Abasic understanding of how cells are constructed and how they operate will allow for an appreciation of ketones and for their importance in the body, but especially in the brain.
The individual cells that make up the many tissues of our body are extremely complicated structures, much more than the simple cell with a nucleus and cytoplasm that older generations learned about in grade school. Each cell of our body requires fuel to operate. This fuel must pass through the membrane of the cell and be carried to a specialized part of the cell, called the mitochondrion, where it is processed into energy. The cell then uses this energy, called ATP (adenosine triphosphate), to keep itself in working order and also to produce proteins and other substances, which are different for each type of cell.
An amazing amount of activity goes on within the cell membrane. The processes that take place there decide what can enter and what can leave the cell. The cell membrane is made up of fatty molecules that line up in such a way that the fluids outside of the cell are repelled, thereby keeping the environment out of the cell. At the same time, the fluids inside the cell are protected, keeping the contents of the cell inside. Receptors for various substances sit on the cell membrane and act like keyholes in this process. When the right substance (the key) comes along and attaches to the receptors (the keyhole), this unlocks the door into the cell for a particular substance to enter.
One important example of this transport process, relevant to our concern here, involves the transport of glucose, the simplest form of carbohydrate, into the cell. When you eat something that contains carbohydrate, or sugar, it is broken down into smaller glucose (blood sugar) molecules, and this event signals the pancreas to release insulin, a hormone. Insulin (the key) must attach to the insulin receptor (the keyhole) so that glucose can be allowed into the cell. A transport protein, named GLUT for glucose transporter, carries glucose through the cell membrane and releases the glucose inside of the cell. Different types of cells use different GLUTs. Once inside the cell, the molecules of glucose make their way to the mitochondria, the energy plants of the cell. This sets off a complex chain reaction involving many enzymes and other substances to make the final, important energy particle called ATP.
When everything is normal, every cell membrane has insulin receptors so all the cells can use glucose as fuel. But if insulin receptors are absent, there is no way for glucose to enter the cell and be turned into ATP. This in turn can lead to serious health problems such as diabetes mellitus.
Diabetes mellitus is a group of conditions that involves a problem with the way the body metabolizes glucose; specifically, the levels of glucose in the blood are abnormally high, although the reasons for this differ. Diabetes is one of the most common chronic conditions, affecting nearly 26 million people in the United States, or 8.3 percent of the population, according to the National Diabetes Fact Sheet 2011 from the Centers for Disease Control (CDC) and Prevention. In addition, an astounding 79 million people, or one in four, have prediabetes, meaning that levels of glucose are elevated but not quite to the levels of those seen in diabetes. People with prediabetes are at high risk of developing diabetes but can often avoid this by close attention to diet and exercise.
Diabetes becomes more common as we age, affecting about 3.7 percent of people between twenty and forty-four and gradually increasing to nearly 27 percent of people who are sixty-five or older. Also, about half the U.S. population sixty-five and older have prediabetes, therefore more than three-quarters of the people in this age group either have diabetes or are at high risk of developing diabetes.
People with diabetes mellitus often develop other chronic conditions: it is the leading cause of kidney failure, representing about 44 percent of cases, and is also the leading cause of new cases of blindness in people between the ages of twenty and seventy-four. In addition, people with diabetes are at greater-than-normal risk of developing high blood pressure, heart disease, and stroke, as well as damage to the nervous system, such as impaired sensation or pain in the extremities, skin breakdown, and difficulty with wound healing. The brain is affected as well—the diabetic is more likely to develop dementia than the nondiabetic (Akomolafe, 2006; Pasquier, 2006).
In type 1 diabetes mellitus, the pancreas fails to make insulin, and glucose builds up in the bloodstream, unable to get into cells. Without this basic fuel, the cells cannot continue to function, and when enough cells malfunction, the various organs of the body shut down. Type 1 diabetes can develop rather suddenly, and the person may become acutely ill, even slipping into a coma as the blood sugar rises and the blood becomes acidotic. In this instance, the fat cells begin to release extremely large quantities of fatty acids, which are then converted in the liver to ketones. The ketone levels become extraordinarily high—much higher than the levels proposed by Dr. Richard Veech for use in his ketone ester. This is called diabetic ketoacidosis, and the affected person will die unless insulin is administered.
Type 1 diabetes used to be called “juvenile-onset” diabetes, since most cases start during childhood and adolescence, in fact, about one in 400 children and adolescents have type 1 diabetes. More than 90 percent of cases of diabetes under age ten are type 1. Overall, nearly 3 million people in the United States have type 1 diabetes.
A person afflicted with type 1 diabetes must continue to receive insulin on at least a daily basis, sometimes two or three times daily, in order to survive. Blood sugar levels can vary significantly depending on the foods that are consumed and need to be monitored throughout the day. Blood sugar levels guide the diabetic about how much insulin to use for each injection. Some diabetics are so unstable, or “brittle,” that they must use a pump that injects insulin at programmed intervals under the skin.
It is very important for the diabetic to adhere to a healthy diet and to keep the blood sugar within reasonable limits. The well-controlled diabetic can expect to live a longer and healthier life than the “poorly controlled” diabetic who ignores his or her doctor’s and dietician’s advice.
In type 2 diabetes mellitus, the pancreas is able to make insulin, but may have trouble making enough insulin to handle the amount of glucose in the circulation. In fact, insulin levels may be higher in some people with type 2 diabetes than in someone without the disease. In some cases, certain types of cells do not respond normally to insulin because some of the insulin receptors may be defective or may not be on the surface of the cell membrane where they belong. Other agents may also interfere with insulin receptors. As a result, glucose may not be able to get into the cell in sufficient amounts. This is called insulin resistance. Eventually, when the energy in the cell is depleted, the cell will die.
Type 2 diabetes was formerly known as “adult-onset” diabetes. About one in five people over age sixty-five in the United States have type 2 diabetes, and it is becoming much more common in younger people, representing about one-third of cases in ten- to nineteen-year-olds. Overall, there are about nine people with type 2 diabetes for each person with type 1 diabetes. Obesity that results from an excess of calories, so common in the United States today, is thought to play a major role in the rising rates of type 2 diabetes and related diseases. Modification of diet to reduce overall caloric intake, and paying close attention to the types of carbohydrates consumed, can play a very important role in preventing and controlling the disease.
Diabetics who experience one or more episodes of severe hypoglycemia (low blood sugar) are even more likely to have memory and other cognitive problems as they age. Episodes of low blood sugar happen most often when too much insulin is produced in relation to how much carbohydrate is eaten. This can be a very serious problem, particularly for people with type 1 diabetes who have difficulty controlling their blood sugar. Confusion and other problems related to cognitive functioning are common symptoms of low blood sugar. Consuming medium-chain triglyceride (MCT) oil appears to protect people with diabetes from experiencing these cognitive problems during hypoglycemic spells (Page, 2009). There will be more about this research study in Chapter 18.
The effects of insulin go well beyond simply letting glucose into cells. Insulin also reduces the use of fat as a source of energy, causes lipids to be stored in fat cells, and causes glucose to be stored in the form of glycogen in muscle and liver. Insulin affects the activity of numerous enzymes, causes the walls of arteries to relax, and increases cell growth and survival. These are just a few of the more important effects of insulin.
Until just a few years ago, it was commonly believed that insulin was made only in the pancreas, a gland located just behind the stomach. Then, in 2005, Suzanne M. de la Monte, M.D., Jack R. Wands, M.D., and their associates at Brown University and Rhode Island Hospital reported that insulin and some of the related insulin growth factors are, in fact, made in the brain (De la Monte, 2005).
I am going to repeat this because it is such a profound discovery: the brain can make its own insulin.
The earliest reference I have been able to find suggesting that a dementia such as Alzheimer’s may involve a problem with glucose metabolism is in a 1970 German paper by Siegfried Hoyer, M.D., and others (Hoyer, 1970). The researchers found decreased levels of glucose and a lower cerebral metabolic rate (the speed at which energy is used) in the brains of some people with dementia. Building on further work by Hoyer and many other groups begun in the 1970s and exploding in the 2000s, de la Monte’s group presented more evidence supporting the developing concept that insulin resistance and a deficiency of insulin in the brain are responsible for cognitive impairment and Alzheimer’s disease. They coined a new term, “type 3 diabetes,” to refer to Alzheimer’s disease (Steen, 2005) and published another paper in 2008 with evidence that Alzheimer’s disease is type 3 diabetes. In the summary of this article, they state: “Alzheimer’s disease represents a form of diabetes that selectively involves the brain and has molecular and biochemical features that overlap with both type 1 diabetes mellitus and T2DM [type 2 diabetes mellitus].”
Dr. de la Monte and her associates have learned there is a gradual progression of insulin deficiency and insulin resistance in parts of the brain in people with Alzheimer’s. This means the brain does not make enough insulin and some cells in the brain do not respond normally to insulin. The researchers also found that this process worsens gradually over time. In one of their studies, they looked at the brains of people who died with advanced Alzheimer’s disease. They found that:
• Levels of insulin and factors related to making and using insulin are greatly reduced.
• All the signaling pathways involved in the use of energy are abnormal.
• The functioning of mitochondria is abnormal.
None of the people with advanced Alzheimer’s they studied had either type 1 or type 2 diabetes. Thus, the concept of type 3 diabetes, or diabetes that affects only the brain, was born (Steen, 2005). Researchers have also learned that obesity and type 2 diabetes can increase the risk of developing Alzheimer’s and hasten the progression of Alzheimer’s, but do not appear to cause it. Given that diet can be modified to reduce weight and reverse type 2 diabetes, then changing to a healthier diet could delay or slow the progression of Alzheimer’s disease. The primary goal with such a diet would be to increase the effectiveness of insulin by reducing how much carbohydrate we eat, especially simple sugar. Our bodies need carbohydrate, so eliminating it completely is not realistic or desirable. But most people in this country consume too much, which could spell big problems for us as we age. If we want to avoid dementia and a host of other problems, we need to eliminate as much carbohydrate as possible. (For more on what constitutes a healthy diet, see Chapter 22.)
Dr. de la Monte and her group then looked at the brains of people who died at various stages of Alzheimer’s disease. They found that the loss of insulin and neurons with insulin growth factor receptors begins early in the disease. (Neurons are highly specialized brain cells that are responsible for transmitting information throughout the body.) This worsens with each stage of the disease until it is very severe and occurs throughout the brain in the most severe cases of Alzheimer’s.
In their reports, de la Monte and her group have suggested that some of the treatments for type 1 and 2 diabetes might also help people with type 3 diabetes. For example, insulin administered as a nasal spray can penetrate into the brain. Insulin given this way is showing some promise as a treatment and is currently in clinical trials.
The problem with insulin is not the whole story, as Dr. de la Monte acknowledges in her papers. What causes this defect in insulin production and use in the first place? Inflammation in the brain is a major factor in Alzheimer’s disease. Is the problem with insulin a result of inflammation? And what about the “plaques and tangles” that are seen in the brains of people with Alzheimer’s? Two avenues of research have been exploring these issues. Simply put, some researchers believe that the amyloid plaques cause the destruction of neurons that results in Alzheimer’s disease, and some believe that the tangles cause Alzheimer’s. For example, those in the beta-amyloid camp believe that a treatment that removes beta-amyloid from the brain will stop the worsening of the disease process and may even reverse it. Many groups of researchers throughout the world are working on every aspect of these issues.
After reading everything I can find, I believe we will learn that neither the plaques nor the tangles cause Alzheimer’s disease. I believe these are byproducts of brain cells, specifically neuron cells, are dead and dying as they disintegrate, or that they are a response to the disease process that causes cell destruction and death.
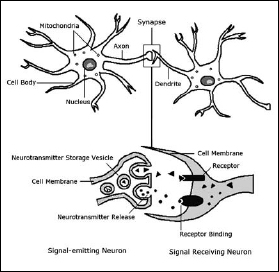
To further explain the tangles of Alzheimer’s, the neuron cell has thin extensions from it that allow it to connect with other cells (Figure 14.1). In general, the shorter dendrites receive signals from other cells and the axons transmit signals to other cells. The axons of one neuron can be very lengthy, up to several feet long. Inside of the body of the neuron and its axons and dendrites is a skeleton made of neatly arranged tubules that support the cell, much like our own skeleton. As the neuron deteriorates and dies, the tubules in this skeleton are chemically changed and become disorganized instead of neatly arranged. Eventually, the tubular structure pulls up out of the axons, wads up, and forms a tangle inside of the cell. Once this begins, it is unlikely anything can be done to bring this cell back to life.
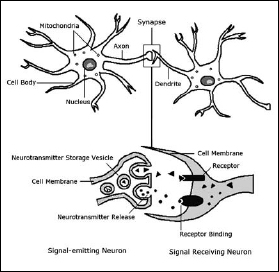
Figure 14.1: Neurons have a membrane that is designed to send information to other cells. The axons and dendrites are unique structures designed to transmit and receive information. The connections between cells are known as synapses. Neurons release chemicals known as neuro transmitters into these synapses to communicate with other neurons. Diagram by Joanna Newport.
I believe that the problem of glucose not getting into the cells is ultimately responsible for the malfunction and death of these cells. If adequate amounts of glucose cannot get into the neuron cell, and there is no other fuel to replace it, the whole chain of events that comes thereafter is affected. Without enough fuel, the mitochondria cannot manufacture enough ATP. Without ATP, the cell cannot make the proteins it usually makes, may make defective proteins, and/or may not have enough energy to release their proteins and enough of the chemicals called neurotransmitters that it needs to communicate with other cells.
I believe that up to a certain point, this process may be reversible. If the cell can get some form of fuel, so that certain substances are replenished, the mitochondria can make more ATP again. Then there may be some recovery and reversal of the process, much like someone whose heart has stopped and is brought back to life by a defibrillator. But without enough ATP, proteins and other chemicals accumulate inside the cell; the cell membrane deteriorates, no longer able to fulfill its purpose of deciding what gets in and what gets out; the proteins leak out and accumulate outside the cell; and the skeleton of the brain cell collapses and begins to wad up, forming the tangle inside the cell.
While the process of how cells function is far more complicated than what I’ve discussed here, it is clear to me that if a cell cannot get enough energy and is in the process of dying, at some point reversal will not be possible. I want to make it clear that the ideas presented in these last two paragraphs are my opinion, rather than proven facts, and they are based on what I have read up to now.