Chapter 3: A Brief History of Medicine
‘Whenever a doctor cannot do good, he must be kept from doing harm.’
– Hippocrates
Adding fuel to the mad fat fire are the changes in medicine – specifically the changes to mental health medicine.
In 1431, during one of the most famous trials in history, Joan of Arc testified to hearing voices in her head. Apparently they told her to deliver France from the invading English and establish Charles VII as the rightful heir to the French throne. Almost 600 years later doctors have ‘diagnosed’ Joan with a wide range of mental disorders ranging from schizophrenia, to bipolar disorder, to epilepsy. Today, it’s likely that Joan would be prescribed psychotropic drugs to deal with her ‘disorder’. What a loss to France and history that would have been!
There is little doubt that the tremendous breakthroughs in our understanding of health and the treatment of disease have saved millions of lives and improved the quality of life for many millions more. But, often these innovations have also had significant unintended consequences.
We Stopped Taking Responsibility
For a start, these medical breakthroughs and innovations allowed us to outsource responsibility for our own health.
In my grandparents’ day, you needed to pay to see the doctor; most people were fairly poor so they engaged in preventative medicine – before there was even a term for it! With the advent of wonder drugs, like antibiotics that could cure a vast range of diseases, people became less concerned with prevention because if worst came to worst at least there was a magic pill that would make them better. This mindset has gathered pace ever since and we have become major pill poppers. In the US, pharmaceutical companies will offer free trials of their medication via TV adverts without really going into detail about what the pill actually does and yet people clearly phone up for their free sample!
It’s easy to see the attraction of popping a pill to solve our problems but that approach definitely has side effects. Our overuse of antibiotics in animals and humans is a classic example. Antibiotics revolutionised human health – they have saved millions of lives and their benefit to humanity can’t be underestimated.
But, we have used them far too often for conditions or ailments that really didn’t require their use. Every sniffle, cough and splutter was treated with a prescription of antibiotics. Of course, they were so effective that the patient soon began to feel better and stopped taking the medication, thereby allowing the infection to mutate in the body and become antibiotic resistant. Even though it clearly states that we need to finish the full course of antibiotics when we are prescribed them, most of us don’t. This coupled with the overuse of antibiotics in animal rearing has resulted in superbugs such as MRSA that do not respond to antibiotics at all. In 2015, Mark Baker, director of clinical practice at the National Institute for Health and Care Excellence (NICE), warned that doctors write 10 million needless antibiotic prescriptions each year. This overuse means that antibiotics may soon be obsolete – an outcome that will have Fleming spinning in his grave. What a waste of a phenomenal drug. Of course, antibiotics are still essential for critical care and operations but their impact has been reduced by overuse. We urgently need to move away from antibiotics for anything except emergency care.
There is now way too much antibiotic residue in our bodies. On top of the antibiotics we may have taken as a prescription from our doctor, that residue is now being constantly ‘topped up’ because of the food we eat. Interestingly, the link between antibiotic overuse and mental health is beginning to emerge.
Conservatively there are about 1,000 different varieties of microbes coexisting harmoniously within a typical healthy person’s gut. In fact, the average adult carries up to five pounds of bacteria. Ninety per cent of serotonin, so crucial for mood and mental well-being, is created in the gut from healthy gut bacteria. Healthy good bacteria, known as probiotics, also regulate dopamine levels and ‘talk to the brain’ through the immune system or parts of the nervous system. The problem is that antibiotics don’t discriminate between good bacteria and bad. They don’t just kill the bad bacteria – they kill
all
the gut bacteria. According to Dr Martin Blaser, Chairman of the Department of Medicine at New York University’s Langone Medical Center, overuse of antibiotics may be changing our entire bacterial make-up. In a paper published in
Nature
, one of the most prestigious medical journals in the US, Blaser cited evidence that antibiotics may permanently change the beneficial bacteria in our gut.
A study co-led by researchers at the Universitat de València reveals that antibiotics produce changes in the microbial and metabolic patterns of the gut. For the first time this research showed that gut bacteria presents a lower capacity to produce proteins, as well as deficiencies in key activities, during and after the antibiotic treatment. Specifically, the study suggests that the gut microbiota show less capacity to absorb iron, digest certain foods and produce essential molecules. Iron is essential for mental (and physical) well-being because iron carries oxygen throughout our bloodstream. Low levels of iron can reduce the oxygen in the blood which can cause the development of psychological problems such as anxiety, panic attacks and extreme mental fatigue. If we are iron deficient we are also unable to digest certain foods, which also affects how much micronutrients we absorb – the vitamins and minerals essential for keeping us healthy.
In a separate study in 2013, low levels of healthy gut bacteria were linked to mental health issues such as anxiety, schizophrenia and autism. The study published in
Nutritional Neuroscience
from the Great Plains Laboratory showed that HPHPA levels – a chemical by-product of clostridia bacteria (bad bacteria) – are much higher in autistic children. The study showed that after treating teenagers who suffer from obsessive-compulsive disorder (OCD) and attention deficit hyperactivity disorder (ADHD) for six months with high-strength probiotics their symptoms began to disappear and after a year they were completely gone! Just stop and think about that for a moment…These conditions affect millions of people worldwide, causing stress and anxiety to them and the people who love them. Drug companies get richer from endless prescriptions and yet increasing our probiotics, either through improved diet and/or supplements, is much more effective and could cure these conditions.
And finally, McMaster University in Canada published the results of their research project in the
Journal of Communicative and Integrative Biology
in 2010 showing a link between gut bacteria and mental health. Scientists compared the behaviour of normal eight-week-old mice to mice of the same age that had been stripped of their natural gut bacteria. The mice without any gut bacteria showed higher levels of the stress hormone cortisol and were exhibiting risk-taking behaviour. Granted, I’m not exactly sure what risk-taking behaviour in a mouse looks like, but in all seriousness the lack of bacteria was shown to alter levels of a brain chemical called BDNF which is linked to depression and anxiety in humans.
Commercialisation of Medicine
The second big change was the commercialisation of medicine. New innovations created new opportunities to make money and, boy, did the big pharmaceutical companies coin it in!
In her book
The Truth About Drug Companies
, author Marcia Angell MD, who is also incidentally the first woman to serve as editor-in-chief of the prestigious
New England Journal of Medicine
, reported that in 2002 the profits earned by the top ten drug companies in the Fortune 500 (the richest companies in the US) were greater than the profit of the other 490 Fortune 500 companies combined!
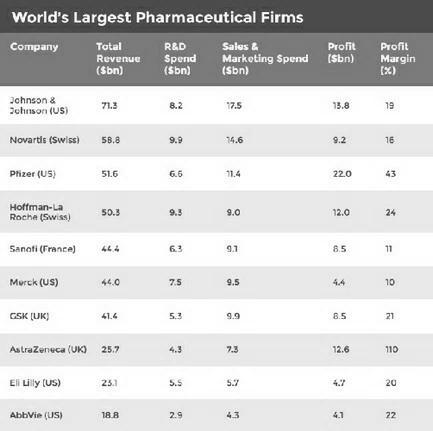
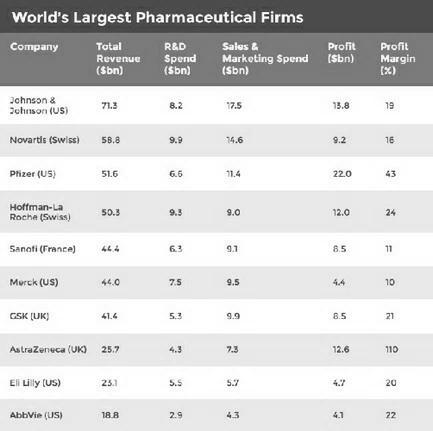
Figure 3.1: World’s largest pharmaceutical firms
Source: GlobalData (http://www.bbc.co.uk/news/business-28212223)
Before you read on, just take a minute to stop and
really
look at Figure 3.1…These drug companies are making an absolute fortune! The revenues of many of these global businesses are greater than the gross domestic product (GDP) of entire countries. Also have a look at the research and development (R&D) spent in comparison to revenue. These drug companies try to justify the cost of their medication because the cost of testing and researching drugs is so enormous. That’s true – it is. But when those same companies can legally suppress clinical trial data and cherry-pick the results that suit their objective – to get the drug approved so they can sell it – then the clinical trials are actually a farce (see the Reboxetine example below). Which means that we (personally, our medical insurance company or the NHS) are buying incredibly expensive drugs that may not even work for us, may actually make us sicker or – worse – kill us. In fact, in his book
Deadly Psychiatry and Organised Denial
, author Professor Peter Gøtzsche states that the third highest cause of death in the UK after heart disease and cancer is psychiatric drugs! And Gøtzsche should know – he’s an investigator for the independent Cochrane Collaboration – an international body that assesses medical research. Considering that 80 million prescriptions for psychiatric drugs are written in the UK alone every year that’s terrifying.
The purpose of many of these drugs is clearly not about health and well-being, it’s about money, money and more money. For example, some cancer drugs cost upwards of $100,000 for a full course. But they cost a fraction of that to manufacture. How much incentive is there for pharmaceutical companies to find a cure for cancer when they can make that sort of money treating it? In 2013 100 leading oncologists from around the world wrote an open letter in the journal
Blood
calling for a reduction in the price of cancer drugs. Dr Brian Druker, director of the Knight Cancer Institute, and one of the signatories, asked: ‘If you are making $3bn a year on Gleevec [a cancer drug], could you get by with $2bn? When do you cross the line from essential profits to profiteering?’
But that’s not all. Look at the sales and marketing spend in comparison to the R & D spend. In some cases it’s almost double. So hang on, drug companies say they charge so much and profit from other people’s misery because the cost of R & D is so huge – only the R & D is a lie and actually the companies spend twice that trying to convince us – patients and doctors – that it’s not.
Oh, and by the way, sales and marketing for big pharmaceutical companies is not about where to place a full-page advertisement in what national newspaper or what TV commercial to make. It’s actually lobbying health groups to lower ‘the healthy limit’ to create new markets like the cholesterol example I shared in the last chapter, or seeking approval to market the drug to a different demographic, or rebranding the same drug for a different condition. Often this approach ends in fines. For example, GlaxoSmithKline were fined $3 billion in 2012 for promoting Paxil for depression to under-18-year-olds. In 2009, Pfizer was fined $2.3 billion over misbranding the painkiller Bextra. Johnson & Johnson was fined $2.2 billion in 2013 for promoting drugs not approved as safe. In 2012 Abbott was fined $1.5 billion for illegal promotion of the antipsychotic drug Depakote. Eli Lilly were in trouble in 2009 and fined $1.4 billion for wrongly promoting antipsychotic drug Zyprexa and Merck was fined $950 million in 2011 for illegally promoting painkiller Vioxx.
These are huge fines but they are nothing to the money that was made before the fine was imposed. Plus these companies have epic legal teams fighting these battles every day. Even when they are fined these faceless corporations are still the winners, as evidenced by their billion-dollar revenues year on year.
The other really popular sales and marketing tactic is to create new ‘conditions’. I have a friend who ran a half-marathon in Sydney a few years ago and she ended up running with a PR officer for a large pharmaceutical company. She had actually just quit her job because she couldn’t stand it any more – most of her job involved sitting around the corporate boardroom with other sales and marketing executives dreaming up new diseases, disorders or conditions that the team could then publicise and sell products for. This practice is so morally and ethically screwed up that it’s hard to believe it actually happens and yet it is normal business practice in big pharmaceutical companies.
And of course we’ve lapped it up…We have become obsessed with health and we are increasingly conscious of when we don’t feel well. So we ‘Google’ our symptoms and before lunchtime we have shortlisted our disease to two pages of A4 paper. Come on, admit it – you’ve done it. We’ve all done it! We could easily mount a very strong case, especially in the developed Western world, that we are a bunch of hypochondriacs. But the drug companies have had a direct hand in creating our collective hypochondria. As a sales and marketing strategy it’s pure genius – dream up new ‘conditions’, advertise the condition to raise our awareness of it, so we can think we have it and then sell us the cure!
It’s just a lie based on money and it rarely has anything to do with you or your health.
Ever since antibiotics the scientific community and the big pharmaceutical companies have sought to find a magic bullet that will cure every condition on the planet. This objective was brought ever closer once the human genome was mapped. Today there are hundreds of thousands of scientists around the world trying to isolate what gene causes what condition so pharmaceutical companies can patent it and sell us the drug for ever. Of course, it’s not yet yielded the fruits they were hoping for because human beings are incredibly complex and what works for one will not necessarily work for another. The way our genes express themselves depends on a myriad of factors, from diet to environment, to physiology to gender, to ethnicity and beyond. So the very idea that we will reach a point where one pill will cure cancer, diabetes, obesity etc. is almost science fiction.
Please understand, I’m a huge fan of science and the people on the front line doing the research and genuinely seeking cures for terrible conditions, but I am not a fan of the companies that are so often pulling the strings or funding that research (often without the researchers knowing about it) so they can profit from illness and misery.
According to a recent global analysis project, if current trends continue, depression will be the second greatest disease burden by the year 2020 and the first by 2030. It is now estimated that 350 million people globally are affected by depression. And that doesn’t take other mental health issues into account.
Mental health is booming. Not just in terms of the escalating number of drugs created to ‘treat it’ but the escalating number of mental health disorders to treat. In the last 20 years there has been a huge increase in the number of new ‘mental health disorders’ classified and labelled. People who were previously viewed as simply shy, eccentric, or easily bored are now labelled with a disorder or condition.
The Diagnostic and Statistical Manual of Mental Disorders (DSM)
– the ‘go-to guide’ for all mental illness – adds new entries to their book every year, voted in by a show of hands in a room full of men in suits. Last year they even added ‘Internet gaming disorder’ to their list of mental health disorders and have requested further study to decide which medication is best to prescribe. Again, this is not about health and well-being. This is about money. If something can be labelled, then big pharmaceutical companies can sell pills to medicate it!
And, with such huge numbers lining up to take those pills (often for non-existent conditions) it’s easy to see why, in 2015, the mental health pharmaceutical market was estimated to be worth $88.3 billion. And of course, once someone is prescribed antidepressants, many of which are very addictive, that revenue is going to pour in for years, possibly decades.
I suppose in some ways we should be grateful – before Thorazine (the brand name for chlorpromazine) was developed in the 1950s mental illness was often treated with surgery – known as a lobotomy. In fact, the man who developed this psychosurgery procedure was awarded the Nobel Prize for his work in 1949. When a patient had a lobotomy the surgeon removed part of the brain. Now considering that in 2016 we still don’t yet know all the mysteries of the brain and probably know more about the surface of the moon than we do about the interconnections and functions of the human brain, slicing off chunks doesn’t seem like a particularly sophisticated approach. And yet unbelievably, more than 20,000 people underwent lobotomies in the US during the 1940s until these new drugs were invented to treat our madness.
My Early Experiences of Madness Medication
I was first prescribed antidepressants in my late teens and, to be honest, I didn’t notice much difference in the first few weeks. In fact, I started to doubt whether they were working. But a week or so later, they kicked in and my world went from glorious Technicolor and the ups and downs of life to bland black and white. My feisty, sassy personality disappeared as I descended into the uneventful world of life on antidepressants. I don’t know what it’s like for you – but for me nothing seemed to matter that much any more. Things that I would normally get so worked up about would just breeze past without incident. I didn’t get overly excited about anything but nor did I get overly upset by anything. I wasn’t happy but I wasn’t sad either and initially that stability was a relief. I was glad to be rid of the black dog that had burdened me for years – it was a welcome respite from feelings of self-loathing and hopelessness. I got used to the metallic taste in my mouth and the broken sleep at night. I hated the weight gain but at least I could function during the day without crying – so I kept taking the pills.
This went on for years until I fell pregnant and decided to stop – ‘cold turkey’. For the record, cold turkey is not a good idea when stopping antidepressants. In hindsight, I think I was saved from severe withdrawal because there were so many happy hormones pumping around my body as a result of the pregnancy. Carrying my son was an epiphany. During the months he grew in my belly, I remember driving to work and the sky really did look bluer to me, my perception was heightened, I noticed more, I felt like a child again full of wonder and excitement for the future. I remember looking at the planes in the sky as I travelled to work, singing along to tunes on the radio and feeling the best I’d ever felt in my life! Of course, I put this down to the pregnancy hormones coursing through my body. It certainly didn’t occur to me at the time that my new ‘Ms Blue Sky’ feelings may have been down to the fact that I was religiously taking folic acid and various vitamins and of course I was no longer taking the fluoxetine antidepressant. I was too busy enjoying the novelty of optimism – I felt alive for the first time in years and when my son was born I was on top of the world – despite a pretty horrific birth.
Unfortunately it didn’t last. Once I’d stopped taking the supplements I’d been taking throughout my pregnancy things soon returned to my grim ‘normal’. I panicked, looking after myself had been hard enough and now I had a beautiful newborn baby to look after, so I went back to the doctors. Of course, I was immediately put back on the antidepressants, along with a long lecture for coming off them in the first place. Within a matter of weeks I was back to the old routine. I couldn’t work out what was worse, the depression or the fact that I felt like I was back to square one.
Things were OK for a while, I seemed to be able to deal with everyday life, but then I suffered a bereavement and that tipped me over the edge into a full-on nosedive. My doctor increased my dose and that’s when I really noticed a difference. It was like taking drugs in a nightclub except the music was scary and I was the only person on the dance floor with a spotlight on me. As a single parent I really struggled to cope, sitting in my living room on my own as my young son lay in bed, not knowing how I could care for him, or how I could face work in the morning. I was tripping out of my head but Pink Floyd wasn’t playing in the background. I experienced hallucinations, terrors and thoughts most of us couldn’t even imagine. It was horrific and even though I was in a mess I knew medication was not the answer. I went back to my doctor for help but he just put me on a different type of antidepressant (paroxetine).
Although I wasn’t even sure, it was possible the new drug made things even worse. The black dog was back with a vengeance and this time I couldn’t fend him off. I remember sitting crouched on my kitchen floor terrified of the future. I just didn’t know what to do so I called my parents and I will never forget the confused look on their faces as they took my son – now a toddler – away to their house ‘for safekeeping’.
I phoned in sick to work and spent days in bed. When I surfaced I started researching online for an alternative solution because the one I was prescribed was clearly not working. I discovered orthomolecular medicine – a form of alternative medicine which was based on maintaining health through nutritional supplementation and had men like Max Gerson, Abram Hoffer and Linus Pauling (the only man in history to have won the Nobel Prize twice) supporting its efficacy. In other words, these great scientists were coming out and publicly saying this approach really worked. Plus there was a whole bunch of studies and clinical evidence that supported the theories.
I thought if twice-winning Nobel laureates are promoting this stuff then there must be something in it – so I investigated further. There are days, I’m not even sure I’d still be here if I hadn’t – it literally saved my life. And it absolutely changed my life! And my son’s too. He had been suffering from chronic food allergies, asthma and eczema, and the doctors had prescribed steroid ointments, Ventolin syrup and inhalers. When he was just four years old he nearly died on a holiday when he had an allergic reaction to a pony he was riding in the mountains. He had an almost immediate reaction to the pony and his face blew up like a balloon and he could hardly speak. Unbelievably, a Canadian lady who was also on the tour had a bottle of Benadryl in her handbag, she pushed his tongue, which was now huge, to the side and poured it down his throat. The antihistamine in the Benadryl was enough to stop the swelling from getting any worse while I drove like a maniac to get him to hospital for a steroid injection. If that lady hadn’t had a cold and hadn’t had the Benadryl in her bag my son would probably have died. In a separate incident I had to take him to hospital in Chicago after he ate some chocolate pudding.
Thankfully, I immersed myself in orthomolecular medicine and we changed our diet and started to take supplements. Within a matter of months my son’s allergies miraculously disappeared, he could breathe without the need of an inhaler, and I lowered my dose of antidepressants one week at a time until I was finally free of them 12 weeks later. I’ll explain exactly how I achieved this in the action plan later in the book, so you can see if you can successfully and safely do the same.
Other than the odd podiatrist appointment due to an ingrown toenail, my son and I have not visited the doctor in almost a decade. Touch wood – we never get the flus, colds and stomach bugs that everyone else seems to get and we are both fighting fit!
Turning Back the Clock
Before big pharmaceutical companies muscled in to profit from our madness and ill health, early pioneers intent on finding answers, not money-making opportunities, were doing amazing and important work.
In the early 1900s, for example, psychiatrists like the infamous Dr Henry Cotton practised experimental ‘surgical bacteriology’ on mental health patients. The thinking at the time was that insanity was the result of untreated infections. Dr Cotton would remove teeth and various organs from patients in an effort to rid the body of infection. The colon was of particular interest and doctors believed that bad bacteria in the gut, or as they called it at the time ‘intestinal putrefaction’, was the cause of mental illness. Therefore if the doctor removed the colon or part of the colon then the patient would be restored to normal health. The main stumbling block to this theory was that antibiotics had not yet been invented, so the surgery ended up killing one in three patients.
However, other doctors at the time such as Doctors Louis Julianelle and Franklin G. Ebaugh discovered a less invasive method of treating patients, stating, ‘We do not believe that colectomy is justifiable. Putrefaction, if present, may be eliminated by a change in the intestinal flora.’
Their paper, ‘Implantation of Bacillus and Acidophilus in Persons with Psychoses’, published in 1923 was a study based on treating mental health patients by populating their guts with good bacteria. It never ceases to amaze me just how ironic it is that despite our breakthroughs and innovations we have repeatedly turned our back on common sense that our grandparents seemed to already know, not to mention the insightful science and accurate diagnosis in favour of the flashy answer or the magic potion. And we are still doing it today.
It has taken a while but finally, some 100 years later, scientists are now recognising the link between good bacteria in the gut and mental health. You simply can’t have one without the other.
Doctors in the Dark
I’m sure, like me, you rely on your doctor and you may already be thinking, ‘OK, but hang on. Surely if all this were true our doctor would know about it and they would be making alternative suggestions.’ It’s a perfectly reasonable question and the answer is that doctors should know about this but they don’t. But before you get upset at your doctor – it’s often not their fault.
There are a number of issues that keep doctors in the dark about the importance of nutrition and especially the key role of micronutrients in the diet and how their loss can have a profound impact on our mental and physical well-being.
The first is that they are simply not taught about it in medical school. In the mid 1980s, a landmark report by the
National Academy of Sciences
highlighted the lack of adequate nutrition education in medical schools and the writers recommended a minimum of 25 hours of nutrition instruction. Two and a half decades later, a 2010 study by researchers at the University of North Carolina,
Chapel Hill,
found that the vast majority of medical schools still fail to meet the minimum recommended 25 hours of instruction. Only a quarter of 100 medical schools surveyed offered the recommended 25 hours on nutrition – four schools offered nutrition as an option, and one school offered nothing at all.
But even at 25 hours, it’s nowhere near enough time to understand the impact of nutrition on the body. It isn’t close to adequate for doctors to understand the various minerals, vitamins and micronutrients we need in the body and how a lack of one can have a knock-on effect elsewhere. The human body is a highly interconnected, subtle and extremely complex system, and yet we know virtually nothing about the fuel we put into the system and how it can impact performance. You wouldn’t buy a Ferrari and put fizzy juice in it and expect to get very far, and yet we have an amazing body and we constantly put crap in it and expect to live long and healthy lives.
To be fair to doctors, results of a study carried out in the Aberdeen district of Scotland showed that despite their ignorance on the subject, over 90 per cent of doctors requested more teaching on the practical aspects of nutrition. Indeed both medical students and junior doctors were very enthusiastic to learn about nutrition, and also felt that their teaching was inadequate.
The other big issue that keeps doctors in the dark is time. Just think about everything that a GP needs to know. It’s a genuinely phenomenal amount. But even once they qualify and start practising they also have to keep up to date with latest breakthroughs. Those that specialise become an ‘ologist’ of one form or another and tend to have a deeper and deeper knowledge about a narrower and narrower field. Often those fields have their own language and argue over finer and finer points of differentiation, which means that getting up to date and staying up to date is almost impossible. Plus doctors always have a waiting room of patients to attend to.
Even if they did manage to carve out some time to research the latest drugs on offer or the latest procedures, they often don’t have access to accurate clinical trials data when making decisions about what drugs to prescribe to patients.
Before a drug is approved for use the drug company has to invest billions in clinical trials – these are supposed to make sure the drug works and to find out about any side effects the medication may have. It would make sense therefore that doctors, or other medical professionals who could interpret that data, should have access to all the results of the various clinical trials. But that doesn’t happen. What you may not know about clinical trials is that a drug company is under no legal obligation to share those results. So they only ever publish the data of the clinical trials that worked and bury the trials that didn’t. So when your GP is punching in their diagnosis of your condition the recommended drugs that come back are often based on erroneous or incomplete clinical trial data. Neither you nor your doctor have any way of knowing whether you match the profile of people on the successful clinical trial, in which case the drug might work, or whether you fit the demographic of the clinical trials where the drug didn’t work or, worse, created severe side effects.
Take the antidepressant Reboxetine as an example; Ben Goldacre writes about this in his brilliant book
Bad Pharma
. (If you want to get really mad – I highly recommend you read that book!) When he’s not writing books that lift the lid on medicine he’s a GP and he readily admits he has prescribed Reboxetine himself.
He’d looked at the available clinical trial data and considered them well-designed trials with overwhelmingly positive results. It was shown to be better than placebo and better than head-to-head comparisons with other antidepressants. And, it was approved by the Medicines and Healthcare products Regulatory Agency (MHRA) which governs all drugs in the UK. Millions of people around the world are on Reboxetine. In October 2010 a group of researchers managed to collect
all
the clinical trial data for
all
the trials of Reboxetine. The result was
ver
y different. Seven trials had been conducted comparing the drug with a placebo or sugar pill. Only one of those trials, with 254 patients, showed a positive result against a sugar pill with no pharmaceutical properties at all. Needless to say that trial was published in an academic journal for doctors and researchers to read. But it was publication bias, or at best an anomaly, caused by something other than the drug. How else can we explain the fact that the other six trials which featured almost ten times as many patients showed that Reboxetine was no better than the sugar pill? Of course, none of those trials were published anywhere.
So millions of people are being prescribed a drug that they believe is going to make them feel better when in actual fact they would be better off taking a jelly bean every day. But that’s not the worst of it. It’s blatant profiteering, but at least it’s not doing any harm – right? Unbelievably no, that’s not the case.
In other trials Reboxetine was compared to other antidepressant medication and 507 patients demonstrated that the drug did just as well in head-to-head tests. Again that trial was published.
Again
doctors and researchers, like Ben Goldacre, would read these results and be further convinced of the efficacy of the new drug. Many, like Ben Goldacre, probably went on to prescribe Reboxetine as a result. But there were another 1,657 patients who took the new drug and they all did worse than those on other drugs. Again, that data was squirrelled away and not published anywhere. But it gets worse.
In terms of side effects Reboxetine looked fine in all the published papers about the drug that appeared in academic and medical journals. But when the researchers looked at all the clinical trial data it turned out that patients were more likely to have side effects – and were more likely to stop taking the drug and withdraw from the trial because of those side effects than when they took the comparison drugs. As Goldacre states, ‘In the published data, Reboxetine was a safe and effective drug. In reality, it was no better than a sugar pill and, worse, it does more harm than good.’
What you absolutely have to understand is this is not a one-off isolated incident or event – this is business as usual in big pharmaceutical companies and it’s not limited to this one drug. In fact it’s almost unfair to call out Reboxetine because it implies this is rare. It’s not rare – what is rare is that researchers were able to get access to all the clinical trials. That is almost impossible.
Even though the World Health Organization (WHO) made a fresh call for the public disclosure of all clinical trial data in 2015, there is so far no change to the law and no change to ‘business as usual’ for the big pharmaceutical companies.
The drug companies are of course resisting – very strongly. For a start many of the drugs simply wouldn’t get approved if all the data was available. Plus many of these clinical trials also include placebo trials – many of which demonstrate that a sugar pill or saline injection delivered by a doctor is just as effective as the drug company’s expensive new drug. At the moment these results are also suppressed. After all, even drug companies can’t charge billions of dollars for Smarties!
The same thing has happened in complementary and herbal medicine. Despite the fact that herbs have well-documented healing powers that have been used by human beings for thousands of years, in 2002 the EU and UK tried to ban vitamins and herbal remedies. Luckily there was a public outcry, but in 2011 EU rules came into force banning hundreds of herbal remedies – forcing many natural practitioners and manufacturers out of business. As a result, in the UK today herbal remedies – medicines and treatment that have been used successfully for millennia – have to be assessed by the Medical and Healthcare products Regulatory Agency (MHRA) and are only allowed to go on sale to the public if the MHRA approve them. This is in stark contrast to the downright dangerous drugs that are already on sale by big pharmaceutical companies based on incomplete clinical trial data. Something is seriously wrong when GPs regularly hand out antidepressants with thousands of side effects – some of them lethal – but the notion of taking plants as medicine is somehow more dangerous? It’s utterly ludicrous.
In the UK herbal remedies now need to be registered on the Traditional Herbal Registration (THR) scheme – a process which costs many thousands of pounds for each remedy. This has all but crippled small independent herbalists who don’t have the means to register their products – often remedies they have used safely and effectively for years. The THR scheme can also only be used for minor ailments – not chronic conditions – further stifling the industry. Of course, this government intervention, usually aided by big business lobbying, plays right into the hands of the pharmaceutical companies because their natural remedy competitors have to either increase the price to cover the costs of registration or they simply go out of business altogether. This is why herbal medicines are so expensive compared to over-the-counter pharmaceutical drugs.
Plus if you look on the UK NHS website, for example, you will find some terrifying information about herbal medicine. Visitors are warned, ‘You may experience a bad reaction’, and ‘They may cause problems if you are taking other medicines’. ‘Pregnant women, breastfeeding mothers, children and the elderly should avoid them’, ‘Using them for more serious conditions could put you at risk’. We are told, ‘The claims made for herbal medicines are based on traditional usage and not on evidence of the products’ effectiveness.’ Claims made by big pharmaceutical companies are often not even based on traditional use and, in many cases, little evidence of the products’ effectiveness, and yet they are sold in their billions, often with serious and extremely dangerous side effects.
Clearly there are some pharmaceutical drugs that have been immensely important for human health but it doesn’t alter the fact that we’ve used plants since the beginning of human history to heal ourselves and thousands of studies show they’re effective. The scaremongering by those who want to sell us something else instead is all about money and control, and nothing about health and well-being.
It’s also bonkers when you consider there are 4,719 evidence-based herbal medicine research paper links on the National Institute for Health and Care Excellence (NICE) website – an organisation and website that is part of the UK government Department of Health. Talk about mixed messages! Of course, those looking for advice on herbal medicine are unlikely to find that website. Instead they will probably log on to the NHS site for information – information that is likely to scare them away from herbal medicine or any complementary medicine techniques and approaches.
What you have to remember is that the goal of big pharmaceutical companies is not health – it’s money. In the same way that food companies continuously sell us diet products that don’t work but give us hope, drug companies are happy to continuously sell us drugs that don’t work but give us hope. Often they are making a huge amount of money by simply masking the symptoms or treating the condition and are not even genuinely looking for a cure. And they don’t want placebos, herbal or complementary medicine screwing with their profits so they seek to discredit the alternatives instead.
Finally, the last, although connected, issue that is keeping doctors in the dark is a combination of the other two. Doctors don’t have enough time to do the research so they rely on others to keep them abreast of new drugs and developments. Often those ‘others’ are pharmaceutical company sales reps. The doctors are therefore being ‘informed’ by the very people charged with selling the resulting drugs to GPs so they will prescribe them to their patients and boost profits. You don’t need to be Einstein to realise that this ‘information’ is seriously biased.
NHS cardiologist Dr Aseem Malhotra, the doctor leading the call for a public inquiry into drug companies’ ‘murky’ practices, warned that commercial conflicts of interest are contributing to an ‘epidemic of misinformed doctors and misinformed patients in the UK and beyond’. Dr Malhotra stated, ‘There is no doubt that a “more medicine is better” culture lies at the heart of healthcare, exacerbated by financial incentives within the system to prescribe more drugs and carry out more procedures. But there’s a more sinister barrier to making progress to raise awareness of – and thus tackle – such issues that we should be most concerned about, and that’s the information that is being provided to doctors and patients to guide treatment decisions.’ Dr Malhotra accused drug companies of ‘gaming the system’ by spending twice as much on marketing than on research. Something I drew your attention to earlier in this chapter.
Wrap Up
I have come to believe that almost all mental illnesses – apart from the criminally insane – can be cured with love and a good diet. This is not a novel opinion. Hippocrates, the father of medicine and the man who created the Hippocratic oath, taken by doctors to ‘first, do no harm’, mostly prescribed food, herbs and sometimes wine to his patients. There’s always a silver lining!
The link between nutrition and mental health is undeniable and one that must be taken seriously by GPs and psychiatrists before scribbling that prescription for psychotropic drugs. The drugs on their own won’t cure you and can even hinder recov-ery as you then have the problem of coming off them. Plus in many cases they can make things worse because they are packed with ingredients that further damage our brain and body.
In a comprehensive peer-reviewed paper published in the
International Journal of Health and Nutrition
in 2013, the authors cited over 100 research studies in support of their evaluation that lack of certain nutrients can contribute to the formation of psychiatric disease and we will fully explain which ones and why in the following pages.
This is great news for everyone who is currently fat, mad or both, because it means that we can eradicate the mad fat epidemic. We can heal ourselves and it’s time to learn how.