CHAPTER 9: H IS FOR HEAD TRAUMA: THE SILENT EPIDEMIC THAT UNDERLIES MANY MENTAL ILLNESSES
After at least five concussions, SPECT and hyperbaric oxygen therapy helped my brain get back to normal.
HALL-OF-FAME NFL QUARTERBACK JOE NAMATH[304]

GARY
On December 4, 1988, Gary Busey was involved in a near-fatal motorcycle accident, striking his head on a curb. The Academy Award-nominated actor, who had been appearing on screen since 1971, was not wearing a helmet and suffered massive head injuries. Surgeons opened up his scalp, drilled holes through his skull, and scraped the temporal side of his brain. The brain surgery was deemed a success, the scars on his scalp sealed over, and he underwent occupational and speech therapy. Gary thought he was healed, but for 30 years, the traumatic brain injury (TBI) inside his skull went untreated. After the accident, the rising star tumbled into freefall. He suffered explosive outbursts (many of them caught on camera in reality TV shows), was arrested on battery charges, overdosed on cocaine, and went to rehab.
In 2008, he met his future wife, Steffanie Sampson. At first, she found him charismatic. “Sometimes he’s ultimately charming and appears caring,” she said “and then sometimes he’s just in your face like a bull in a china shop. It’s weird.” Over the years, she became so worn out she felt like she couldn’t put up with his erratic behavior anymore and threatened to leave if he didn’t do something about it. In order to save his relationship, Gary agreed to get help, and that’s when he came to see me. When we scanned his brain, it showed very low activity in parts of the prefrontal cortex (PFC) and temporal lobes —areas involved in judgment, forethought, empathy, impulse control, and anger management. When Gary and Steffanie saw the scans, they were stunned. Gary had thought he had fully recovered from the accident.
In taking Gary’s history, we learned that the motorcycle accident was only one of many things affecting his brain. He likely had attention deficit hyperactivity disorder (ADHD) as a child; he played tackle football in high school and college; he smoked cigars; he abused cocaine and smoked marijuana; and when he had cancer of the sinuses, he had radiation that affected the brain. All of this chipped away at his brain reserve, leading to a breaking point.
Now we’re fixing Gary’s brain (see the chart below). In the first few months of treatment with our BRIGHT MINDS program, he has cut out marijuana, cigars, and sodas. He has increased his water intake; he is eating healthy, organic, nutrient-dense foods; he’s having hyperbaric oxygen therapy (HBOT) treatments and is taking supplements. He’s even lost weight. I’m excited to see how much more of a change it will make in Gary’s life. I know you are not stuck with the brain you have. You can make it better, and Gary and I are proving it.
BRIGHT MINDS |
GARY’S RISK FACTORS |
INTERVENTIONS |
Blood Flow |
Low blood flow on SPECT |
Exercise, BRIGHT MINDS diet, omega-3 EPA and DHA, ginkgo |
Retirement/Aging |
Age 75 |
New learning |
Inflammation |
High CRP, low Omega-3 Index |
BRIGHT MINDS diet |
Genetics |
||
Head Trauma |
Motorcycle accident, playing tackle football |
HBOT, neurofeedback, nutraceuticals |
Toxins |
Drug use, cigar smoking |
Stop using drugs, stop smoking |
Mind Storms |
Temper flares |
Stress management tools |
Immunity/Infections |
Low vitamin D level |
Vitamin D |
Neurohormone Issues |
Low testosterone |
Testosterone replacement |
Diabesity |
High blood-sugar levels |
Eliminate sugar and sodas, BRIGHT MINDS diet, exercise, targeted nutraceuticals |
Sleep |
Insomnia |
Sleep strategies |
Gary’s SPECT Scan Before
GARY’S SPECT SCAN BEFORE
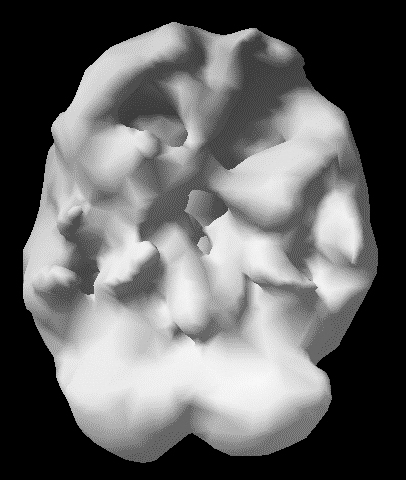
Overall low activity, especially to frontal and temporal lobes
As you have seen throughout this book, your brain is at the heart of what makes you who you are. When it works right, you work right; and when it is troubled for whatever reason, you are much more likely to have trouble in your life. Many people think the brain is rubbery and fixed within the skull, but it isn’t. As I’ve taught for decades, your brain is soft, about the consistency of soft butter, tofu, or custard —somewhere between egg whites and gelatin. It floats in cerebrospinal fluid and is housed in a very hard skull that has many sharp bony ridges (see next page). As such, it is easily damaged.
In this chapter, we are focusing on physical trauma to the brain (biological circle). Whiplash, jarring motions (think shaken baby syndrome), blast injuries, and blows to the head can cause the brain to slosh around, slamming into the hard ridges inside the skull. Here is what happens in the brain after physical trauma:
- Bruising
- Broken blood vessels and bleeding
- Increased pressure
- Lack of oxygen
- Damage to nerve cell connections
- Ripping open of brain cells that spill out proteins like “tau” that cause inflammatory reactions
On top of that, your pituitary gland (which regulates your hormones) sits in a vulnerable part of your skull, so it is often hurt in head injuries, causing major hormonal imbalances.
A Look inside the Skull
A LOOK INSIDE THE SKULL
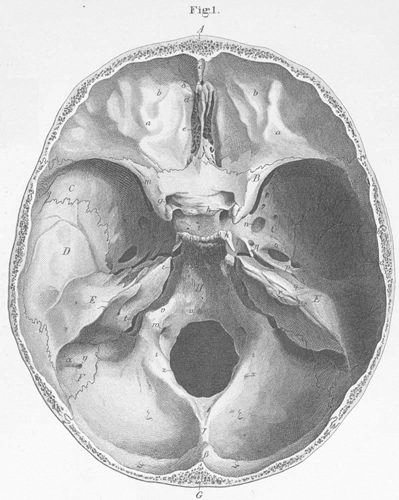
Looking down from the top, you can see the protective bony ridges, which can damage your soft brain in an accident or injury.
According to the CDC,[305] more than 2 million new head injuries occur in the United States every year. That means over the last 40 years, more than 80 million people have sustained head injuries. And the number of concussions is also rising, especially among children. From 2010 to 2015, concussion diagnoses jumped 43 percent among the general population. For young people from 10 to 19 years of age, however, concussion diagnoses skyrocketed 71 percent.[306] We have to do a much better job of preventing TBIs as well as repairing the brain whenever they occur.
Common causes of head injuries include:
- Falls —falling out of bed, slipping in the bath or shower, falling down steps, or falling off ladders
- Motor vehicle–related collisions —involving cars, motorcycles, or bicycles; also, accidents where pedestrians are involved.
- Violence —caused by gunshot wounds, assaults, domestic violence, or child abuse
- Sports injuries —besides football, they are common in soccer, boxing, baseball, lacrosse, skateboarding, hockey, cycling, basketball, and other high-impact or extreme sports
- Explosive blasts and other combat injuries[307]
At Amen Clinics, we see patients with head injuries from all of these causes. In particular, we have been studying the association between football and brain injuries for several years. When I first started looking at scans, I saw Pop Warner and high school players between the ages of 8 and 18 with clear evidence of TBIs. I was horrified. And then I saw college players whose brains showed even more damage. In the past decade, I’ve met with many active and former NFL players whose scans were even worse. I was heartened when President Barack Obama and LeBron James both said they would not let their children play tackle football. I took it as a sign that this principle is beginning to become part of our cultural fabric. However, this message isn’t hitting the population equally. A 2019 article in the Atlantic reported that white boys in upper-income communities are ditching football for other sports while black boys in lower-income neighborhoods are still flocking to football. In a study of 50,000 students from 8th grade to 12th grade, 44 percent of black boys reported playing tackle football compared with 29 percent of white boys.[308] We need to do a better job of getting the message out to all parents and young people that tackle football and other contact sports can have devastating lasting effects on their lives.
Tackle football and other contact sports can have devastating lasting effects on your life.
Since 2000, more than 350,000 military veterans have had TBIs.[309] Those injuries mean the Iraq and Afghanistan wars will likely have consequences for the next 70 years because these veterans will have an increased risk for brain health/mental health issues. And as you have seen, the impact of those TBIs will spread beyond the veterans themselves and affect their children and the generations after that. To put an end to this, they need our BRIGHT MINDS approach more than ever and to stand against the cultural norms that dismiss head trauma as a serious issue.
HEAD TRAUMA
THE EVIL RULER WOULD . . .
- 1. Allow children to hit soccer balls with their heads; play tackle football; ski or ride bicycles without helmets; ride large horses; play hockey; and engage in other high-risk behaviors.
- 2. Encourage players on a team (especially the better ones) to go back into the game as quickly as possible after suffering a concussion.
- 3. Put fluorescent lights in all classrooms and workspaces to increase symptoms of anxiety, irritability, depression, or decreased concentration related to Irlen syndrome.
THE BENEVOLENT RULER WOULD . . .
- 1. Encourage the population to love their brains and the brains of their children and protect them at all costs.
- 2. Ban children and teenagers from hitting soccer balls with their head or engaging in high-risk activities. Children and teens cannot give informed consent admitting they know and accept the risks of head injuries. Often parents approve of behaviors where they are unaware of the risks.
- 3. Consider delaying teens getting their driver’s licenses by a year to help cut down on motor vehicle accidents and head injuries.
HEAD INJURY AND MENTAL ILLNESS
Research shows that head injuries increase the risk of:
- Depression[310]
- Anxiety and panic disorders[311]
- Psychosis[312]
- Post-traumatic stress disorder (PTSD)[313]
- Suicide[314]
- Drug and alcohol abuse[315]
- ADD/ADHD[316]
- Learning problems[317]
- Borderline and antisocial personality disorders[318]
- Dementia[319]
- Aggression[320]
- Homelessness[321]
- Victimization[322]
- Loss of or changes in sense of smell or taste[323]
Head trauma may also increase the risk of incarceration.[324] In the United States, 25 to 87 percent of inmates say they have suffered a TBI compared with 10 to 38 percent of the general population.[325] And the latest statistics from the Bureau of Justice Statistics show that 181,500 veterans are incarcerated.[326]
In our database of tens of thousands of patients, 40 percent had a significant brain injury before they came to see us. When people ask me what the single most important lesson I’ve learned from looking at more than 170,000 brain scans is, I reply, “Mild traumatic brain injury is a major cause of psychiatric problems, and very few people know it.”
I hate the terms mild traumatic brain injury and mild concussions because they imply these injuries don’t cause lasting damage, which is often not the case at all. Anyone who has played a contact sport likely has experienced many subconcussive blows, which jostled the brain but did not cause immediate symptoms. The famous boxer Joe Louis (1914–1981) is quoted as saying, “It’s not the big hits that cause dementia, but rather it is the thousands of little hits.”
Head trauma is a major cause of psychiatric illness, and very few people know it because most mental health professionals never look at the brains of their patients, nor do they check the hormones of the brain.
It is important to note that many people forget they’ve had a significant head injury in the past. At Amen Clinics, we routinely ask patients several times whether they have had a head injury. Our intake paperwork asks the question “Have you ever had a head injury?” The historian, who gathers patients’ histories before they see the physician, asks them again about head injuries. The computer testing we have patients complete asks a third time about head injuries. If I see no, no, no as answers, I ask again. If I get a fourth no, I will then say, “Are you sure? Have you ever fallen out of a tree, fallen off a fence, or dived into a shallow pool? Did you play contact sports? Have you ever been in a car accident?”
I’m constantly amazed at how many people think their head injuries were too insignificant to mention. For others, they simply do not remember the incident because amnesia is a common occurrence in head traumas. When asked the question for the fifth time, one patient put his hand on his forehead and said, “Oh, yeah! When I was five years old, I fell out of a second-story window.” Likewise, I have had other patients forget they went through windshields, fell out of moving vehicles, or were knocked unconscious when they fell off their bicycles.
Consider YouTube superstar Logan Paul. The controversial internet personality, who is known for his wild, risk-taking pranks and dangerous stunts, has gained more than 15 million followers. But he has also amassed some harsh critics and was named one of the most hated celebrities of 2018. Some people demanded he be banned from YouTube after he posted an insensitive video of a corpse hanging in a Japanese forest where people go to die by suicide. Logan came to see me to find out why he makes so many bad decisions, why he lacks empathy, and why he is incapable of maintaining a committed relationship. “I want to figure out why I think and act the way I do,” he said in a video about his visit to Amen Clinics. “I’m a bit of a hooligan, a troublemaker.”
As I do with all our patients, I asked him if he had ever experienced head trauma. He told me about a trampoline accident that had fractured his skull when he was in seventh grade. I asked him if there was any other trauma, and he said no. But a few hours later, he revealed something else. Logan shared that he had also been a linebacker and running back on his high school football team. “I was always getting hit in the head,” he admitted. He didn’t think of that as “trauma,” though.
Logan’s brain SPECT scan showed low blood flow and abnormal activity in key areas of his PFC. His history of repetitive head trauma from football combined with the trampoline accident was the main reason behind his bad decisions, lack of empathy, and trouble with relationships.
One of the saddest professional encounters I had was with a mother after I wrote a column on head trauma in the Daily Republic, the local newspaper where I lived in Northern California during the 1990s. A week or so after it appeared, a mother came to see me. She told me that her 20-year-old daughter had killed herself several months earlier, and she was grief stricken over the unbelievable turn of events in her life. “She was the most ideal child a mother could have,” she said. “She did great in school. She was polite, cooperative, and a joy to have around. Then it all changed. Two years ago, she had a bicycle accident. She accidentally hit a branch in the street and was flipped over the handlebars, landing on the left side of her face. She was unconscious when an onlooker got to her, but shortly thereafter she came to. Nothing was the same after that. She was moody, angry, easily set off. She started to complain of ‘bad thoughts’ in her head. I took her to see a therapist, but it didn’t seem to help. One evening, I heard a loud noise out front. She had shot and killed herself on our front lawn.”
Head Trauma Risk Factors
(and the Four Circles They Represent)
PRESCRIPTIONS FOR REDUCING YOUR HEAD TRAUMA RISK FACTORS
(AND THE FOUR CIRCLES THEY REPRESENT)
The Strategies
BRIGHT MINDS: HEAD TRAUMA
STEPS TO CREATE MENTAL ILLNESS . . . AND MAKE MY NIECES, ALIZÉ AND AMELIE, SUFFER
- 1. Deny that brain injuries are likely to cause mental health issues.
- 2. Engage in habits that increase your risk for head trauma.
- Play contact sports.
- Never wear a helmet while skiing, biking, riding a motorcycle, etc.
- Play soccer and head soccer balls repeatedly.
- Participate in high-risk adventure activities —free climbing, bungee jumping, etc.
- Climb trees and ladders and go on the roof.
- Dive into the ocean or pool without knowing the depth of the water.
- Don’t wear a seat belt.
- Drive too fast and text while driving.
- Text while walking.
- Don’t practice balance exercises as you age.
- 3. Avoid the strategies that protect your brain.
STEPS TO END MENTAL ILLNESS . . . AND KEEP MY NIECES, ALIZÉ AND AMELIE, HEALTHY
- 1. Acknowledge that brain injuries could be causing mental health issues and actively repair past head trauma.
- 2. Avoid anything that increases your risk for head trauma.
- 3. Engage regularly in healthy habits that protect your brain.
- Avoid contact sports.
- Avoid high-risk activities.
- Don’t climb trees or ladders or go on the roof.
- Don’t dive headfirst into any body of water.
- Always wear a seat belt in the car.
- Always wear a helmet when skiing or riding a bike.
- Don’t text while driving or walking.
- Consider neurofeedback, HBOT, and nutraceuticals.
- Practice balance exercises, especially as you age.
Pick One BRIGHT MINDS Head Trauma Tiny Habit to Start Today
- When I get in the car, I will fasten my seat belt.
- When I go into the house, I will limit the number of packages I carry at one time to minimize the risk of falling.
- When I go skiing or biking, I will put on a helmet.
- When I must go up on the roof, I will make sure it is absolutely safe.
- When I walk or drive, I will slow down and pay attention to my surroundings.
- When I walk or drive, I will put my phone out of sight so I cannot text.
- When I go downstairs, I will hold the handrail.
- When (and if) I experience a head trauma, I will check my hormones and optimize any that are low.



