CHAPTER 1
Why Are We So Fat Despite Our Best Efforts?
The Hidden Factor No One Is Talking About
If we could give every individual the right amount of nourishment and exercise, not too little and not too much, we would have found the safest way to health.
—Hippocrates, the father of medicine (460–370 BCE)
If you could go back in time to an era when people believed the earth was flat, how difficult do you think it would be to convince someone that it was, in fact, round? What argument would you use to prove your point? And no, you cannot time travel with a globe in your pocket or images taken from the moon. Without any evidence of a round earth on hand, chances are you would have a tough time convincing anyone that you were right. After all, it is difficult to see the curvature of the earth from its surface—we see straight horizons, not curves. The idea of a spherical shape first appeared in Greek philosophy, credited to Pythagoras in the sixth century BCE. Aristotle provided evidence for it on empirical grounds by around 330 BCE, but it would take centuries for universal acceptance of a round earth that revolved around the sun. Even today, at least four U.S. professional basketball players claim to believe the earth is flat, so you cannot convince everyone, no matter how strong the data are!
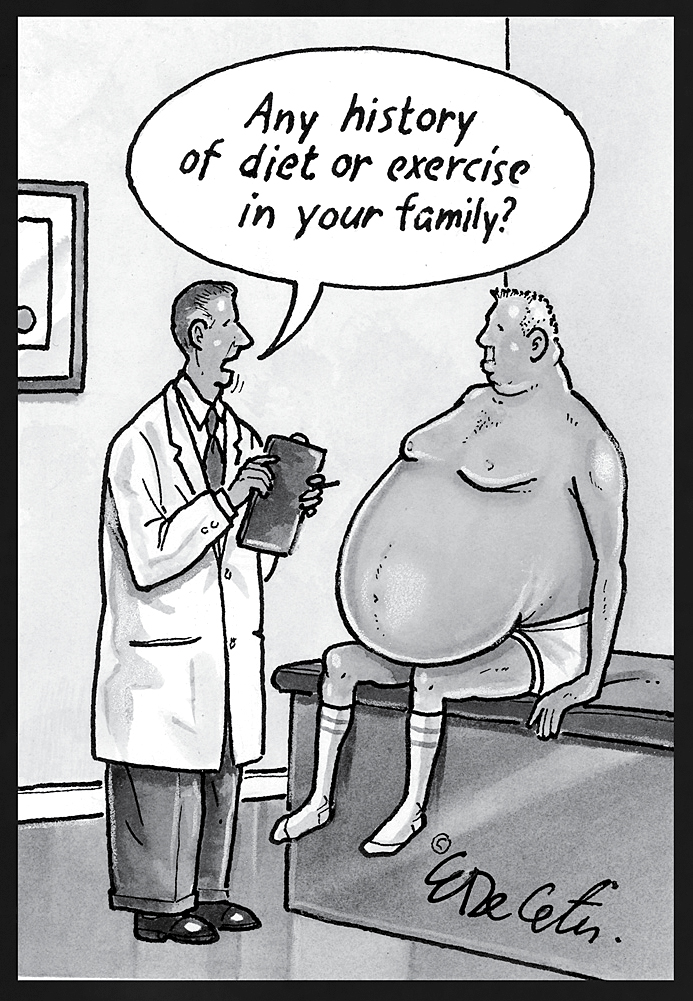
When I speak before large professional audiences about obesogens and their impact on the obesity epidemic, I used to feel like that hapless individual trying to persuade the Flat Earth Society that the planet is indeed spherical. Old theories die hard, especially ones that people have clung to for a long time or when the reality seems to defy logic. This is absolutely true when it comes to our ideas about how and why we are so fat today. Laymen and doctors alike continue to believe that body weight is exclusively determined by the number of calories consumed compared with those burned—simple as that. Just look at the website of the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), where it states definitively: “Overweight and obesity result from an energy imbalance.”9 If only this were the case. You might be surprised to learn that the number of health clubs has doubled over the same period that obesity has doubled. Clearly people are trying hard not to be obese. If only the solution revolved around diet and exercise alone.
Though most everyone has a clear picture of what obesity looks like, obesity is primarily defined by the body mass index (BMI). According to the WHO and American Medical Association, you are considered to be “underweight” if your BMI is less than 18.5, “normal weight” if your BMI is between 18.5 and 24.9, “overweight” if your BMI is between 25 and 29.9, and “obese” if your BMI is 30 or higher. A BMI beyond 40 is considered to be morbidly obese and indicative of a serious health problem. The BMI is a calculation based on height and weight but does not distinguish muscle from fat and bone in the body. I often show a slide comparing three people with identical BMIs of 32. One has extensive subcutaneous (below-the-skin) fat, which is not really problematic for health; another has abundant visceral fat deep inside and around the organs, which, as we will describe later, confers many of the health risks associated with obesity. The third picture is of the “Governator,” Arnold Schwarzenegger, at the pinnacle of his bodybuilding career. Despite having a BMI of 32, he was not remotely obese or even overweight. Thus, BMI is not a perfect indicator of whether or not you are obese. However, it is easy to calculate and a convenient generalization.
Let’s do one more imaginary time-travel experiment: Think about what it would be like for a family of Stone Age hunter-gatherers to experience the modern world (think The Flintstones meets My 600-lb Life). I picture stunned looks on the faces of our ancestors as they take in our modern conveniences—cars, cell phones, computers, electricity, and even supermarkets. And they are also taken aback by our body size. Given our twenty-first-century bulk, would they recognize us as members of their own species? Unlike us, they worked hard for every morsel and probably rarely had much leisure time to sit around eating unhealthy food. There were no fast-food restaurants or processed meals.
Hippocrates was right to stress the importance of moderation in diet and exercise as well as the value of food; diet was considered to be one of the most important interventions in Hippocratic medicine. This was certainly true in his time, but it misses a key part of the equation today. Hippocrates could not have known about endocrine disruptors or the effects they can have on our health and weight. And he, too, would probably be scratching his head in bewilderment at the obese masses at the dawn of the twenty-first century—a mere twenty-four hundred years after he lived.
Inexorably, we have grown accustomed to seeing a world of fat around us. The obesity facts are played over and over again in the media, so much so that they no longer surprise us. Overweight and obese individuals are the norm in most areas of the country instead of an anomaly. But fifty years ago you would have been hard-pressed to find many such people on the planet, let alone in one geographic location. As recently as 1990, obese adults in the United States comprised less than 15 percent of the population in most states. By 2010, thirty-six states had obesity rates of 25 percent or higher, and twelve of those had rates of 30 percent or higher.10 Obesity has increased threefold over the past forty years and has doubled worldwide in the last twenty years; in the last thirty years, obesity has more than doubled in children and quadrupled in teens. Today there are more overweight and obese adults aged twenty years and older in the United States (70.7 percent) than those of normal, healthy weight and underweight.11-13 More than one-third of U.S. adults are obese, and a whopping 86 percent of us are expected to be overweight by 2020. A full 20.6 percent of adolescents aged twelve to nineteen years are obese; 17.4 percent of children aged six to eleven years are obese; and almost 10 percent of kids only two to five years old are already saddled with obesity.11,13 Individuals who had previously enjoyed life in the slim lane at the lower end of the body mass index are now gaining weight, too, and entering the “overweight” and “obese” categories. It becomes difficult to even see the problem because when everyone around you is overweight, it turns into the expected.
But this is not normal. Could it be that we really lack the willpower to control our waistlines through classic diet and exercise because we live in an age of abundance? That it is all about lack of self-control? I don’t think so. Let’s not forget that there is also an obesity epidemic among infants of six months of age and younger, an age group where food choices and limited physical activity cannot explain this phenomenon; infants move as little or as much as they want and eat until they are full. The obesity epidemic is not limited to humans, either—it is also affecting animals living with us, including domestic dogs and cats, feral rats living in cities, and, crucially, primates and rodents living in research colonies where diets are carefully controlled.14 Are these animals also suffering from a lack of willpower? Highly doubtful.
The seminal 2016 study on our increased average BMI that I mentioned in the introduction was among the first to really call out the new facts.5 The researchers in this particular study mined dietary data from 36,377 U.S. adults from the National Health and Nutrition Examination Survey (NHANES) between 1971 and 2008 and showed that we are 2.3 points higher on the body mass index today than we were just a generation ago—even after correcting for how much we eat and exercise. The published conclusion spoke volumes: “Factors other than diet and physical activity may be contributing to the increase in BMI over time.” Granted, as I mentioned, BMI itself is not the best measure of obesity because it does not differentiate between fat mass and muscle mass or even where the fat is located, an important factor we will explore later. Yet despite the shortcomings of BMI as a metric, it does offer a reasonable reference point to use in evaluating body composition in the population.
So what is the most compelling explanation for these new facts? Something has changed in our environment—something that occurs where humans live, work, and eat.
HOW EXPOSED ARE YOU?
Take a look around you and think about a typical day, including that of your young children if you have them. In what ways can your environment impact your biology—and especially that of your children who are still developing, which makes them uniquely vulnerable? Here is a brief quiz that can help clue you in to the kinds of exposures that can cause a human body to create more fat. Many of these exposures could have happened long ago.
 Do you regularly drink from plastic beverage containers, including soda bottles, juice, and so forth?
Do you regularly drink from plastic beverage containers, including soda bottles, juice, and so forth?
 Do you have trouble sleeping well on a regular basis? (And yes, sleep deprivation can be considered an “exposure”; see chapters 5 and 9.)
Do you have trouble sleeping well on a regular basis? (And yes, sleep deprivation can be considered an “exposure”; see chapters 5 and 9.)
 Do you live in an urban environment with air pollution or in a loud setting such as near a busy highway or airport?
Do you live in an urban environment with air pollution or in a loud setting such as near a busy highway or airport?
 Do you feel that you have a lot of stress and/or don’t respond well to stress?
Do you feel that you have a lot of stress and/or don’t respond well to stress?
 Do you buy a lot of prepackaged foods/meals rather than whole foods and fresh ingredients from which to create meals?
Do you buy a lot of prepackaged foods/meals rather than whole foods and fresh ingredients from which to create meals?
 Do you eat conventionally grown fruits and vegetables?
Do you eat conventionally grown fruits and vegetables?
 Do you drink tap water?
Do you drink tap water?
 Are you taking drugs that list weight gain as a potential side effect?
Are you taking drugs that list weight gain as a potential side effect?
 Do you clean your home with commercial, non-green products?
Do you clean your home with commercial, non-green products?
 Are you exposed to herbicides, pesticides, and fungicides around your home or neighborhood?
Are you exposed to herbicides, pesticides, and fungicides around your home or neighborhood?
 Do you use air fresheners or scented products (including cosmetics that list “fragrance” in their ingredients)?
Do you use air fresheners or scented products (including cosmetics that list “fragrance” in their ingredients)?
 Do you spend most of your days being inside, in a car, in an office?
Do you spend most of your days being inside, in a car, in an office?
 Do you sit more than three hours per day?
Do you sit more than three hours per day?
 As a child, did you drink a lot of juice, soda (regular or diet), and flavored milk or eat a lot of processed foods?
As a child, did you drink a lot of juice, soda (regular or diet), and flavored milk or eat a lot of processed foods?
 Did your mom smoke when she was pregnant, or were you exposed to secondhand smoke as a child?
Did your mom smoke when she was pregnant, or were you exposed to secondhand smoke as a child?
 Was your mom overweight or obese while she was pregnant with you?
Was your mom overweight or obese while she was pregnant with you?
 Was your dad obese before you were conceived?
Was your dad obese before you were conceived?
Don’t panic if you answered “yes” to any of these questions. Knowledge is power, and I will equip you with the information you need to take better charge of your waistline and health. In this chapter, we will take a tour of the obesity epidemic so you have a solid foundation to understand what I am calling “the new science of fat.” It will help you begin to see why some people gain weight faster and lose it more slowly than others, irrespective of diet and exercise.
THEN AND NOW: THE MYSTERY OF OUR MODERN SCOURGE
The image below shows two different individuals.
Back in our hunter-gatherer days more than ten thousand years ago, when we had to forage for our food by collecting wild plants, fishing, and pursuing wild animals, most of us resembled the individual on the left. Modern hunter-gatherers in Africa and elsewhere who continue to live this way still look like the woman on the left. However, many of us come closer to looking like the person on the right.

Some would argue that one of the reasons it is so easy to turn into the person on the right is that we evolved when food was much harder to find. We were programmed for survival in a world where food was scarce and periods of famine were frequent. But today we live in a calorie-rich environment 365 days a year. Food is abundant, and unhealthy foods tend to be the most affordable, available options. Many of these unhealthy foods are engineered to act on our brain’s pleasure centers to keep us addicted and coming back for more, similar to how drug addicts on heroin or crack cannot easily quit.15 While the theories around whether obesity-causing genes are widespread, or whether there is an obesity-favoring metabolic program, the idea that we have been molded by evolution to use calories sparingly makes some sense and is worth considering.
The “thrifty gene” hypothesis suggests that the two images here reflect an obvious mismatch between our Stone Age genes and space age circumstances. Having access to ample calories allowed the body to build fat stores quickly when food was available so it could endure long stretches of food shortages, which were inevitable and common throughout much of human evolution. Perhaps we retain essential components of this hunter-gatherer genome—after all, a small percentage of each of our genomes is derived from our Neanderthal and Denisovan cousins.16 These genes helped us store fat during times of abundance so that this fat could be used during those regular periods of scarcity, and thus they lead to energy being spent sparingly. The end of famine in developed countries means that accumulated changes in genes that were once favorable for storing fat instead could cause widespread obesity. In other words, “famine genes” that were once advantageous for survival became liabilities that could threaten health and longevity in the land of plenty.
Geneticist James Neel first described the “thrifty gene” hypothesis in 1962 to help explain why diabetes has such a strong genetic basis yet results in such negative effects.17 According to the theory, the genes that predispose someone to diabetes—the “thrifty genes”—were advantageous long ago. But once modern society changed and we developed agriculture, our access to food changed, too. Our bodies no longer needed those thrifty genes, but they were still active. Today they continue to prepare us for a famine that will not arrive. Our thrifty genes are partially responsible for the obesity epidemic, which is closely tied to the development of diabetes.
If there are such things as “thrifty genes,” then it must be possible to identify them with the advent of modern, affordable DNA-sequencing methods. This is where the thrifty gene hypothesis has run into some critics. If these thrifty genes have been around for the two hundred thousand years or so that we Homo sapiens have existed, and agriculture began only around twelve thousand years ago, then pretty much everyone should carry the majority of the thrifty genes that have ever existed. Dr. John Speakman, a prominent challenger of the thrifty gene hypothesis, showed in a 2016 paper that none of the common obesity-related genes that had been identified conferred any properties or traits that could be considered to have provided an adaptive advantage.18 On the other hand, perhaps there are bona fide thrifty genes that have yet to be identified, so the case is not yet closed. As we will discuss in chapter 5, it is clear that there is a “thrifty phenotype.” That is, in both human and animal studies, it is possible to identify individuals that store more of the calories they consume as fat, whereas others burn more calories or eliminate more in their feces. If thrifty genes are not responsible, then what is?
I am sure that you know people who can eat large volumes of food at meals yet remain remarkably lean. But consider this: They would not have lasted long in the Stone Age. These people we view as fortunate today have the opposite of a thrifty phenotype. The person who eats a sandwich and gains weight does so by retaining more of those calories. He will survive much longer under conditions of starvation due to the excess energy his body stored in the form of fat. This is only viewed as a negative today because instead of facing starvation, we live amid abundance (at least of calories) and can easily end up looking like the individual on the right here. In our culture, that is neither attractive nor healthy in the long term.
Every week I encounter skepticism about the biology of weight gain and loss. For decades, we have been told that our weight is a black-and-white reflection of the energy balance equation. If you take in more than you expend, you will gain weight; and if you burn more than you consume, you will lose weight. This rationale has always sounded so plausible and commonsensical. It is true to some extent when dieting. But the “calories in/calories out” model is obsolete. People want so badly to believe in this trivial explanation of metabolism, but if it were that simple and straightforward, then we would not be as overweight and obese as we are. As I posited earlier, why can we easily balance our financial but not our caloric checkbooks? Too much food and too little exercise does not fully account for the extent of our obesity. It fails to explain all the factors at work; it does not consider all of the contributing factors to obesity, including obesogens, which we will talk about in the following chapters.
Before I get to the conversation about obesity-causing chemicals, we should cover a few fundamental facts that need to be clarified.
A CALORIE IS NOT A CALORIE
Ask a group of people what a calorie is and most will tell you it is “the thing in food that makes me fat.” Well, not really. A calorie is a unit of heat energy, specifically the amount of heat required to raise the temperature of 1 gram of water 1 degree Celsius (about 1.8 degrees Fahrenheit). What we in the United States commonly call a calorie is, in fact, equal to 1,000 calories, or 1 kcal (as you will see on food packaging in Europe). Calories in food are measured using what is called a bomb calorimeter. Bomb calorimeters determine heats of combustion by igniting a sample in pure oxygen at high pressure in a sealed vessel and measuring the resulting rise in temperature. However, people—including many scientists and medical doctors—misunderstand that the human body is not like a bomb calorimeter.
The human body does not burn calories the same way a bomb calorimeter does. A calorie is a calorie only if you are trying to heat your house. You have probably heard that protein and carbohydrates give approximately the same amount of energy, about 4 kcal per gram, while fat provides 9 kcal per gram. Fats are more energy dense. But biologically speaking, proteins, carbohydrates, and fats are vastly different because each gets metabolized differently and affects us in separate ways. The way your body responds to your eating 100 calories of carbohydrates in the form of refined sugar (about 4 heaped teaspoons of the white stuff) will not be the same as if you consumed 100 calories of pure fat in the form of butter (about 1 tablespoon). You can even feel the difference in hunger cues and levels of satiety. Want an example? You can do an experiment yourself: one day, have a bowl of cereal with fresh fruit and nonfat milk and see how long you can go without feeling hungry and eating again. The next day, try an egg-plus-cheese breakfast that contains the same number of total calories as the cereal breakfast. The carb-heavy cereal breakfast will leave most people hungry within about ninety minutes. The fat-and protein-heavy egg-and-cheese plate will likely keep you satisfied for hours. Clearly, the body didn’t use—or experience—each breakfast in the same way, even though each contained the same amount of “energy.” Why?
A lot is going on when you eat. You are not just consuming food. Eating triggers a multitude of hormonal pathways in the body that impact how food gets processed, how your brain interprets satiety signals, and how you feel. Later in the book, we will go into all these details about how food affects the body and whether or not it leads to weight gain or loss. But for now, I want you to begin to change how you perceive calories.
If everyone used calories the same way, then you would never see a difference between person A and person B in their ability to maintain a certain weight with the same dietary intake and physical activity. Just balance the caloric checkbook and that’s that. But just as distinct foods trigger different processes within the body, each individual body does not process identical foods in the same way. Nutrition labels lead to a “one size fits all” mentality. The “calorie is a calorie” dogma assumes that everyone uses calories equally, which is far from the truth. Another way to quickly grasp the gap between how calories behave in a vacuum and how they affect a human body is to consider a 2015 study that challenged a lot of what we thought we knew about “healthy” food.
Eran Segal, Eran Elinav, and their colleagues at the Weizmann Institute of Science in Israel homed in on one key component often considered in designing balanced diet plans: the glycemic index, or GI for short.19 The GI was developed decades ago as a metric for how foods, particularly carbohydrate-containing foods, impact the amount of glucose in the blood. The GI uses a scale of 0 to 100, comparing foods with the reference point of pure glucose, which has a GI of 100. Foods with a high GI, such as potatoes, crackers, and white bread, are quickly digested and absorbed, causing rapid but transient elevations in blood sugar, which in turn trigger a spike in insulin, the hormone responsible for ushering glucose out of the bloodstream and into cells for use or storage. Insulin also stimulates fat and amino acid uptake into cells and inhibits the body from breaking down stored fat, glycogen, and proteins. Lower-GI foods such as whole grains, rice, black beans, and some starchy vegetables are digested more slowly, producing a gradual rise in blood sugar and insulin levels. Low-GI foods hardly change blood sugar levels at all.
GI values have long been assumed to be fixed numbers, intrinsic to the food itself. If this were the case, then everyone would respond to the same food in the same way. Segal and Elinav’s team conducted an elegant experiment to test whether this was the case or not. First, they recruited eight hundred healthy and prediabetic volunteers aged eighteen to seventy years and gathered data through health questionnaires, blood tests, body measurements, glucose monitoring, and stool samples. Using a mobile app, the participants recorded food intake and lifestyle information. Everyone was instructed to eat a standardized breakfast that included foods such as bread each morning.
Their study analyzed the responses of participants to a total of 46,898 meals.19 What they found shook the foundations of the diet field. As expected, age and body mass index appeared to impact blood sugar levels after meals. Surprisingly, people showed radically different responses to the same food! The GI of any given food was not a set value; rather, GI could differ depending on the individual. Person A, for instance, ate tomatoes and experienced an immediate spike in blood sugar levels, whereas person B ate the same tomatoes but did not experience an equivalent surge in blood sugar. The researchers concluded that customizing meal plans to personal biology may be the future of dieting,19 and I could not agree more. While the concept of personalized medicine is widely accepted with respect to how pharmaceutical drugs affect individuals differently, the same doctors who readily accept that people respond differently to the same drug are much less willing to believe that people can respond differently to the same diet. One size does not fit all. We will also see in chapter 5 that a widely underappreciated factor in how people respond to foods is their gut microbiome—the microbial communities that live in the stomach and intestines and play important roles in how we metabolize food and even whether we feel hungry or not.
No two metabolisms are identical. This is strikingly evident when you consider that about 20 percent of type 2 diabetics are of normal weight and that some people who are obese never develop metabolic diseases and obesity-related conditions such as high blood pressure and unfavorable cholesterol profiles.20 Therefore, while obesity and type 2 diabetes are not inextricably linked, most type 2 diabetics are obese, and most obese people are at risk for type 2 diabetes, among other conditions. But it is not so simple as obesity causes type 2 diabetes. Let’s consider some of the other myths swirling around obesity.
IT MUST BE GENETIC, RIGHT?
The next time you are in a public venue surrounded by lots of people, take a look around you and note the different body types. You will likely find that there are roughly three different, dominating patterns in how people are built physically. In the 1940s, the American psychologist William Sheldon and colleagues proposed that people could be grouped into three different body types (“somatotypes”), named after the three germ layers—the first major types of cells that are formed in the early embryo.21 The “ectomorph” tends to be thin and slight in stature; he or she does not appear to have a lot of muscle or fat (but according to Sheldon has a more developed nervous system). The “endomorph,” on the other hand, is the person who is described as rotund with more fat mass than well-defined muscle mass. The “mesomorph” is somewhere in the middle with an overall lean body and defined muscles.22 Sheldon went too far by assigning psychological characteristics to these physiques—the round endomorph being fun loving and the thin ectomorph being anxious and intense.22 This idea was about as reliable as attributing personality traits to the signs of the zodiac. Nevertheless, the popularity of the body type classification has remained, because like some stereotypes, it contains a kernel of truth: the somatotype designations recognize that a person’s propensity toward building muscle or storing fat is largely predetermined.23
This leads to an important question: How much of obesity is genetic? While the hereditary origins of obesity have long been assumed, a genetic contribution to obesity became evident only in the last two decades. Evidence from twins and animal studies once suggested that genetic factors account for 40 to 70 percent of the variation in BMI.24 But recent studies put this number much lower, at perhaps only 20 percent.25 Although several single genes are linked to obesity, there is no “obesity gene” or even a group of obesity genes that accounts for a major part of the obesity epidemic. Most geneticists believe that obesity is polygenic. That is, it would take changes in many genes (largely those associated with appetite and metabolism) to produce the obesity epidemic we are witnessing. But these kinds of changes could not possibly have happened worldwide over the past forty years. On the other hand, many people who carry these genetic variants linked to increased BMI are not obese; therefore, it is highly likely that other factors interact with any such genetic predispositions.26,27 One such factor is the environment, and we will see in a later chapter just how powerful environmental forces can be to change the expression of a variety of genes in your body—without making any changes in your personal genetic sequence. Not only can you be born with a tendency to gain weight easily due to environmental influences in utero, but the expression of your genes throughout your entire life can be changed by environmental factors that can make either weight gain or weight loss easy.
YOU MUST NOT BE EXERCISING ENOUGH
The prevailing wisdom, I call it “the couch potato syndrome,” is narrow-minded and largely wrong. Although it is commonly stated that we are more sedentary today than in years past, that is debatable—the facts don’t fully support this point of view. Just as there are studies showing less physical activity28 today than in generations past, there are other studies revealing that we are in fact more active today.5 By some reports, overall inactivity has dropped in recent years and participation in sports, fitness, and related physical activities has increased. When I think about my own life, I find that adults try to be more active today than the adults I knew growing up. I can’t recall that there were very many health clubs when I was young. Today, many people strive to stay fit and keep moving, which is reflected by the number of gyms, the popularity of online fitness programs, and the increasing number of fitness apps and fitness tracking devices (for instance, Fitbit and Jawbone). People are trying hard to get into shape.
No matter what your position on the value of exercise (and I think it is beneficial in very many ways), even inactivity coupled with poor diet cannot explain the magnitude of the obesity epidemic. In addition, exercise is linked to weight gain rather than weight loss in many studies. A provocative 2014 study showed that a substantial number of women who take up an exercise regimen wind up heavier afterward than they were at the start, with the weight gain due mostly to extra fat, not muscle.29 Although exactly why this happens is not completely clear, one of the reasons is likely to be physiological: when you exercise more, your appetite naturally increases.30 Feeling hungrier can cause you to crave carbohydrates to restore the glycogen depleted from your muscles, which could cause you to gravitate to unhealthy snack foods containing lots of refined sugars, fats, and salt. Counterintuitively, you might also move less at times when you are not exercising (perhaps because you are sore). For some people, especially those who are already obese, rigorous, challenging exercise can cause measurable and significant neural activity in brain regions responsible for food reward and craving.31,32 Such brain activity can make it nearly impossible to say no to, and not overindulge in, tasty snacks high in fat and sugar. Interestingly, studies investigating the brain activity of lean, fit people show their food-reward centers respond less aggressively to images of delectable foods33 (but more aggressively to low-calorie foods).34,35
Another explanation is psychological: when you know that you are burning more calories by exercising, you tend to give yourself greater permission to eat more. Ultimately, this could make you overcompensate for the number of calories lost through physical activity.
To be sure, exercise serves an important role in your overall health. Although you can’t rely on exercise alone to promote weight loss or as the ultimate antidote to weight gain, physical activity is useful in reducing the risk of developing heart disease, diabetes, dementia, and many other conditions.
YOU EAT TOO MUCH, DUMMY
Diet trends come and go. Sometimes, low-fat is all the rage; other times, it’s low-carb, Paleo, or Atkins-type diets. There is no doubt many of us consume too many carbohydrates, especially in the refined, sugary form. This was a natural consequence of the “war against dietary fat” that began with the McGovern Report, which first established Dietary Goals for the United States, published in 1977.36 Unfortunately, since fat often helps to make food tasty, a substitute ingredient was needed, so—you guessed it—sugar was added to food to replace the tasty fats. Take a walk down the candy aisle in any supermarket and count how many types of candy say they are low-fat or zero-fat foods, implying that they are therefore healthy. We also gravitate toward salty, fatty foods with added sugars that provide little nutritional value, titillate our taste buds, and apparently increase food consumption.37 But even these dietary shortcomings do not explain our weight problems. If they did, then focusing on nutrient-dense foods and steering clear of classic fattening foods such as fried chicken and doughnuts would cinch our waistlines. Adhering to the strictest, “best” diet does not necessarily guarantee that the weight will melt away and you will stay lean for life.
Is there another explanation for people who eat well and cannot lose weight? Just look at the example of obese people who have fought the good fight and lost hundreds of pounds. Why do more than 83 percent of these people who have worked and sweated to lose large amounts of weight gain it back within a few years?38,39 How does the weight loss industry—comprising diet companies, nutritionists, supplement manufacturers, pharmaceutical giants, diet book authors, fitness trainers, lifestyle experts, “detox” juice bars, obesity doctors, and gastric surgeons—rake in multiple billions every year without offering a bulletproof cure?
My answer, in short, is: obesogens. Clearly, other factors play into the risk for obesity, such as chronic sleep disruption and stress, but we will get to these other fat-inducing factors later in the book. For now, we are going to focus chiefly on the growing body of evidence pointing to environmental substances called obesogens as additional, under-acknowledged factors that alter metabolism and predispose some individuals to weight gain.
THE OBESOGEN HYPOTHESIS
In 2002, Dr. Paula Baillie-Hamilton of the United Kingdom wrote the first article relating environmental chemicals to obesity. She had a pet theory: exposure to toxic chemicals was preventing her from losing weight after having four children. Her article, “Chemical Toxins: A Hypothesis to Explain the Global Obesity Epidemic,” was a review of published toxicological studies dating as far back as the 1970s.40 Baillie-Hamilton showed a correlation between the rise in chemical manufacturing after World War II and the rise in obesity, claimed that chemicals caused obesity, and declared that purging the chemicals would reverse the process. However, her most important contribution went unnoticed by most readers. This was that exposure to high doses of a variety of environmental chemicals, including some pesticides, solvents, plastics, flame retardants, and heavy metals, was shown in some studies to lead to weight loss, whereas animals exposed to low doses of the same chemicals gained weight. This seemingly small yet significant fact was ignored because the toxicologists who conducted these studies typically were concerned only with weight loss—a prime indicator of toxicity. Moreover, the idea that a chemical could have one effect (weight gain) at a low dose and the opposite effect (weight loss) at a high dose did not fit with the orthodox “dose makes the poison, toxicity is linear” worldview of many toxicologists. Baillie-Hamilton’s work went largely unnoticed because it was published in an obscure place, the Journal of Alternative and Complementary Medicine, which is not read much by researchers.
Another reason Baillie-Hamilton’s work did not receive much attention was that she had detected only a correlation between chemicals and obesity and was overselling the story. You can correlate many things with the increase in obesity. In my talks, I sometimes humorously point out a number of absurd correlations between the rise in obesity and other factors. These include such things as the number of gyms/health clubs (which, as I mentioned earlier, have doubled in step with the doubling of obesity in the United States), the number of SUVs on U.S. highways, or even the number of dermatologists. While it can be entertaining to link two seemingly unrelated phenomena just because you can, correlation is not causation. Gyms, driving an SUV, and dermatologists probably do not cause obesity. Many, if not most, correlations are entirely coincidental. As scientists, it is our job to identify causation, not just correlations.
One person who did notice Baillie-Hamilton’s paper was Jerrold (Jerry) Heindel at the National Institute of Environmental Health Sciences (NIEHS). Jerry was a program officer—an agency official who is responsible for managing a portfolio of grants to ensure that the research being funded fits the mission of the agency, in this case to understand how the environment (broadly defined) influences health. Upon reading the Baillie-Hamilton article, Jerry made the intellectual leap that it was not all toxic chemicals per se that were responsible for obesity, but rather endocrine disrupting chemicals (EDCs), which are chemicals that can interfere with how hormones work in our bodies (much more on this later). He then set out to drum up interest in this new field among scientists already working on EDCs. Jerry wrote an influential article, “Endocrine Disruptors and the Obesity Epidemic,” which appeared in a mainstream journal, Toxicological Sciences, in 2003, placing endocrine disruptors and obesity on the same map for the first time.41 He is too modest to admit it, but Jerry is really the father of the environmental obesogen hypothesis. I often jokingly tell waitresses that he is my dad when we travel to meetings around the world. Sadly, Jerry retired from NIEHS at the end of 2016. The community of researchers working on EDCs will greatly miss his infectious optimism and influence and his propensity for calling BS on any conclusions not strongly supported by high-quality data. Jerry had a very strong, positive influence on the field that was unique among NIH program officers.
In 2006, my team and I published our now classic paper identifying tributyltin (TBT) as an environmental chemical that leads to fat cell development and weight gain.42 TBT is a chemical (specifically, an organotin) that kills fungi and was once widely used in antifouling paints on ship hulls but continues to be found in seafood and can be found as a contaminant in vinyl plastics. We coined the term “obesogen” to describe these fattening chemicals. Obesogen exposure changes how energy is stored and used in the body to favor weight gain and obesity. We proposed that obesogens can act directly on the fat to produce more fat cells, larger fat cells, or more cells that are destined to become fat cells. We suggested that obesogens can also derail the normal processes that the body uses to maintain weight, regulate appetite, and control metabolism, causing exposed individuals to be increasingly susceptible to weight gain despite normal diet and exercise. Work in my lab and in other labs around the world has shown all of these mechanisms to be at play.7 Limiting exposure to obesogens is not just about reducing risk for overweight and obesity. Reducing exposure to endocrine disrupting chemical obesogens will reduce your risk for various illnesses—from heart disease to cancer43,44 and even dementia.45 In upcoming chapters, you will gain an understanding of these mechanisms together with some insights into how you can avoid more damaging effects from fat-inducing chemicals.
WHERE DO OBESOGENS LURK?
To be sure, not all EDCs are obesogens, and not all obesogens are the kinds of nasty toxic chemicals we think about, such as those from a smoke-belching factory exhaust pipe. Obesogens can come from sources such as food (including fruits, vegetables, and your favorite homemade comfort foods), beverages (including water), pharmaceuticals, and everyday household items we use routinely, such as personal care products, cosmetics, sunscreens, shower curtains, air fresheners, mattresses, clothing, kitchen tools and plastic storage containers, canned goods, toys, furniture, flooring, and cleaning supplies. We have currently identified about fifty potential obesogens,7 but there has been no systematic attempt to identify obesogens, and there are more than one thousand known EDCs (despite no systematic program to identify them either). Therefore, I expect that more research will discover hundreds of new obesogens. Following is a general list of known obesogens to date:
Chemical pesticides: Commonly used pesticides in conventional farming, especially the breakdown product of DDT (DDE), have been definitively linked to increased BMI in children.46-48 In laboratory settings, they cause rodents to become resistant to insulin, which can lead to diabetes. While DDT is banned in most of the world (but is still used in many parts of Africa), other obesogenic pesticides exist and are present in conventionally grown produce and can contaminate tap water.
BPA: Found in plastic bottles, can linings, medical devices, and cash register receipts, bisphenol A (BPA) has been shown to cause fatty liver as well as increased abdominal fat and glucose intolerance in animals.49 Early studies show that replacement chemicals such as BPF and BPS have the same activity as BPA.
PFOA: Perfluorooctanoic acid (PFOA) is used in nonstick coatings such as Teflon, food packaging (microwave popcorn bags), backpacks and luggage, carpeting, and clothing and has even been found in water.50 Studies are still under way, but the current thinking is that such chemicals are obesogens, among their many other detrimental effects.
Phthalates: Phthalates are ubiquitous—they are found in plastic and vinyl, including medical devices and tubing, toys, wall paint, air fresheners, as well as in numerous beauty and personal care products. Some phthalates have been classified as carcinogens and have been shown to be obesogenic in animal studies and linked with obesity in humans.7
TBT: My laboratory favorite obesogen, tributyltin (TBT), is a powerful fungicide and bactericide that was once widely used in antifouling paints on ship hulls. TBT still contaminates seafood and can be found in vinyl plastics as an unintended contaminant of other organotins used as heat stabilizers and as a wood preservative.42
PCBs: Polychlorinated biphenyl chemicals were once used as electrical insulators and flame retardants until they were banned in 1979. But they still persist in the environment, and exposures typically come from contaminated fish, meat, and dairy products.47,48 PCBs are obesogens and are also known to cause diabetes.
PBDEs: Polybrominated diphenyl ethers are flame retardants found in a lot of furniture, particularly foam. They are also found in cars, electronics, building materials, plastic foams, and textiles. Many have been banned, but others are still in use. PBDE replacements such as triphenylphosphate and tetrabromo bisphenol A are also obesogens.7
Soy: A common feed for livestock, soy contains high levels of phytoestrogens, many of which can be obesogenic when consumed by infants or children. Perinatal exposure to most types of estrogens, including soy, can promote the growth of fat cells and obesity later in life.51
MSG: Used to make foods taste better, monosodium glutamate (MSG) first made the news as the suspect in “Chinese restaurant syndrome,” which in sensitive people can cause flushing, headaches, tachycardia (rapid heartbeat), and excessive sweating. Most people lack this sensitivity to MSG, but it is also an obesogen that is found in many canned and packaged foods, soups, and a variety of restaurant foods.52
HFCS: You likely already know that high-fructose corn syrup (HFCS), a refined sugar, is not the same as real sugar. We will be going into detail about why sugar is so obesogenic. The conversation about sugar can be complex, and much has been written about it (see the works of Robert Lustig and Gary Taubes, among others). Added sugar, natural or otherwise, is often considered to be “toxic” now, but what does that mean? And what is the difference between glucose, which serves as fuel in the body, and fructose, which is processed almost entirely by the liver, where it is stored as triglycerides? In 2014, a study by Michael Goran and his colleagues at the Childhood Obesity Research Center at the Keck School of Medicine of USC found that the levels of fructose in many popular beverages and juices were much higher than expected, so high that they could increase one’s risk not just for obesity, but also for diabetes, cardiovascular disease, and liver disease.53 They went on to show that fructose levels in breast milk were positively associated with body fat in infants.54
Artificial sweeteners: Swapping your regular soda for diet will not make you thin. The same goes for diet and low-fat foods that are filled with artificial sweeteners. Even ones marketed as “natural” can be problematic. When we cover the microbiome, you will see what these chemicals do to the gut bacteria, which in turn adversely affects your metabolism.
Nicotine: The main chemical found in cigarette smoke encourages obesity in the children of mothers who smoked when they were pregnant. In fact, one of the first connections made between obesity and human fetal development came from studies of exposure to nicotine in utero. Smoking has decreased over the past generation, but nicotine by-products can still be found in the blood of nonsmokers, attributable to secondhand smoke. More on this later.
Air pollutants: Many chemicals found in polluted air, especially in urban environments, are obesogens. See chapter 9 for more details.
Parabens: These are a class of obesogens known to disrupt hormones by mimicking estrogen. They are used as preservatives in many personal care and beauty products such as cosmetics, lotions, and hair products.
Two questions that scientists have been trying to answer are: (1) How much does obesogen exposure contribute to the obesity epidemic? And (2) What is its cost to society? My colleague Professor Leo Trasande from NYU is a specialist at such calculations. Leo is a pediatric epidemiologist who has led several teams of experts in brainstorming exercises intended to estimate the cost of EDC exposure in particular to the disease burden in the United States and in the European Union.55,56 These efforts used very conservative estimates for how certain we were about exposure-disease linkages, the quality of the evidence, the types of studies they were based on, and so forth. The numbers are sobering: €23.9 billion in the EU and $5.9 billion in the U.S. for exposure to only three obesogens (bisphenol A, diethylhexyl phthalate, and the pesticide DDT) per year. These were the only obesogens (out of at least fifty known chemical obesogens) for which sufficient data were available to make the calculations. Therefore the actual economic impact of obesogens is probably much higher.
The hardest fact to accept is that it can be very difficult, if not impossible, to lose weight permanently, due at least in part to the effects these chemicals have on the body. Unlike a computer program that can be debugged, human programming does not work like that. Our bodies are self-regulating for the most part (temperature, blood pressure, hormonal cycles, and the like), and the biological control mechanisms for these can be thought of as a type of “programming.” I am amused and also somewhat frustrated when I see diet books claiming that their protocol can help you to “reprogram” or “rewire” your fat cells and “make over” your metabolism. In reality, those are very difficult goals to achieve—especially in the continual presence of obesogens. These chemicals are reprogramming the body in ways that are not easily reversible. But with knowledge and strategy, it is possible to protect yourself and your family, particularly your young children, from exposure. We will start by establishing a solid understanding of how obesogens can program the body to store more of the calories you consume as fat and contribute to weight gain that is difficult to overcome.