Chapter 1
Diabetes and Nutrition 101
Today is the first day of your journey to good health and well-being with a top-notch diabetes nutrition plan. As you learned in the Introduction, the majority of diabetes care is self-care. Managing your nutrition when you have diabetes involves learning as much as you can about your condition as well as making positive behavior changes related to food. It’s time to get started learning about diabetes and its relationship to food. Welcome to Diabetes and Nutrition 101!
Even if you’ve just been diagnosed with type 2 diabetes, you may be surprised to find that you could have had diabetes for quite some time. This is because type 2 diabetes usually develops gradually, and its symptoms can be so subtle that they may go unnoticed for a while. Looking back, you might realize that you had some of these classic diabetes symptoms even before you were diagnosed:
• Urinating often
• Feeling very thirsty
• Feeling very hungry
• Unusual fatigue
• Blurry vision
• Cuts and bruises that are slow to heal
• Unexplained weight loss
• Tingling, pain, or numbness in your hands or feet
• Dry or itchy skin
• Recurring infections
Many people ignore these symptoms or simply chalk them up to “getting older.” Then they put off visiting their health-care provider because the symptoms don’t seem serious, which further delays the diabetes diagnosis.
If you have already been diagnosed with type 2 diabetes, then you may know that your family could also have an increased risk for the condition. Fortunately, the same healthy eating and physical activity plan that you will be following can give your family members a better chance at delaying or preventing type 2 diabetes if they join you in your journey toward health and well-being.
What Is Type 2 Diabetes? Can It Be Prevented?
Type 2 diabetes is a lifelong condition marked by high levels of glucose (sugar) in the blood. It begins when the body does not respond correctly to insulin, which is a hormone released by the pancreas. Insulin allows glucose to move into cells, so the glucose can be used for energy. If glucose doesn’t get into the cells, then it will build up in the bloodstream, causing the symptoms of diabetes.
Insulin resistance and obesity are usually associated with type 2 diabetes. Insulin resistance means that fat, liver, and muscle cells do not respond normally to insulin, and, as a result, the pancreas produces more and more insulin. But over time it isn’t able to keep up. Eventually, the pancreas cannot produce enough insulin to cover the increased needs, and then blood glucose levels rise. The diagnosis of prediabetes or diabetes is based on the results of blood glucose testing. (More information on prediabetes follows.)
Type 2 diabetes is a progressive condition that develops in a predictable pattern. Over time, the body’s insulin-producing cells gradually lose their ability to function well, and treatments such as oral medications, injectable medications, or both may be needed—in addition to healthy eating, physical activity, and behavior change—to maintain the best blood glucose control.
The good news is that the progressive nature of type 2 diabetes often allows you or your health-care professional to recognize the developing condition in its early stage, known as prediabetes. Making simple lifestyle changes at the point of prediabetes can prevent or delay the development of type 2 diabetes.
Prediabetes: How Diabetes Develops
Prediabetes is the first step in the development of type 2 diabetes. In people with prediabetes, blood glucose levels are above the normal range but below the level at which diabetes is diagnosed. Prediabetes is diagnosed when:
• Fasting blood glucose is between 100 mg/dL and 125 mg/dL
• OR the 2-hour glucose value on an oral glucose tolerance test is between 140 mg/dL and 199 mg/dL
• OR the A1C test is between 5.7% and 6.4%
Many people with prediabetes develop type 2 diabetes within 10 years. There are about 86 million people aged 20 years and older with prediabetes in the U.S. If you have prediabetes, then you will be happy to know that it is a condition that responds well to healthy eating habits, weight loss, and exercise. A very large research study called the Diabetes Prevention Program (which included a nutrition counseling component) found that modest weight loss (about 7% of your body weight) and physical activity (at least 30 minutes a day of moderate-intensity activity, five days a week) reduced the chances of prediabetes developing into diabetes by 58%. Lifestyle changes provided even better results than treating prediabetes with medication! Although some health-care professionals may recommend a medication to prevent type 2 diabetes, lifestyle changes are always the foundation of diabetes prevention.
A key point to remember is that preventing or delaying type 2 diabetes requires only fairly small changes in lifestyle. Notice that success doesn’t mean starving yourself to reach an “ideal body weight” or running endless laps. A 7% weight loss translates to losing 14 pounds for someone who weighs 200 pounds. Moderate-intensity physical activity equates to taking a brisk walk for about 30 minutes each day, five days a week.
These goals are small steps toward the bigger reward of good health. As you take these small steps and experience small successes, you will develop more confidence in yourself and your ability to make the changes you need to stay healthy.
What Is Moderate-Intensity Physical Activity?
Your heart rate is the number of times your heart beats per minute. Moderate-intensity physical activity causes your heart to beat at 50–70% of your maximum heart rate. According to the American Heart Association, your maximum heart rate is about 220 minus your age. If you’re 60 years old, your maximum heart rate is about 160 beats per minute; 50–70% of your maximum heart rate is about 80–112 beats per minute. Examples of moderate-intensity physical activity include:
• Walking 2 miles in 30 minutes
• Cycling 4 miles in 15 minutes
• Water aerobics for 30 minutes
• Stair walking for 15 minutes
• Gardening for 30–45 minutes
• Raking leaves for 30 minutes
What to Do If You Have Type 2 Diabetes
Type 2 diabetes is a progressive disease. This means that despite your best efforts at lifestyle changes, over time prediabetes can progress to type 2 diabetes, or type 2 diabetes may begin to require treatment with oral medications or injectable medications in addition to healthy eating and physical activity. This doesn’t mean you have “bad” diabetes or only had a “mild” case in the beginning. Don’t blame yourself if you feel that you didn’t take the best possible care of your condition. Would you blame yourself if you needed stronger glasses because your eyesight changed? Because of the progressive nature of diabetes, self-management education with your diabetes team can be customized to provide you with support no matter where you are in your life with diabetes.
When diagnosed with type 2 diabetes, you are at increased risk for many serious complications. Some complications of poorly controlled type 2 diabetes are:
• Heart disease (cardiovascular disease)
• Blindness (retinopathy)
• Nerve damage (neuropathy)
• Kidney damage (nephropathy)
High blood glucose, high blood pressure, and high blood lipids (total cholesterol, LDL cholesterol, and triglycerides) are contributing factors to diabetes complications.
Complications are not always a consequence of high blood glucose. Studies show that the risk for cardiovascular complications is indeed associated with diabetes but is favorably modified by the control of high blood pressure and the treatment of high blood lipids more clearly than by glycemic control. However, glucose control has been shown to have an impact on retinopathy, nephropathy, and neuropathy.
Better health care for those with diabetes has led to the good news that rates of certain diabetes-related complications (heart attacks, ketoacidosis, coma, stroke, amputations, and end-stage kidney disease) have dropped in the past 20 years. The American Diabetes Association has made recommendations for diabetes control based on important clinical research, but remember that these goals need to be personalized for you based on your age, how long you’ve had diabetes, and your other health conditions (if any).
It’s vitally important that you and your diabetes health-care team discuss your personal goals for blood glucose, blood pressure, and blood lipids. Your goals for diabetes control may differ from American Diabetes Association recommendations based on your own individual situation.
Managing Type 2 Diabetes
You won’t learn everything you need to know about managing type 2 diabetes just by reading this book or going to one appointment with your diabetes educator. Learning about successful diabetes management is a lifelong process with several areas to master. The American Association of Diabetes Educators (AADE) has developed a list of seven self-care behaviors (see Table 1.1) that you can use to focus your diabetes management. Working with your diabetes educator or diabetes health-care team, you can use these behaviors as a checklist to be certain you’ve learned about every important area of diabetes self-management.
You can also learn more about managing all aspects of your diabetes by going to the American Diabetes Association’s website (at www.diabetes.org) or by reading a good diabetes book, such as Real-Life Guide to Diabetes, American Diabetes Association Complete Guide to Diabetes, or Your First Year with Diabetes, Second Edition (all available at www.shopdiabetes.org).
Nutrition: A Special Focus in Type 2 Diabetes
Nutrition has long been recognized as the cornerstone for successful diabetes management. Even as far back as 1550 B.C., doctors recommended that people with diabetes follow a diet of wheat grain, fresh grits, grapes, honey berries, and sweet beer to replace the sugar lost through the urine! Today, good nutrition for type 2 diabetes is based on the following nutrition goals and the nutrition recommendations (see Table 1.2) from the American Diabetes Association.
American Diabetes Association Nutrition Goals
• Attain individualized blood glucose, blood pressure, and lipid goals. General recommended goals from the American Diabetes Association are as follows:
+ A1C <7%
+ Blood pressure <140/90 mmHg
+ Blood lipids:
^ LDL cholesterol <100 mg/dL
^ Triglycerides <150 mg/dL
^ HDL cholesterol >40 mg/dL for men
^ HDL cholesterol >50 mg/dL for women
• Achieve and maintain body weight goals.
• Delay or prevent complications of diabetes.
• Address individual nutrition needs.
• Maintain the pleasure of eating.
• Learn about practical tools for day-to-day meal planning rather than focusing on individual nutrients or single foods.
Weighty Issues
The vast majority of individuals with type 2 diabetes are overweight and have insulin resistance. They also often have high blood pressure and high blood lipids. Weight loss is an important part of therapy for improving all aspects of type 2 diabetes. Just as in the treatment of prediabetes, small changes can yield big results.
If your weight is a concern, you can start managing it by determining your weight status. A measurement known as the body mass index (BMI) takes into account your height and weight, making it a reliable indicator of body fat. You can find your BMI by using:
• An online BMI calculator. You can find an excellent BMI calculator at the website for the National Heart, Lung, and Blood Institute (www.nhlbi.nih.gov/guidelines/obesity/BMI/bmicalc.htm).
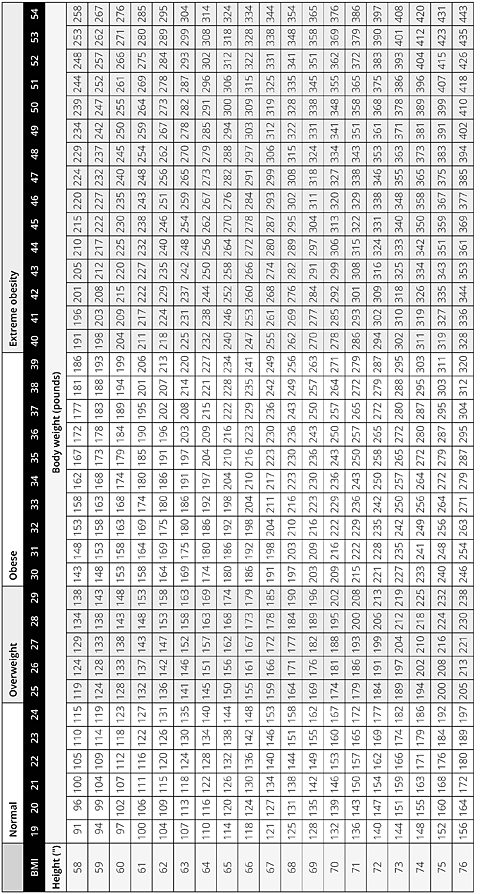
• An adult BMI chart (see Table 1.3). Locate your height in the left column and read across the row for that height to find your weight. Follow the column of the weight up to the top row that lists your BMI.
• Calculate it yourself. Multiply your weight in pounds by 703 and then divide by your height in inches squared. The formula looks like this:
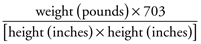
For example, if you’re 5′5″ (65 inches) tall and weigh 180 pounds, here’s how you’d calculate your BMI:
Use your BMI to pinpoint your weight status and potential health concerns.
As body fat or BMI increases, health risks increase. Being overweight (BMI of 25–29.9) or being obese (BMI ≥30) increases the risk of having high blood pressure, heart disease, stroke, diabetes, certain types of cancer, arthritis, and breathing problems. Research shows that being obese lowers your life expectancy.
Which Meal Plan Is Best for Diabetes and Weight Loss?
There are many, many approaches to losing weight. In fact, if you do a Google search of “how to lose weight,” over 100 million entries appear! Which weight-loss approach is best for people with diabetes? Certainly, losing those extra pounds is an important first step to managing type 2 diabetes, and the best approach to use for weight loss is the one that enables you to keep the weight off forever.
Diabetes nutrition recommendations are now focusing more on healthful eating patterns (combinations of different nutrient-dense foods and food groups including starch, fruits, milk and milk substitutes, nonstarchy vegetables, protein, fats, sweets/desserts, and other carbohydrates) than on single nutrients such as carbohydrate, fat, or sodium. A variety of eating patterns are acceptable for the management of diabetes, and your personal preferences and diabetes goals are important considerations when choosing an eating pattern to follow. Table 1.4 describes some of the most common eating patterns and provides a few sample food ideas.
While more research is needed, each of these eating patterns has shown varying levels of success in improving glucose control and cardiovascular risk factors and helping with weight loss—particularly if calories, carbohydrate, and portion sizes are monitored. Work with your nutrition professional to determine which eating pattern is the best for you based on your personal preferences and diabetes goals.
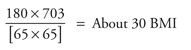
Create Your Plate
Another helpful meal planning tool for those recently diagnosed with diabetes is called “Create Your Plate.” This tool is an easy way for people with diabetes to control portion sizes and limit their intake of starchy foods.
Follow these seven easy steps to Create Your Plate:
1. Using your dinner plate, put a line down the middle of the plate. Then on one side, cut it again so you will have three sections on your plate.
2. Fill the largest section with colorful nonstarchy vegetables such as:
+ Spinach, carrots, lettuce, greens, cabbage, bok choy
+ Green beans, broccoli, cauliflower, tomatoes
+ Vegetable juice, salsa, onion, cucumber, beets, okra
+ Mushrooms, peppers, turnips
3. Now in one of the small sections, put grains and starchy foods such as:
+ Whole-grain breads, such as whole wheat or rye
+ Whole-grain, high-fiber cereal
+ Cooked cereal such as oatmeal, grits, hominy, or cream of wheat
+ Rice, pasta, dal, tortillas
+ Cooked starchy beans and peas, such as pinto beans or black-eyed peas
+ Potatoes, green peas, corn, lima beans, sweet potatoes, winter squash
+ Low-fat crackers, snack chips, pretzels, and light popcorn
4. And then in the other small section, put your protein-rich foods such as:
+ Chicken or turkey without the skin
+ Fish such as tuna, salmon, cod, or catfish
+ Other seafood such as shrimp, clams, oysters, crab, or mussels
+ Lean cuts of beef and pork such as sirloin or pork loin
+ Tofu, eggs, low-fat cheese
5. Add a serving of fruit, a serving of dairy, or both as your meal plan allows.
6. Choose healthy fats in small amounts. For cooking, use oils. For salads, some healthy additions are nuts, seeds, avocado, and vinaigrettes.
7. To complete your meal, add a low-calorie drink like water, unsweetened tea, or coffee.
Lifestyle Changes That Work for Weight Loss!
No matter which eating pattern or weight-loss options you choose, lifestyle changes based on healthy eating, physical activity, and behavior change are the foundation of any successful weight-loss program. Here are a few examples of lifestyle changes you can make to promote weight loss:
Other Options?
In addition to healthy eating, physical activity, and behavior change, other options for weight loss include:
• Weight-loss medications, which can help you achieve a loss of 5–10% of weight when combined with lifestyle changes. Some of these medications have unpleasant side effects, and, of course, they only work when you take them. Medications are generally only recommended for those with a BMI >27 (other weight-related factors may be taken into consideration in addition to BMI).
• Bariatric surgery may be a consideration if your BMI is >35 and your diabetes or associated comorbidites are difficult to control with lifestyle changes and medication. Although bariatric surgery has been shown to lead to near or complete normalization of blood glucose in about 40–95% of patients with type 2 diabetes, it is a costly and potentially risky approach to weight loss. It’s not regarded as a “cure” for type 2 diabetes, so those who have had a bariatric procedure need lifelong lifestyle support and medical monitoring, including regular screenings of their blood glucose.
Putting It All Together
Many people with diabetes aren’t able to see a registered dietitian/registered dietitian nutritionist or certified diabetes educator immediately after being diagnosed with diabetes. But if that’s your situation, you can still get started on the path to balanced eating and learn more about the basics of good nutrition before you attend your first appointment with a nutrition professional.
Take advantage of a great online nutrition resource from the American Diabetes Association—the “Food & Fitness” page on the Association’s website (available at www.diabetes.org/food-and-fitness). The American Diabetes Association site is brimming with food tips, meal planning tools, shopping lists, and recipes, as well as a guide to healthy eating and physical activity that can lead to better blood glucose control. Another important feature included on the site is “Create Your Plate.”
The United States Department of Agriculture (USDA) also has a wealth of no-cost information about healthy eating for the general public as well as meal plans for weight loss on the Choose My Plate website (available at www.choosemyplate.gov). While not diabetes-specific, this online resource includes a step-by-step approach to weight management, which includes tips on determining your current eating habits, an online SuperTracker, guidance on what to eat and drink along with personalized Daily Food Plans, and tips for making better food choices while at home or eating out. Check out the “Weight and Calories” page of the website to access these features.
It Starts with a Single Step
Small steps lead to big achievements. Whether your nutrition goal is to lose weight or lower your blood glucose, it won’t happen on its own. First, think about each action you need to take to achieve your goal; then, divide it into small steps that are easy to achieve. After you complete several small steps, you will have achieved your overall goal. For example, if your goal is to eat less fast food and cook more meals at home, you should:
• Set aside time to make healthful eating a priority.
• Plan menus and choose recipes.
• Shop so you have the ingredients in your kitchen to prepare healthy recipes.
• Rediscover the lost art of cooking to minimize the use of prepackaged foods.
It’s been said that whoever wants to reach a distant goal must take small steps. Let’s move forward and take the next steps!
Next Steps
Review the nutrition goals you set in the Introduction. Choose your highest-priority nutrition goal and list three changes you can make today to help you move toward accomplishing that goal.
My highest-priority nutrition goal is:
__________________________________________________________________________
__________________________________________________________________________
__________________________________________________________________________
The three steps I will take TODAY to reach that goal are:
1. ________________________________________________________________________________
2. ________________________________________________________________________________
3. ________________________________________________________________________________
What Do I Eat for Dinner?
For 45–60 Grams of Carbohydrate*
Recipe: Salmon and Asparagus Foil Packet (1 serving)
1/2 cup wild rice
3/4 cup citrus fruit salad (white/red grapefruit and orange sections)
For 60–75 Grams of Carbohydrate*
Recipe: Salmon and Asparagus Foil Packet (1 serving)
1/2 cup wild rice
1 slice sourdough bread
3/4 cup citrus fruit salad (white/red grapefruit and orange sections)
*For most women, 45–60 grams of carbohydrate at a meal is a good starting point; for most men, 60–75 grams of carbohydrate per meal is appropriate. Check with your diabetes health-care team to find the amount of carbohydrate that’s right for you.
Swift, Simple Tips
• You can buy sourdough bread (in rolls or loaves of various shapes and sizes) in the bakery or health food section of most grocery stores. It’s traditionally a white bread, but whole-wheat and rye versions are available. Choose the whole-grain variety whenever possible.
• No time to prepare a citrus fruit salad? Check out your grocer’s produce section for chilled, ready-to-serve mixtures of white/red grapefruit and orange sections.
Salmon and Asparagus Foil Packets
Serves: 4 / Serving size: 1 packet
Preparation time: 20–25 minutes / Cooking time: 15–18 minutes
1 pound fresh asparagus
4 sheets 12 × 18-inch heavy-duty foil wrap
Nonstick cooking spray
4 (5-ounce) fillets skinless salmon
2 tablespoons low-sodium soy sauce
2 teaspoons freshly squeezed lemon juice
2 tablespoons packed light brown sugar
1 tablespoon honey
1 teaspoon bottled minced fresh garlic
1 teaspoon sesame seeds
1. Preheat oven to 450°F.
2. Break ends off asparagus spears and divide spears into four portions.
3. Spray center of each foil sheet with nonstick cooking spray. Place one salmon fillet in the middle of each sheet of foil along with 1/4 of the asparagus.
4. Combine low-sodium soy sauce, lemon juice, brown sugar, honey, and garlic in a small bowl. Drizzle 1/4 of mixture on top of salmon and asparagus in each foil packet. Sprinkle 1/4 teaspoon of sesame seeds on top of salmon and asparagus in each packet.
5. Bring up sides of foil and fold the top over twice. Seal the ends, leaving room for air to circulate inside the packet. Place packets on a cookie sheet and bake for 15–18 minutes, until salmon is opaque. Be careful opening packets; moisture creates steam during cooking, which can burn your hand if you quickly tear open the foil.
Choices/Exchanges
1 Carbohydrate, 5 Lean Protein
Calories 280
Calories from Fat 80
Total Fat 9.0g
Saturated Fat 1.9g
Trans Fat 0.0g
Cholesterol 65mg
Sodium 350mg
Potassium 700mg
Total Carbohydrate 15g
Dietary Fiber 2g
Sugars 12g
Protein 33g
Phosphorus 385mg
Food for Thought
• Type 2 diabetes is a progressive condition. Healthy eating, physical activity, and behavior changes are the foundation for diabetes treatment, but new therapies and medications may need to be added to your diabetes-care plan over time.
• Type 2 diabetes responds well to weight loss, healthy eating, and physical activity.
• The healthy eating guidelines for people with type 2 diabetes are the same as those for everyone in your family:
+ Eat high-fiber grains, beans, fruits, and vegetables.
+ Consume small portions of meat and protein foods.
+ Limit your intake of fats, refined starches, sweets, and alcohol.