CHAPTER 19 Cardiovascular System: Blood
653
derived from hemocytoblasts, give rise to
proerythroblasts.
Afterseveral mitotic divisions, proerythroblasts become
early erythroblasts.
These cells are also called
basophilic erythroblasts
because they stainwith a basic dye. The dye binds to the large numbers of ribosomesnecessary for the production of hemoglobin, giving the cytoplasm apurplish color. Early erythroblasts give rise to
intermediateerythroblasts.
These cells are also called
polychromatic erythroblasts
because they stain different colors with basic and acidic dyes. Forexample, when an acidic dye is used, intermediate erythroblasts staina reddish color when it interacts with the hemoglobin accumulating inthe cytoplasm. Intermediate erythroblasts continue to produce hemo-globin, and then most of their ribosomes and other organellesdegenerate. The resulting
late erythroblasts
have a reddish colorbecause about one-third of the cytoplasm is hemoglobin.The late erythroblasts lose their nuclei to become immaturered blood cells, called
reticulocytes
(re-tik′ ū -l ō -s ī tz).
Reticulo-cyte
refers to a reticulum, or network, that can be observed in thecytoplasm when a special staining technique is used. The reticu-lum is artificially produced by the reaction of the dye with thefew remaining ribosomes in the reticulocyte. Reticulocytes arereleased from the bone marrow into the circulating blood. A nor-mal reticulocyte level is 0.5–2% of circulating red blood cells.Reticulocyte counts are clinically useful to monitor red blood cellproduction, particularly when monitoring treatments for anemia.Also, reticulocyte counts can provide information about thehealth of the hemocytoblasts in the red bone marrow. Within 2days, the ribosomes in the reticulocytes degenerate, and thereticulocytes become mature red blood cells.
Decreasedbloodoxygen
Increasedbloodoxygen
cell
marrow
Increasederythropoietin(EPO)
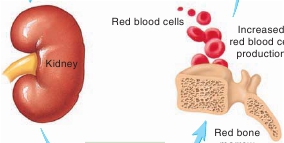
FIGURE 19.5
Red Blood Cell Production
In response to decreased blood oxygen, the kidneys release erythropoi-etin into the bloodstream. The increased erythropoietin stimulates redblood cell production in the red bone marrow. This process increases bloodoxygen levels, restoring homeostasis.
Predict 3
During a local Red Cross blood drive, Juan donated one unit of blood(about 500 mL). Predict how his reticulocyte count changed during theweek after he donated blood, and explain why the change occurred.
tissues. Conversely, if blood oxygen levels rise, less erythropoie-tin is released, and red blood cell production decreases.
Predict 4
Cigarette smoke produces carbon monoxide. If a nonsmoker smokeda pack of cigarettes a day for a few weeks, what would happen to thenumber of red blood cells in the person’s blood? Explain.
Cell division requires the B vitamins folate and B
12
, which arenecessary for the synthesis of DNA (see chapter 3). Hemoglobinproduction requires iron. Consequently, adequate amounts offolate, vitamin B
12
, and iron are necessary for normal red bloodcell production.Red blood cell production is stimulated by low blood oxygenlevels, which result from several conditions: decreased numbers ofred blood cells, decreased or defective hemoglobin, diseases of thelungs, high altitude, inability of the cardiovascular system todeliver blood to tissues, and increased tissue demands foroxygen—for example, during endurance exercises.Red blood cell production is regulated by the glycoprotein
erythropoietin
( ĕ -rith-r ō -poy′ ĕ -tin), a hormone produced mostlyby the kidneys (figure 19.5). Erythropoietin secretion increaseswhen blood oxygen levels are low. This stimulates red bone mar-row to produce more red blood cells by increasing the number ofproerythroblasts formed and by decreasing the time required forred blood cells to mature. Thus, when blood oxygen levelsdecrease, erythropoietin production increases, which increases redblood cell production. The greater number of red blood cellsincreases the blood’s ability to transport oxygen. This negative-feedback mechanism returns blood oxygen levels to normal andmaintains homeostasis by increasing the delivery of oxygen to
The normal lifespan of a red blood cell is about 120 days inmales and 110 days in females. These cells have no nuclei and there-fore cannot produce new proteins or divide. As their existing proteins,enzymes, plasma membrane components, and other structures degen-erate, the red blood cells are less able to transport oxygen, and theirplasma membranes become more fragile. Eventually, the red bloodcells rupture as they squeeze through a tight spot in the circulation.
Macrophages
located in the spleen, liver, and other lymphatictissue take up the hemoglobin released from ruptured red bloodcells (figure 19.6). Within a macrophage, lysosomal enzymesdigest the hemoglobin to yield amino acids, iron, and bilirubin. Theglobin part of hemoglobin is broken down into its componentamino acids. Most of the amino acids are reused to produce otherproteins. Iron atoms released from heme are carried by the blood tored bone marrow, where they are incorporated into new hemoglo-bin molecules. After the removal of the iron atoms, the non-ironpart of the heme groups is first converted to
biliverdin
(bil-i-ver′din)and then to
bilirubin
(bil-i-roo′bin). The bilirubin is then releasedinto the plasma, where it binds to albumin and is transported to livercells. This bilirubin, called
free bilirubin,
is taken up by the liver