
How I Became a Dizzy Cook
I can only imagine what you’re thinking right now. Did I really just buy a migraine cookbook from some woman who is neither a neurologist nor a registered dietician? Yes, you did! And thank you for taking a chance on me. While I may not have a medical background, I am a chronic migraine patient and I like good food. I understand what it feels like to put every ounce of energy one has left into cooking a meal while dealing with a migraine attack. I know that the last thing you want is for that meal to be a disappointment and not leave you with a sense of accomplishment and pride for the effort you put into it. In addition, I know from experience—and loads of research—that good food can help you feel better and have fewer migraine attacks.
Let me start by telling you about my journey with migraine. A few years ago, I was a normal thirty-year-old, doing thirty-year-old things. I was working hard to get promoted at my corporate job in wristwatch development. Newly married, I had just bought my first house with my husband and we were headed off on a two-week trip to Japan, Thailand, and Hong Kong. When we returned from our trip, I dove back into work immediately. At the time, my company had trimmed down my team on the development side to just me. As a result, I was constantly overwhelmed and stressed. Between the stress and not sleeping well, I started to feel sick, but I figured it was the jet lag, and I powered through.
That next weekend we flew to a wedding in Arizona and my ears were in terrible pain during the flight. I started to feel a cold coming on and I became dizzy, but I attributed it to cold symptoms. Once my cold symptoms cleared up, I started to feel better, but the slight dizziness persisted. Over the next month, my dizziness, which I describe as a lightheaded or “floaty” feeling, progressively got worse. My primary care doctor told me it was just stress and I needed to chill out, but I knew in my heart that this was more than just stress. At one point I was driving my coworkers to lunch and I slammed on my brakes, but the car had already been put into park. I felt as if the car was moving forward when it was perfectly still.
Not wasting more time with my primary care physician, I made an appointment with a highly rated ear, nose, and throat doctor (ENT). He ran a few tests to check my hearing and make sure I didn’t have Benign Paroxysmal Positional Vertigo (BPPV), a common cause of vertigo and dizziness that occurs where calcium crystals get loose in your inner ear. Because I wasn’t helped by the Epley or Dix-Hallpike Maneuvers, common techniques that help BPPV sufferers, my ENT decided that I might have Vestibular Neuritis and sent me to a dizziness center for further testing. The dizziness center ran an ENG and VNG, both designed to test balance and detect weakness in the inner ear. They found a slight weakness in my left ear, indicating Vestibular Neuritis. I was given a high dose of steroids and I faithfully attended vestibular therapy four times a week. I suddenly felt a little glimmer of hope. My balance tests were improving, and I appeared to be making progress. Then it all came crashing down. My steroid taper ended, and I was even more dizzy and disorientated than when I first began treatment. At this point, I could no longer drive safely, and looking at a computer for work made me run to the bathroom.
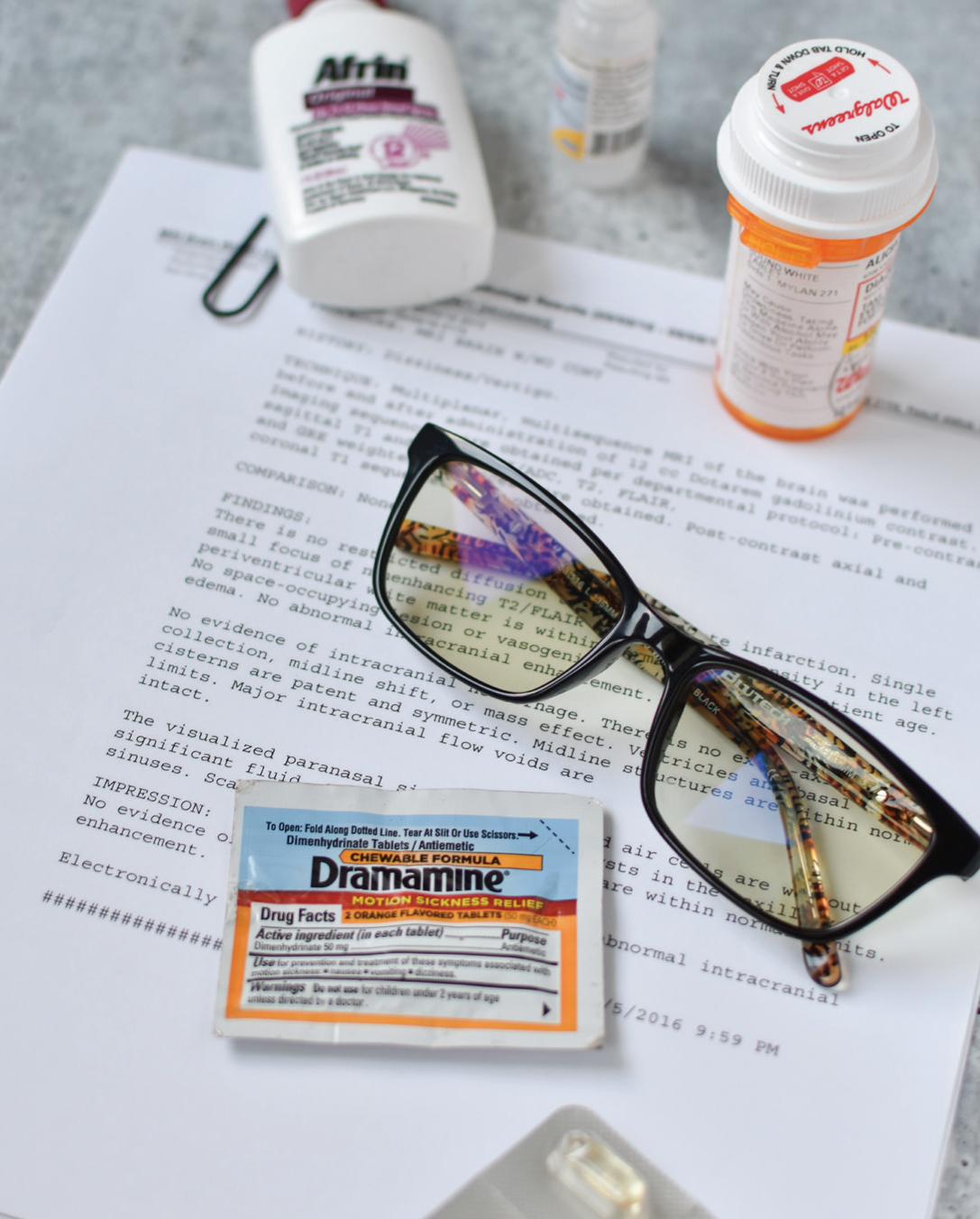
One night, my symptoms got so bad, I was convinced I had a brain tumor. My husband and I were having dinner, and everything began to spin around me. I couldn’t keep my head up. He rushed me to the ER, where they sent me for an MRI. The results all came back normal, so my diagnosis was “vertigo” and they sent me home with meclizine, an anti-nausea medication. Here’s one thing I wish more doctors knew: vertigo is a symptom and not a diagnosis.
Back at the dizziness center, they suspected I had a perilymph fistula, essentially a small tear in the inner ear. They suggested an experimental surgery that would render me deaf in that ear. Again, I felt in my heart this couldn’t be the answer. In my last attempt to get answers, I went back to the ENT who told me there was nothing else he could do. I also saw another neurologist who insisted I was just stressed and needed to relax—that all of this was in my head and anxiety related. Other highly recommended doctors in Dallas even turned me down as a patient after they received my lengthy paperwork.
Without a diagnosis, my employer questioned my absence. I could barely leave my bed, but it was nearly impossible to get a doctor to sign off on my Family Medical Leave Act (FMLA) approvals without a clear diagnosis. Desperate, I pleaded on social media for my friends to help me with any suggestion they had. No one I had known had ever experienced symptoms like extreme dizziness, ataxia (physical impairment), memory loss, brain fog, vertigo, and rocking/falling/swaying sensations when sitting still.
A close friend recommended Dr. Peter Weisskopf at the Mayo Clinic in Phoenix. We made the sixteen-hour drive instead of flying because of my potential “perilymph fistula” diagnosis. I spent a day in testing—hearing tests, balance tests, any kind of test you could think of! The equipment they had at the Mayo was the best I had seen in my five-month quest to figure out what was wrong with me. For the first time, I felt hopeful they would figure it out. The next morning, Dr. Weisskopf walked in. He looked at me directly and said, “You have vestibular migraine.” I came back with: “That can’t be possible.” I rarely had headaches, and never once had pain so bad I thought it would be classified as a migraine attack. He explained that not all migraine disorders have head pain, and that they can manifest themselves in different (and very odd) ways. Some come with dizziness, vertigo, and imbalance—a migraine that affects the vestibular system. You can also be in a 24/7 continuous cycle of a migraine, which was what I was experiencing.
In a serendipitous moment, the next day I got a call from the University of Texas Southwestern Medical Center that an appointment had opened with Dr. Shin Beh, a neurologist who specializes in vestibular disorders. Word on the street was that he could solve any patient’s unexplained dizziness. I had been trying to get into Dr. Beh for months, as other doctors around Dallas had told me he was one of the best doctors in the nation for the symptoms I was experiencing. But he had been booked out for about six months, and I knew I would surely lose my job by the time I could get in to see him. Luckily a friend’s mom happened to work with him and let him know my story. I was curious to see if Dr. Beh would agree with the Mayo Clinic’s diagnosis.
I’m sure he thought I was nuts since I brought both my mother, who is a nurse, and my husband into the room with me. This was something I started doing a few months prior when I wasn’t getting answers from doctors. (Sadly, I found that many doctors took my case more seriously with my spouse in the room.) In fact, some of the physicians I saw prior to Dr. Beh would strictly talk to my husband while I was sitting right there. Having family in the examination room also allowed me to be more present at my appointment. With my brain fog, it was difficult to concentrate and ask the questions I needed to, even when they were written down.
Dr. Beh had his own set of crazy tests, a little different from the Mayo Clinic’s, but he finally confirmed it was vestibular migraine. He gave me three options for medication, all with benefits and drawbacks. I chose the treatment plan that I considered to be the easiest to wean off because I wanted to start trying for a family within a few months. Dr. Beh suggested I also begin the three most researched supplements for migraine prevention: magnesium, B2, and CoQ10. While we waited for those to begin working, I began my treatment regimen.
Within just a few weeks, I was feeling slightly better, although still dizzy every day. An overachiever, I assumed I was ready to jump back into working again. I was out of paid FMLA time and knew I would never get promoted if I continued to be out of work. Sadly, being back in the bright fluorescent lights, rows of desks, and stress triggered my symptoms almost immediately. When I had to use the bathroom, I ran my fingers along the cubicles to steady myself and feel supported. Walking down long hallways always felt like I was walking on clouds or in a bouncy house. My husband was driving me to and from work most days, but on the days he couldn’t, I just prayed in my car that I could get home safely.
While I was out on FMLA, my employer decided to change nearly everything about my job. They also moved my desk to a busy main walkway, where I had to face glare from outdoor windows. It was my worst nightmare. I wore tinted FL-41 lenses, as Dr. Beh instructed, but coworkers would laugh at me and ask why I was wearing sunglasses inside. I could only laugh too because it hurt so much.
To help with the stress, which always intensified my symptoms, I began to see a counselor. We worked on setting daily, weekly, and monthly goals. It took all my effort not to make these into career goals, but rather health-related goals. It could be anything like take a walk, practice mindfulness for ten minutes, or work on my vestibular therapy exercises. She had me write comments about each day in a journal so that I could review them at the end of the week or month. Looking back at some of my journal entries, it was so obvious what I needed to do, even though I didn’t see it at the time. On the days I was at the office, I felt horrible. My neurologist and my counselor both urged me to try to keep my stress levels low. They suggested I do a part-time FMLA, where I take time off as needed. This seemed like a good solution to my problem since I was never quite sure when a disabling vertigo attack might happen.
The intermittent FMLA was not as easy as it seemed. I had to make a call to my insurance company any time I left my desk. There was one point where I got mixed up on my hours or days (hello, constant brain fog!) and the insurance company called me to say they couldn’t approve my time. It felt as though I was constantly fighting with my HR department and my insurance company. After a long and honest conversation with myself, I decided I could not heal under this kind of stress.
There are many ways to protect yourself and work with your company to deal with migraine attacks. I just wasn’t aware of them until after I had left. At that point, I’m not sure I would have even tried. I was truly exhausted. And so, I handed in my two weeks’ notice. Want to know what happened after I left? They hired someone at the level I wanted to be promoted to, and then provided her with help. It was proof they wanted me out. My disability was a burden to them.