CHAPTER 5
Eruption and Shedding of Teeth
Göran Koch, Sven Kreiborg, and Jens O. Andreasen
Chronology of normal tooth eruption
Primary dentition
The chronology of eruption of primary teeth for Swedish children is given in Box 5.1. The sequence of eruption and the timing of eruption for each tooth are similar for both sexes. The variability in the age of the children at emergence of the individual teeth is relatively small, with standard deviations of 2–3 months. On average, the eruption of primary teeth begins at about the age of 8 months with the mandibular central incisors, and ends at the age of about 30 months with the maxillary second molars. Thus, in most children the total period of eruption of primary teeth spans about 2 years.
Permanent dentition
The chronology of eruption of permanent teeth (except for the third molars) for Danish children is given in Box 5.2. The sequence of tooth eruption is almost identical for both sexes. However, all teeth erupt significantly earlier in girls than in boys. The sex difference in eruption times averages approximately 6 months. There is, however, no appreciable difference in the variability of the eruption times between the sexes. In general, the variability in eruption times for the permanent dentition is much larger than the variability observed in the primary dentition, with standard deviations of 8–18 months (about five times greater than in the primary dentition). The smallest variability in time of emergence is observed for the first molars and incisors, whereas the largest variabilities are found for the canines and premolars in each jaw. The eruption of the permanent dentition begins with eruption of the mandibular central incisors at 6 years of age and ends with the eruption of the maxillary second molars at 12 years. Thus, in most children, the total period of eruption of permanent teeth (except for the third molars) spans about 6 years. In both sexes, a tendency for grouped emergence is noted, the teeth within a group showing similar mean times of emergence. The following groups are distinguishable:
- first molars in each jaw and the mandibular central incisors
- maxillary central and mandibular lateral incisors
- mandibular canines and the first premolars in both jaws
- maxillary canines and the second premolars in both jaws
- second molars in both jaws.
Mechanism and theories of tooth eruption
Tooth eruption is defined as the movement of a tooth, primarily in the axial direction, from its site of development in the jaw bone to its functional position in the oral cavity. This process continues, in principle, until the tooth meets the teeth in the opposing jaw. However, with the subsequent growth of the jaws and alveolar processes the teeth will exhibit continued vertical, mesial, and transverse drift until adult age. In addition, even through the second to fifth decade of life very slow but continuous eruption and alveolar growth have been documented.
The eruption phase has been divided into the following stages: pre‐eruptive; intraosseous; mucosal penetration; preocclusal; and postocclusal.
In the pre‐eruptive stage, the tooth crown is formed and the position of the tooth in the jaw bone is relatively stable. When the root begins to form, the tooth starts moving inside the jaw bone towards the oral cavity (the intraosseous stage). The eruption path is, for most teeth, not only through the bone, but also through the roots of the primary teeth. The mucosal penetration stage occurs, in general, when half to three‐fourths of the root of the erupting tooth is formed. The preocclusal stage is relatively short (a few months), whereas the postocclusal stage is much longer (several years) and is characterized by much slower tooth movement. Although the movement of teeth during eruption primarily occurs in the axial direction, the teeth actually move in all three planes of space. Apart from the rather precise eruption pattern of various tooth types there appears to be an individual very precise eruption time for homologous teeth, i.e., that left–right‐side eruption should not deviate by more than 2–4 months. If that is not the case then an eruption obstacle may be present [1].
Until recently, clinical studies of tooth eruption have been based on two‐dimensional X‐rays. However, with newer medical imaging techniques, such as computed tomography and magnetic resonance scanning, three‐dimensional analysis of tooth eruption has become possible (Figure 5.1a,b). With these technologies more accurate determination of the eruption path of individual teeth is now possible.

Figure 5.1 Transparent mandible at age 10 years. (a) Frontal view. Mental foramina, and segmented teeth (posterior to the incisors) from four different ages (0, 1, 7, and 10 years) are aligned automatically on the symphysis menti and the mandibular canals. Only the teeth and the mental foramen on the right side are illustrated. Lines indicate the eruption paths of the individual teeth. Tooth color code: purple = permanent third molar, blue = permanent second molar, red = permanent first molar, green = permanent premolars and the permanent canine. The mental foramen = blue. The symphysis menti = yellow. The mandibular canals = pink. (b) Lateral view. Lines indicate the eruption paths of the individual teeth. Color coding is the same as in part (a).
The eruption path is determined by genetic and local environmental factors. One of the most important local environmental factors is crowding among the developing and erupting teeth [2].
Tooth eruption is a biological process which is still not fully understood. The process is accompanied by multiple tissue changes, such as resorption and apposition of the alveolar bone, and development of the root and periodontium.
The eruption mechanism has for a long time been under investigation and several theories have been proposed, including eight different explanations of how eruption takes place [2,3]. At present, the “polarized follicle theory” is possibly the one which can best explain the initial stages of tooth eruption in humans (Figure 5.2). According to this theory, the coronal part of the follicle will start its resorbing activity when root formation starts. This process is coordinated by selective bone growth in the apical part of the follicle. Due to this coordinated osteoclast/osteoblast activity an eruptive movement of the tooth will take place. The direction of this movement is apparently directed by an eruption canal, a canal in the bone filled with an odontogenic mesenchymal tissue with odontogenic epithelial islands. This will expand during eruption, and thereby guide the tooth into its right position in the jaw. When the erupting permanent tooth has resorbed the overlying primary tooth and/or bone, the next step is to penetrate the oral mucosa (usually when half to three‐fourths of the root is formed). The coronal part of the follicle with the reduced enamel epithelium has been shown to possess the necessary collagenase activity to allow the permanent tooth germ to penetrate the mucosa (however, large amounts of fibrous tissue may present an obstacle to eruption; see later). After mucosal penetration, a fast extraalveolar eruption takes place, possibly related to periodontal ligament (PDL) traction and/or apical alveolar bone formation. Finally, when occlusion has been reached, vertical and horizontal changes can occur and the mechanisms for these events are largely unknown.

Figure 5.2 Histologic section of a human second premolar in its initial stage of eruption. In the figure various theories behind eruption are presented. Experimental studies have shown that the following mechanisms might only play a minor role in eruption, namely: PDL and pulp tissue pressure (6 and 7), coiled vessels creating a slight tissue pressure (8 and 6), pulpal growth (4) and root elongation (3). The most important mechanisms appear to be tissue changes induced by the follicle, namely, induced coronal resorption and apical bone apposition (1 and 5). PDL traction (2) may play a role after penetration of the oral mucosa.
Source: Marks et al. 1997 [3]. Reproduced with permission of Munksgaard.
Longitudinal studies of aplasia sites with persistent primary teeth have shown that over a 10‐year period, approximately 10% of the teeth showed very little resorption whereas the remaining teeth showed an average loss of approximately 5% root length each year [4].
Mechanism of shedding of primary teeth
Prior to shedding of primary incisors, canines and molars, the roots of the primary teeth are resorbed and their crowns shed. Dentinoclasts appear on the apical surface of the roots of the primary teeth, possibly initiated by the pressure created by the dental sac of the erupting permanent teeth. However, even if a permanent tooth is missing, the primary predecessor usually undergoes root resorption, although commonly at a much slower pace. The role of pulpal dentinoclasts in this process is still being investigated.
Figure 5.2 illustrates the histologic picture during resorption of the roots of a primary mandibular second molar in connection with eruption of the second premolar. Figure 5.3 shows the histologic picture of the resorption of the palatal part of the root in a primary maxillary central incisor during eruption of the permanent maxillary central incisor.
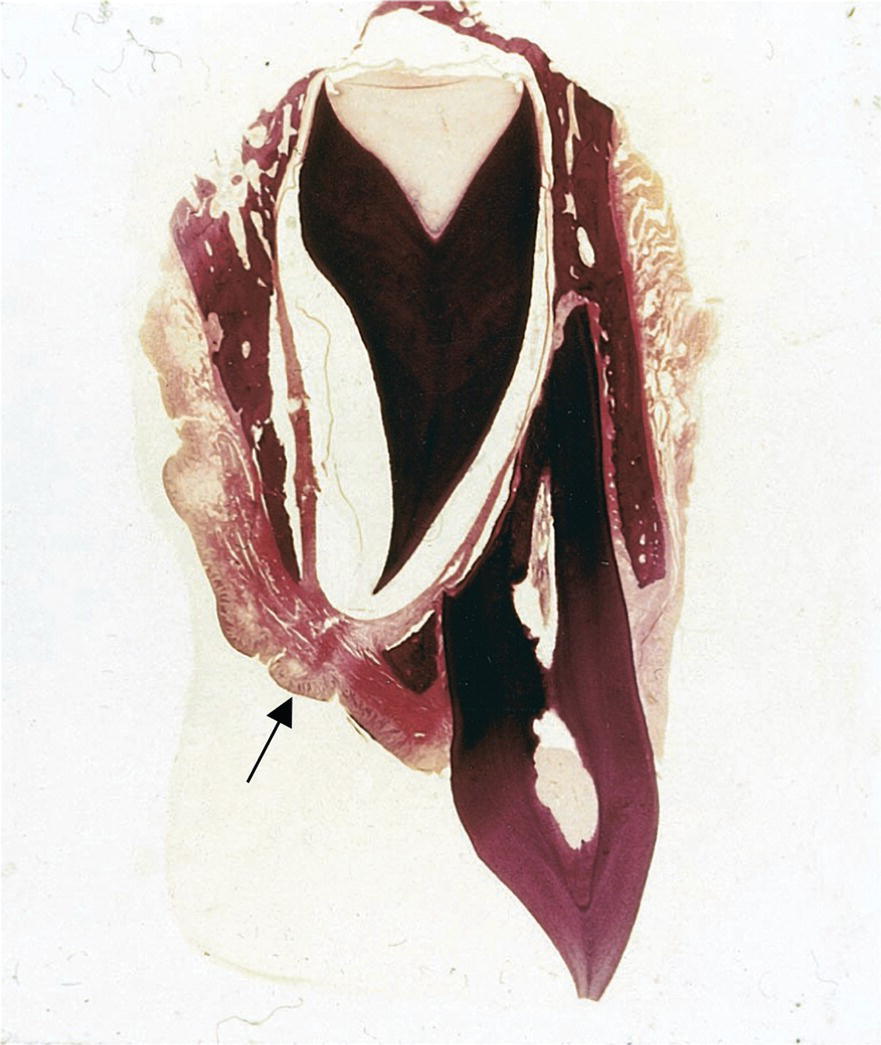
Figure 5.3 Histologic findings associated with the palatal resorption of a primary maxillary central incisor during eruption of the permanent incisor. Note also the presence of the eruption canal (arrow).
Systemic disturbances affecting tooth eruption and shedding
A number of systemic diseases and syndromes affect tooth eruption and shedding of primary teeth. Premature tooth eruption and shedding of primary teeth are far more common than delayed eruption and shedding. In general, delay in eruption in the primary dentition is associated with delay in the permanent dentition, and the delay in the permanent dentition is mostly more pronounced than in the primary dentition.
Premature tooth eruption
Natal or neonatal teeth have been shown to occur in about 50 different syndromes. Of these, about 10 syndromes are associated with chromosomal aberrations, e.g., trisomy 13. Among other syndromes are Hallermann–Streiff syndrome and Ellis–van Creveld syndrome.
Delayed tooth eruption
In general, children with chronic diseases show delay in both physical and dental development, and will, consequently, show delayed tooth eruption. Several general diseases, including more than 150 different syndromes, have been shown to exhibit delayed tooth eruption [5].
Endocrinopathies and chromosomal aberrations
Endrocrinopathies, such as hypopituitarism, hypothyroidism, and hypoparathyroidism, often result in retardation of dental emergence in both the primary and the permanent dentition. Many chromosomal aberrations, including trisomy 21 (Down syndrome), are associated with delayed tooth eruption.
Syndromes
Many syndromes, and especially those involving skeletal dysplasias with disturbed bone metabolism, show severely retarded or arrested tooth eruption.
In the following, a few relevant examples will be given.
Subjects with cleidocranial dysplasia (CCD) are characterized by short stature, aplasia or hypoplasia of the clavicles, and severe disturbances in cranial ossification. These patients often develop numerous supernumerary permanent teeth occlusal to the normal permanent teeth. Tooth eruption is delayed in both the primary and permanent dentitions, but the delay is most severe in the permanent dentition, often with arrest of eruption and multiple retentions of both normal and supernumerary teeth. The disturbances in tooth eruption are related both to the skeletal pathology with retardation of osteoblast, osteoclast, and odontoclast differentiation, and to the presence of supernumerary teeth. Thus, even in regions without supernumerary teeth, shedding of primary teeth and eruption of permanent teeth can be extremely delayed or arrested (Figure 5.4). Therefore, children with CCD should be monitored for disturbances in tooth eruption (and other dental abnormalities) from early childhood, and treatment should be instituted as early as possible [6–9].
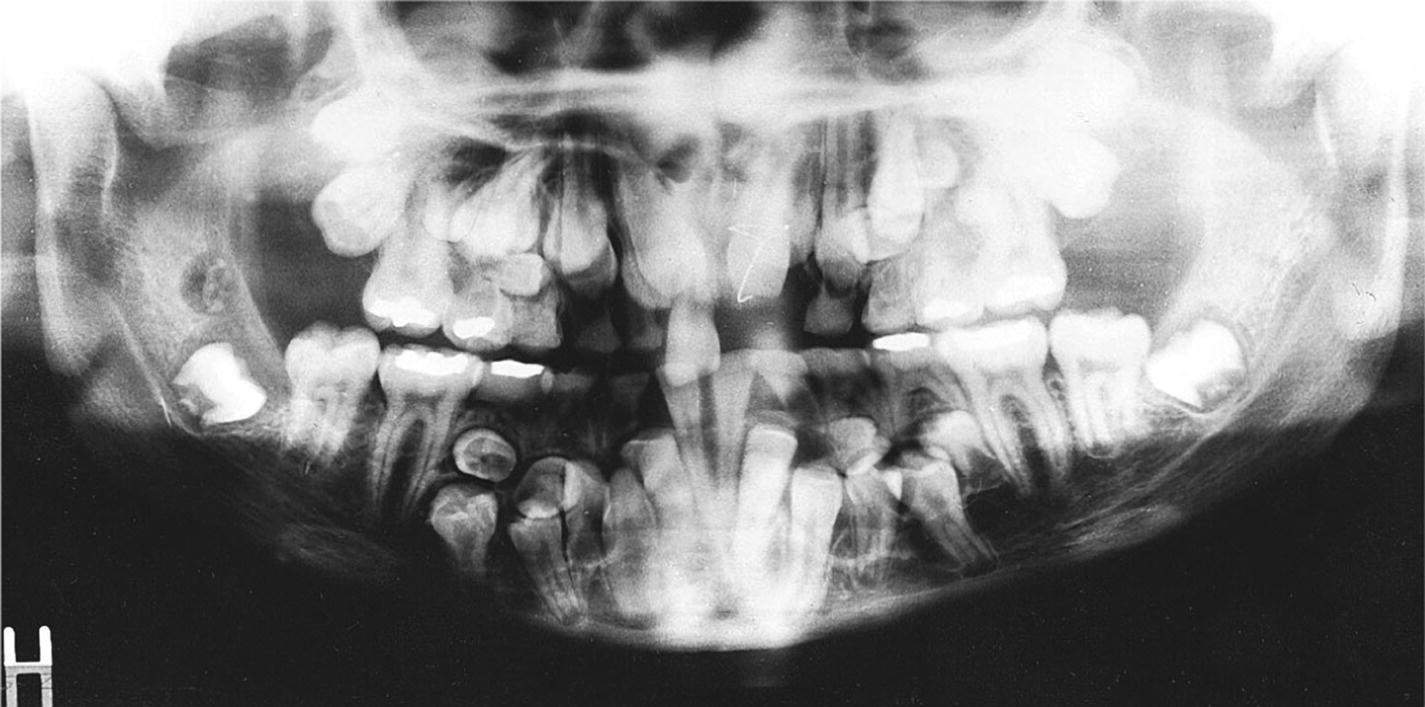
Figure 5.4 Orthopantomogram of a 16‐year‐old boy with cleidocranial dysplasia. Note the numerous supernumerary permanent teeth and the arrested eruption of many of the normal permanent teeth.
Subjects with tricho‐dento‐osseous syndrome (TDO) are characterized by disturbances in the development of hair, teeth, and bones. The patients are of normal height, but the skeleton, including the craniofacial skeleton, is dense and reveals disturbed bone remodeling with reduced osteoclastic activity. Tooth eruption is delayed in both dentitions, but most severely so in the permanent dentition, which may also show arrested eruption leading to retention of several permanent teeth (Figure 5.5). The cause of the eruption problems is related to the reduced osteoclastic activity. Therefore, children with TDO should be monitored for disturbances in tooth eruption (and other dental abnormalities) from early childhood, and treatment should be carried out as early as possible [9].

Figure 5.5 Orthopantomogram of a 13‐year‐old girl with tricho‐dento‐osseous syndrome. Note the severely delayed eruption of several permanent teeth and the dense jaw bones.
Subjects with pycnodysostosis are characterized by short stature, caused by shortening of the extremities. The skeleton, including the craniofacial skeleton, is characterized by osteopetrosis with increased bone fragility. The increased bone density of the jaws, combined with pronounced crowding, leads to delayed eruption in both dentitions, but is most pronounced in the permanent dentition. Thus, the permanent dentition may even show arrested tooth eruption and several other dental abnormalities (Figure 5.6). These children should be monitored for disturbances in tooth eruption from early childhood, and treatment should take place as early as possible [10].

Figure 5.6 Orthopantomogram of a 10‐year‐old boy with pycnodysostosis. Note the delayed eruption of several permanent teeth and the osteopetrotic bones.
Premature shedding of primary teeth
Systemic diseases that are associated with premature shedding of primary teeth include histiocytosis, hypophosphatasia, and neutropenia.
Histiocytosis is a symptom complex, which includes multiple eosinophilic granulomas, Hand–Schüller–Christian disease, and Letterer–Siwe disease. Early loss of posterior primary teeth is frequently observed, whereas the anterior teeth are less commonly involved.
Hypophosphatasia is a metabolic disease with impaired bone mineralization. The activity of alkaline phosphatase in plasma and tissues is reduced. Premature loosening and shedding of primary teeth are often seen. The anterior teeth are most frequently affected, whereas the primary molars are rarely involved. The teeth have a defect in cementum. There is often severe loss of alveolar bone with no or little gingival inflammation. The teeth are often shed without any signs of root resorption.
In neutropenia, the decrease in circulating neutrophils leads to lack of resistance to infection, which may predispose the children to gingivitis and periodontitis.
Premature shedding of primary teeth can occur in other diseases where the periodontium undergoes pathologic breakdown as seen in Papillon–Lefèvre syndrome (hyperkeratosis palmoplantaris with periodontoclasia), Down syndrome, and Ehlers–Danlos syndrome.
Other causes of premature shedding of primary teeth can be cystic lesions of the jaws, as seen in cherubism (Figure 5.7).
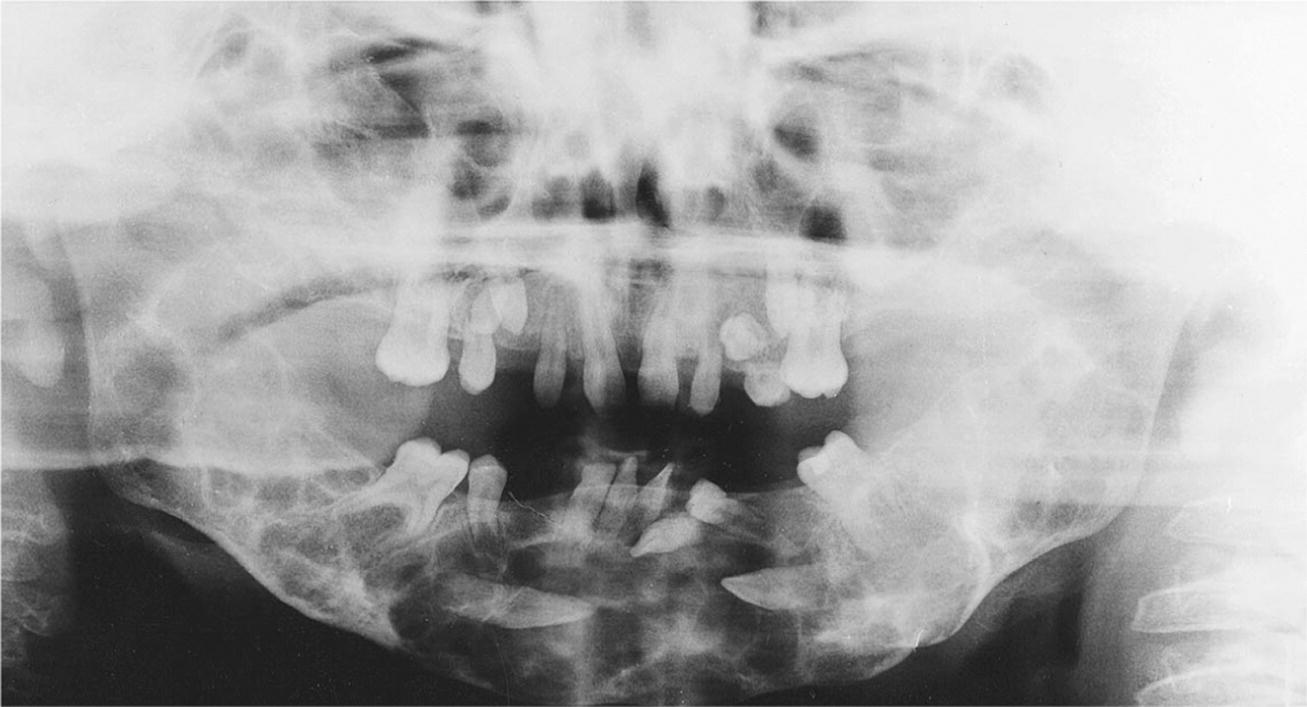
Figure 5.7 Orthopantomogram of 10‐year‐old boy with cherubism. The large cystic lesions in the maxilla and mandible have caused premature loss of primary teeth.
Local disturbances affecting tooth eruption and shedding
It is essential to diagnose where the obstacle for the eruption process is located. The overwhelming cause is crowding, which may lead to impaction, and if this is the case, dental arch expansion or extraction is indicated. Crowding often leads to follicle collisions where one follicle is placed on top of the other thereby leaving both teeth unerupted. Another frequent cause is an ectopic eruption path, and in these cases extraction of primary predecessors and/or surgical creation of a new eruption path are the treatments of choice. Sometimes orthodontic traction must be used. In the case of follicle and PDL pathology, arrest of eruption may occur; this condition is termed retention. Retention has further been divided into primary retention and secondary retention. Primary retention means that the eruption is arrested in the intraosseous stage due to pathology of the follicle and sometimes an ankylosis affecting either the crown or the root. Secondary retention means that an already erupted tooth due to ankylosis of the root is prevented from further eruption and thereby gradually comes more and more into infraocclusion. In the case of primary retention, the treatment of choice will normally be denudation of the tooth. In the case of secondary retention, the tooth is ankylosed, and should be surgically removed. Finally, an eruption disturbance can be diagnosed to be a delayed eruption. In asymmetric cases where expected eruption time on one side is exceeded by more than 4 months, surgical exposure is indicated.
In Table 5.1 various causes for noneruption of permanent teeth are listed according to tooth type.
Table 5.1 Most frequent causes of noneruption for various types of permanent teeth and suggested treatment
| Cause | Treatment | |
| Maxillary incisors | Dilaceration (trauma) | Surgical exposure |
| Supernumerary teeth | Surgical removal of supernumerary teeth | |
| Maxillary canines, palatal impaction | Unknown | Surgical exposure and orthodontic traction |
| Maxillary canines, labial impaction | Crowding | Expansion of dental arch or removal |
| Mandibular canines, ectopic position | Unknown | Surgical removal or transplantation |
| Maxillary second premolar | Crowding | Expansion of dental arch or removal |
| Mandibular second premolar | Unknown | According to tilting extraction of primary molar, surgical exposure or transplantation |
| Maxillary first molar, mesial tilt | Unknown | None or distalization of first molar |
| Mandibular first molar, mesial tilt | Unknown | None or distalization of first molar |
| Maxillary first molar, infraocclusion | Ankylosis | Extraction |
| Mandibular first molar, infraocclusion | Ankylosis | Extraction |
| Second maxillary molar | Follicle collision with third molar | Remove third or second molar (usually third molar) |
| Second mandibular molar | Follicle collision with third molar | Remove third or second molar (usually third molar) |
Local aberrations in primary dentition
Natal and neonatal tooth eruption
The frequency of natal or neonatal teeth is estimated at one case per 2000–3000 births and is equally common in boys and girls. Most of these premature erupting teeth are mandibular central incisors belonging to the normal dentition and they have a normal shape. The root has not yet developed and the tooth is loosely attached to the gingiva (Figure 5.8). The symptoms related to natal/neonatal teeth include gingivitis, extreme mobility, self‐mutilation of the tongue, and trauma to the mother’s breasts. Natal and neonatal teeth should be extracted only if they are loose enough to involve risk of aspiration or if feeding is severely disturbed.

Figure 5.8 Natal teeth in a 2‐day‐old girl.
Symptoms associated with “teething”
Often, the primary teeth pierce the gums without causing any symptoms. However, in some children local symptoms such as redness and swelling in the oral mucosa overlying the erupting tooth is found. These symptoms appear a few days before clinical eruption. The child may also show signs of local irritation, drooling, and sometimes slight fever. Treatment for teething troubles was formerly directed at both local and supposed general symptoms. Since local massage of the gum pads obviously relieves the discomfort, various remedies with which the gums can be rubbed have been proposed. A bite‐ring of rubber may be recommended because it is easy to clean, cannot be swallowed, and does not injure the gums.
Fibrotic mucosa and eruption cysts
Changes in the oral mucosa overlying the erupting tooth may cause eruption disturbances. If the child is chewing intensively on hard objects, the alveolar mucosa may turn more fibrotic and cause delayed eruption (Figure 5.9). In some cases surgical removal of the changed tissues might be necessary due to pain at chewing. A common finding in small children is eruption cysts. They are often swellings overlying an erupting tooth and may vary in size. They contain tissue fluid and sometimes some blood (eruption hematoma) accumulated superficially to the reduced enamel epithelium. In most cases no treatment is indicated since the changed mucosa will delay the eruption by only a few weeks. However, if the cyst is causing discomfort or the alveolar mucosa is pathologically thickened, surgical exposure of the tooth may be necessary. Similar changes are also found in the permanent dentition (Figure 5.10a,b).
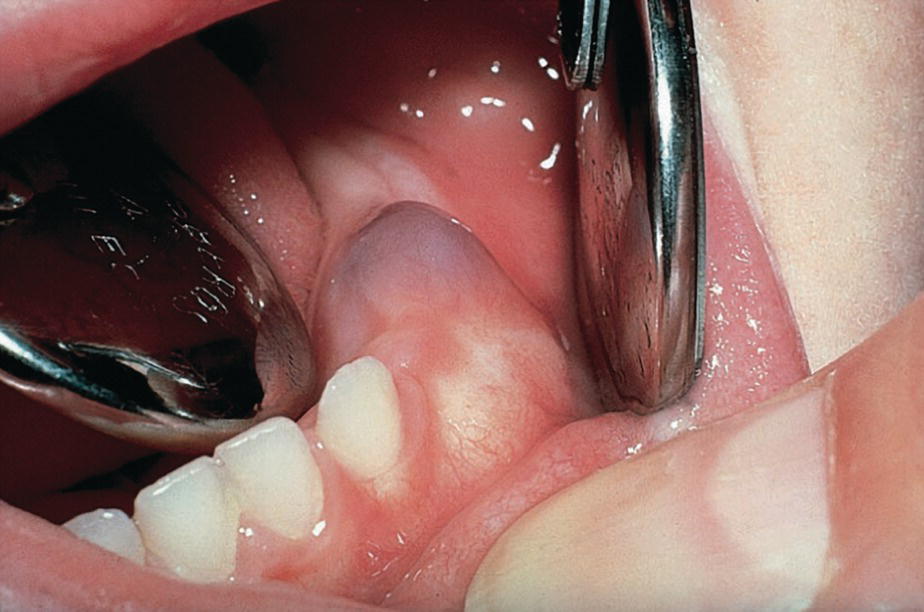
Figure 5.9 Fibrous gingival tissue delaying eruption of primary molars.
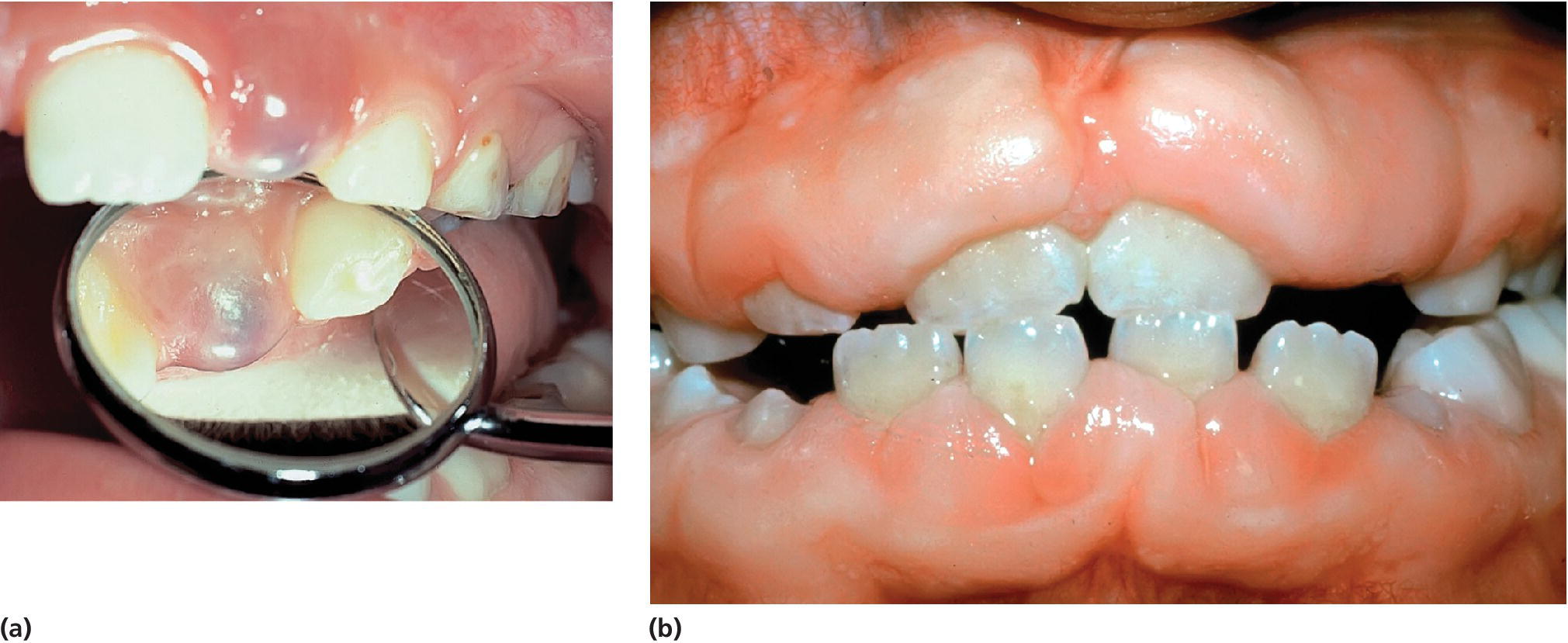
Figure 5.10 (a) Eruption cyst. (b) Gingival overgrowth caused by phenytoin medication influencing tooth eruption.
Infraocclusion of primary molars
The definition of infraocclusion is that a tooth is positioned 1 mm or more below the normal occlusion plane/level. Infraoccluded primary molars mostly reach occlusal contact before they develop ankylosis. Following vertical growth of the surrounding alveolar bone, the ankylosed tooth seems to gradually be submerged into an infraoccluded position. The diagnosis of ankylosis is difficult to verify by radiography but easy to establish by percussion test and the clinical picture. Infraocclusion of primary molars can be found as early as 3–4 years of age but is more predominant at 10 years of age; the aberration is then found in about 10% of the children. Infraocclusion has been found to be genetically influenced. The treatment depends on the presence of permanent successors to the infraoccluded tooth. If there is a permanent successor, normal exfoliation can be expected with a delay of 6–12 months (Figure 5.11) without removal of the ankylosed tooth. If the neighboring permanent tooth is severely tilting over the ankylosed tooth, early orthodontic correction may be indicated. In cases with no successor, the therapy planning must be based on the conclusion that normal exfoliation cannot be expected.

Figure 5.11 Infraocclusion of primary molars. Periapical radiographs of a boy followed from 11 years 7 months to 14 years 2 months of age. Left side, extraction side. Extraction resulted in the eruption 1 year earlier of the successor compared to the nonextraction side. Normal marginal alveolar bone height at end of observational period.
Source: J. Kurol, 1984. Reproduced with permission of Swedish Dental Association.
Retention of primary teeth
The primary tooth that is most commonly involved is the maxillary second molar. The tooth anlage is malpositioned and often the roots bend and follow the wall of the sinus during development (Figure 5.12). This means that spontaneous eruption cannot be expected. The impacted tooth can cause tilting of the permanent molar and disturbance in eruption of the permanent premolars. The impacted primary tooth has to be surgically removed. Also the primary second molar in the mandible may become retained and thereby lead to severe eruption problems for the permanent successor.
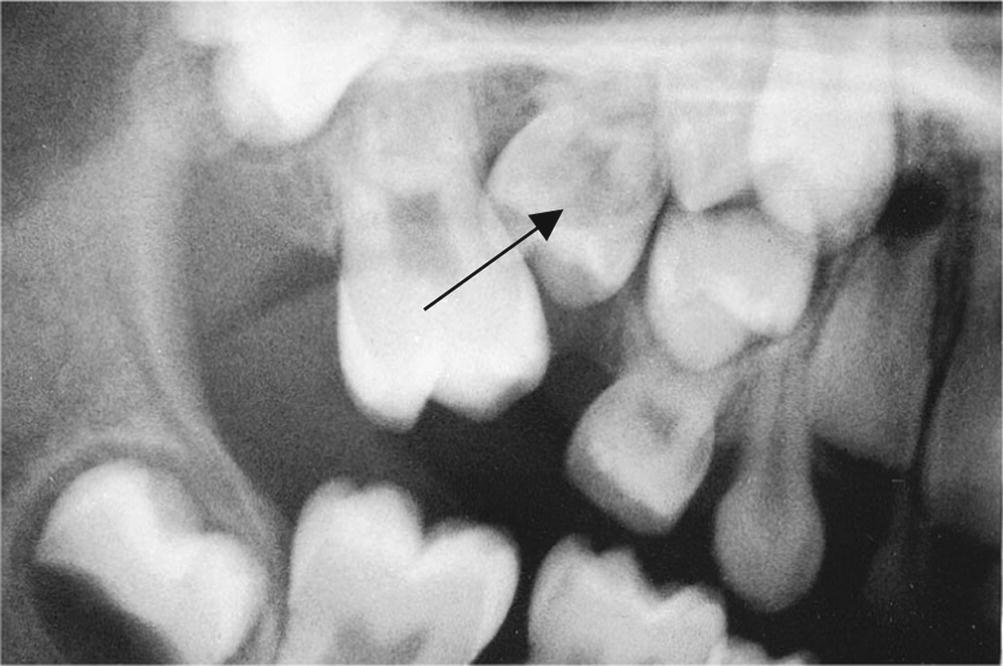
Figure 5.12 Impacted primary maxillary second molar (arrow) causing eruption disturbances for the permanent premolars.
Local aberrations in permanent dentition
Disturbances in eruption are common in the permanent dentition. Besides the normal variation in eruption time a number of genetic disorders, diseases, and syndromes can affect tooth eruption as has been described earlier in this chapter. However, the most frequent disturbances in tooth eruption in the permanent dentition are local in origin (Box 5.3).
Ectopic eruption
In crowded arches the maxillary first molar may be impacted by the distal surface prominence of the primary second molar (Figure 5.13). The primary molar will be resorbed at the distal root surface, the permanent molar gets stuck, and the eruption stops. However, it has been reported that spontaneous correction occurs in about half of the cases. A reasonable observational period is therefore recommended before extraction of the primary tooth or orthodontic treatment is performed.
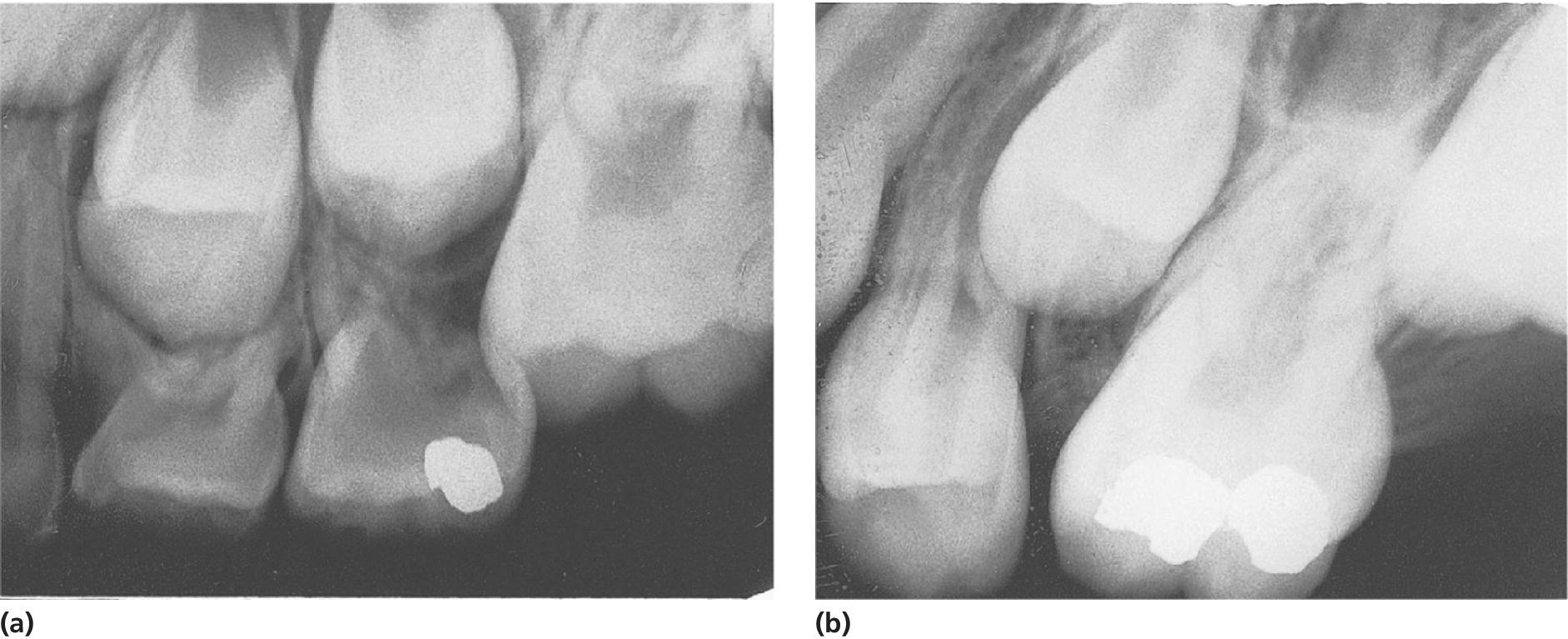
Figure 5.13 (a) Retention of permanent maxillary first molar caused by the primary second molar. (b) After extraction/exfoliation of the primary tooth, loss of space will often occur.
Ectopic eruption of maxillary canines occurs in about 2% of children. It has been reported that 12% of these ectopically erupting canines will cause different degrees of resorption of the root of adjacent incisors (Figure 5.14). It is therefore important, as a matter of routine, always to palpate buccally and palatinally for the canine when the child is 9–10 years old. If the canine cannot be palpated buccally, a detailed radiographic examination has to be carried out to reveal any resorptions or risk for resorptions of neighboring teeth. The treatment in case of resorption will be to change the eruption direction of the canine. This can in most cases be achieved by extraction of the primary canine. In severe cases, orthodontic intervention is necessary, including surgical exposure of the canine and a fixed appliance to place the tooth in a proper eruption path (see also Chapter 21).

Figure 5.14 Ectopic eruption of left maxillary canine which has resorbed the root of the left maxillary lateral incisor. Extraction of the primary left maxillary canine result in a changed path of eruption of the permanent canine. The resorption stopped and a normal periodontal condition was established.
Ectopically, labial late eruption of maxillary central incisors can occur as a result of early trauma in the region, odontomas or supernumerary teeth. Due to positioning and root angulation they sometimes tend to erupt in the vestibulum mucosa. After surgical exposure the incisor often erupts unaided and will end up in the right position and with reinstituted mucosa (Figure 5.15a,b). In children with crowded arches it is common that the second premolar in the maxilla will be displaced and erupt palatinally (Figure 5.16) while the mandibular second premolar has a tendency to be impacted in a central position in the jaw. The treatment in the maxilla is mainly extraction of the ectopically erupting tooth, while in the mandible the first premolar may often be extracted and the impacted second premolar will erupt. Alternatively, a persistent second primary molar should be extracted which in many cases will lead to eruption of the ectopic premolar.
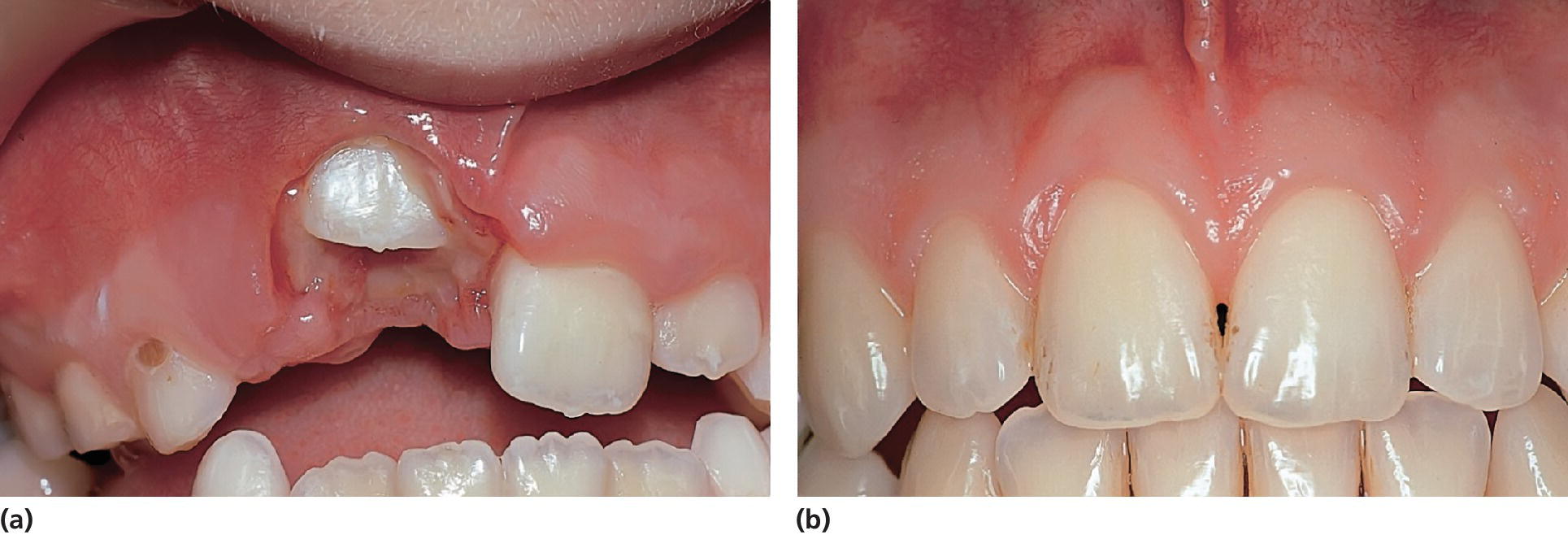
Figure 5.15 (a) Ectopic position of right maxillary central incisor due to a supernumerary tooth in the region causing root angulation and displacement of the central incisor. After removal of the supernumerary tooth and surgical exposure the central incisor erupted. (b) Eight years later.

Figure 5.16 Maxillary second premolar erupting in the palate due to crowding.
Ectopic malpositions
In children with malposition of teeth, e.g., premolars or canines horizontally situated in the jaw, the most common treatment is surgical removal. However, if there is space enough, a surgical exposure can result in a spontaneous eruption in the occlusal line (Figure 5.17a to 5.17c). Sometimes a malpositioned tooth may cause eruption disturbances of surrounding teeth. In children this can occur when a malpositioned third molar interferes with the eruption of the second molar (Figure 5.18).

Figure 5.17 (a) Late development of impacted mandibular second premolar in a 14‐year‐old boy. (b) Two years later and after surgical exposure. (c) After another 2 years, spontaneous eruption and completed root development had occurred.
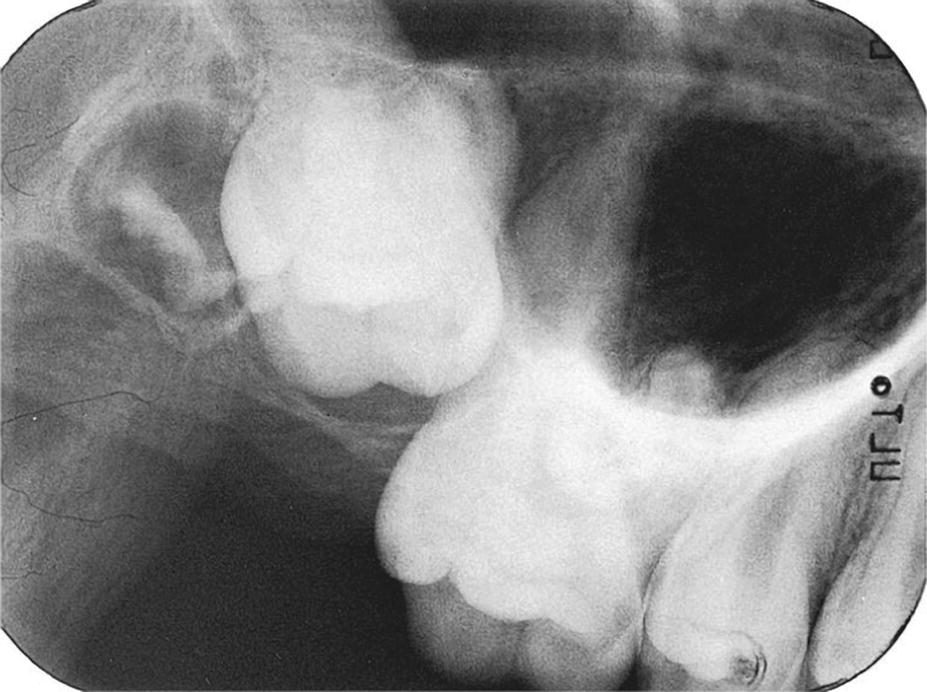
Figure 5.18 Ectopically positioned maxillary third molar disturbing eruption of the second molar in a 15‐year‐old boy. Observe the curved roots of the impacted tooth close to the sinus.
Sequelae to trauma
Traumatic injuries to the teeth involving intrusion of primary incisors may cause extensive damage of the developing permanent successor (see Chapters 18 and 19). The resulting dilaceration can cause severe disturbances in eruption. In approximately half of the cases there will be no eruption and the deformed tooth has either to be surgically removed or undergo a denudation procedure which will result in spontaneous eruption. Soon after this has occurred it is important to remove the dilacerated part of the crown and restore the tooth with composite. This will prevent bacteria from invading the pulp canal due to the invagination found in relation to the crown dilaceration. On the other hand, dilaceration might cause premature development and eruption (Figure 5.19).

Figure 5.19 Premature development and eruption of a dilacerated mandibular central incisor caused by intrusive trauma against the primary incisors at the age of 1 year.
Supernumerary teeth, mesiodentes, and odontomas
Supernumerary teeth, mesiodentes, and odontomas constitute major reasons for disturbances in tooth eruption (Figures 5.20 and 5.21). However, it has to be understood that not all supernumerary teeth, mesiodentes or odontomas will have an influence on eruption. Only if the follicle surrounding the tooth element is located in the eruption pathway will impaction (follicle collision) occur. Early diagnosis based on clinical and radiographic examinations is important to decide on the treatment and when it should be performed with an optimal result. In most cases the treatment involves surgical removal of the supernumerary teeth, mesiodentes, and odontomas.

Figure 5.20 Mesiodens interfering with eruption of a central incisor in a 10‐year‐old boy.
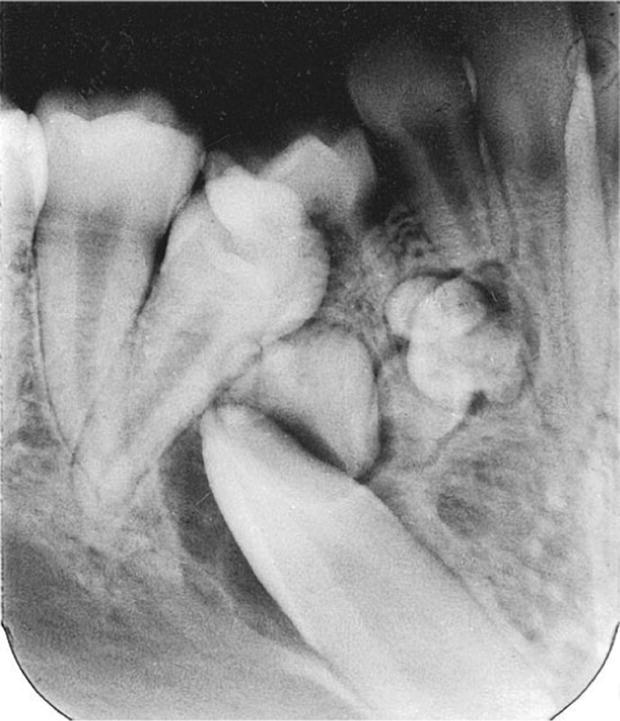
Figure 5.21 Odontoma interfering with eruption of a permanent mandibular canine.
Ankylosis
Infraocclusion and ankylosis of permanent incisors and first molars constitute a major clinical problem for the pediatric dentist. The ankylosis of incisors is often caused by traumatic injuries to the teeth and the treatment is discussed in Chapter 18. Diagnosis of ankylosis of a permanent molar is made following percussion test and the increasing infraposition of the tooth following growth (Figure 5.22a,b). A typical radiographic feature is an interradicular sign of ankylosis affecting the furcation area. Attempts to orthodontically extrude the ankylosed tooth will fail. The treatment of teeth with severe infraocclusion caused by ankylosis is surgical removal as soon as the diagnosis is made.
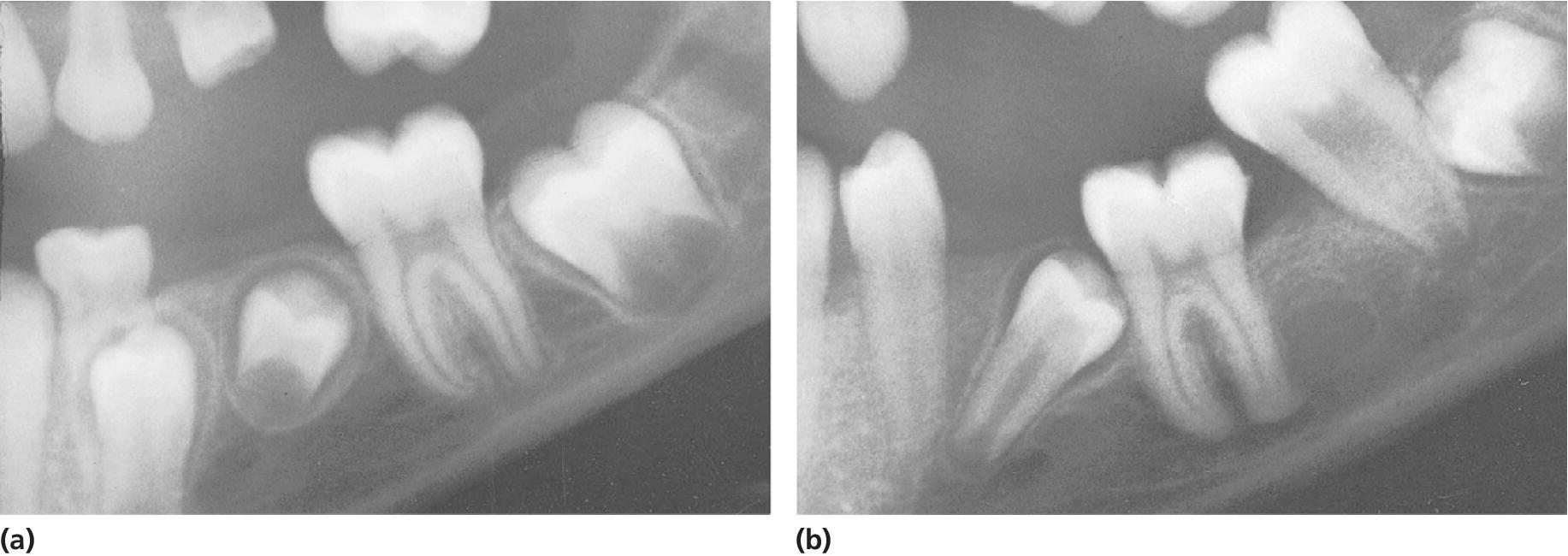
Figure 5.22 (a) An 8‐year‐old girl with history of several teeth in ankylosis. Percussion test revealed slight suspicion of ankylosis of permanent left mandibular first molar. (b) Four years later severe infraocclusion and ankylosis were verified.
Developmental disturbances
Tooth developmental disturbances such as morphologic aberrations and severe mineral disturbances can delay or inhibit the tooth eruption process, possibly due to defects in the coronal follicle. In cases with, for example, local odontodysplasia (“ghost teeth”) eruption will often not take place (Figure 5.23).

Figure 5.23 Odontodysplasia resulting in ceased eruption both in the primary and in the permanent dentition.
Cysts
The most common cysts causing tooth eruption problems are dentigerous (follicular) cysts. These cysts originate from the dental follicle of nonerupted teeth. The cysts can reach substantial size and thereby inhibit eruption of the involved tooth but can also displace surrounding tooth germs. The treatment of small cysts is enucleation but large cysts are recommended to be treated with decompression of the cyst to avoid post‐surgery defects (see Chapter 15). Normally eruption of the involved tooth can be expected after treatment (Figure 5.24a to 5.24d).

Figure 5.24 (a) A 12‐year‐old boy with a large dentigerous cyst emanating from nonerupted 37 and displacing germ of 38 high up in the mandible ramus. (b) Two months after fenestration of the cyst and rinsing with saline the cyst had been reduced. (c) Nine months later 37 was seen in the mouth. (d) Another two months later 37 was in occlusion and 38 could be removed with a minor surgical intervention.
Background literature
- Andreasen JO, Petersen JK, Laskin DM, eds. Textbook and color atlas of tooth impactions. Copenhagen: Munksgaard, 1997.
- Gorlin, RJ, Cohen MM Jr, Levin LS. Syndromes of the head and neck, 3rd edn. New York: Oxford University Press, 1990.
- Hall RK. Pediatric orofacial medicine and pathology. London: Chapman & Hall, 1994.
- Kurol J. Infraocclusion of primary molars. Thesis. Swed Dent J 1984; Suppl 21.
References
- 1. Haavikko K. The formation and the alveolar and clinical eruption of the permanent teeth. Suom Hammaasläk Toim 1970;66:103–70.
- 2. Marks SC, Schroeder HE. Tooth eruption: theories and facts. Anat Rec 1996;245:374–93.
- 3. Marks SC, Svendsen H, Andreasen JO. Theories of tooth eruption in humans. In: Andreasen JO, Kølsen Petersen J, Laskin DM, eds. Textbook and color atlas of tooth impactions. Copenhagen: Munksgaard, 1997; 20–43.
- 4. Rune B, Sarnaes KV. Root resorption and submergence in retained deciduous second molars. Eur J Orthod 1984;6:123–31.
- 5. Suri L, Gagari E, Vastardis H. Delayed tooth eruption: pathogenesis, diagnosis, and treatment. A literature review. Am J Orthod Dentofacial Orthop 2004;126:432–5.
- 6. Jensen BL, Kreiborg S. Development of the dentition in cleidocranial dysplasia. J Oral Pathol Med 1990;19:89–93.
- 7. Kreiborg S, Jensen BL, Larsen P, Schleidt DT, Darvann T. Anomalies of craniofacial skeleton and teeth in cleidocranial dysplasia. J Craniofac Genet Dev Biol 1999;19:75–9.
- 8. Kreiborg S. Syndromer med alvorlige dentitionsafvigelser. In: Hjørting‐Hansen E, ed. Odontologi ‘89. Copenhagen: Munksgaard, 1989; 161–76.
- 9. Østergaard RL, Kreiborg S, Niebuhr E. Trikodentoossøst syndrom. En oversigt og præsentation af et tilfælde. Tandlœgebladet 1999;103:326–9.
- 10. Østergaard RL, Kreiborg S, Niebuhr E. Pycnodysostosis. En oversigt og præsentation af et tilfælde. Tandlœgebladet 1999;103:508–11.
- 11. Lysell L, Magnusson B, Thilander B. Time and order of eruption of the primary teeth. A longitudinal study. Odontol Rev 1962;13:217–34.
- 12. Helm S, Seidler B. Timing of permanent tooth emergence in Danish children. Community Dent Oral Epidemiol 1974;2:122–9.