Chapter 15
Epstein-Barr Virus and Post-transplant Lymphoproliferative Disorders
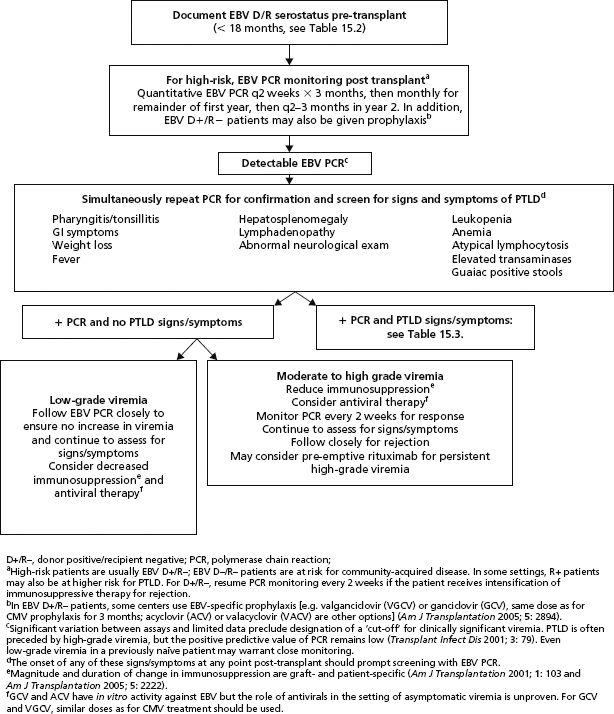
15.1 Prevention of Epstein-Barr virus (EBV)-related Post-transplant Lymphoproliferative Disorders (PTLDs)
15.2 Pediatric EBV serology in donors and recipients < 18 monthsa
Atul Humar
| EBV serology positive | EBV serology negative | |
| Donor < 18 months of age | Assumption = positive (even though this may be false positive due to maternal transfer) | Assumption = negative |
| Recipient < 18 months of age | Assumption = negative (in this case, assume this is likely due to maternal transfer) | Assumption = negative |
aSerology at < 18 months of age may not be reliable due to passive transfer of antibody. The above assumptions are made to assign the highest risk donor/recipient serostatus to the transplant patient.
Rebecca Madan & Betsy Herold
| WHO classification of PTLDb | Suggested therapy |
| Early lesions Plasmacytic hyperplasia Infectious mononucleosis-like |
Reduce immunosuppressionc Consider antiviral therapyd Rituximab if lesion(s) CD20+ and no response to reduction of immunosuppression |
| Polymorphic PTLD | Reduce immunosuppressionc Surgical resection if lesion(s) may result in obstruction Consider antiviral therapyd Rituximab (CD20+ lesion) if there is no response to reduction of immunosuppression Consider addition of chemotherapyf if no response following rituximab monotherapy |
| Monomorphic PTLD B-cell neoplasms Diffuse large B-cell lymphoma Burkitt/Burkitt-like lymphoma Plasma cell myeloma Plasmacytoma-like lesion Maltoma Other T-cell neoplasma Peripheral T-cell lymphoma, not otherwise specified Hepatosplenic T-cell lymphoma Anaplastic large cell lymphoma Natural killer-cell lymphoma Other |
Reduce immunosuppressionc Rituximab (CD20+ lesion)e Chemotherapyf Surgical resection if lesion(s) may result in obstruction |
| Hodgkin lymphoma and Hodgkin lymphoma-like PTLD | Reduce immunosuppressionc Rituximabe Chemotherapyf |
aPTLD treatment plans should be patient-specific and formulated by a multidisciplinary team familiar with PTLD management.
bHarris NL et al. (2001). PTLD. In: Jaffee ES et al., eds. Pathology and Genetics: Tumours of Haematopoietic and Lymphoid Tissues (World Health Organization Classification of Tumours). Lyons, France: IARC Press, 264.
cWhere possible, reduction of immunosuppression is important for the treatment of PTLD, although the appropriate magnitude and duration of reduction depends upon multiple factors, including graft type and staging, classification, and aggressiveness of patient’s PTLD (Am J Transplantation 2001; 1: 103).
dThe efficacy of antiviral therapy (acyclovir/ganciclovir) has not been documented by controlled trials. These agents offer the theoretical benefit of preventing spread of lytic phase EBV to previously uninfected B lymphocytes but do not affect the proliferation of EBV-immortalized cells. If used, ganciclovir or vanganciclovir should be given at doses similar to CMV treatment.
eConsider initiating rituximab earlier for patients with aggressive lesions or with worsening clinical status on reduced immunosuppression (Am J Transplantation 2006; 6: 569). Rituximab is typically indicated only for lesions with positive CD20 immunostaining.
fChemotherapy regimens are often disease- and patient-specific but may include cyclophosphamide and prednisone therapy (J Clin Oncol 2005; 23: 6481) and combination therapy with cyclophosphamide, doxorubicine, vincristine, and prednisone (CHOP) (Am J Transplantation 2006; 6: 569).