It’s a sunny June morning in Berlin’s Schöneberg district as I walk down a shady sidewalk with two young men, Andrei and Georgi. Although the 19-year-olds arrived from Romania just a few months earlier, they had visited Germany many times before. They’re dressed to impress: Andrei’s jeans are fastened in place by a flashy silver belt buckle with the Dolce & Gabbana logo, complemented by black Puma sneakers and a fitted blue T-shirt. As he walks, he nonchalantly eats breakfast, a small package of cookies from the gas station. Georgi is dressed in similar fashion: a sequined Ed Hardy print T-shirt, his spiky gelled black hair in need of a trim. They’re full of “swag”—an English term popular among young Berliners—which seems to belie their current activity: picking up discarded cigarette butts. As we walk, Georgi bends over to collect the butts, which he hands to Andrei. Every four or five steps, he bends over or squats to the ground. They have a system in place: bend, pick up, hand over, walk, bend, pick up, hand over. It takes a keen eye to distinguish which are worth picking up, those that have enough white left behind the brown filter, but they have a good pace going. Before an afternoon nap, they tear open the thin paper and mix the tobacco with a small chunk of hashish. It’s a Friday, so they get some rest before heading to the bars and working until early the next morning.
Andrei and Georgi are part of the growing phenomenon of migrant male sex workers (MSWs) in German cities, a population that remains underexplored by social scientists, despite a long history of male sex work as part of the nation’s erotic landscape (Evans, 2003).1 In this chapter, I argue that this increase in migrant MSWs is a response to the complementary but contradictory appearance of economic opportunities (freedom of movement across European Union [EU] borders) and constraints (transitional measures restricting migrants’ access to the labor market). A major focus of this chapter is the primary health concerns faced by this population, moving beyond the myopic association between sex work and HIV to contextualize health risks as a result of macro-level processes, including poverty, discrimination, unemployment, lack of housing, inadequate health-care access, and removal from kin support structures through migration. Especially troubling is their lack of access to medical services, reflecting a socio-legal position that resembles that of unauthorized migrants rather than EU citizens. To encourage and maintain the availability of appropriate services for MSWs, it is important to add to the sparse literature on their health status and use of health services.

FIGURE 16.1
Still from the award-winning German film Rentboys (Die Jungs vom Bahnhof Zoo), which describes the lives of male sex workers in Berlin.
The lives of MSWs in Berlin are the subject of the award-winning 2011 film Rent Boys (German title: Die Jungs von Bahnhof Zoo) by director and prominent gay rights activist Rosa von Praunheim. A Berlin organization working with this population reported that the film provides a “relatable picture of life in prostitution and illustrates the experiences of familial, societal, and sexual violence that the boys have traversed,” as well as “exploitation because of inequality, racism, and poverty” (Subway, 2012).2 Rent Boys focuses on three young Roma migrants who take up sex work in Germany to escape poverty in their native Romania. The filmmakers follow one of the men, Lionel, back to his home village, where it becomes obvious that migration into sex work is a common, but hushed, strategy adopted by local youth.
Indeed, only in recent years have scholars begun to turn their attention to the largely invisible population of migrants who sell sex in a number of host country settings (Agustin, 2006). Contrary to many assumptions, there is a significant demand for male sex workers (Dennis, 2008). However, the men and boys in the global sex trade are almost completely ignored by social service agencies, administrative bodies, the media, and in scholarship. This is matched by “a silence in the literature on how men who are structurally disadvantaged in the global political economy—as gendered beings who are situated within multiple social hierarchies related to race, class, masculinity, and sexuality—are implicated in the patterns of ‘structural violence’ that shape the HIV/AIDS epidemic” (Padilla, 2007, p. xii). Examining structural violence provides an analytic tool for understanding how health and disease are impacted by social inequalities and how political economic systems put particular individuals or groups in situations of extreme vulnerability. The concept of structural vulnerability can extend this analysis to an examination of how a host of mutually reinforcing economic, political, cultural, and psychodynamic insults that dispose individuals and communities toward ill health are embodied (Quesada, Hart, & Bourgois, 2011). MSWs face a lack of economic options, live in precarious social situations, and encounter structures of dependency that may lead them to engage in risky practices associated with the transmission of HIV and other sexually transmitted infections (STIs). In much of the existing literature, MSWs are assigned considerably more agency than females, thus framing them as active risk-takers and negating the importance of constrained opportunity (Dennis, 2008). Indeed, despite impressive documentation of associations between structural forces and the prevalent burden of illness, public health interventions continue to focus primarily on changing the micro-behaviors of individuals through educational interventions and models of rational decision making. Furthermore, prevention efforts for this population have been insufficient because specific risks differ from those for female sex workers and require tailored interventions (Allman & Myers, 1999).
This chapter first explores the role of migration as it relates to male sex work, before turning to a description of the German case in particular. Unique to the German situation is not only the fact that prostitution is a legal activity but that these migrant MSWs are not “illegal” because they are EU citizens. However, while permitted to travel across borders, at the time of this study, most were not yet authorized to work in Germany because of transitional measures curbing access to national labor markets. After considering why these young men migrate away from their home countries, including social marginalization and a lack of economic opportunities, I describe their life in a large city, in this case Berlin. The chapter then turns to major health concerns, using a structural vulnerability framework and arguing for a more holistic understanding of the health needs of Germany’s migrant MSWs.
Background: Male Sex Work and Migration
Sex work is defined as any occupation where an individual is hired to provide sexual services in exchange for money and/or other items of value (Minichiello et al., 2001). This characterization views sexual labor as a legitimate means of employment; however, at the same time, it does not preclude the very real occurrence of exploitation. It underscores the need to understand prostitution as labor, rather than making assumptions about individual pathology (Parsons, 2005) or overestimating the role of human trafficking (Agustin, 2006).
Male and transgender sex work remains underresearched, even in the commercial sex literature, where the bulk of scholarship remains focused on the experiences of women. This is due in part to the multiple marginalities MSWs experience and a lack of solid theoretical frameworks. Men are involved in intimate sexual labor within an increasingly global or transnational context, even though intimacy is far more often attributed to the physical and emotional labor of women (Constable, 2009). With prostitution often discursively constituted as “women’s work,” the lack of attention to the risks MSWs face reinforces the very dualism that many feminists would wish to challenge, since it reproduces preexisting heteronormative assumptions about gender in which women are “naturally” sexual objects. Thus, work on MSWs strongly challenges prevailing gender logic (Smith, 2011). Similarly, in contrast to research on women, research on male sex workers often focuses on sexual orientation; by contrast, female sex workers are rarely asked in studies if they enjoy heterosexual activity. This points to a need for more nuanced discussions on scholarly preconceptions about male and female bodies and the possibilities of same-sex desire.
Another reason for the lack of attention given to men and boys may be the belief that they constitute a negligible proportion of sex workers; “many authors reason that most clients are men, straight men outnumber gay men, and surely only gay men patronize male sex workers” (Dennis, 2008, p. 13). Thus, heteronormative definitions of “male” dominate the literature, especially as it pertains to those who purchase sex, and that when males purchase sex from other males, it cannot be linked to oppression. MSWs often are presented as “active, agentive, capitalizing on their talents, running their own business, never coerced, never degraded” (p. 19). While this may be the case for some high-salaried sex workers, most enter the field because of a lack of other options; many also report having experienced abusive childhoods, no opportunity to acquire legitimate marketable skills, and life on the streets.
Male sex workers are a heterogeneous group with diverse experiences, motivations, and identities. A clear distinction can be made between professional and nonprofessional (“street”) sex workers. Professional MSWs (also referred to as escorts or call boys, and who often solicit over the Internet) tend to be more financially secure, independent, and able to be more selective about clients and the types of sexual activities in which they engage. By contrast, nonprofessional sex workers—the focus of this chapter—largely enter this work because of poverty or poor social circumstances. Their environment is characterized by informality, dependency, and financial insecurity. Venue has a clear effect on power and control in sex work interactions, and thus has a direct impact on health and risk behavior (Parsons, 2005; Wright, 2003). While used throughout the literature, “street based” can be a misleading term, since solicitation typically occurs in bars, clubs, casinos, train stations, parks, and inside or in front of sex cinemas. In Germany, migrants dominate these sites because of their structural position as nonprofessional sex workers in addition to language barriers and a resultant inability to find and negotiate with clients over the Internet (although this is changing). Unlike professionalized escort services, street-based sex work is usually a temporary strategy characterized by a shifting set of people and locations. The dynamic features that make these men vulnerable also create significant barriers to social work and public health efforts, including a lack of monitoring data (Wright, 2012).
Migrants selling sex have been long neglected, even within migration studies, resulting in an entire category of labor migration that has been “discursively shunted—or perhaps tidied away” (Agustin, 2006, p. 29). Studies on male, transsexual, and transgender migrants who sell sex are even further marginalized, in part because of the emphasis on trafficking, which is largely viewed as happening only to women. As noted above, male sex workers generally do not fit the portrait of victimization and thus are not targeted by nor eligible for most programs.
Male Sex Workers in Germany
Male sex work has long been an integral part of the sexual topography in Germany. Using police surveillance records, court documents, and social service reports, Evans (2003) explores transgressive sexuality in postwar Berlin, describing men and youths risking incarceration under Germany’s slow-to-be-reformed, Nazi-era anti-sodomy legislation. The Bahnhof (train station) in particular became the primary site and symbol of male sex workers in Germany. Especially in Berlin, long divided administratively and sandwiched between two countries, the Bahnhof was thus a potent symbol of political transgression, debates over policing, social welfare, and criminality, as well as the site of much of the city’s clandestine sex trade (Evans, 2003). Red-light districts in Hamburg and public sites in cities like Bonn and Frankfurt have provided spaces for male prostitution since the 1950s (Whisnant, 2006). “Bahnhof boys” were a paradox for social service professionals in the postwar years, as they were viewed as both victims of and contributors to community instability. Hustlers attracted attention in the first half of the 1950s because they combined and concentrated many concerns that were central to public debates in the early Federal Republic: crime, prostitution, homosexuality, youth, and the dangers of the public sphere (Evans, 2003). A number of studies published on male prostitution in this period suggest a pattern of involvement of men between age 16 and 23 of working-class origin, who came from difficult family situations, a lack of economic opportunities, and involvement with other criminal activities (Whisnant, 2006).
Up to 90 percent of MSWs in Germany currently are migrants (KISS, 2012), up from an estimated 55 percent in 2007 (Gille, 2007). The specific needs of migrant sex workers from Central and Eastern Europe have been noted for some years (European Network on Male Prostitution, 2003; Wright, 2003). The current majority is overwhelmingly from Bulgaria and Romania, which joined the EU in 2007, partly explaining the timing of the increase. In previous years the majority was from Poland and the Czech Republic, following these countries’ entry to the EU in 2004. Inclusion in the EU has meant increased opportunities to travel, which is especially attractive to those crossing borders in search of work. The increase in migrant MSWs in Germany must be viewed as a response to both economic opportunities and constraints, as noted earlier. Both countries of origin for the migrants discussed here—Bulgaria and Romania—have considerably poorer standards of living than neighboring member states, leading to continued outmigration. In addition, both have a large number of socially and economically marginalized citizens of Roma ethnicity, who, as a result of the recent enlargement of the EU, are now Europe’s largest and poorest ethnic minority. Thus, migration and willingness to engage in sex work should be understood as a reflection of social exclusion and poor economic conditions within the framework of a transnational political economy.
Thus, unique to the German situation is not only the fact that prostitution is a legal activity but that these migrant MSWs are not “illegal” because they are EU citizens. Nonetheless, while permitted to travel freely throughout the EU, at the time of this study most individuals from the new member states were not yet authorized to work in Germany because of transitional measures curbing access to national labor markets until 2014. Individual governments of countries already part of the EU, including Germany, were given the option to apply restrictions to workers from Bulgaria and Romania for up to seven years. As a result, these new EU citizens faced many everyday forms of exclusion, including unemployment, unequal relationships in the housing market, and difficulty accessing medical care. If they are no longer participating in the health insurance schemes of their home countries, they are ineligible for the European Health Insurance Card, which provides coverage in other member states. Migrant participation in home country health insurance is notably uneven, even though the coordination of social security schemes is part of the EU enlargement process. Evidence from daily practice suggests that it can be difficult to maintain insurance enrollment because of the financial burden and/or bureaucratic constraints, and this has resulted in noticeable health disparities among many migrants from the new EU member states living in Germany (Castañeda, 2011).
Notably, the recent influx of migrants to German cities has resulted in heightened competition among street sex workers in places like Frankfurt, where clients have reported being approached by up to eight boys at a time (Fiedler, 2011). This has resulted in lower prices, with many sex workers earning only 200-350 euros a month (US$260-$460). This has created antagonism between migrants and German sex workers, as evident from the following postings in an online forum: “Over here there are a lot of Romanians that have ruined business. They offer a cheap screw and ruin everything for us. I don’t have a problem with foreigners … but that is some real damage they are creating. A screw for five or ten euros, I wouldn’t do that and neither would anyone else.”
The Impetus to Migrate: Social Marginalization, Economic Constraints
It is implicitly understood and sometimes explicitly noted that most migrant MSWs in Germany today are of Roma ethnicity (KISS, 2012; Marikas, 2012; Subway, 2012; Unger & Gangarova, 2011). This is similar to other reports from NGOs across Europe (Gille, 2007). However, very few data reflect this trend. Germany does not collect “ethnic” data in official statistics, due to discomfort in dealing with these categories and strict privacy protection laws. Germany’s Federal Data Protection Act was one of the first of its kind and it continues to provide some of the highest levels of identity protection in Europe. This can be “readily accounted for by its past, and by suspicion concerning potential misuse of personal data, particularly by the state” (Simon, 2007, p. 56); thus the statistics collected on groups likely to face discrimination is a sensitive issue. There is an understanding that, if racial or ethnic stereotypes are the product of racism, then the use of such categories is likely to reinforce discrimination and create visible divisions, which works against integration efforts. In Germany, “there is no public debate on the statistics, which are discussed only by some NGOs and scientific experts. The organisations which represent ethnic minorities are generally very reluctant to tackle the question, an example being the Roma organisations, which are suspicious … of the use to which statistics may be put” (Simon, 2007, p. 57). As a result, to avoid contributing to the stigma of already marginalized groups, most organizations serving migrant MSWs do not collect data on ethnicity. On the other hand, it is also understood that they migrated away from their home countries precisely because of ethnic marginalization. The result is an implicitly understood target group, without sufficient information about exactly who is included. While understandable, given Germany’s recent history, this lack of data may also result in a lack of accounting for actual patterns of de facto racial or ethnic discrimination.
How do these young men self-identify? When asked, a minority identify as Rom or Roma, or use descriptors such as Zigeuner (gypsy) or Romanian gypsy, but most embrace a national identity and simply identify as Romanian or Bulgarian. Because of their ethnic minority background, many Bulgarian Roma speak a variant of Turkish and thus often describe themselves as Turkish or of mixed Bulgarian, Turkish, and/or Roma ethnicity. Indeed, being considered Turkish in some parts of Germany gives them benefits in the social hierarchy of immigrants in which Turks have ascended to become the “model minority” and are considered highly entrepreneurial and active in local politics. As one 18-year-old told me, “Pretending to be Turkish makes you not as obvious in Berlin.” By contrast, Roma face the same negative stereotypes in Germany that they do in their home countries. This flexible practice of self-identification—pretending to be Turkish—is an example of how marginalized groups can actively use and control local ethnic/national hierarchies in transnational settings.
By all accounts, these young men are between 17 and 30, with an average age of 21. Most are from the same regions of Bulgaria and Romania and know one other, often working alongside cousins and friends. Many migrate back and forth to their home country, where they may have a wife and children, or they bring their wives and children to Germany. Some report spending several months at a time in other countries (e.g., Italy, Spain, or France), and their family members may be spread out across Europe. One social worker described a village in northeastern Romania where poverty is extremely high and almost all the young men have left for sex work in Germany. He noted, “There is no concept of a ‘career’ as a hustler; it is not their career goal.” Rather, it is viewed as a temporary move before finding a job in another industry, such as construction. However, the transitional measures restricting employment, coupled with a lack of education and job skills, means that work opportunities for these men are largely out of reach. Upon arriving in Germany, they remain relatively isolated, rarely leaving the neighborhoods in which they live or work. Most are unfamiliar with the city and its geography, making it difficult to register officially or interact with authorities; they often pay unscrupulous brokers several hundred euros to help them with these tasks. Living conditions are often extremely poor; as many as ten young men may share an illegally sublet room. Some are illiterate and most have limited German skills, even though they are multilingual, having grown up speaking Turkish or Romanes at home and Bulgarian or Romanian in other settings.
Motivations to migrate often include a quest for “a little bit big money” to pay for a modest used car or begin construction on a house in Romania, or just to get a little spending money for needs and desires beyond daily sustenance (Gille, 2007). The wish to buy or construct a house in the home country is common and implies independence, and being able to provide an economic buffer for the family. However, they may have multiple goals or their goals may shift over time, and many young men adopt a new identity and habits of consumption in Germany in order to adapt to their lifestyle. These include a distinctly globalized social construction of masculinity and incorporating a range of imported fashions, identities, behaviors (Padilla, 2007). As described in the opening vignette, “swag”—propelled into the lexicon of contemporary German through pop culture and designated 2011 “word of the year” by dictionary company Langenscheidt—is adopted in attitude and clothing styles. However, swag and designer clothes, as I note, contrast markedly with simultaneous experiences of real deprivation, such as the collection of used cigarette butts and homelessness. While many young men are driven into sex work because of poverty, they rarely accumulate or remit money, often spending any earnings immediately. A popular way to spend money is on apps for mobile phones or gambling on tabletop slot machines. There has been an explosion of casinos and gaming halls in the past several years, especially in heavily migrant districts of Berlin such as Wedding and Neukölln. Interestingly, the young MSWs say they never played these machines in their home countries, only in Berlin. “For them, it is dirty money, so when they make money from sex, they spend it immediately. They are addicted to gambling or drugs, or they buy new clothes, so the next day they have nothing and have to go back to work” (Dowling, 2011).
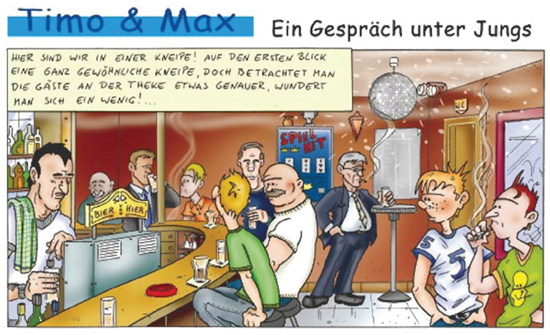
FIGURE 16.2
“A conversation among boys”: Comic strip created by the German male sex work support organization LOOKS eV.
While this group may appear to have few advocates, nonprofit organizations in several major cities provide assistance specifically to MSWs. While not united over the terminology used to describe their clientele, many employ the German term Jungs (boys or guys) to avoid the stigma attached to the Stricher (hustler) label, which has an explicitly sexual connotation. Jungs is a more neutral and “generally recognized term” in the scene (Subway, 2012) and sometimes is used as a self-descriptor (LOOKS, 2012). Other organizations use Stricher precisely because of its precision and everyday use, or simply refer to the clientele as male prostitutes. The increasing number of MSWs from Bulgaria and Romania has presented new challenges for these organizations, which were not initially focused on migrants (KISS, 2012; LOOKS, 2012; Marikas, 2012; Unger & Gangarova, 2011). Most of these projects started in the early to mid-1990s and remain largely funded by municipal HIV prevention monies (Wright, 2003). They offer a combination of drop-in center and street work outreach. According to reports from 2011, drop-in centers in each city served between 200 and 500 sex workers annually, an increase over previous years. In the drop-in centers, clients can eat, wash clothes, shower, shave, use Wi-Fi, relax, play games, and store belongings. Most also offer sleeping accommodations during the day, as many of the young men are homeless and generally are excluded from traditional shelters because of their migrant status, or they avoid them because they feel they are hostile settings. Social work consultations—when possible, in the client’s native tongue—provide advice on work-related concerns, illness prevention and health, dealing with government offices, housing, sexual identity, mental health, family relationships, debt, and getting out of prostitution. Finally, most of these organizations also provide weekly medical consultations (discussed in more detail below) in conjunction with the local health department or volunteer physicians.
Regular street work outreach is important because the street hustling scene shifts often and “no collective consciousness has emerged” (KISS, 2012, p. 13), which is unlike many other subcultures. Outreach workers’ activities consist of visiting cruising areas at night to inform sex workers about services, and to distribute health information, condoms, and lubricants. Outreach also involves one-on-one conversations as well as more sophisticated tools, such as a Bluetooth application to distribute health information to mobile phones. Bar and club owners and their staff are generally supportive of outreach efforts, and many agree to post information or keep free condoms available for those who ask. Novel prevention efforts to emerge in recent years include Internet chats, peer health promoters, and community mapping activities that allow men to exchange experiences and locate social and health services (Unger & Gangarova, 2011). However, outreach has been negatively impacted by the introduction of restricted areas that prohibit public prostitution in certain locations outside of designated red-light districts or “toleration zones.” The implementation of restricted areas that encompass entire cities has consequences for prevention and outreach efforts, since prostitution continues in these cities in hidden locations. This worsens the situation for nonprofessional MSWs, as they face risks associated with law enforcement, have less power to negotiate with clients, and become more difficult for outreach workers to locate (Unger & Gangarova, 2011).
Studying the Health of Male Sex Workers
While the earliest studies on male sex workers were underpinned by deviancy discourses, the HIV/AIDS epidemic heralded a new era and tone in research. Studies have since focused on behavior and practices to minimize the spread of STIs and called for more comprehensive social and health services. A recent national progress report on HIV conservatively estimates its prevalence among MSWs in Germany at 5 percent to 10 percent (UNAIDS, 2012). Other studies focused on this population have found higher rates, ranging from 27 percent prevalence of STIs and 15 percent of HIV (Wright, 2001) to an overall STI rate of 24 percent to 33 percent (Steffan & Sokolowski, 2008). While new HIV infections in Germany have declined over the years, an estimated 75 percent of syphilis cases are among men who have sex with men, and up to 50 percent of these men are considered likely to be HIV positive (Marcus, Bremer, & Hamouda, 2004). Research findings overall suggest very good knowledge of transmission risks among the German population of men who have sex with men. However, more risky behaviors have been reported with the advent of highly active antiretroviral therapy, along with a trend toward having more sexual partners and unprotected anal intercourse; condom use based on the real or perceived HIV status of sexual partners (“serosorting”); sexual role assignments (insertive versus receptive) based on HIV status (“seropositioning”); and seeking sexual partners on the Internet (Marcus, Voss, Kollan, & Hamouda, 2006). One study concluded that about 40 percent of MSWs in Germany did not use a condom with regular clients who paid more, and that only a third knew where they could receive anonymous HIV testing (Steffan & Sokolowski, 2008). Migrant MSWs were especially poorly informed about the risks associated with specific sex practices.
Many MSWs describe themselves as heterosexual and are involved in intimate relationships with women, with whom they often avoid open communication about their same-sex behavior. Moreover, MSWs are more likely to use condoms with paying partners than in intimate private relationships (Padilla, 2007; Parsons, 2005; Wright, 2003). Indeed, men who practice bisexual behavior eventually became a central focus of HIV research because of the associations between sexual risk behavior, serostatus, and disclosure. The bridge model of the late 1980s considered bisexuality to be narrowly contained within a small group of “risky men” and thus singled out male sex workers as central to the spread of HIV to the general population (Aggleton, 1996). This approach neglected to contextualize disclosure patterns within broader experiences of social inequality and stigma management. Researchers continue to debate the role disclosure of HIV status plays in safer sex practices (Padilla et al., 2008), with some suggesting that nondisclosure does not necessarily equate with higher sexual risk for HIV. Men who migrate are at increased risk for HIV infection and face a number of barriers affecting disclosure to their stable female partners (Hirsch, 2003; Padilla, 2007). Furthermore, claims reporting condom use among a definitive percentage of sex workers should be viewed with skepticism, as this assumes there is a fixed MSW population, which is a “fiction” (Altman, 1999). Human interactions and relationships follow a continuum, and many sexual transactions may involve people who do not identify as sex workers. The outbreak of HIV meant that “grudging attention came to be paid to … ‘men who have sex with men’ (a clumsy phrase adopted to overcome the confusion of identity with behaviour)” (Altman, 1999, p. xiii). One danger in the literature that frames sex work as the product of economic necessity is that the sexual orientation of male sex workers is always questioned, whereas female sex workers are often assumed to be heterosexual (Dennis, 2008). By overemphasizing that many MSWs are not “really” homosexual, researchers may have fueled one of the great panics of the HIV epidemic, namely, the fear that male sex workers would serve as “vectors” of infection to the “general” community (Altman, 1999).
Because of the bridge effect and a fixation on bisexuality, most research evaluating the health needs of MSWs has emphasized HIV rather than general health concerns or high rates of violence (Dennis, 2008). However, their multiple interrelated vulnerabilities put them at risk for a number of health problems beyond STIs (Wright, 2003). One of the only studies of German MSWs that mentions non-STI health problems noted that they were “diverse but within normal range” (Steffan & Sokolowski, 2008). While the authors did not elaborate further, this suggests a pattern typical for this age group, including sporadic acute health issues and lower rates of chronic disease. Few studies have examined actual male sex workers’ access to health care and use of health services.
Health-Care Access and Primary Complaints
The remainder of this chapter will focus on health concerns among migrant MSWs, the most serious of which is a lack of health insurance. In Germany, selling sex is considered a legitimate economic activity and people working in the sex industry are entitled to participate in the social welfare and health-care systems. Most migrant MSWs, however, are not officially registered as residents, often because they cannot afford to rent an apartment on their own so they cannot obtain the small business license required to indicate this as their primary employment. Even if they are legally registered, they may be unable to afford health insurance, which can cost 250 euros (US$300) or more a month. While assistance is available to help low-income earners maintain health insurance, social workers note that they have difficulty obtaining information about benefits because of their clients’ unclear status as EU citizens. One noted that she calls government offices on behalf of MSWs, but “they always just say, ‘send in the application and we’ll let you know what other paperwork is required.’ But then you never hear back, or they just reject this application with no explanation.” If MSWs later enter a different field of employment with a legal work permit, they often have to pay retroactively to enter the statutory health insurance system, beginning when they registered as having entered the country. This often means paying thousands of euros.
Because they lack health insurance, many MSWs access care at the weekly medical consultations offered through the drop-in centers. Physicians are sometimes provided by the local health department, while others are volunteers or retired doctors. The following sections draw upon interviews with physicians, social workers, health department staff, and male sex workers, as well as annual reports from organizations providing assistance to male sex workers in eight major cities: Berlin, Hamburg, Frankfurt am Main, Cologne, Stuttgart, Munich, Dortmund, and Essen. In 2011, the Berlin organization serving men who have sex with men whose reports were reviewed for this study provided 354 medical consultations (Subway, 2012). Over the last seven-and-a-half years (2005 through mid-2012) it has provided 2,603 medical consultations to at least 756 individuals. The Frankfurt organization provided care to 91 patients (KISS, 2012), while the Cologne organization provided 456 consultations on health-related issues and accompanied 41 people to medical services (LOOKS, 2012). The Berlin organization also has a mobile clinic that is set up outside local bars 12 times a year and advertised through street worker outreach and word of mouth. While much in demand, services are limited because of time and space constraints, as well as low levels of lighting that impede thorough physical examinations. Physicians must improvise for the medications or treatments they offer. Some young men are sent to the hospital for emergencies such as appendicitis or injuries from a fight, and many mobile consultations involve testing and vaccinating for hepatitis. The physicians and staff interviewed for this study noted that the young men’s knowledge of health and bodily processes was poor, which, coupled with language barriers, often led to misunderstandings.
An overview of major health concerns for MSWs can be found in the annual reports of these organizations, along with additional medical data provided by one of the organizations. Physicians working with this population primarily encounter illnesses associated with lifestyle and poverty. At the Berlin organization, 77.2 percent of all medical visits were for issues unrelated to STIs (Subway, 2012). Another organization reported that the main illnesses, in order of frequency, were respiratory (28.6 percent), dermatological (17 percent), urological (13.2 percent), back pain (9 percent), toothache (6.5 percent), headache (5.5 percent), and injuries (5.5 percent; KISS, 2012). The physicians interviewed noted that the primary medical conditions for which migrant MSWs seek help are general concerns such as headaches, stomachaches, and fungal infections. These issues stem from a lack of personal care by those living on the streets without regular access to health care. One doctor noted, for instance, that “nail fungus can be easily treated—most people are able to go to the pharmacy and obtain topical medication. But these boys are in bars two or three nights straight, often without sleep, showers, food, and clean clothing, and as a result the problem becomes worse and worse until it is unbearable.” Lice and bedbug bites are common problems resulting from sleeping in crowded, unhygienic conditions. Other young men face the unpredictable illnesses typical for this age group, such as a hernia requiring surgery. Describing one such case, a physician stated that there was little chance of a breech, but “the boy was in pain and we can’t let him just continue to walk around like that,” so a low-cost surgery was negotiated with a local hospital. Violence, usually fighting, was noted to be a common cause of injury that was not addressed in weekly clinics, as such injuries are often severe enough to send men straight to the emergency room.
Some physicians stated that they were unable to adequately address mental health issues, even though many young men report somatic symptoms and depression. Some organizations work with volunteer psychologists, but their time and ability to provide therapy is very limited. The nature of sex work remains difficult for many, and some men cope by turning to alcohol or smoking hashish. Cigarette smoking is universal. Other drugs are generally not used, although a few men report occasionally consuming cocaine provided by clients. This is in line with results from a prior study, which concluded that most substance use involved alcohol, cannabis, and poppers (Steffan & Sokolowski, 2008).
In the words of a staff member from one of the organizations serving MSWs, dental issues are considered “a huge problem with no clear solution.” One organization reported that they used to send men for free dental services at a local homeless shelter, but this is no longer available because, to protect their own funding stream, the shelters no longer serve migrants. One organization has a private dentist in its network who will take some patients for a small fee. However, as one physician noted,
when you start taking people, as a dentist you either have to open your door to many, or you have to set strict limits. Some dentists will say, “Oh, but I’ve already taken three this year,” or ask, “Is it an emergency?” She says indignantly, “How do I know if it’s an emergency? This person is in pain, bad pain. Crying in front of me. When exactly does that become an emergency?”
Most dentists, she claimed, do not understand the limitations associated with the migrant MSWs’ lifestyle. She gave the example of a young man who showed up late at a dentist’s office and was refused to be seen. As she explained, “You can’t do that with this population, they don’t know their way around the city; it’s sad, they may live here for years but stay in one area, and thus have never really explored Berlin.” Or, she added, they may have had an appointment with a paying client during the day: “You just can’t schedule like that for this population.”
Referrals are a common part of the weekly medical visits, mobile clinics, and social work consultations. MSW clients are referred directly to the health department for STIs, but are otherwise sent to charity or nonprofit clinics. One physician stated that she “has to be careful about which boys I send to which organizations, because some are more judgmental than others.” This is because of the stigma associated with being a sex worker and Roma. At the same time, she noted, many Roma are reluctant to go to the doctor because they have had bad experiences in the past and have “been treated differently their whole lives. Many have never been to a doctor before … So, you are negotiating these two positions.”
“Hustling Is Hustling, It Has Nothing to Do with Your Sexuality”: STIs, HIV, and Sexuality
HIV and other STIs are a major focus of medical consultations and health education efforts, even if the most common medical problems encountered are unrelated. Migrant MSWs are at high risk for HIV infection for a number of reasons. First, a lack of job options, language barriers, and an insecure housing situation mean they are pushed to work in riskier settings. This leads to more dependency, greater competition, and higher susceptibility to violence, all of which influence their willingness to engage in riskier sex practices. Second, social workers and physicians report that migrant MSWs have little knowledge of STIs, which they attribute to a lack of formal education and the fact that the men are quite young and inexperienced. With an average age of 21, they enter into sex work largely without instruction or mentorship, and they are ill informed about the possible threats to their health and thus willing to take risks. They rarely discuss their experiences or possible dangers, such as a client refusing to use a condom. In interviews and health education sessions, the misinformation they encounter comes to light. For example, some believe that HIV infections can occur only after a series of other diseases, so one first acquires gonorrhea, then syphilis, and only then is susceptible to HIV. Many believe that one can “see” if someone is HIV positive based on their general habits and grooming; one said that “if a person is [physically] dirty, I just don’t go with him.” These beliefs, along with few years of formal schooling, a lack of German language skills, and, in some cases, illiteracy, hamper preventive health efforts.
Sexual orientation further affects these men’s perceptions of risk and preventive behavior. While some identify as gay and describe escaping severe discrimination in their home countries (where, as one noted, “being gay is worse than being a prostitute”), many consider themselves heterosexual (Gille, 2007; KISS, 2012; LOOKS, 2012). Others identify as bisexual or, in the words of one social worker, “aren’t quite sure yet—they are still experimenting.” In an annual report from one of the organizations serving MSWs, 51.3 percent identified as heterosexual, 23.5 percent as homosexual, 20.2 percent as bisexual, and less than 1 percent as transgender; 44 percent did not provide information on sexual orientation (LOOKS, 2012). Another source reports that 36 percent defined themselves as heterosexual, 30 percent as homosexual, and 33 percent as bisexual (Steffan & Sokolowski, 2008). Some also report being hired by female clients; thus their sexual reality is complex, making the label of men who have sex with men not necessarily accurate, although it is the most dominant aspect of their work lives. In their private lives, however, it is not uncommon for the young men to be married, and some bring their wives and children to Germany with them. Since many plan on having children, condom use in these marital relationships is atypical. Moreover, truthful disclosure of their work life in Germany is uncommon. “My girlfriend [in Romania]?” one young man told me, “I tell her I am working for my uncle on construction sites.” Since many of the boys identify as heterosexual, organization staff serving MSWs in the various metropolitan settings often encourage them to think about sexuality as encompassing a range of forms and that “what’s in their head does not have to always match the actions of their body.” Put another way, one social worker emphasizes that “hustling is hustling, it has nothing to do with your sexuality.”
To complicate preventive health efforts, many MSWs claim that they only practice a sexually active (insertive) role, due to social taboos surrounding homoeroticism. Certain acts may be considered homosexual while others are not; as long as they do not perform any of these techniques or do not confess to offering them (or enjoying them), they are generally able to reconcile their sex work with their preferred identity. Social workers and physicians noted a disconnect between this discourse and everyday practice, however, as the men likely participate in a range of sexual activities. This disconnect, according to one social worker, allows the men to preserve their dignity and to “show they are the ones in control.” These stigma management techniques minimize the effects of their marginality but also constrain their disclosure of sexual risks with their female partners. When asked about how this affects discussion of HIV prevention, one doctor said she “simply lay[s] out what can happen in both roles, that the passive role has a higher chance of [HIV] infection. They get both messages.”
While only a small percentage of health consultations were prompted by an STI, there was a strong emphasis on prevention and diagnosis. Out of 364 encounters in 2011, physicians working with the Berlin organization reported 38 STI diagnoses: gonorrhea (10, ~3 percent), chlamydia (10, ~3 percent), syphilis (7, ~2 percent), condyloma/genital warts (5, ~1.2 percent), hepatitis C (5, ~1.2 percent), and hepatitis B (1, 0.3 percent). Physicians also provided significant preventive care, educating about STIs in 37 percent and hepatitis in 31 percent of their encounters with MSWs, and providing a hepatitis vaccine in 11 percent. A study from Dortmund found that about 50 percent of male sex workers had been vaccinated against hepatitis A/B, confirming the success of outreach efforts. However, only 46 percent said they had ever had an STI checkup, and only 2 percent of those had taken place in the previous two years. The most frequent illnesses mentioned in the study were gonorrhea and syphilis (Steffan & Sokolowski, 2008).
Because organizations serving MSWs generally do not test for HIV on site for a number of logistical and ethical reasons, these men are referred to the health department. In many cities, the department is considered a trusted place where the men recognize people because they become familiar with health department staff during medical visits at the drop-in centers. Gonorrhea, chlamydia, and syphilis can be treated for free. Syphilis is easily treated with a monthlong course of pills or weekly injections; one health department physician shared her preference for injections because of this group’s irregular lifestyle. If they insist on pills, she will “only give them a week’s supply at a time to be sure they return for follow-up.” In this way, she tries to ensure that therapy continues and that the men avoid losing or sharing their pills. Hepatitis is more difficult to treat; health departments reported having the ability to treat type B only as it becomes symptomatic, and treatment for hepatitis C is simply too expensive for the uninsured men (500-600 euros, or about US$600-$720 a month). In these cases, patients are monitored but not treated, which often opens up a dialogue about the benefits of obtaining health insurance in their home country and then applying for the EU Health Insurance Card to reduce their out-of-pocket portion.
Some medical and health outreach staff stated that they found it ethically problematic to test people for HIV when therapy is out of reach. A range of strategies must be considered if an uninsured person is diagnosed as HIV positive, but it still becomes, as one social worker noted, a “matter of luck” whether they are able to access treatment. HIV/AIDS does not qualify as an acute illness eligible for coverage by the state, even though, as the same social worker noted wryly, he has seen other cost-intensive treatments like chemotherapy approved. Ultimately, a migrant MSW diagnosed with HIV/AIDS has three options. First, he can apply for unemployment benefits on the grounds that the illness prevents him from working; this is problematic if he was never eligible to work in the first place because of the German labor market restrictions mentioned earlier. Second, if he has obtained a small business license, he may become eligible for health insurance coverage through the unemployment system after proving to have insufficient income. Finally, the best option may simply be to return to his country of origin, especially if social workers are able to locate treatment resources there. Wide networks are cultivated in other countries for this very reason. However, one social worker stressed that HIV is generally acquired in Germany, therefore it is “simply not fair to send them back to their countries, as this shifts responsibility away” from the host society. Indeed, epidemiological data support the fact that, among migrant men who have sex with men, more than 90 percent acquired the infection in Germany (Robert Koch-Institut, 2010).
Discussion
As explained above, constrained options resulting from national policies that restrict access to the labor market clash with the promise of economic opportunity through freedom of movement across EU borders. This reality is framed by multiple disadvantages, including poverty, discrimination, unemployment, and low educational attainment. Structural transformations in the economy that lead to an increase in men’s labor migration increase the likelihood that a given individual will be confronted with the possibility and the need to exchange sex for money (Padilla, 2007).
In Western Europe, a high demand for sexual services meets a relatively unregulated market, despite instances of legalization. In Germany, selling sex is considered a legitimate economic activity, and the 2002 Act Regulating the Legal Status of Prostitutes protects sex workers from discrimination, strengthens their legal rights, and promises regular screenings and eligibility for the statutory health insurance system as self-employed individuals, which has a positive impact on individual and public health. Excluded from these benefits, however, is the large population of migrant sex workers without clear legal status or a work permit, and no improvement in the situation of migrant MSWs is evident, based on Germany’s 2002 prostitution law. Already critiqued for its vague components, inconsistent implementation, and the fact that most sex workers remain unfamiliar with its provisions (Helfferich, 2005), I would add that MSWs are not the primary beneficiaries of the law and that some migrant groups cannot even apply for the work permits necessary to take advantage of its protections.
This example also demonstrates that there are significant limits to the entitlements and meaning associated with what, on the surface, appear to be widening citizenship practices. These practices negatively affect the health of marginal populations, like migrant MSWs from poor EU countries who live in more prosperous ones, as citizenship constructs solidify new and existing inequalities. The high proportion of Romanian and Bulgarian MSWs in Germany is clearly linked to the expansion of the EU and the limited employment opportunities associated with transitional measures imposed by the German government. In previous years—and immediately following their countries’ entry to the EU—young men from Poland and the Czech Republic filled these positions. As the transitional measures were lifted, their numbers decreased. One health department physician said she was able to “literally watch the borders shift, based on the patients that came in,” noting that they had to fire some of their best interpreters when, for example, Polish language skills were no longer needed. The same process, she and others reasoned, will undoubtedly unfold with Bulgarians and Romanians once the transitional measures are lifted in 2014 and other employment options become available. Presuming continued demand for male sex work, the question remains: from where will the next waves of multiply structurally disadvantaged young men come?
This chapter argues for going beyond targeting “risky men,” which leads to further stigma, and focusing instead on the ways men move in and out of risky social contexts and how focusing on their structural vulnerability can help us understand mutually reinforcing insults that have a negative impact on health at the economic, political, cultural, and individual levels. It encourages researchers and social workers working with MSWs to move beyond the basic association between sex work and HIV to contextualize health risks as a result of macro-level processes, including immigration and restrictive labor policy. In the case of Germany, as discussed here, access to medical services is sharply limited for sex workers whose socio-legal position resembles that of irregular migrants and is indicative of fragmentary membership and asymmetrical citizenship practices in the EU (Castañeda, 2011). Migrant MSWs are largely excluded from medical care or are treated by ad hoc clinics that cannot cover the entire range of treatment needs. These include everyday medical concerns and experiences of violence, which are often obscured in the myopic focus on HIV (Dennis, 2008). The data presented here indicate that MSWs face many of the same health issues as unauthorized migrants, particularly a lack of dental and mental health-care options (Castañeda, 2009).
Migration of MSWs between German cities and their home communities creates a shift in the meanings and practices of masculinity. Thus, “the gender imperative for men to provide economically for their families may ironically increase the chances that female partners and children will be affected by the AIDS epidemic as male labor migrants engage in high-risk sexual practices for instrumental purposes while geographically separated from families and communities” (Padilla, 2011, p. 162). This study also noted patterns of selective condom use, whereby MSWs generally used condoms with male clients but not with trusted male or female intimate partners. In addition, in the interviews described here, some also refused condom use with female partners because they wanted to become fathers. Thus, rather than attributing this to a lack of knowledge or willingness to engage in risky behavior, it should be understood within the context of long-term social goals and responsibilities.
Anthropologists contributed to the development of more nuanced perspectives in the early years of the AIDS epidemic by questioning the assumed congruence between sexual identity and behavior. Ethnographic data point to a variety of cross-cultural constructions of gender, and to the importance of structural processes for sexual meaning and practices. The exchanges in which MSWs engage unfold “within a much more fluid pattern of behavioral and situational bisexuality than the narrowly heterosexual pattern described in most prior studies” (Padilla, 2007, p. 7). Such men are largely invisible to research models that rely on discrete concepts of sexual identity and obfuscate the fact that bisexual behavior may be an integral feature of sexual life and the epidemiology of HIV. Indeed, sexual identity is actually irrelevant to the transaction, which more often revolves around the roles played by the partners (e.g., active/passive; Dennis, 2008). Thus, while important information for prevention efforts, it is not a new finding that MSWs claim to participate in active or insertive anal sex with male partners or that many consider themselves heterosexual. This is underscored in literature on MSWs from across the globe, including earlier research among Bulgarian and Romanian (Gille, 2007) and Turkish MSWs in Germany (Bochow, 2003), and on sexual norms among Roma in Bulgaria (Kelly et al., 2004). The resulting discrepancies between MSWs’ statements and their actual sexual practice should be viewed as a way they deal with complex pressures and constraints. Health promotion projects are hindered by inaccurate or unrealistic conceptualizations of sexual behavior, as well as a stubborn focus on narrowly framed risk groups (men who have sex with men or sex workers), rather than on causal factors that shape the social context of risk. Traditional public health approaches are largely incapable of capturing the nuances of MSWs’ intimate experiences and how this risk behavior is shaped by larger structural factors.
References
Aggleton P. (Ed.). (1996). Bisexualities and AIDS: International perspectives. London: Taylor & Francis.
Agustin, L. (2006). The disappearing of a migration category: Migrants who sell sex. Journal of Ethnic and Migration Studies, 32, 29-47.
Allman, D., & Myers, T. (1999). Male sex work and HIV/AIDS in Canada. In P. Aggleton (Ed.), Men who sell sex (pp. 61-81). London: Taylor & Francis.
Altman, D. (1999). Foreword. In P. Aggleton (Eds), Men who sell sex. London: Taylor & Francis.
Bochow, M. (2003a). Die Lebenswelten von Strichern: Interviews aus der Szene. [Lifeworlds of hustlers: Interviews from the scene.] In M. T. Wright (Ed.), Prostitution, Prävention und Gesundheitsförderung: Teil 1, Männer [Prostitution, prevention, and health promotion: Part 1, Men] (pp. 25-48). Berlin: Deutsche AIDS Hilfe.
Castañeda, H. (2009). Illegality as risk factor: A survey of unauthorized migrant patients in a Berlin clinic. Social Science & Medicine, 68, 1552-1560.
Castañeda, H. (2011). Effects of transitional measures associated with EU integration on medical care access for Central and Eastern European migrants in Germany. Anthropological Journal of European Cultures, 20, 68-86.
Constable, N. (2009). The commodification of intimacy: Marriage, sex, and reproductive labor. Annual Review of Anthropology, 38, 49-64.
Dennis, J. (2008). Women are victims, men make choices: The invisibility of men and boys in the global sex trade. Gender Issues, 25, 11-25.
European Network on Male Prostitution. (2003). Final report: 2003. Amsterdam: Author.
Evans, J. E. (2003). Bahnhof boys: Policing male prostitution in post-Nazi Berlin. Journal of the History of Sexuality, 12, 605-636.
Fiedler, M. (2011, August 25). Helfer in einer verstohlenen Welt. [Assistance in a clandestine world.] Frankfurter Allgemeine.
Gille, C. (2007). Romanians and Bulgarians in male street sex work in German cities. Unpublished master’s thesis, Hogeschool Zuyd, Maastricht and Metropolitan University London.
Helfferich, C. (2005). Untersuchung zu den Auswirkungen des Prostitutionsgesetzes (ProstG). [Study of the impact of the Prostitution Law.] Freiburg, Germany: Bundesministerium für Familie, Senioren, Frauen und Jugend.
Hirsch, J. S. (2003). A courtship after marriage: Sexuality and love in Mexican transnational families. Berkeley: University of California Press.
Kelly, J. A., Amirkhanian, Y. A., Kabakchieva E., Csepe, P., Seal, D. W., Antonova, R., et al. (2004). Gender roles and HIV sexual risk vulnerability of Roma (Gypsy) men and women in Bulgaria and Hungary: An ethnographic study. AIDS Care, 16, 231-245.
Marcus, U., Bremer, V., & Hamouda, O. (2004). Syphilis surveillance and trends of the syphilis epidemic in Germany since the mid-90s. Eurosurveillance Monthly, 9, 11-14.
Marcus, U., Voss, L., Kollan, C., & Hamouda, O. (2006). HIV incidence increasing in MSM in Germany: Factors influencing infection dynamics. Eurosurveillance Monthly, 11(9), ii-645.
Minichiello, V., Mariño, R., Browne, J., Jamieson, M., Peterson, K., Reuter, B., et al. (2001). Male sex workers in three Australian cities: Socio-demographic and sex work characteristics. Journal of Homosexuality, 42(1), 29-51.
Padilla, M. (2007). Caribbean pleasure industry: Tourism, sexuality, and AIDS in the Dominican Republic. Chicago: University of Chicago Press.
Padilla, M. (2011). Regional masculinities, tourism labor, and sexual risk: Toward a structural framework for reproductive health research in the Caribbean. In C. Sargent & C. Browner (Eds.), Globalization, reproduction, and the state (pp. 159-174). Durham, NC: Duke University Press.
Padilla, M., Castellanos, D., Guilamo-Ramos, V., Reyes, A. M., Sanchez Marte, L. E., & Soriano, M. A. (2008). Stigma, social inequality, and HIV risk disclosure among Dominican male sex workers. Social Science & Medicine, 67, 380-388.
Parsons, J. T. (2005). Researching the world’s oldest profession: Introduction. In J. T. Parsons (Eds), Contemporary research on sex work (pp. 1-3). Binghamton, NY: Haworth Press.
Quesada J., Hart L. K., & Bourgois, P. (2011). Structural vulnerability and health: Latino migrant laborers in the United States. Medical Anthropology, 30, 339-362.
Robert Koch-Institut. (2010). HIV bei Migranten in Deutschland. [HIV among migrants in Germany.] Epidemiology Bulletin, 5, 39-44.
Simon, P. (2007). “Ethnic” statistics and data protection in the Council of Europe countries. Strasbourg: Council of Europe.
Smith, N. (2011) The international political economy of commercial sex. Review of International Political Economy, 18, 530-549.
Steffan, E., & Sokolowski, S. (2008). Studie zur Lebenslage von Strichern/mann-männlichen Prostituierten im östlichen Ruhrgebiet/Dortmund: Eine Bedarfsanalyse. [Study on the situation of hustlers/male-male prostitutes in the eastern Ruhr region/Dortmund: A needs assessment.] Essen, Germany: AIDS Hilfe Essen.
Subway. (2012). Bericht über die Arbeit im Jahr 2011. [Report of work in the year 2011.] Unpublished report.
UNAIDS. (2012). Global AIDS response country progress report: Germany. Geneva: UNAIDS.
Unger, H., & Gangarova, T. (Eds.). (2011). PaKoMi Handbuch. [PaKoMi manual.] Berlin: Wissenschaftszentrum Berlin für Sozialforschung and Deutsche AIDS-Hilfe.
Whisnant, C. J. (2006). Styles of masculinity in the West German gay scene, 1950-1965. Central European History, 39, 359-393.
Wright, M. T. (2001). Die Lebenslage von Strichern in Köln, Düsseldorf und im Ruhrgebiet: Eine Bedarfsanalyse. [The situation of hustlers in the Cologne, Dortmund, and the Ruhr region: A needs assessment.] Köln: AIDS-Hilfe Essen e.V. und von Looks e.V.
Wright, M. T. (2003). Stricher und Stricherarbeit: Erkenntnisse aus Wissenschaft und Praxis. [Hustlers and hustling work: Insights from scholarship and practice.] In M. T. Wright (Ed.), Prostitution, Prävention und Gesundheitsförderung: Teil 1, Männer (pp. 11-25). Berlin: Deutsche Aidshilfe.
Wright, M. T. (2012). Der sozialwissenschaftliche Beitrag zu Fragen der mann-männlichen Prostitution. [The social science contribution to questions of male-male prostitution.] Presentation made to the Runder Tisch Prostitution, Düsseldorf, Germany.
Endnotes