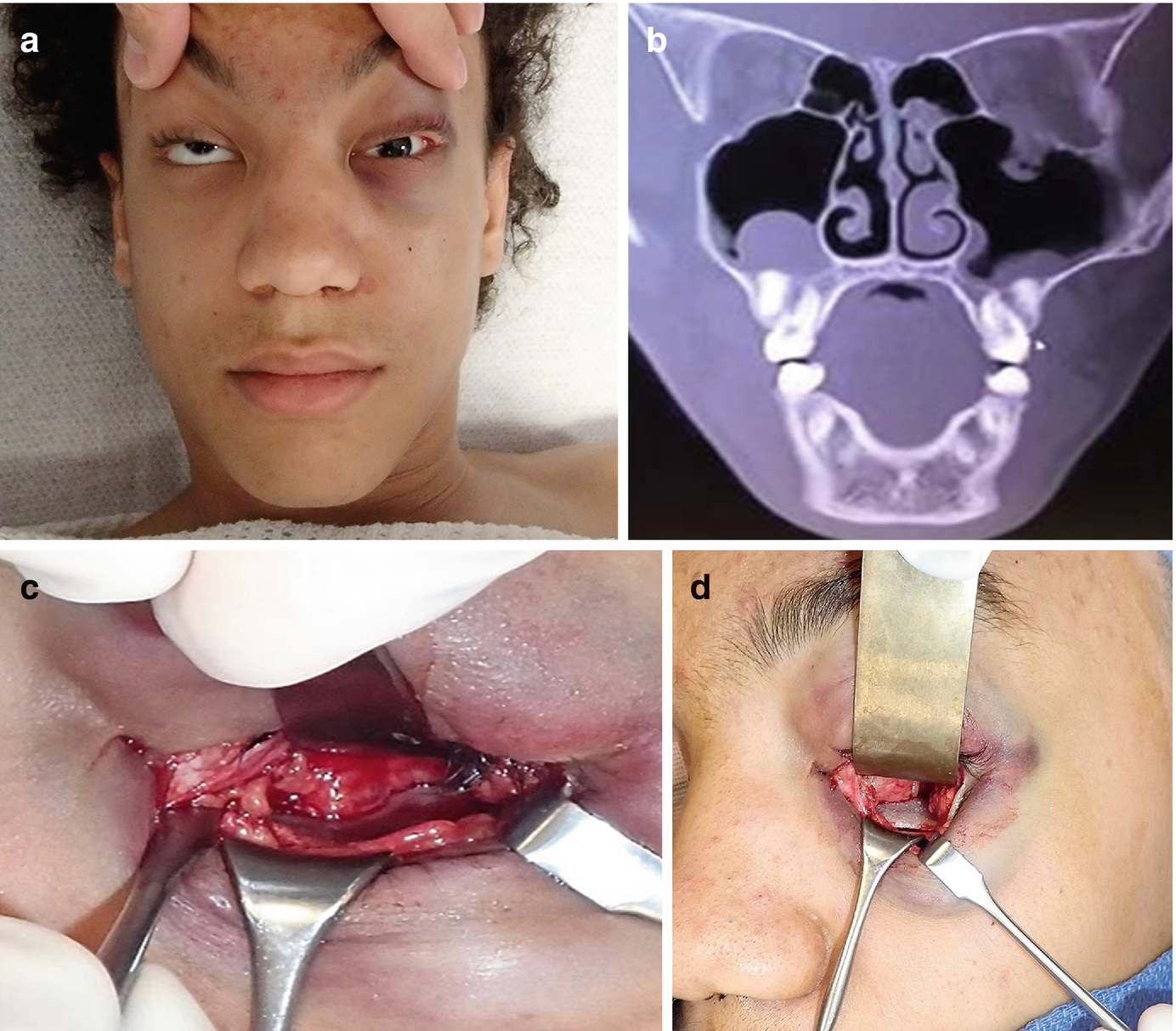
A case of a 14-year-old boy with left orbital floor fracture. (a) Clinical photograph clearly demonstrating entrapment and classic appearance of the “white-eyed” blowout fracture. (b) Coronal CT computed tomographic scan demonstrating herniation of ocular contents. (c) Exposure of the fracture via a transconjunctival approach. (d) Placement of implant
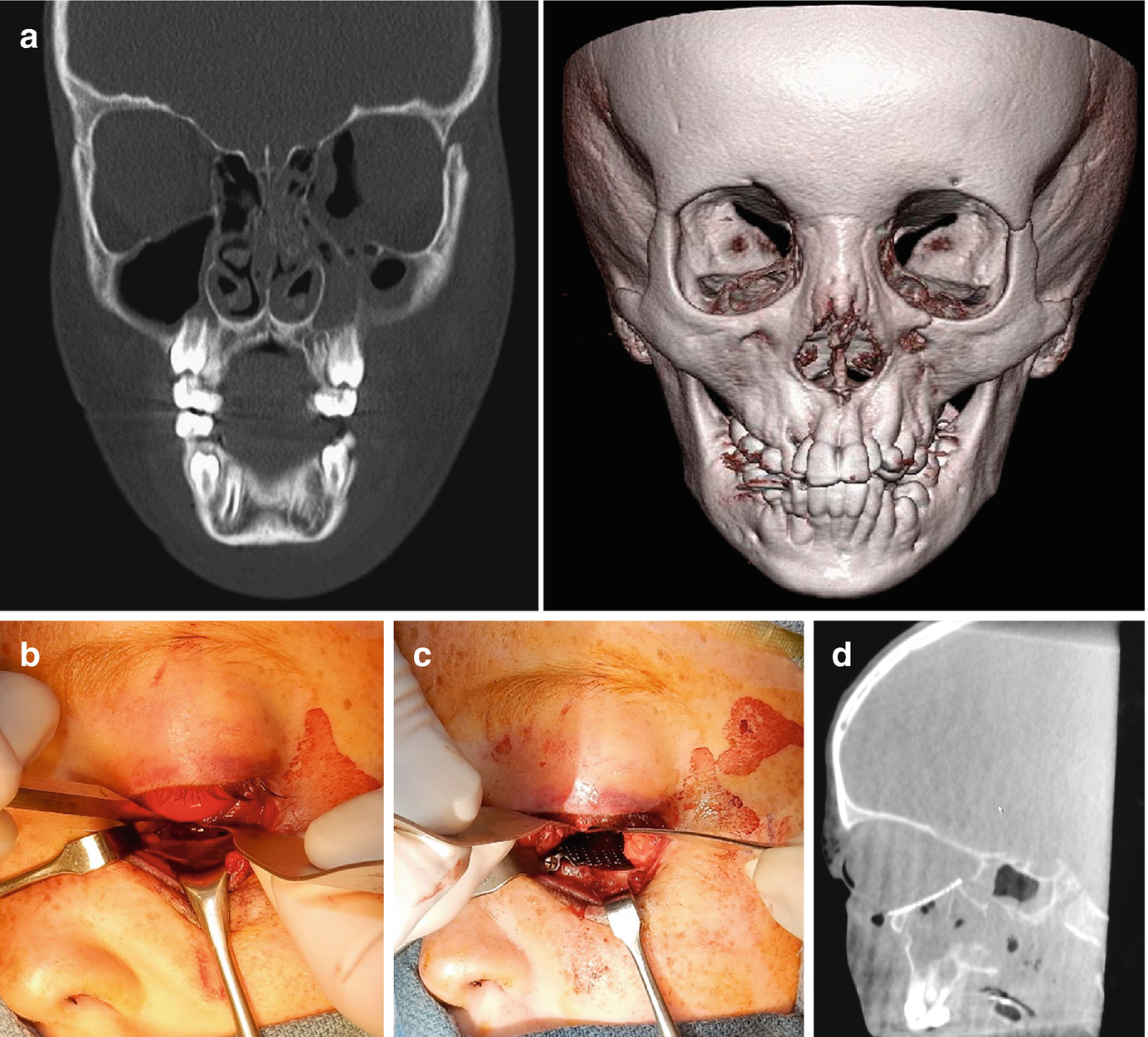
A case of an 11-year-old boy with left orbital floor and medial orbital wall fracture after an ATV accident. (a) Coronal computed tomographic scan (left) and 3-dimensional reconstruction demonstrating the fractures. (b) Exposure of the fracture via a subconjunctival approach with lateral canthotomy. (c) Placement of titanium orbital implant. (d) Intraoperative CT scan in the sagittal plane demonstrating appropriate orientation of implant
Fractures involving the orbital roof and supraorbital rim generally occur in children less than 7 years of age [14]. As a general rule, these fractures are managed conservatively [28]. Considering the anatomic location, the possibility of simultaneous neurocranial injury is high. Specific indications to proceed with surgical intervention are impairment of ocular movements, dural tear/leaking of cerebrospinal fluid, and finally injuries resulting in esthetic issues or severely displaced fractures [13]. Consultation and surgery with our neurosurgical colleagues may be indicated. The surgical approach that gives the best access to fracture sites in this area is the bicoronal approach. This approach allows for direct visualization of fracture segments facilitating reduction and direct stabilization of the bones. Resorbable plates and screws can be used in these fractures [29]. Patients should be followed closely postoperatively to monitor resolution of not only symptoms from fractures of the craniofacial skeleton but also related injuries to the dura and brain if present.
9.3 Conclusions
It is important for clinicians to be aware of the differences in treating facial factures of adults and children. Any treatment rendered should minimize the long-term disruption of facial growth. The clinician should be acutely aware of the importance of diagnosing septal hematomas. Furthermore, closed management of nasal fractures is preferred. Children with orbital floor fractures requiring surgical intervention should be completed within 24–72 h.