Chapter 20: Nervous and Endocrine Systems
Lesson 20.1: The Nervous System
Lesson Objectives
- Identify the type of cells that make up nervous tissue.
- Describe the structure of a neuron.
- Relate membrane potential to action potential.
- Outline the role of neurotransmitters in neuron communication.
- Distinguish between the sensory and motor divisions of the peripheral nervous system.
- Describe the structure of the eye and identify the roles of rods and cones in vision.
- Describe the structure of the ear and identify the structures that are important to hearing and balance.
- Distinguish between the receptors for pain, pressure, and temperature.
- Identify the main effect of psychoactive drugs on the CNS.
- Summarize the mechanism of addiction.
Introduction
Your body has two systems that help you maintain homeostasis: the nervous system and the endocrine system. The nervous system is a complex network of nervous tissue that sends electrical and chemical signals. The nervous system includes the central nervous system (CNS) and the peripheral nervous system (PNS) together. The central nervous system is made up of the brain and spinal cord, and the peripheral nervous system is made up of the nervous tissue that lies outside the CNS, such as the nerves in the legs, arms, hands, feet and organs of the body. The nervous system mediates communication between different parts of the body as well as the body’s interactions with the environment.
The endocrine system is a system of glands around the body that release chemical signal molecules into the bloodstream. The electrical signals of the nervous system move very rapidly along nervous tissue, while the chemical signals of the endocrine system act slowly in comparison and over a longer period of time. Working together, the nervous and endocrine systems allow your body to respond to short or long term changes in your environment, such as a pedestrian suddenly stepping out in front of your bike, or your body adapting to cycling in a warm, humid summer evening, as shown in Figure below.

Figure 20.1
Cycling home in rush-hour traffic demands a lot of your nervous and endocrine systems. Your nervous systemmostly through your eyes and earsconstantly monitors your surroundings, alerting you instantly at any sign of change or danger. Your endocrine system gears up your muscles and cardiovascular system for the ride, by flooding your body with metabolism-boosting hormones.
Nerve Cells
Although the nervous system is very complex, there are only two main types of nerve cells in nervous tissue. All parts of the nervous system are made of nervous tissue. The neuron is the "conducting" cell that transmits electrical signals, and it is the structural unit of the nervous system. The other type of cell is a glial cell. Glial cells provide a support system for the neurons, and recent research has discovered they are involved in synapse formation. A type of glial cell in the brain, called astrocytes, is important for the maturation of neurons and may be involved in repairing damaged nervous tissue. Neurons and glial cells make up most of the brain, the spinal cord and the nerves that branch out to every part of the body. Both neurons and glial cells are sometimes referred to as nerve cells.
Structure of a Neuron
The special shape of a neuron allows it to pass an electrical signal to another neuron, and to other cells. Electrical signals move rapidly along neurons so that they can quickly pass “messages” from one part of the body to another. These electrical signals are called nerve impulses.
Neurons are typically made up of a cell body (or soma), dendrites, and an axon, as shown in Figure below. The cell body contains the nucleus and other organelles similar to other body cells. The dendrites extend from the cell body and receive a nerve impulse from another cell. The cell body collects information from the dendrites and passes it along to the axon. The axon is a long, membrane-bound extension of the cell body that passes the nerve impulse onto the next cell. The end of the axon is called the axon terminal. The axon terminal is the point at which the neuron communicates with the next cell. You can say the dendrites of the neuron receive the information, the cell body gathers it, and the axons pass the information onto another cell.

Figure 20.2
The general structure of a neuron. Neurons come in many different shapes and sizes, but they all have a cell body, dendrites, and an axon. The cell body contains a nucleus and other organelles. However, not all neurons have a myelin sheath.
The axons of many neurons are covered with an electrically insulating phospholipid layer called a myelin sheath. The myelin speeds up the transmission of a nerve impulse along the axon. It acts like a layer of insulation, like the plastic you would see around an electrical cord.
The myelin is an outgrowth of glial cells. Schwann cells which are shown wrapped around the neuron in Figure above, are a type of glial cell. Schwann cells are flat and thin, and like other cells, contain a nucleus and other organelles. Schwann cells supply the myelin for neurons that are not part of the brain or spinal cord, while another type of glial cell, called oligodendrocytes, supply myelin to those of the brain and spinal cord. Myelinated neurons are white in appearance, and they are what makes up the "white matter" of the brain. A cross section of a myelinated neuron is shown in Figure below. Myelin is not continuous along the axon. The regularly spaced gaps between the myelin are called Nodes of Ranvier. The nodes are the only points at which ions can move across the axon membrane, through ion channels. In this way the nodes act to strengthen the nerve impulse by concentrating the flow of ions at the nodes of Ranvier along the axon.

Figure 20.3
A transmission electron microscope (TEM), image of a cross section of a myelinated axon. The rings around the axon are made up of Schwann cell membrane, which is wrapped many times around the axon.
Neurons are specialized for the passing of cell signals. Given the many functions carried out by neurons in different parts of the nervous system, there are many different of shapes and sizes of neurons. For example, the cell body of a neuron can vary from 4 to 100 micrometers in diameter. Some neurons can have over 1,000 dendrite branches, which make connections with tens of thousands of other cells. Other neurons have only 1 or 2 dendrites, each of which has thousands of synapses. A synapse is a specialized junction at which neurons communicate with each other, and is shown in Figure below. Also, a neuron may have 1 or many axons. The longest axon of a human motor neuron can be over a meter long, reaching from the base of the spine to the toes. Sensory neurons have axons that run from the toes to the spinal cord, over 1.5 meters in adults. Giraffes have single axons several meters in length running along the entire length of their necks.

Figure 20.4
The location of synapses. Synapses are found at the end of the axons (called axon terminals) and help connect a single neuron to thousands of other neurons. Chemical messages called neurotransmitters are released at the synapse and pass the message onto the next neuron or other type of cell.
Nerve Impulses
In the late 18th century, the Italian doctor and physicist Luigi Galvani first recorded the action of electricity on the muscle tissue of frogs. He noted that an electrical charge applied to a nerve in the legs of a dead frog made the legs move. Galvani attributed the movement of the frog’s muscles to an electrical current that was carried by the nerves. Galvani coined the term "animal electricity" to describe this vital force for life.
Galvani believed that animal electricity came from the muscle and was unique to living creatures. However, his fellow Italian, and physicist, Alessandro Volta disagreed with him and reasoned that animal electricity was a physical phenomenon, that occurred between metals. Volta disproved Galvani’s claim by building the first battery, which showed that a current could flow outside an organism’s body. Since then scientists have learned much about electrical charges in living systems.
Ion Channels and Nerve Impulses
Ion transport proteins have a special role in the nervous systems because voltage-gated ion channels and ion pumps are essential for forming a nerve impulse. Ion channels use energy to build and maintain a concentration gradient of ions between the extracellular fluid and the cell’s cytosol, as shown in Figure below. This concentration gradient results in a net negative charge on the inside of the membrane and a positive charge on the outside. Ion channels and ion pumps are very specific; they allow only certain ions through the cell membrane. For example, potassium channels will allow only potassium ions through, and the sodium-potassium pump acts only on sodium and potassium ions.
All cells have an electrical charge which is due to the concentration gradient of ions that exists across the membrane. The number of positively charged ions outside the cell membrane is greater than the number of positively charged ions in the cytosol. This difference causes a voltage difference across the membrane. Voltage is electrical potential energy that is caused by a separation of opposite charges, in this case across the membrane. The voltage across a membrane is called membrane potential. Membrane potential is the basis for the conduction of nerve impulses along the cell membrane of neurons. Ions that are important in the formation of a nerve impulse include sodium (Na+) and potassium (K+).
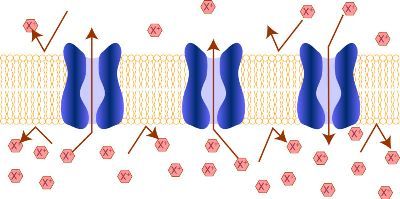
Figure 20.5
Channel proteins in the plasma membrane. Membrane channel proteins (or channel proteins), allow the movement of specific ions across the cell membrane, in this case the hypothetical X ion. The concentration gradient results in electrical potential energy building up across the membrane, the basis for the conduction of a nerve impulse.
Resting Potential
When a neuron is not conducting a nerve impulse, it is said to be at rest. The resting potential is the resting state of the neuron, during which the neuron has an overall negative charge. In neurons the resting potential is approximately -70 milliVolts (mV). The negative sign indicates the negative charge inside the cell relative to the outside.
The reasons for the overall negative charge of the cell include:
- The sodium-potassium pump removes Na+ ions from the cell by active transport. A net negative charge inside the cell is due to the higher concentration of Na+ ions outside the cell than inside the cell.
- Most cells have potassium-selective ion channel proteins that remain open all the time. The K+ ions move down the concentration gradient (passively) through these potassium channels and out of the cell, which results in a build-up of excess positive charge outside of the cell.
- There are a number of large, negatively charged molecules, such as proteins, inside the cell.
Action Potential
An action potential is an electrical charge that travels along the membrane of a neuron. It can be generated when a neuron’s membrane potential is changed by chemical signals from a nearby cell. In an action potential, the cell membrane potential changes quickly from negative to positive as sodium ions flow into and potassium ions flow out of the cell through ion channels, as shown in Figure below.
The change in membrane potential results in the cell becoming depolarized. An action potential works on an all-or-nothing basis. That is, the membrane potential has to reach a certain level of depolarization, called the threshold, otherwise an action potential will not start. This threshold potential varies, but is generally about 15 millivolts (mV) more positive than the cell's resting membrane potential. If a membrane depolarization does not reach the threshold level, an action potential will not happen. You can see in Figure below how two depolarizations did not reach the threshold level of -55mV. The first channels to open are the sodium ion-channels, which allow sodium ions to enter the cell. The resulting increase in positive charge inside the cell (up to about +40 mV) starts the action potential. Potassium ion-channels then open up, allowing potassium ions out of the cell, which ends the action potential. Both of the ion channels then close, and the sodium-potassium pump restores the resting potential of -70 mV. The action potential will move down the axon toward the synapse like a wave would move along the surface of water.
In myelinated neurons, ion flows occur only at the nodes of Ranvier. As a result, the action potential signal "jumps" along the axon membrane, from node to node, rather than spreading smoothly along the membrane, as they do in axons that do not have a myelin sheath. This is due to clustering of Na+ and K+ ion channels at the Nodes of Ranvier. Unmyelinated axons do not have Nodes of Ranvier; and ion channels in these axons are spread over the entire membrane surface.

Figure 20.6
The movement of an action potential down an axon. A chemical message from another nerve causes the sodium ion channels at one point in the axon to open. Sodium ions rush across the membrane and cause the interior of the axon to become positively charged (depolarized) because the cell now contains more positive charges. Potassium ion channels then open and potassium ions flow out of the cell, which end the action potential. The action potential then moves down the axon membrane toward the synapse.
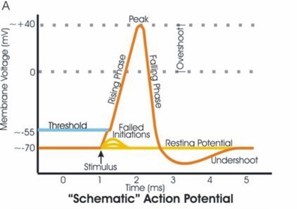
Figure 20.7
The changes in membrane potential during an action potential. Note the failed initiations that did not start an action potential. These depolarizations did not reach the threshold level (of about -55mV), so they did not start an action potential.
Types of Neurons
Neurons are highly specialized for the processing and transmission of cellular signals and can be classified by their structure or function. Structural classification is based on the number of dendrites and axons that a cell has. Functional classification groups neurons according to the direction in which the nerve impulse is moving in relation to the CNS.
We will discuss the three functional groups of nerves:
-
Sensory neurons carry signals from tissues and organs to the central nervous system and are sometimes also called afferent neurons. Sensory neurons typically have a long dendrite and short axon. Sensory neurons are found in reflex arcs and are involved in several forms of involuntary behavior, including pain avoidance.
-
Motor neurons carry signals from the central nervous system to muscles and glands and are sometimes called efferent neurons. Motor neurons have a long axon and short dendrites.
-
Interneurons connect sensory and motor neurons in neural pathways that go through the central nervous system. Interneurons are also called association or relay neurons. Interneurons are found only in the central nervous system where they connect neuron to neuron.
Communication Between Neurons
Neurons communicate with each other at specialized junctions called synapses. Synapses are also found at junctions between neurons and other cells, such as muscle cells like the one shown in Figure below. To see a synapse between two neurons, refer to Figure above.
There are two types of synapses:
-
chemical synapses use chemical signaling molecules as messengers
-
electrical synapses use ions as messengers
We will primarily discuss chemical synapses in this chapter. The axon terminal of one neuron usually does not touch the other cell at a chemical synapse. Between the axon terminal and the receiving cell is a gap called a synaptic cleft. The transmitting cell is called the presynaptic neuron, and the receiving cell is called the postsynaptic cell or if it is another neuron, a postsynaptic neuron.

Figure 20.8
A synapse between a neuron and a muscle cell. The connection between a neuron and a muscle cell, called a . The finger-like projections of the axon are the axon terminals. An action potential moves down to the axon terminals where it causes a chemical message called a neurotransmitter to be released into the synaptic cleft. The neurotransmitter then causes an action potential to start on the membrane of the muscle cell.
Your brain has a huge number of synapses. Each of your 1012 (one trillion) neurons—including glial cells—has on average 7,000 synaptic connections to other neurons. It has been estimated that the brain of a three-year-old child has about 1016 synapses (10 quadrillion). This number declines with age, and levels off by adulthood. An adult has between 1015 and 5 x 1015 synapses (1 to 5 quadrillion).
Neurotransmitter Release
When an action potential reaches the axon terminal, it causes the neurotransmitter vesicles to fuse with the terminal membrane, and the neurotransmitter is released into the synaptic cleft. A neurotransmitter is a chemical message that is used to relay electrical signals between a neuron and another cell. Neurotransmitter molecules are made inside the presynaptic neuron and stored in vesicles at the axon terminal. Some neurons make only one type of neurotransmitter, but most neurons make two or more types of neurotransmitters.
When an action potential reaches the axon terminal, it causes the neurotransmitter vesicles to fuse with the terminal membrane. Neurotransmitter is released into the synaptic cleft. The neurotransmitters then diffuse across the synaptic cleft and bind to receptor proteins on the membrane of the postsynaptic cell, as shown in Figure below.

Figure 20.9
The synaptic cleft. Neurotransmitter that is released into the synaptic cleft diffuses across the synaptic membrane and binds to its receptor protein on the post synaptic cell.
Neurotransmitter Action
Many types of neurotransmitters exist, a few of which are listed in Table below. Neurotransmitters can have an excitatory or inhibitory effect on the postsynaptic cell. An excitatory neurotransmitter initiates an action potential and an inhibitory neurotransmitter prevents one from starting. Glutamate is the most common excitatory transmitter in the body while GABA and glycine are inhibitory neurotransmitters. The release of acetylcholine, an excitatory neurotransmitter causes an inflow of positively charged sodium ions (Na+) into the postsynaptic neuron. This inflow of positive charge causes a depolarization of the membrane at that point. The depolarization then spreads to the rest of the postsynaptic neuron. Acetylcholine is the neurotransmitter that initiates muscle movement.
The effect of a neurotransmitter also can depend on the receptor it binds to. That is, a single neurotransmitter may be excitatory to the receiving neuron, or it may inhibit such an impulse by causing a change in the membrane potential of the cell. Synapses too can be excitatory or inhibitory and will either increase or decrease activity in the target neuron, based on the opening or closing of ion channels.
Common Neurotransmitters and Their Receptors
|
Name
|
Receptor Name and Type
|
Ions Involved
|
|
Glutamate (glutamic acid)
|
Glutamate receptors (ligand-gated ion channels and G protein-coupled receptors)
|
Ca2+, K+, Na+
|
|
Acetylcholine
|
Acetylcholine receptors (ligand-gated ion channel)
|
Na+
|
|
Norepinephrine (noradrenaline)
|
Adrenoceptors (G protein-coupled receptors)
|
Ca2+
|
|
Epinephrine (adrenaline)
|
Adrenoceptors (G protein-coupled receptors)
|
Ca2+
|
|
Serotonin (5-hydroxytryptamine)
|
5-HT receptors 5-HT3 is a ligand-gated ion channel
5-HT1, 5-HT2, 5-HT4, 5-HT5A, 5-HT7 are G protein-coupled receptors
|
K+, Na+
|
|
Gamma-aminobutyric acid (GABA)
|
GABAA and GABAC (ligand-gated ion channels) GABAB (G protein-coupled receptors)
|
Cl- K+
|
|
Histamine
|
Histamine receptors (H1, H2, H3, H4) (G protein-coupled receptors)
|
|
Neurotransmitter receptors can be gated ion channels that open or close through neurotransmitter binding or they can be protein-linked receptors. Protein-linked receptors are not ion channels; instead they cause a signal transduction that involves enzymes and other molecules (called second messengers) in the postsynaptic cell. Refer to the Cell Structure and Function chapter for more information about signal transduction mechanisms.
Neurotransmitter Reuptake
Many neurotransmitters are removed from the synaptic cleft by neurotransmitter transporters in a process called reuptake. Reuptake is the removal of a neurotransmitter from the synapse by the pre-synaptic neuron. Reuptake happens after the neurotransmitter has transmitted a nerve impulse. Without reuptake, the neurotransmitter molecules might continue to stimulate or inhibit an action potential in the post-synaptic neuron. The process of release and reuptake of neurotransmitters is shown in Figure below.

Figure 20.10
A synapse before and during reuptake. Neurotransmitter transporter proteins (also called reuptake pumps) release the neurotransmitter and also reuptake it from the synaptic cleft. Reuptake is a way of controlling the effect the neurotransmitter has on the post-synaptic cell.
Re-uptake is carried out by transporter proteins which bind to the released transmitter and actively transport it across the plasma membrane into the pre-synaptic neuron. The reuptake of neurotransmitter is the target of some types of medicine. For example, serotonin is a neurotransmitter that is produced by neurons in the brain. Serotonin is believed to play an important role in the regulation of mood, emotions, and appetite. After release into the synaptic cleft, serotonin molecules either attach to the serotonin receptors (called 5-HT receptors) of the post-synaptic neuron, or they attach to receptors on the surface of the presynaptic neuron that produced the serotonin molecules, for reuptake. Reuptake is a form of recycling because the neuron takes back the released neurotransmitter for later use. Medicines called selective serotonin reuptake inhibitors (SSRIs) block the reuptake of the neurotransmitter serotonin. This blocking action increases the amount of serotonin in the synaptic cleft, which prolongs the effect of the serotonin on the postsynaptic neuron. Some scientists hypothesize that decreased levels of serotonin in the brain are linked to clinical depression and other mental illnesses. So SSRI medications such as sertraline and fluoxetine are often prescribed for depression and anxiety disorders.
Another way that a neurotransmitter is removed from a synapse is digestion by an enzyme. At cholinergic synapses (where acetylcholine is the neurotransmitter), the enzyme acetylcholinesterase breaks down the acetylcholine.
Neurotransmitters and Disease
Diseases that affect nerve communication can have serious consequences. A person with Parkinson's disease has a deficiency of the neurotransmitter dopamine. Progressive death of brain cells that produce dopamine increases this deficit, which causes tremors, and a stiff, unstable posture. L-dopa is a chemical related to dopamine that when given as a medicine, eases some of the symptoms of Parkinson’s disease. The L-dopa acts as a substitute neurotransmitter, but it cannot reverse the disease.
The soil bacterium Clostridium tetani produces a neurotoxin that causes the disease tetanus. The bacteria usually get into the body through an injury caused by an object that is contaminated with C. tetani spores, such as a puncture wound caused by stepping on a nail. The C. tetani neurotoxin blocks the release of the neurotransmitter GABA, which causes skeletal muscles to relax after contraction. When the release of GABA is blocked, the muscle tissue does not relax and remains contracted. Tetanus can be fatal when it affects the muscles used in breathing. Thankfully, tetanus is treatable and can be prevented by vaccination.
Another bacterium called Clostridium botulinum produces a toxin that is occasionally found in preserved foods that have been improperly sterilized. The toxin causes a disease called botulism. Botulin toxin blocks the release of the excitatory neurotransmitter acetylcholine. Blockage of acetylcholine causes the progressive relaxation of muscles because they are unable to contract. Paralysis of the muscles used for breathing can be fatal unless the patient is treated with a respirator.
Synapses and Recent Research
Recent studies have found that electrical synapses are more common in the central nervous system than were previously thought. An electrical synapse is a link between two neighboring neurons that is formed at a narrow gap between the pre- and postsynaptic cells called a gap junction. At gap junctions, cells are about 3.5 nm from each other, a much shorter distance than the 20 to 40 nm distance that separates cells at chemical synapses.

Figure 20.11
Electrical synapses. Electrical synapses are more common in the nervous system than was once thought. Cell signaling at electrical synapses is much faster than signaling at chemical synapses. The image at the bottom left of the figure shows the location of gap junctions between cells.
Each gap junction has many channels which cross the plasma membranes of both cells, as is shown in Figure above. Gap junction channels are wide enough to allow ions and even medium sized molecules like signaling molecules to flow from one cell to the next. For example, when positive ions move through the channel into the next cell, the extra positive charges depolarize the postsynaptic cell.
Signaling at electrical synapses is faster than the chemical signaling that occurs across chemical synapses. Ions directly depolarize the cell without the need for receptors to recognize chemical messengers, which occurs at chemical synapses. Such fast communication between neurons may indicate that in some parts of the brain large groups of neurons can work as a single unit to process information. Electrical synapses are numerous in the retina and cerebral cortex.
In addition to neurons, glial cells are an important part of the nervous system. The word glia means "glue" in Greek. Glial cells can be thought of as partners to neurons by aiding in the maintenance of homeostasis, signal transduction, formation of myelin and providing support and nutrition. The importance of neurons as the conductive cells of the nervous system, known as the neuron doctrine, has been questioned by recent research. The role of glial cells in processing neural information has begun to be appreciated more. There are far more glial cells than neurons, it has been estimated that glial cells outnumber neurons by as many as 50:1.
Central Nervous System
The central nervous system (CNS), which includes the brain and the spinal cord, shown in Figure below, represents the largest part of the nervous system. The brain is the central control of the nervous system. The spinal cord carries nerve impulses from the brain to the body and from the body to the brain. Together with the peripheral nervous system (PNS), which includes all nervous tissue outside of the central nervous system, it controls virtually every activity in the body. The brain is protected by the skull and the spinal cord is protected by the vertebrae. An overview of the CNS can be viewed at http://vimeo.com/2024719.

Figure 20.12
The components of the central nervous system (CNS).
The Brain
The brain is the most complex organ in the body. The brain contains about 100 billion neurons each of which can be connected to tens of thousands of other neurons within the brain. The brain is the source of what makes us human; the conscious mind. The mind is the set of cognitive processes related to perception, interpretation, imagination, memories, and language. Beyond cognitive functions, the brain regulates processes related to homeostasis such as respiration and heartbeat. An average adult human brain weighs between 1 and 1.5 kg (3 lb). An adult brain uses about 20-25% of the total energy used by the body, while the developing brain of an infant consumes around 60% of total energy used by the body.
The brain can be classified by the processes its different parts control. The cerebrum generally controls conscious functions such as problem-solving and speech, while the midbrain and the brain stem are more involved with unconscious (autonomic) functions such as breathing, heartbeat, and temperature regulation. The cerebellum is involved in coordination and control of body movement. For a video of "Brain Basics," see http://www.teachers.tv/video/13838.
Cerebrum
The cerebrum is what most people would think of as the "brain." The cerebrum lies on top of the brainstem. It is made up of two cerebral hemispheres, which are shown in Figure below. The two cerebral hemispheres are connected to each other at the corpus callosum, the light-colored X-shaped structure in the center of the image. The corpus callosum is a wide, flat bundle of axons found deep inside the brain. Mammals (including humans), have the largest and most well-developed cerebrum among all species.

Figure 20.13
A magnetic resonance image (MRI) of the human brain in which the two hemispheres of the cerebrum can be seen.
Each hemisphere of the cerebrum can be divided into four parts, or lobes. These are: the frontal lobe, the parietal lobe, the temporal lobe, and occipital lobe. Researchers have identified a number of functional areas within each lobe, some of which are listed in Table below. Both hemispheres look identical, but there are functional differences between them. For example, there are differences between the centers of function for spatial awareness between right and left-handed people. Each cerebral hemisphere receives sensory information and controls muscle movements of the opposite side of the body. The right hemisphere controls the left side of the body, and the left hemisphere controls the right side of the body.
Functions Controlled by the Cerebral Lobes
|
Lobe
|
Functions
|
|
Frontal
|
Speech, intellectual function (reasoning, abstract thought), touch
|
|
Parietal
|
Speech, taste, reading
|
|
Temporal
|
Hearing, smell
|
|
Occipital
|
Vision
|

Figure 20.14
The lobes of the cerebral cortex-frontal, temporal, occipital, and parietal. The cerebellum (purple) and brain stem (gray) are not part of the hindbrain. In vertebrates, a gross division into three major parts is used.
The cerebral cortex is the highly-folded outer layer of the cerebrum that is between 2 mm and 4 mm thick. The lobes that make up the cerebral cortex, shown in Figure above, are named after the skull bones that cover those areas of the brain. The many folds in the cortex allow for the large surface area of the brain to fit inside the skull. The cerebral cortex controls higher functions, such as consciousness, reasoning, emotions, and language. It also controls sensory functions such as touch, taste, smell, and responses to external stimuli. In the cerebrum, and found below the cerebral cortex, is the white matter. White matter is made up of myelinated axons that act as “cables” that link up certain parts of the right and left hemispheres.
Diencephalon
The diencephalon is the region of the brain that includes structures such as the thalamus, the hypothalamus, and a portion of the pituitary gland. The thalamus is believed to “translate” sensory signals for the cerebral cortex. The thalamus also plays an important role in regulating states of sleep and wakefulness. The hypothalamus gland controls certain metabolic processes and other autonomic activities such as body temperature, hunger, thirst, and circadian cycles. The hypothalamus also makes and releases neurotransmitters that control the action of the pituitary gland. The thalamus, hypothalamus, and hippocampus together are considered part of a set of structures called the limbic system. The limbic system is considered the “emotional center” of the brain.
Brain Stem
Sometimes called the “lower brain,” the brain stem is the lower part of the brain that is joined to the spinal cord. There are three parts to the brainstem: the midbrain, the pons, and the medulla oblongata, shown in Figure 15. The midbrain is more involved with unconscious, autonomic functions. The midbrain deals with several types of sensory information including sound and sight. It also “translates” sensory information to be sent to the forebrain. The brainstem also helps coordinate large body movements such as walking and running. The pons relays messages to different parts of the brain (the cerebrum and cerebellum), and helps regulate breathing. Some researchers propose that it has a role in dreaming. The medulla oblongata, also called the medulla, shares some of the function of the pons. It controls several homeostatic functions that you are usually unaware of, such as breathing, heart and blood vessel activity, swallowing, and digestion.
One of the brain stem’s most important roles is that of an “information highway.” That is, all of the information coming from the body to the brain (sensory) and the information from the cerebrum to the body (motor) go through the brain stem. Sensory pathways for such things as pain, temperature, touch, and pressure sensation go upward to the cerebrum, and motor pathways for movement and other body processes go downward to the spinal cord. Most of the axons in the motor pathway cross from one side of the CNS to the other as they pass through the medulla oblongata. As a result, the right side of the brain controls much of the movement in the left side of the body, and the left side of the brain controls much of the movement in the right side of the body.
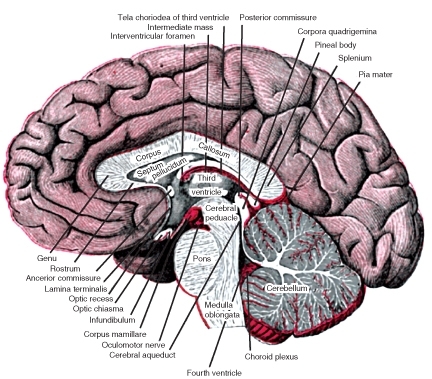
Figure 20.15
The locations of the brainstem and cerebellum. The brainstem is in the center of this image. It is made up of the pons, medulla oblongata, and the midbrain. The cerebellum is the red structure to the right of the brainstem.
Cerebellum
The cerebellum is found just below the occipital lobe of the cerebrum. It plays an important role in coordination and the control of body movements. Many nerve pathways link the cerebellum with motor neurons, which are neurons that send information to the muscles causing them to move, and a group of nerves that provides information on the position of the body in space. The cerebellum processes information from both these pathways, and uses the feedback on body position to fine-tune body movements. Hand-eye coordination is an example of such a function. If the cerebellum is damaged, there will not be paralysis, but the fine movement of the body (such as hand-eye coordination), balance, posture, and the ability to learn new motor skills will be negatively affected. The cerebellum is the purple structure in Figure above. A section of the cerebellum is shown in Figure above.
Spinal Cord
The spinal cord is a thin, tubular bundle of nervous tissue that extends from the medulla oblongata and continues to the lower back, where it ends in a group of fibrous extensions. It is protected by the spinal vertebrae. The main function of the spinal cord is as an information superhighway that links the sensory messages from the body to the brain. The outer cortex of the cord contains white matter (myelinated sensory and motor neurons). The central region, the grey matter, is made up of unmyelinated neurons. A cross section of the spinal cord is shown in Figure below.

Figure 20.16
A cross section of the spinal cord. The central butterfly-shaped area is the gray matter and the area that surrounds it is the outer cortex (made up of white matter). Instructions go to the bodys muscles and other areas through the motor neurons that leave the spinal cord in the spinal nerves. Sensory information from the body enters the spinal cord through sensory neurons.
Peripheral Nervous System
The peripheral nervous system (PNS) consists of the nervous tissue that lies outside the central nervous system, shown in Figure below. The nervous tissue of the peripheral nervous system serves the limbs and organs. The central nervous system interacts with the peripheral nervous system through twelve pairs of cranial nerves that connect the brain to areas of the head and neck and 31 pairs of spinal nerves that connect the spinal cord (and CNS) to the rest of the body, such as the internal organs, arms, and legs. A nerve is an enclosed, cable-like bundle of axons. Unlike the central nervous system, the peripheral nervous system is not protected by bone, making it more vulnerable to toxins and injuries.
Spinal nerves originate from the spinal cord. They control functions of the rest of the body. Each spinal nerve has a dorsal root and a ventral root, which are shown in Figure below. The dorsal root is the “nerve highway” that carries sensory information from sensory receptors in the body to the CNS. The ventral root contains axons of motor neurons which carry information away from the CNS to the muscles and glands of the body.
These two nerve “highways” are actually parts of two subdivisions of the PNS. The sensory division, also known as the afferent division, carries sensory information from sensory receptors in the body to the CNS. The sensory division keeps the CNS constantly updated on events happening inside and outside the body. The motor division, or efferent division, carries nerve impulses from the CNS to the muscles, glands and organs of the body. The nerve impulses of the motor division cause muscles to contract and cause glands to secrete chemical signals.

Figure 20.17
The peripheral nervous system (PNS). The peripheral nervous system extends from the CNS and reaches out to all parts of the body, from the cranial nerves found in the head to the plantar nerves in the tips of the toes.

Figure 20.18
A cross section of the spinal cord. The central butterfly-shaped area (1, 2, 3) is the gray matter, the outer cortex is the white matter. Instructions going to the bodys muscles and other areas go through the motor neurons that leave the spinal cord in the ventral roots (11). Sensory information from the body enters the spinal cord through sensory neurons in the dorsal roots (12). Dorsal and ventral roots occur on both sides of the spinal cord, only one side is shown in this diagram.
Somatic and Autonomic Nervous Systems
The motor division of the peripheral nervous system is divided into the somatic nervous system and the autonomic nervous system:
The somatic nervous system is the part of the PNS that is associated with the conscious (voluntary) control of the body through the movement of skeletal muscles and the perception of external stimuli through senses such as touch, hearing, and sight. The system includes all the neurons connected with muscles, skin and sense organs. The somatic nervous system is made up of sensory nerves that receive sensory information from the external environment, and motor nerves responsible for muscle contraction.
Together with interneurons, the sensory and motor neurons are found in a reflex arc. A reflex is an automatic (involuntary) action caused by a defined stimulus and carried out through a reflex arc. For example, a person stepping on a sharp object would start the reflex action through the creation of a stimulus, (pain) within specialized pain receptors located in the skin tissue of the foot. The resulting stimulus would be passed along sensory neurons to the spinal cord. This stimulus is usually processed by an interneuron to create an immediate response to pain by initiating a motor response in the muscles of the leg which pull the foot away from the object. This reflexive action would occur as the pain sensation is arriving in the brain. A reflex arc is shown in Figure below.

Figure 20.19
The components of a reflex. A sensory receptor that detects a stimulus and sends nerve signals to the spinal cord. These signals activate motor neurons that lead back to the effector (muscle).
The autonomic nervous system (ANS) is the part of the peripheral nervous system that maintains homeostasis in the body. Your body carries out most of these maintenance activities without your conscious control, which is why the autonomic nervous system is also called the involuntary nervous system. The ANS has far reaching effects, such as the control of heart rate, digestion, respiration rate, salivation, and perspiration. Some autonomic nervous system functions work in line with the conscious mind, such as breathing.
The ANS is also made up of the sensory and motor neurons that send messages to and from the internal organs. These neurons form reflex arcs that pass through the medulla oblongata. This explains why even a person's cerebrum may experience trauma, yet their cardiovascular, digestive and respiratory functions will continue even if higher level functions such as awareness and consciousness, are lost. Such a low level of brain functioning is referred to as a vegetative state.
The ANS has two subdivisions: the sympathetic division and parasympathetic division. The sympathetic division generally stimulates body systems during emergency situations. It gets the body ready for "fight or flight," which would probably be required by the situation shown in Figure below, while the parasympathetic division controls non-emergency functions such as digestion. The relationship between the divisions of the nervous system is illustrated in Figure below.

Figure 20.20
Watch out! A situation in which your sympathetic nervous system (and hopefully your somatic nervous system), would be firing at full speed.

Figure 20.21
Levels of Organization of the Nervous System.
Sense Organs and Sensory Perception
Your senses are your body’s means of making sense of the information your nervous system receives from inside your body and from the outside world. Your senses enable you to adapt to change in your environment and survive. The sensory division of the peripheral nervous system is organized into highly developed sense organs, which are groups of tissues that work together in responding to a specific kind of physical stimulus, such as the stimulus in Figure below. The sense organs correspond to a defined region (or group of regions) within the brain where the nerve signals are received and interpreted. Your sense organs include your eyes, ears, nose, mouth, and skin. They all have sensory receptors that are specific for certain stimuli. For example, the nose has sensory receptors for odors (smells). Sensory neurons send nerve impulses from sensory receptors to the central nervous system. The brain then interprets the nerve impulses to form a response.

Figure 20.22
Can you smell these fresh, juicy oranges and kumquats? Your senses of smell, taste and sight are also important in developing an appetite. Just think of how appetizing these fruits would be if they were blue, crunchy, and smelled like burned toast.
A sensory receptor is a cell, or a group of cells that detect stimuli. Sensory receptors can be classified based on the type of stimuli to which they respond.
-
Chemoreceptors respond to chemical stimuli.
-
Mechanoreceptors respond to mechanical stress or strain (movement).
-
Thermoreceptors respond to temperature changes.
-
Photoreceptors respond to variations in light.
-
Baroreceptors respond to pressure.
Specific areas of the brain interpret information from each sense organ. For example, regions of the occipital lobe interpret nerve impulses that come from the sensory receptors of the eyes, and regions of the temporal lobe interpret sensory information from the ears through the nerves that enter the brain in these areas, as shown in Figure below. It is generally agreed that there are at least seven different senses in humans. These are sight, sound, taste, smell, touch, balance, and body awareness (the sense of knowing where the regions of your body are located at any one time). At least two other senses that humans do not have are observed in other organisms. Examples include electroreception, the ability to detect electric fields, and magnetoreception, the ability to detect magnetic fields.

Figure 20.23
The entry of sensory nerves into the brain. Among other nerves, the sensory nerves for smell, sight, hearing, and taste (yellow structures) can be seen entering the skull. You can also see how the cerebrum, thalamus, cerebellum, and brain stem are nested within the skull.
Sight
Sight or vision describes the ability of the brain and eye to detect certain wavelengths of electromagnetic radiation (light), and interpret the image as "sight." Different receptors are responsible for the perception of color (the frequency of photons of light) and perception of brightness (number of photons of light). Photoreceptors are found in the retina, shown in Figure below.

Figure 20.24
The structure of the eye. The macula is a spot near the center of the retina that has a diameter of about 1.5 mm. Near its center is the fovea, a small pit that contains the largest concentration of cone cells in the eye and is responsible for central vision. The macula is the point of sharpest vision. A video of the human eye is available at
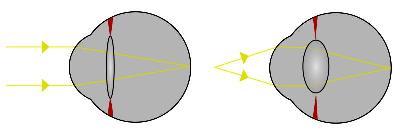
Figure 20.25
Focusing light in the retina. This diagram shows how light from a distant source is bent by the stretched lens to strike the retina, and how light from a closer source is bent even more sharply by the relaxed lens to strike the retina.
The structure of the eye owes itself completely to the task of focusing light onto the retina, the light-sensitive inner layer of the eye. First, light passes through a clear protective layer called the cornea, shown in Figure above. Light then passes through the pupil, which is the opening in the iris, and into the interior of the eye. After passing through the pupil, the light then travels through the lens, a transparent, biconvex structure that, along with the cornea, helps to focus light on the retina. Muscles attached to the lens change the shape of the lens to bend the light rays so that they focus on the retina, as shown in Figure above. Light hitting the retina causes chemical changes in the photosensitive cells of the retina, the products of which trigger nerve impulses which travel to the brain along the optic nerve.
The retina has two forms of photosensitive cells important to vision—rods and cones. Rod cells are highly sensitive to light which allows them to respond in dim light and dark conditions, but, they cannot detect color. These are the cells which allow humans and other animals to see by moonlight, or in a dimly-lit room. This is why the darker conditions become, the less color objects seem to have. Cone cells respond to different wavelengths of bright light to initiate a nerve impulse. They are also responsible for the sharpness of images. Cones do not respond well in poor light conditions, which is the reason why you see things in dim light as fuzzy shades of gray.
Humans have three different types of cone cells that respond to different wavelengths of light. These cone cells contain a pigment that absorbs the energy from different wavelengths of light to initiate a nerve impulse. Activation of the visual pigments by certain wavelengths of light opens ion channels on the membrane of the cone or rod cell. This leads to an action potential that is carried by the millions of neuron axons that make up the optic nerve to the visual centers of the brain. The brain integrates the nerve impulses from the cone cells and perceives the world in all the colors of the visual spectrum. A person who is colorblind has damaged or missing cones, and is unable to perceive certain colors.
Hearing
Hearing is the sense of sound perception that results from the movement of tiny hair fibers in the inner ear. These hairs detect the motion of a membrane which vibrates in response to changes in air pressure. Sound can also be detected as vibrations that are conducted through the body. Sound wave frequencies that are too low or too high to be heard by the ear can be detected this way. Audible sound is sensed by the ear.
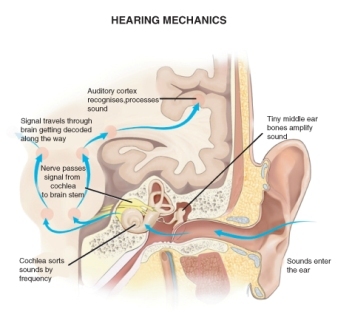
Figure 20.26
The detection of sound by your ear.
The folds of cartilage surrounding the outer ear canal are called the pinna. Sound waves are gathered by the pinna, and channeled down the auditory canal, a tube-shaped opening of the ear which ends at the tympanic membrane, or eardrum.
Sound waves traveling through the ear canal hit the eardrum and cause it to vibrate. This wave information travels across the air-filled middle ear cavity through a group of three tiny, delicate bones: the hammer, the anvil, and the stirrup, shown in Figure above. This group of bones transfers the eardrum vibrations to another membrane called the oval window. The oval window separates the middle ear from the inner ear. The inner ear contains the cochlea.
The cochlea is a coiled tube that is filled with a watery liquid, which moves in response to the vibrations coming from the middle ear through the oval window. As the fluid moves, thousands of mechanoreceptors called hair cells bend, releasing a neurotransmitter. The neurotransmitter causes an action potential in the neurons of the auditory nerve. The action potential travels along the auditory nerve to structures in the brainstem, then to the thalamus, and then to the auditory centers of the brain in the temporal lobe of the cerebral cortex.
A very strong movement of the fluid within the cochlea, caused by very loud noise, can kill hair cells. This is a common cause of partial hearing loss and is the reason why users of firearms or heavy machinery should wear earmuffs or earplugs. Destruction of the hair cells usually leads to permanent hearing loss because once destroyed, the hairs do not generally grow back.
Balance and the Ears
It might be hard to believe, but your ears are also in charge of your sense of balance! The semicircular canals are three fluid-filled interconnected tubes found inside each ear. They can be seen in Figure above, directly above the cochlea. The canals are positioned at angles between 95 to 115 degrees relative to one another. The angles between the canals are not perpendicular, so movements of the head cause movement of fluid in two canals at the same time.
Each canal is filled with fluid called endolymph and motion sensors with little hairs, called cilia, line each canal. Movement of the head and body cause the endolymph in the canals to move about. The hair cells sense the strength and direction of the fluid’s movement and send electrical signals to the cerebellum which interprets the information and responds to help keep the body’s sense of balance. The interaction of the semicircular canals and the cerebellum allow the performer in Figure below to do his act.

Figure 20.27
Good balance required! This performers sense of balance is dependent on communication between his semicircular canals and his cerebellum.
When the sense of balance is interrupted it causes dizziness and nausea. Balance can be upset by an inner ear infection, a bad head cold or a sinus infection, or a number of other medical conditions. It can also be temporarily disturbed by rapid and repetitive movement, for example riding on a merry-go-round or spinning around in a circle.
Taste and Smell
Taste is one of the two main chemical senses, the other being smell. There are at least four types of taste receptors on the tongue. Taste stimuli from each receptor type send information to a different region of the brain. The four well-known receptors detect sweet, salt, sour, and bitter. The existence of a fifth receptor, for a sensation called umami, was confirmed in 2000. The umami receptor detects the amino acid glutamate, which causes a savory, “meaty” flavor in foods.

Figure 20.28
The location of taste buds. Most of the taste buds in the mouth are embedded in the papillae, the little bumps that cover the tongue. The deep groove (fissure) that runs down the center of the tongue in this photo is a common and perfectly normal condition.
The chemoreceptors of the mouth are the taste cells that are found in bundles called taste buds. Most of the taste buds are embedded within the tiny papillae or “bumps” that cover the tongue, shown in Figure above. Each receptor has a different way of detecting certain compounds and starting an action potential which alerts the brain. The compounds bind to receptors in the taste cells and stimulate neurons in the taste buds. The action potential moves along the facial nerves to the thalamus and then to the taste center of cerebral cortex for interpretation by the brain. The tongue can also feel sensations that are not generally called tastes. These include: temperature (hot or cold), coolness (as in “minty” or “fresh”), spiciness or hotness (peppery), and fattiness (greasy).
Smell is the other "chemical" sense. The chemoreceptors of smell are called olfactory receptors. About 40 million olfactory receptor neurons line the nasal passages. Different odor molecules bind to and excite specific olfactory receptors. The combination of excitatory signals from different receptors makes up what we identify as “smell.” Signals from the olfactory receptors travel along nerves to the olfactory bulb in the brain where they then move to the smell center in the frontal lobe of the cerebral cortex. Olfactory receptor neurons in the nose differ from most other neurons in that they die and regenerate on a regular basis. A dog’s keen sense of smell is due to the large area of its nasal passages that are covered by olfactory receptors, and the large number of nerves that bring nerve impulses from the receptors to its brain. For example, the area in which olfactory receptors are located inside the human nose (called the olfactory epithelium), which is shown in Figure below, measures about 12 cm2. The olfactory epithelium of some dogs’ noses can measure about 150 cm2!
Have you ever noticed that you cannot taste anything when your nose is stuffed up? That is because your senses of smell and taste are closely linked. This is due to the fact that your nasal cavity, located behind the nostrils, connects to your mouth at the back of your throat, as shown in Figure below. Your olfactory receptors and taste receptors both contribute to the flavor of food. Your tongue can only tell among a few different types of taste, while your nose can distinguish among hundreds of smells, even if only in tiny amounts.

Figure 20.29
The location of olfactory nerves. Olfactory receptors and their associated nerves (yellow) line the top of the nasal passages. Nerve messages from the receptors are sent to the brain to be interpreted as certain smells.
Touch, Pressure, and Pain
Touch is the sense of pressure perception, which is generally felt in the skin. There are a variety of pressure receptors that respond to variations in pressure and tension. Mechanoreceptors are most numerous on the tongue, lips, face, palms (including fingertips), and soles of the feet.
There are several types of pain receptors, called nociceptors, which respond to potentially damaging stimuli. They are mostly found in the external parts of the body such as the skin, cornea, and mucous membranes, but are also found in muscles, joints, and some internal organs. Nociceptors are classified according to the stimuli to which they respond: thermal, mechanical or chemical. But some receptors respond to many different damaging stimuli of a chemical, thermal, or mechanical nature. Thermal receptors are activated by potentially harmful heat or cold, temperatures above 45°C and below 5°C. Mechanical receptors respond to excess pressure, squeezing, or bending, the type of painful stimuli that a cactus such as the one in Figure below would cause. Together these nociceptors allow the organism to feel pain in response to damaging pressure, excessive heat, excessive cold and a range of chemicals, the majority of which are damaging to the tissue surrounding the nociceptor.

Figure 20.30
Mechanical pain receptors in your skin would warn you if you got too close to this prickly cactus.
Drugs and the Nervous System
A drug is any chemical or biological substance that affects the body’s structure or functions. Drugs in the form of medicines are used to treat many illnesses and disorders. A medicine (or medication), is a drug that is taken to cure or reduce the symptoms of an illness. However, drugs, whether they are medicines, legal or illegal drugs, can be abused for the effects they have on the central nervous system (CNS). In fact many medical uses of drugs depend on the powerful effect they have on brain function. For example, anti-depression medicines are used to treat depression and anxiety disorders, and antipsychotic medicines are used to treat schizophrenia and bipolar disorder.
A psychoactive drug is a substance that affects the central nervous system by altering cognitive function. Change in cognitive function results in changes in how a person feels, thinks, perceives, and acts. Almost everyone has used a psychoactive drug at some time in their life, and many people take such drugs daily. For example, the coffee or tea that you may have drank to waken yourself up this morning, or the cola, energy drink, or chocolate that you had as a snack contain the psychoactive drug caffeine. Caffeine is a CNS stimulant that makes you feel less drowsy and more alert. Coffee beans, the most common source of caffeine, are shown in Figure below.

Figure 20.31
Roasted coffee beans. Coffee beans are a common source of the stimulant caffeine. Other plant sources include the leaves of tea, cocoa, yerba mate, and guarana plants. These plants use caffeine as a means of protection against being eaten. The caffeine in the leaves of these plants can paralyze and kill the insects that feed upon them.
Drugs and the Brain: How Psychoactive Drugs Work
How we perceive stimuli, feel, think, and do is a result of neurons sending action potentials and neurotransmitters to each other and to other cells in the body. Psychoactive drugs affect how neurons communicate with each other. These drug molecules can alter neurotransmission, by blocking receptor proteins, mimicking neurotransmitters, or changing the amount of neurotransmitter in the synapse, shown in Figure below, by blocking reuptake. In this way a psychoactive drug can change how we feel, think, and interact with the world. Sometimes such effects are beneficial, such as taking a prescribed painkiller (hydrocodone, for example), to ease the pain of a broken bone. Sometimes the effects are harmful, which could happen if the person continued to take the powerful painkiller long after their broken bone had healed. Some examples of psychoactive medicines are listed in Table below.

Figure 20.32
The release of neurotransmitter into the synaptic cleft. Depending on its method of action, a psychoactive substance may block the receptors on the post-synaptic neuron, or block reuptake or affect neurotransmitter synthesis in the pre-synaptic neuron.
Some Psychoactive Medicines and Their Uses
|
Type
|
Uses
|
Example
|
Action
|
|
Anesthetics
|
Block pain and other sensations. Often induce unconsciousness, which allows patients to undergo medical procedures.
|
Lidocaine, nitrous oxide
|
Mimic the inhibitory neurotransmitter GABA, or increase the amount of GABA in the synapse which prevents an action potential.
|
|
Painkillers (analgesics)
|
Reduce the sensation of pain. Includes narcotics and non-steroidal anti-inflammatory drugs (NSAIDS)
|
-
NSAIDS: aspirin and acetaminophen (paracetamol).
-
Narcotics: morphine and codeine
|
Drug molecules mimic endogenous opioids “natural painkillers,” such as endorphins, by binding to opioid receptors.
|
|
Antidepressants
|
Antidepressants are used to treat disorders such as clinical depression, anxiety, and eating disorders
|
Selective Serotonin Reuptake Inhibitors (SSRIs); Monoamine oxidase inhibitors (MAOIs)
|
SSRIs: Block the uptake of the neurotransmitter serotonin by presynaptic neuron MAOIs: Prevent an enzyme from breaking down serotonin in the synapse. Both actions result in an increase of serotonin in the synapse.
|
|
Stimulants
|
Used to treat disorders such as attention deficit disorder and to suppress the appetite
|
Amphetamine salts
|
Increases extracellular levels of dopamine, norepinephrine and serotonin by various means
|
|
Antipsychotics
|
Used to treat psychoses such as schizophrenia and mania.
|
Chlorpromazine
|
Blocks dopamine receptors in post synaptic neurons
|
|
Cough medicines (antitussives)
|
Used to treat persistent coughing.
|
Dextromethorphan (DXM) and codeine
|
Inhibit the action of, the NMDA receptor in the post synaptic cell. Reduces action potential, similar in action to anesthetics
|
Drug Abuse
Psychoactive drugs bring about changes in mood and feelings that a user may find desirable, therefore many psychoactive substances are abused. Drug abuse is the repeated use of a drug without advice or guidance of a medical professional, and use for reasons other than for what the drug was originally intended. With continued use of a drug, a person might find that they cannot function normally without the drug, a state called physical dependence. However, note that physical dependence is not in itself bad, for example, a person who has diabetes is physically dependent on insulin injections. Their body cannot work properly without it. Emotionally or mentally needing a drug to be able to function normally is called psychological dependence. When a person continues to take a psychoactive drug, they eventually need to take larger doses of the drug to get the desired effect; this process is known as building a tolerance to the drug. Drug tolerance can involve both psychological and physical factors.
A person who is abusing a drug may eventually lose control of their drug-taking behavior, partly due to the changes the drug has caused in their brain, and partly due to learned drug-abuse behaviors (such as stealing and lying to get money or drugs). In the state of addiction, a drug addict’s life and activities revolve around getting more of the drug to feed their habit, even if it leads to severe consequences such as getting arrested, dropping out of school, or isolation from friends and family. In a person who is addicted to a drug, the pattern of increasing dose due to tolerance can lead to a drug overdose, also known as an OD. A drug overdose is generally considered harmful and may lead to death. Drug dependence and addiction are caused by changes in the way neurons in the CNS send and receive neurotransmitters. It is for this reason dependency and addiction are treated as brain disorders by medical professionals.
Several classes of psychoactive drugs are commonly abused. Stimulants such as cocaine, nicotine, and amphetamine increase the activity of the sympathetic nervous system, the central nervous system, or both. Stimulants generally increase heart rate, blood pressure, and increase the sense of alertness. Some stimulants, such as caffeine, are used medicinally to increase or maintain alertness, and to counteract fatigue. High doses of stimulants can be fatal. A common source of nicotine is cigarette tobacco, shown in Figure below.

Figure 20.33
Cigarettes are a common source of nicotine. Nicotine is a compound that is found in the leaves of the tobacco plant. It is a potent neurotoxin for insects, and was once used as an insecticide. In addition to the addictive nature of nicotine, long-term tobacco use carries significant risks of developing various cancers as well as strokes and severe cardiovascular and respiratory diseases.
Hypnotics, also known as depressants, such as alcohol, codeine, barbiturates, and benzodiazepines generally decrease the activity of the central nervous system. Depressants slow down brain function and give a drowsy or calm feeling. However, taking too much of a depressant drug can cause dangerously slow breathing and heart rates, and may result in death. Many depressants acting on the CNS do so by increasing the activity of the inhibitory neurotransmitter gamma-aminobutyric acid (GABA), although there are many receptors that are affected by different depressants. GABA calms the activity of the CNS and promotes sleep. Drugs that stimulate the activity of this amino acid slow down brain function and cause a drowsy or calm feeling, so depressants are generally prescribed to relieve symptoms of anxiety or insomnia.
Hallucinogens, also known as psychedelic drugs, such as lysergic acid diethylamide (LSD), phencyclidine (PCP), and ketamine, are psychoactive drugs that do not increase or decrease a certain feeling or emotion, but rather they induce experiences, such as sensory distortions and “out-of-body experiences,” that are very different from those of ordinary consciousness. These experiences are often called trance-like states. The use of psychedelic drugs has been linked to a potential for brain damage.
There are many ways in which psychoactive drugs can affect the CNS. Each drug has a specific action on one or more neurotransmitters or receptors. Drugs that increase activity in particular neurotransmitter systems are called agonists. They act by increasing the synthesis of one or more neurotransmitters or reducing its reuptake from the synapses. Drugs that reduce neurotransmitter activity are called antagonists, and work by interfering with synthesis or blocking postsynaptic receptors so that neurotransmitters cannot bind to them. The drug ketamine, which is used as an anesthetic and a painkiller, blocks the action of the neurotransmitter glutamate. Diacetylmorphine (heroin) enhances the action of endorphins in the brain. Different drugs also affect different parts of the brain. For example, drugs that affect breathing, such as cough suppressants, affect the brainstem to stop the coughing reflex. Painkillers (analgesics) block pain messages coming through the spinal cord from the body. In Figure below the brainstem region is blue, and the spinal cord is yellow.
How Addiction Happens
The neurobiological theory of addiction proposes that certain chemical pathways are greatly changed in the brain of an addicted person. Almost all drugs that are abused affect a certain set of brain structures in the limbic system called the "brain reward system," shown in Figure above. The neurotransmitter dopamine is commonly associated with the brain reward system. The system providing feelings of pleasure (the “reward”), that motivates a person to perform certain activities over and over again. Dopamine is released at synapses by neurons when a person has a pleasurable experience such as eating a favorite food, or eating when very hungry. Such mechanisms have evolved to ensure the survival of organisms.

Figure 20.34
The limbic system (in red) includes structures in the human brain that have been linked to emotion, motivation, and emotional association with memory. The action of neurotransmitters in the limbic system is altered by addictive drugs.
Some drugs, such as cocaine, nicotine, amphetamines, and alcohol directly or indirectly increase the amount of dopamine in the limbic structures. The pleasurable feelings that these drugs produce trick the body into thinking that the drug is good,important for survival, and needs to be taken repeatedly. Drugs that directly affect the brain reward system are highly addictive. The stimulant nicotine, which is found in tobacco, is highly addictive.
Cocaine is an example of a psychoactive drug that is both used as a medicine, and abused as a drug. Cocaine is highly addictive. It is a dopamine transporter blocker—it blocks the reuptake of dopamine by the presynaptic neuron. This action increases the amount of dopamine left in the synaptic cleft, so dopamine has a stronger effect on the postsynaptic neuron. Continued cocaine use causes a reduction in the number of dopamine receptors on the postsynaptic neuron. Eventually, the post synaptic neuron becomes understimulated because there are fewer dopamine receptors on it to respond to dopamine. At this point, more cocaine must be taken to stimulate the postsynaptic neuron into an action potential. If a person becomes dependent on the drug, they need cocaine for their body to act normally. If a person were to stop taking the drug at this point, their body would not be able to act normally, and they would experience a range of uncomfortable and painful symptoms called withdrawal. Symptoms of withdrawal include vomiting, diarrhea, and depression.
Many psychoactive substances are used or abused for their mood and perception altering effects, including those with accepted uses in medicine and psychiatry. Classes of drugs that are frequently abused include some of the drugs listed in Table below. Drugs that are deemed by to have no medical uses and a high potential for abuse are usually illegal.
Not all drugs are physically addictive, but any activity that stimulates the brain reward system can lead to psychological addiction. Drugs that are most likely to cause addiction are drugs that directly stimulate the dopaminergic system, like cocaine, nicotine, and amphetamines. Drugs that only indirectly stimulate the dopaminergic system, such as psychedelics, are not as likely to be addictive.
Some Common Drugs of Abuse
|
Psychoactive Drugs
|
Effects
|
Examples
|
Some Common Forms or Names
|
|
Stimulants
|
Elevate the central nervous system and raise level of alertness and wakefulness
|
Caffeine, cocaine, amphetamine, methamphetamine
|
Coffee, coke, meth, ecstasy (X)
|
|
Hallucinogens
|
Induce perceptual and cognitive distortions
|
LSD, psilocybin, mescaline, PCP
|
Acid, magic mushrooms, peyote, angel dust
|
|
Hypnotics
|
Depress the CNS, and induce sleep
|
Barbiturates, opioids (e.g. codeine, morphine, oxycodone), benzodiazepines, ethanol
|
Diazapam, alcohol
|
|
Analgesics
|
Induce euphoria, reduce sensation of pain
|
Codeine, morphine, ketamine, heroin, phencyclidine (PCP), tetrahydrocannabinol (THC)
|
Horse, angel dust, cannabis, marijuana
|
Lesson Summary
- Neurons are typically made up of a cell body, dendrites, and an axon. The cell body contains the nucleus and other organelles similar to other body cells. The dendrites extend from the cell body and receive a nerve impulse from another cell. The cell body collects information from the dendrites and passes it along to the axon. The axon is a long, membrane-bound extension of the cell body that passes the nerve impulse onto the next cell.
- Voltage is electrical potential energy that is caused by a separation of opposite charges across the membrane. The voltage across a membrane is called membrane potential. Membrane potential is the basis for the conduction of nerve impulses along the cell membrane. In an action potential, the cell membrane potential changes quickly from negative to positive as sodium ions flow into and potassium ions flow out of the cell through ion channels.
- A neurotransmitter is a chemical message that is used to relay electrical signals between a neuron and another cell. Neurotransmitter molecules are made inside the presynaptic neuron and stored in vesicles at the axon terminal.
- The central nervous system represents the largest part of the nervous system, and includes the brain and the spinal cord. The brain is the central control of the nervous system, and the spinal cord carries nerve impulses between the brain and the body, and from the body to the brain.
- The sense organs include the eyes, ears, nose, mouth, and skin. They all have sensory receptors that are specific for certain stimuli. The eyes have photoreceptors for sight. The ears have mechanoreceptors that interpret stimuli as sound and also endolymph that aids in body balance. The nose has chemoreceptors for odors. The mouth has chemoreceptors for taste. The skin has a variety of mechanoreceptors and baroreceptors for touch.
- Psychoactive drugs affect how neurons in the CNS communicate with each other. In this way a psychoactive drug changes how we feel, think, and interact with the world. Medicinal uses of psychoactive drugs include their use as anesthetics, painkillers, and antidepressants.
- For an animation of the neuromuscular junction see http://www.youtube.com/watch?v=ZscXOvDgCmQ.
Review Questions
- How does the body transmit electrical signals?
- Describe the structure of a neuron.
- Distinguish between a neuron and a glial cell.
- Use this image of an action potential to answer the following questions.
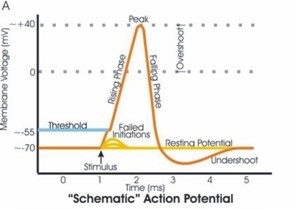
Figure 20.35
What is the membrane potential at the peak (after 2 milliseconds)? Is it positive or negative?
- What happens to the membrane potential after 5 ms?
- At the peak point when the membrane potential is 40mV, does the cell have an overall negative charge or positive charge?
- Hyperpolarization, which means the cell becomes more negatively charged than it is at resting potential (more negative than -70 mV),can happen as a result of the binding of an inhibitory neurotransmitter to its receptor. Propose what happens to sodium and potassium ions during hyperpolarization.
- How does voltage relate to the membrane potential?
- What would happen to a cell if its sodium and potassium pumps failed to work at the end of an action potential?
- The backflow of a nerve impulse is prevented by the fact that at a chemical synapse, the axon terminal does not have neurotransmitter receptors and dendrites cannot secrete neurotransmitter chemicals. What does this statement tell you about the direction of nerve impulses in neurons?
- Identify two types of synapses in the nervous system.
- What is the purpose of the digestive enzymes found in the synaptic cleft?
- Distinguish a neurotransmitter from a hormone.
- What is the major function of the central nervous system?
- Outline the major functions of the cerebral cortex.
- Use this image of the lobes of the brain to answer the following questions.
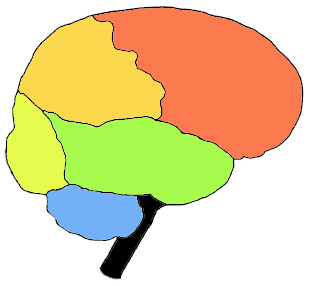
Figure 20.36
What is the name of the blue structure?
- Identify a sense that is interpreted in the yellow-colored lobe (center left), and name that lobe.
- Identify the two main divisions of the peripheral nervous system, and describe their roles in the body.
- What are the two divisions of the autonomic nervous system?
- Distinguish between the sympathetic and parasympathetic nervous systems.
- What type of sensory receptors are found in the eyes?
- Distinguish between rods and cones.
- Why are taste and smell called the “two chemical senses”?
- Outline how the ear is important to the sense of body balance.
- What role does skin have in detecting external stimuli?
- What kind of effects should a drug have for it to be called psychoactive?
- Identify the main effect of psychoactive drugs on the CNS.
- How do the effects of a stimulant differ from the effects of a depressant?
- What is the brain reward system and how is it affected by an addictive drug?
- How does cocaine affect the brain reward system?
- Use this graph that shows the differences in blood concentration of nicotine over time to answer the following questions.

Figure 20.37
- Review the graph that illustrates the increases in blood-nicotine concentrations from four different forms of tobacco; Cigarettes, oral snuff, chewing tobacco, and nicotine gum. Which of the four forms of nicotine increases blood-nicotine concentration the fastest?
- Which of the four forms of nicotine increases blood-nicotine concentration the least?
- Can you tell from this graph whether one form of tobacco is safer than another?
Further Reading / Supplemental Links
Vocabulary
-
action potential
-
An electrical charge that travels along the membrane of a neuron.
-
agonists
-
Drugs that increase activity in particular neurotransmitter systems; act by increasing the synthesis of one or more neurotransmitters or reducing its reuptake from the synapses.
-
antagonists
-
Drugs that reduce neurotransmitter activity; work by interfering with synthesis or blocking postsynaptic receptors so that neurotransmitters cannot bind to them.
-
astrocytes
-
A type of glial cell in the brain; important for the maturation of neurons and may be involved in repairing damaged nervous tissue.
-
autonomic nervous system (ANS)
-
The part of the peripheral nervous system that maintains homeostasis in the body; controls such actions as heart rate, digestion, respiration rate, salivation, and perspiration; also called the involuntary nervous system.
-
axon
-
A long, membrane-bound extension of the cell body that passes the nerve impulse onto the next cell.
-
axon terminal
-
The end of the axon; the point at which the neuron communicates with the next cell.
-
brain stem
-
Part of the brain involved with unconscious (autonomic) functions such as breathing, heartbeat, and temperature regulation; contains the midbrain, the pons, and the medulla oblongata.
-
cerebellum
-
The part of the brain that is involved in coordination and control of body movement.
-
cerebral cortex
-
The highly-folded outer layer of the cerebrum; controls higher functions, such as consciousness, reasoning, emotions, and language; also controls sensory functions such as touch, taste, smell, and responses to external stimuli.
-
cerebrum
-
The part of the brain that generally controls conscious functions such as problem-solving and speech.
-
central nervous system (CNS)
-
Made up of the brain and spinal cord; the brain is the central control of the CNS; the spinal cord carries nerve impulses from the brain to the body and from the body to the brain.
-
chemical synapse
-
A synapse that uses chemical signaling molecules as messengers.
-
cochlea
-
A coiled tube within the ear; filled with a watery liquid which moves in response to the vibrations coming from the middle ear through the oval window; as the fluid moves, thousands of mechanoreceptors called hair cells bend, releasing a neurotransmitter.
-
cone cells
-
Photosensitive cells important to vision; located in the retina; respond to different wavelengths of bright light to initiate a nerve impulse; also responsible for the sharpness of images.
-
dendrites
-
Extend from the cell body and receive a nerve impulse from another cell.
-
diencephalons
-
The region of the brain that includes structures such as the thalamus, the hypothalamus, and a portion of the pituitary gland.
-
dorsal root
-
The “nerve highway;” carries sensory information from sensory receptors in the body to the CNS.
-
drug
-
Any chemical or biological substance that affects the body’s structure or functions.
-
drug abuse
-
The repeated use of a drug without advice or guidance of a medical professional, and use for reasons other than for what the drug was originally intended.
-
electrical synapse
-
Synapse that uses ions as messengers.
-
endocrine system
-
A system of glands around the body that release chemical signal molecules into the bloodstream.
-
glial cell
-
Cell that provides a support system for the neurons; also involved in synapse formation.
-
hallucinogens
-
Psychedelic drugs, such as lysergic acid diethylamide (LSD), phencyclidine (PCP), and ketamine; psychoactive drugs that do not increase or decrease a certain feeling or emotion, but rather they induce experiences, such as sensory distortions and “out-of-body experiences,” that are very different from those of ordinary consciousness.
-
hearing
-
The sense of sound perception that results from the movement of tiny hair fibers in the inner ear.
-
hypnotics (depressants)
-
Drug that decreases the activity of the central nervous system; slows down brain function and give a drowsy or calm feeling; includes alcohol, codeine, barbiturates, and benzodiazepines.
-
interneurons
-
Neurons that connect sensory and motor neurons in neural pathways that go through the CNS; also called association or relay neurons.
-
medicine (or medication)
-
A drug that is taken to cure or reduce the symptoms of an illness.
-
membrane potential
-
The voltage across a membrane; the basis for the conduction of nerve impulses along the cell membrane of neurons.
-
midbrain
-
Part of the brain involved with unconscious (autonomic) functions such as breathing, heartbeat, and temperature regulation.
-
motor division
-
Subdivision of the PNS; carries nerve impulses from the CNS to the muscles, glands and organs of the body; also called the efferent division.
-
motor neurons
-
Neurons that carry signals from the central nervous system to muscles and glands; sometimes called efferent neurons.
-
myelin sheath
-
An electrically insulating phospholipid layer; covers the axon; speeds up the transmission of a nerve impulse along the axon.
-
nerve
-
An enclosed, cable-like bundle of axons.
-
nervous system
-
A complex network of nervous tissue that sends electrical and chemical signals; includes the central nervous system (CNS) and the peripheral nervous system (PNS) together.
-
neuromuscular junction
-
A synapse between a neuron and a muscle cell.
-
neuron
-
The "conducting" cell that transmits electrical signals; the structural unit of the nervous system.
-
neurotransmitter
-
Chemical messages which are released at the synapse and pass the “message” onto the next neuron or other type of cell.
-
nociceptor
-
A type of pain receptor which responds to potentially damaging stimuli.
-
Nodes of Ranvier
-
Regularly spaced gaps between the myelin; the only points at which ions can move across the axon membrane, through ion channels.
-
olfactory receptors
-
The chemoreceptors of smell.
-
oligodendrocytes
-
Glial cells that supply myelin to neurons of the brain and spinal cord.
-
parasympathetic division
-
Subdivision of the ANS; controls non-emergency functions such as digestion.
-
peripheral nervous system (PNS)
-
Made up of the nervous tissue that lies outside the CNS, such as the nerves in the legs, arms, hands, feet and organs of the body.
-
pinna
-
The folds of cartilage surrounding the outer ear canal; gathers sound waves which are channeled down the auditory canal, a tube-shaped opening of the ear which ends at the tympanic membrane, or eardrum.
-
psychoactive drug
-
A substance that affects the central nervous system by altering cognitive function.
-
reflex
-
An automatic (involuntary) action caused by a defined stimulus and carried out through a reflex arc.
-
resting potential
-
The resting state of the neuron, during which the neuron has an overall negative charge.
-
reuptake
-
The removal of a neurotransmitter from the synapse by the pre-synaptic neuron; a way of controlling the effect the neurotransmitter has on the post-synaptic cell.
-
rod cells
-
Photosensitive cells important to vision; located in the retina; highly sensitive to light which allows them to respond in dim light and dark conditions, but, they cannot detect color.
-
Schwann cells
-
Cells that supply the myelin for neurons that are not part of the brain or spinal cord.
-
sensory division
-
Subdivision of the PNS; carries sensory information from sensory receptors in the body to the CNS; also known as the afferent division.
-
sensory neurons
-
Neurons that carry signals from tissues and organs to the central nervous system; sometimes called afferent neurons.
-
sight (vision)
-
Describes the ability of the brain and eye to detect certain wavelengths of electromagnetic radiation (light), and interpret the image.
-
sodium-potassium pump
-
Transport protein that removes Na+ ions from the cell by active transport; also brings K+ ions into the cell.
-
somatic nervous system
-
The part of the PNS that is associated with the conscious (voluntary) control of the body through the movement of skeletal muscles and the perception of external stimuli through senses such as touch, hearing, and sight.
-
spinal cord
-
A thin, tubular bundle of nervous tissue that extends from the medulla oblongata and continues to the lower back; functions as an information superhighway that links the sensory messages from the body to the brain.
-
stimulant
-
Psychoactive drug, such as cocaine, nicotine, and amphetamine, that increases the activity of the sympathetic nervous system, the central nervous system, or both; generally increase heart rate, blood pressure, and increase the sense of alertness.
-
sympathetic division
-
Subdivision of the ANS; generally stimulates body systems during emergency situations.
-
synapse
-
A specialized junction at which neurons communicate with each other.
-
synaptic cleft
-
Gap between the axon terminal of the presynaptic neuron and the receiving cell.
-
threshold
-
Level of depolarization the membrane potential has to surpass for the action potential to start.
-
touch
-
The sense of pressure perception, which is generally felt in the skin.
-
ventral root
-
Contains axons of motor neurons which carry information away from the CNS to the muscles and glands of the body.
-
voltage
-
Electrical potential energy that is caused by a separation of opposite charges.
Points to Consider
- The electrical signals of the nervous system move very rapidly along nervous tissue, while the chemical signals of the endocrine system act much more slowly and over a longer period of time. Identify some of advantages to having two different speeds for communications in the body.
- Identify ways that psychoactive drug abuse may negatively affect organ systems other than the nervous system.
- The cerebral cortex controls functions such as consciousness, reasoning, emotions, and language. The brain stem is the lower part of the brain that is involved with unconscious, autonomic functions. Consider why consciousness and reasoning are called “higher functions” in relation to the “lower functions” of breathing and heartbeat.
Lesson 20.2: The Endocrine System
Lesson Objectives
- Identify the main functions of the endocrine system.
- Identify the structures that produce hormones.
- Outline how hormones affect certain cells and not others.
- Describe two ways that hormones influence the function of cells.
- Identify the two glands that serve as the major control centers of the endocrine system.
- Identify the effects of adrenal hormones on the body.
- Examine the importance of the islets of Langerhans.
- Outline the role of the sex hormones in reproduction.
- Identify non-endocrine organs that secrete hormones.
- Examine how feedback mechanisms control hormone levels and body functions.
- Identify the role of hormone antagonists in the control of substances in the body.
- Identify two medical uses of hormones.
Introduction
The endocrine system is a system of organs that releases chemical message molecules, called hormones, into the blood. Unlike the nervous system whose action helps the body react immediately to change, such as quickly jumping out of the way of an oncoming cyclist, the endocrine system controls changes that happen to the body over a long period of time; from minutes, hours, to years of change. The two systems work closely together to help us respond to our environment, such as the rollercoaster ride shown in Figure below. The endocrine system is important in controlling metabolism, growth and development, reproduction, and salt, water and nutrient balance of blood and other tissues (osmoregulation).

Figure 20.38
What an adrenaline rush! The excitement that the people on this rollercoaster are feeling is a good example of how the nervous and endocrine systems work together. Nerve impulses from the sympathetic nervous system cause the adrenal medulla to release the hormone adrenaline into the bloodstream. Adrenaline causes the racing heart, sweaty palms, and feeling of alertness that together are called the "fight or flight" response.
Function of the Endocrine System
The nervous system uses nerves to conduct electrical and chemical information around the body, while the endocrine system uses blood vessels to carry chemical information. You can think of the nervous system as being similar to the electrical system in a house. Flicking on a light switch is similar to initiating an action potential in a nerve, and it has an almost immediate result: the light bulb illuminates. The endocrine system on the other hand is more like starting up an oil or gas powered water-heating system. You flick on the switch to heat water up for a bath, but it takes a certain length of time for the result to occur: hot water.
Organs of the Endocrine System
The endocrine system is made up of many glands that are located in different areas of the body. Hormones are chemical messenger molecules that are made by cells in one part of the body and cause changes in cells in another part of the body. Hormones regulate the many and varied functions that keep you alive.

Figure 20.39
The major organs of the endocrine system.
Hormones are made and secreted by cells in endocrine glands. Endocrine glands are ductless organs that secrete hormones directly into the blood or the fluid surrounding a cell rather than through a duct. The primary function of an endocrine gland is to make and secrete hormones. The endocrine glands collectively make up the endocrine system. The major glands of the endocrine system and their functions are shown in Figure above. Many other organs, such as the stomach, heart, and kidneys secrete hormones and are considered to be part of the endocrine system.
Exocrine glands are organs that secrete their products into ducts (they are duct glands). They are similar to endocrine glands in that they secrete substances, but they do not secrete hormones. Instead they secrete products such as water, mucus, enzymes, and other proteins through ducts to specific locations inside and outside the body. For example, sweat glands secrete sweat onto the skin and salivary glands secrete saliva into the mouth. The reason we are discussing exocrine glands in a chapter about hormones is because some endocrine glands, such as the pancreas, are also exocrine glands. Ducts in the pancreas secrete fat-digesting enzymes into the intestines. The secretion of the enzymes from the pancreas is controlled by hormones that are made by certain stomach cells.
Hormones
The body produces many different hormones, but each hormone is very specific for its target cells. A target cell is the cell on which a hormone has an effect. Target cells are affected by hormones because they have receptor proteins that are specific to the hormone. Hormones will travel through the bloodstream until they find a target cell with the specific receptors to which they can bind. When a hormone binds to a receptor, it causes a change within the cell.
There are two main types of hormones, and a group of hormone-like substances:
-
Amino Acid-Based Hormones
Amino acid-based hormones are made of amino acids. Some amino acid-based hormones are made of a few amino acids and are simple in structure while others are made of hundreds of amino acids and are very large. These hormones are not fat-soluble and therefore cannot diffuse through the plasma membrane of their target cell. They usually bind to receptors that are found on the cell membrane.
-
Cholesterol-Based Hormones
Cholesterol-based hormones are made of lipids such as phospholipids and cholesterol. Hormones from this group are also called steroid hormones. Steroid hormones are fat soluble and are able to diffuse through the plasma membrane. Steroid hormone receptors are found within the cell cytosol and nucleus.
The term hormone-like substances refers to a group of signaling molecules that are derived from certain types of fatty acids and proteins. Two examples of these substances are prostaglandins and neuropeptides. These substances do not travel around the body in blood as hormones do and tend to be broken down quickly. As a result, the effects of hormone-like substances are localized in the tissue in which it they are produced. For example, prostaglandins, which are made from essential fatty acids, are produced by most cells in the body. Prostaglandins have many different effects such as causing constriction or dilation of blood vessels but they are all are localized within the target cells and tissues. Neuropeptides are signaling peptides found in nervous tissue. Neuropeptides have many effects on nerve cells. For example, they can affect gene expression, local blood flow, and the shape of glial cells. Some neuropeptides such as endorphins and oxytocin have effects on non-nerve cells and are called hormones. Both signaling molecules have an effect on behavior. Among other things, endorphins are involved in pain perception and oxytocin is involved in social bonding and maternal behavior.
The cells that make hormones are usually specialized for the job, and are found within a particular endocrine gland, for example the thyroid gland, the ovaries, or the testes. Hormones may exit their cell of origin by exocytosis or another type of membrane transport. Typically cells that respond to a particular hormone may be one of several cell types that are found in different tissues throughout the body. Such is the case for insulin, which triggers a great number of physical effects. Different tissue types may also respond differently to the same hormonal signal. Because of this, hormonal signaling is a very complex process.
Hormone Receptors
Cells that respond to hormones have two properties in common: they have receptors that are very specific for certain hormones, and those receptors are joined with processes that control the metabolism of the target cells. There are two main ways that receptor-bound hormones activate processes within cells, depending on whether the hormone can pass across the membrane (steroid hormones are fat-soluble), or cannot pass through the membrane (most amino acid based hormones are water soluble).
A water-soluble hormone molecule does not enter the cell, instead it binds to the membrane-bound receptor molecule, which triggers changes within the cell. These changes are activated by second messenger molecules.
A fat-soluble hormone diffuses across the membrane and binds to the receptor within the cytosol or nucleus. The hormone-receptor complex then acts as a transcription factor that affects gene expression.
The two different ways that hormones can activate cells are discussed here, using the amino-acid based hormone glucagon and the steroid hormone cortisol as examples.
Action of Glucagon: A Second Messenger System
The majority of amino-acid based hormones, such as glucagon, bind to membrane-bound receptors. The binding of the hormone triggers a signal transduction pathway, a process of molecular changes that turns the hormone’s extracellular signal into an intracellular response. Activation of these receptors by hormones (the first messengers) leads to the intracellular production of second messengers as part of the signal transduction pathway. A second messenger is a small molecule that starts a change inside a cell in response to the binding of a specific signal to a receptor protein. Some second messenger molecules include small molecules such as cyclic AMP (cAMP), cyclic GMP (cGMP), and calcium ions (Ca2+).
Glucagon is an important hormone involved in carbohydrate metabolism. It is released when the glucose level in the blood is low which causes the liver to change stored glycogen into glucose and release it into the bloodstream. Glucagon is released by the pancreas and circulates in the blood until it binds to a glucagon receptor, a G protein-linked receptor, found in the plasma membrane of liver cells. The binding of glucagon (first messenger) changes the shape of the receptor, which then activates a G protein. The G-protein is an enzyme that in turn activates the next enzyme in the cascade, the second messenger; adenylate cyclase. Adenylate cyclase produces cAMP which activates another enzyme, which in turn activates another enzyme, and so on. The end result is an enzyme that breaks apart the glycogen molecule in the liver cell to release glucose molecules into the blood. The signal transduction pathway, a type of enzyme “domino-effect” inside the cell, allows a small amount of hormone to have a large effect on the cell or tissue. To learn more about second messenger systems, refer to the Cell Structure and Function chapter.
Action of Cortisol: A Direct Gene Activation
Steroid hormones diffuse through cell membrane and bind to receptors in the cytosol or the nucleus of the cell. The receptor-hormone complex acts as a transcription factor that affects gene expression.
Cortisol is a steroid hormone produced by the adrenal glands. It is often called the "stress hormone" as it is involved in the body’s response to stress. It increases blood pressure, blood sugar levels and has an immunosuppressive action. Cortisol crosses the cell membrane and binds to a steroid receptor in the cytoplasm. The cortisol-receptor complex then enters the nucleus of the cell and binds to DNA, where it activates or deactivates gene transcription. The gene that is activated or deactivated depends on the cell type.
Effects of Hormones
The effects of hormones vary widely, and certain hormones, called tropic hormones (or tropins), regulate the production and release of other hormones. Many of the responses to hormones regulate the metabolic activity of an organ or tissue.
Other effects of hormones can include:
- Stimulation or inhibition of growth
- Induction or suppression of programmed cell death (apoptosis)
- Activation or inhibition of the immune system
- Regulation of metabolism
- Preparation for a new activity (e.g., fighting, fleeing, mating)
- Preparation for a new phase of life, for example puberty, caring for offspring, or menopause
- Control of the reproductive cycle
You will learn more about the effects of certain hormones as we examine some of the endocrine glands individually.
Hypothalamus and Pituitary Gland
The hypothalamus links the nervous system to the endocrine system by the pituitary gland. The hypothalamus is located below the thalamus, just above the brain stem. It is found in all mammalian brains, including humans. The human hypothalamus is about the size of an almond; its position in the brain is shown in Figure below.

Figure 20.40
The hypothalamus is here. The red arrow shows the position of the hypothalamus in the brain.
The hypothalamus is a very complex area of the brain, and even small numbers of nerve cells within it are involved in many different functions. The hypothalamus coordinates many seasonal and circadian rhythms, complex homeostatic mechanisms, and the autonomic nervous system (ANS). A circadian rhythm is a roughly-24-hour cycle in the biological processes carried out within organisms, including plants, animals, fungi and certain bacteria. The ANS controls activities such as body temperature, hunger, and thirst. The hypothalamus must therefore respond to many different signals, some of which are from outside and some from inside the body. Thus, the hypothalamus is connected with many parts of the CNS, including the brainstem, the olfactory bulbs, and the cerebral cortex.
The hypothalamus produces hormones that are stored in the pituitary gland. For example, oxytocin and antidiuretic hormone (ADH) are made by nerve cells in the hypothalamus, and are stored in the pituitary prior to their release into the blood. In addition to influencing maternal behavior, oxytocin is involved in controlling circadian homeostasis, such as a person's body temperature, activity level, and wakefulness at different times of the day. Antidiuretic hormone (ADH) is released when the body is low on water; it causes the kidneys to conserve water by concentrating the urine and reducing urine volume. It also raises blood pressure by causing blood vessels to constrict.
Pituitary Gland
The pituitary gland is about the size of a pea and is attached the hypothalamus by a thin stalk at the base of the brain, shown in Figure below. The pituitary gland secretes hormones that regulate homeostasis. It also secretes hormones that stimulate other endocrine glands, called tropic hormones.

Figure 20.41
The position of the pituitary in the brain. A close-up of the anterior and posterior pituitary gland can be seen at right. The orange vessels are the capillary system that comes from the hypothalamus and carries hormones to the anterior pituitary (red) for storage. The blue vessels on the posterior pituitary come from the neurosecretory cells in the hypothalamus.
The anterior pituitary, or front lobe, makes many important hormones, which are listed in Table below. The posterior pituitary, or rear lobe, releases two hormones, oxytocin and antidiuretic hormone (ADH) that are made by nerve cells in the hypothalamus. These hormones are transported down the nerve cell's axons to the posterior pituitary where they are stored until needed.
Pituitary Hormones
|
Location
|
Hormone
|
Target
|
Function
|
|
Anterior Pituitary
|
Adrenocorticotropic hormone (ACTH) Thyroid-stimulating hormone (TSH) Growth hormone (GH)
Follicle stimulating hormone (FSH)
Leutinizing hormone (LH) Prolactin (PRL)
|
Adrenal Gland Thyroid Gland
Body cells
Ovaries, Testes (Gonads)
Ovaries, Testes
Ovaries, mammary glands
|
Stimulates adrenal cortex Stimulates thyroid
Growth hormone
Stimulates production of ovarian follicles in females, sperm production in males Causes ovulation in females Causes milk secretion
|
|
Posterior Pituitary
|
Anti diuretic hormone (vasopressin) Oxytocin
|
Kidneys or Arterioles uterus, mammary glands
|
Promotes water reabsorption in kidneys, raises blood pressure Causes uterus to contract in childbirth, stimulates milk flow
|
Most of these hormones are released from the anterior pituitary under the influence of hormones from the hypothalamus. The hypothalamus hormones travel to the anterior lobe down a special capillary system that surrounds the pituitary.
Oxytocin is the only pituitary hormone to create a positive feedback loop. For example, during the labor and delivery process, when the cervix dilates the uterus contracts. Uterine contractions stimulate the release of oxytocin from the posterior pituitary, which in turn increases uterine contractions. This positive feedback loop continues until the baby is born.
Other Endocrine Glands
Thyroid and Parathyroid Glands
The thyroid is one of the largest endocrine glands in the body. This butterfly-shaped gland is found in the neck, wrapped around the trachea, as shown in Figure below. The hormones released by the thyroid control how quickly the body uses energy, makes proteins, and how sensitive the body should be to other hormones. The thyroid is controlled by the hypothalamus and pituitary. Thyroid hormone generally controls the pace of all of the processes in the body. This pace is related to your metabolism. If there is too much thyroid hormone, every function of the body tends to speed up. The thyroid gland regulates the body temperature by secreting two hormones that control how quickly the body burns calories. Hyperthyroidism (overactive thyroid) and hypothyroidism (under active thyroid) are the most common problems of the thyroid gland.

Figure 20.42
The position of the thyroid and parathyroid glands. A person can have more than four parathyroid glands.
The thyroid hormones thyroxine (T4) and triiodothyronine (T3) regulate the rate of metabolism and affect the growth and rate of function of many other systems in the body. As a result, problems with the under secretion or over secretion of thyroid hormones affect many body systems.
The element iodine is very important for making both T3 and T4. If a person’s diet does not have enough iodine, their thyroid cannot work properly and the person develops an iodine deficiency disease called goiter. Low amounts of T3 and T4 in the blood, due to lack of iodine to make them, causes the pituitary to secrete large amounts of thyroid stimulating hormone (TSH), which causes abnormal growth of the thyroid gland. The addition of small amounts of iodine to mass produced foods, such as table salt, has helped reduce the occurrence of iodine-deficiency in developed countries. The thyroid also produces the hormone calcitonin, which plays a role in calcium homeostasis. The hormones secreted by the thyroid are listed in Table below.
Hormones Secreted by the Thyroid and Parathyroid Glands
|
Location
|
Hormone
|
Target
|
Function
|
|
Thyroid
|
Triiodothyroine (T3) Thyroxine (T4)
Calcitonin
|
-
Bone cells
-
Body Cells
|
Increase metabolic rate, stimulates mental and physical growth Increases calcium absorption by bones, lowers blood calcium level
|
|
Parathyroid
|
Parathyroid hormone (PTH)
|
Cells of the bone, kidney, and intestines
|
Regulates blood calcium levels
|
Parathyroid Glands
The parathyroid glands are usually located behind the thyroid gland, but they are visible in Figure above. Parathyroid hormone (PTH), maintains blood calcium levels within a narrow range, so that the nervous and muscular systems can work properly. When blood calcium levels drop below a certain point, calcium-sensing receptors in the parathyroid gland release the hormone parathyroid hormone (PTH) into the blood. PTH has effects that are opposite to the action of calcitonin. It increases blood calcium levels by stimulating certain bone cells to break down bone and release calcium. It also increases gastrointestinal calcium absorption by activating vitamin D, and promotes calcium uptake by the kidneys. The hormones secreted by the parathyroid glands are listed in Table above.
Pineal Gland
The hormone melatonin is made in the pea-sized pineal gland, which is located at the base of the brain. Production of melatonin by the pineal gland is under the control of the hypothalamus which receives information from the retina about the daily pattern of light and darkness. Very little is currently known about the functions of melatonin, but scientists have found that it is involved in sleep cycles (circadian cycles), the onset of puberty, and immune function. Melatonin secretion also responds to seasonal changes in light, which could be a reason why getting out of bed on a dull, rainy morning can be so difficult, as the boy in Figure below probably knows.

Figure 20.43
Very little is currently known about the role of melatonin, but scientists do know that it is involved in sleep cycles. It is produced by the pineal gland, the retina and the intestines. Production of melatonin by the pineal gland is influenced of by the hypothalamus which receives information from the retina about the daily pattern of light and darkness.
Pancreas
The pancreas is both an exocrine gland as it secretes pancreatic juice containing digestive enzymes, and an endocrine gland as it produces several important hormones. It is located just below and behind the stomach, as shown in Figure below. The endocrine cells of the pancreas are grouped together in areas called islets of Langerhans, shown in Figure below. The islets produce the amino acid-based hormones insulin, glucagon, and somatostatin. Insulin and glucagon are both involved in controlling blood glucose levels. Insulin is produced by beta cells and causes excess blood glucose to be taken up by liver and muscle cells, where it is stored as glycogen, a polysaccharide. Glucagon is produced by alpha cells and stimulates liver cells to break down stores of glycogen into glucose which is then released into the blood. An alpha cell is another type of endocrine cell that is found within the islets of Langerhans. The hormones secreted by the pancreas are listed in Table below.

Figure 20.44
The location of the pancreas in relation to the stomach and gall bladder. The hormone-producing Islet cells a found in groups throughout the pancreas.
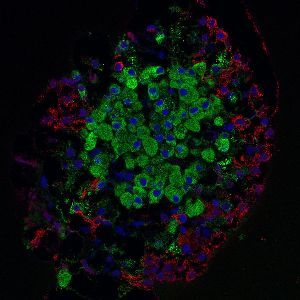
Figure 20.45
Micrograph of an islet of Langerhans isolated from a rat pancreas. Each islet in a human pancreas contains approximately 1000 cells and is 50 to 500 micrometers in diameter. Cell nuclei are stained blue, insulin-producing beta cells are green, and glucagon-producing alpha cells are red.
Hormones Secreted by the Pancreas
|
Hormone
|
Effects
|
|
Insulin Glucagon
Amylin
Somatostatin (inhibitory hormone)
Ghrelin
|
Reduces blood glucose concentration Raises blood glucose concentration
Suppresses glucagons secretion
Suppress the release of insulin, glucagon, and pancreatic enzymes
Stimulates appetite
|

Figure 20.46
The location of the adrenal glands, above the kidneys.
Adrenal Glands
An adrenal gland is located above each of the kidneys, as shown in Figure above. Each adrenal gland is separated into two structures, the adrenal medulla, which is the center of the gland, and the adrenal cortex, which is the outer layer. The medulla and the cortex work as two separate endocrine glands.
The adrenal medulla is the core of the adrenal gland, and is surrounded by the adrenal cortex. Secretion of hormones from the medulla is controlled by the sympathetic nervous system. The cells of the medulla are the body's main source of the hormones adrenaline (epinephrine) and noradrenaline (norepinephrine). These hormones are part of the fight-or-flight response initiated by the sympathetic nervous system. The hormone boosts the supply of oxygen and glucose to the brain and muscles, while suppressing other non-emergency bodily processes, such as digestion.
The adrenal cortex is the site of steroid hormone synthesis. Some cells make cortisol, while other cells make androgens such as testosterone. Other cells of the cortex regulate water and electrolyte concentrations by secreting aldosterone, which helps to regulate blood pressure. In contrast to the medulla that is controlled directly by the nervous system, the cortex is regulated by hormones secreted by the pituitary gland and hypothalamus.
Cortisol is an important steroid hormone that is often called the "stress hormone" as it is involved in the response to stress, and is involved in restoring homeostasis after a stressful event, such as the (good) stress caused by running around a soccer field [football pitch (for non-American-English speakers)], shown in Figure below. Cortisol increases blood pressure, blood sugar levels and has an immunosuppressive action. Long-term stress causes prolonged cortisol secretion, hyperglycemia, and weakening of the immune system. Excess levels of cortisol in the blood result in Cushing's syndrome, symptoms of which include rapid weight gain, a round face, excess sweating, and thinning of the skin and mucous membranes.

Figure 20.47
Regular activity through sport is a good way of allowing your body to respond naturally to its stress hormones, which prepare the body for quick movements or prolonged activity.
Hormones of the Adrenal Glands
|
Location
|
Hormone
|
Function
|
|
Adrenal cortex
|
-
Gonadotropins
-
Glucocortocoids (such as cortisol)
-
Mineralcorticoids (such as aldosterone)
|
-
Stimulates releases of sex hormones that develop sexual characteristics of males and females
-
Depress immune response, provide stress resistance, helps in fat, protein and carbohydrate metabolism
-
Regulate sodium reabsorption and potassium elimination in the kidneys
|
|
Adrenal medulla
|
-
Norepinephrine (noradrenaline)
-
Epinephrine (adrenaline)
|
-
Increases alertness, physical effect similar to epinephrine
-
"Fight or flight" hormone, plays central role in short-term response to stress, increases heart rate and supply of blood and oxygen to the brain
|
Epinephrine, also called adrenaline, is a “fight or flight” hormone which is released from the adrenal medulla when stimulated by the sympathetic nervous system. Epinephrine plays a central role in the short-term stress reaction—the body’s response to threatening, exciting, or environmental stressors such as high noise levels or bright light. When secreted into the bloodstream, it binds to multiple receptors and has many effects throughout the body. Epinephrine increases heart rate, dilates the pupils, and constricts blood vessels in the skin and gut while dilating arterioles in leg muscles. It increases the blood sugar level, and at the same time begins the breakdown of lipids in fat cells. It also “turns down” non-emergency bodily processes such as digestion. Similar to other stress hormones, such as cortisol, epinephrine depresses the immune system.
Stress also releases norepinephrine in the brain. Norepinephrine has similar actions in the body as adrenaline, such as increasing blood pressure. Norepinephrine is also psychoactive because it affects alertness, which would be helpful for studying as shown in Figure below. The hormones secreted by the adrenal cortex and medulla are listed in Table above.

Figure 20.48
Thinking about an upcoming exam can cause your adrenal glands to produce adrenaline (epinephrine). Your bodys stress response can cause you to feel stressed out, but can also motivate you to study.
Gonads
The ovaries of females and the testes of males are the gamete producing organs, or gonads. Ovaries in females are homologous to testes in males. In addition to producing gametes, an exocrine action, the gonads are endocrine glands that produce steroid sex hormones. Sex hormones are responsible for the secondary sex characteristics that develop at puberty. Puberty is the process of physical changes during which the sex organs mature and a person become capable of reproducing. During puberty, among other changes, males begin producing sperm and females begin menstrual cycles.
Luteinizing hormone (LH) and follicle stimulating hormone (FSH), which are both secreted by the pituitary gland, are called gonadotropes because they are tropic hormones of the gonads. Recall that tropic hormones trigger the production of hormones in other endocrine glands. The secretion of LH and FSH are, in turn, controlled by gonadotropin-releasing hormone for the hypothalamus. Those pulses, in turn, are subject to the estrogen feedback from the gonads.
In males LH triggers the production of sex hormones called androgens in the testes. The main androgen produced by the testes is testosterone. Testosterone causes an increase in skeletal muscle mass and bone density and is also responsible for the secondary sex characteristics of males such as facial hair, shown in Figure below. The testes also produce small amounts of estrogen in the form of estradiol, which is believed to be important for sperm formation. On average, the human adult male body produces about eight to ten times more testosterone than an adult female body.
Hormones Produced by Gonads
|
Organ
|
Hormone
|
Target
|
Function
|
|
Ovaries
|
Estrogen
|
Bone cells, cells of sex organs
|
Promotes growth and development of female sex organs
Maintains Uterine lining
|
|
Testes
|
Progesterone
Testosterone
|
Bone cells, muscle cells, cells of sex organ
|
Stimulates growth and development of male sex organs and sex drive
|

Figure 20.49
The male hormone testosterone stimulates the growth of facial hair. Many men develop facial hair in the later years of puberty, usually between the ages of 15 to 18 years. The amount of facial hair on a man's face varies between individuals, and also between ethnic groups. For example, men from many East Asian or West African backgrounds typically have much less facial hair than those of Western European, Middle Eastern, or South Asian descent.
In females a rise in LH concentration triggers the production of estrogen and progesterone by the ovaries. Estrogen causes the release of an egg from the ovaries and progesterone prepares the uterus for a possible implantation by a fertilized egg. The placenta is an endocrine gland of pregnancy because it secretes the hormones estrogen, human chorionic gonadatropin, and progesterone which are important for maintaining a pregnancy, shown in Figure below. The hormones secreted by the male and female gonads are listed in Table above.

Figure 20.50
Maintaining correct hormone levels (especially progesterone), throughout pregnancy is important for carrying a pregnancy to full term.
Other Hormone-Producing Tissues and Organs
Several organs that are generally nonendocrine in function, such as the stomach, the small intestine, the kidneys, and the heart have cells that secrete hormones. For example, the kidneys secrete erythropoietin (EPO), a hormone that regulates red blood cell production, and the heart secretes atriopeptin, a hormone that reduces water and sodium levels in the blood, which decreases blood pressure. Ghrelin is a hormone that stimulates appetite and is produced by certain cells that line the stomach. Certain cancer cells secrete hormones that can interfere with homeostasis.
Regulation: Feedback Mechanisms
Hormones regulate many cell activities and so are important to homeostatic regulation. The rate of hormone production and secretion is often controlled by homeostatic feedback control mechanisms, and the effect of hormones is also controlled by hormone antagonists. In these ways, the concentration of hormones and their products is kept within a narrow range so as to maintain homeostasis.
A feedback control mechanism, or a feedback loop, is a signaling system in which a product or effect of the system controls an earlier part of the system, either by shutting the process down or speeding it up. Most feedback mechanisms of the body are negative, only a few are positive. Hormone antagonists and hormone receptor antagonists are hormones or other molecules that block the action of hormones, and are also used by the body to control the action of hormones.
Negative Feedback
Negative feedback is a reaction in which the system responds in such a way as to reverse the direction of change. Since this tends to keep things constant, it allows for a process to return from a state of imbalance back to a homeostatic equilibrium.
A common, non-biological example of negative feedback happens in a home heating system. When you are home, you set your thermostat to 21˚C (about 70˚F), which is the set point. The thermometer in the thermostat monitors the room temperature and will sense when the temperature drops below the 21˚C set point (the stimulus). The thermometer will then send a message to the thermostat (control center), which in turn sends a message to the furnace to switch on and heat up the room. When the room temperature returns to the set temperature, the thermostat shuts the furnace off. In this home-heating example, the increase in air temperature is the negative feedback that results in the furnace being shut off. In this way a set room temperature of 21˚C (within a degree or two) is maintained.
An example of negative feedback in the body is the control of blood-glucose concentrations by insulin. A higher amount of glucose in the blood (the stimulus), signals the beta cells of the pancreas to release insulin into the blood. Hormone concentration alone cannot trigger a negative feedback mechanism, negative feedback is instead triggered by an overproduction of the effect of the hormone, such as the lowering of blood glucose concentration (the effect), which causes a decrease in the secretion of insulin by the pancreas.
Negative Feedback: Regulation of Thyroid Hormones
The thyroid hormones thyroxine (T4) and triiodothyronine (T3) regulate the rate of metabolism. The production of T4 and T3 is regulated by a thyroid-stimulating hormone (TSH), which is released by the anterior pituitary. The thyroid and the TSH-producing cells of the anterior pituitary form a negative feedback loop, as shown in Figure below.
Thyroid-stimulating hormone production is decreased when the T4 levels are high, and when TSH levels are high, T4 production is decreased. The production and secretion of TSH is in turn controlled by thyrotropin-releasing hormone (TRH), which is produced by the hypothalamus. The rate of TRH secretion is increased in situations such as cold temperature because increasing the metabolic rate would generate more heat. Increased levels of T4 and T3 in the blood cause a reduction in TRH secretion. Among other things, TSH secretion is reduced by high levels of thyroid hormones, as well as the antagonistic hormone somatostatin. These feedback loops keep the concentration of thyroid hormones within a narrow range of concentrations.

Figure 20.51
Two negative feedback loops exist in the control of thyroid hormone secretion. (1) shows the loop between the TSH-producing cells of the anterior pituitary and the thyroid. Increased levels of T4 and T3 in the blood cause a reduction in TSH secretion. (2) shows that increased levels of T4 and T3 in the blood cause a reduction in TRH secretion.
Positive Feedback
Positive feedback is a reaction in which the system responds in such a way as to speed up the direction of change. Positive feedback mechanisms are not as common as negative feedback mechanisms because they cause an increase in the initial signal, which would tend to knock many systems out of balance. Take for example, the analogy of the home heating system. If this system were to work on a positive feedback loop, the furnace would not switch off when the temperature reached the set point of 21˚C. Instead, it would keep going and heat the room indefinitely.
An example of a positive feedback mechanism is milk production by a mother for her baby, as shown in Figure below. As the baby suckles, nerve messages from the mammary glands cause the hormone prolactin, to be secreted by the mother’s pituitary gland. The more the baby suckles, the more prolactin is released, which stimulates further milk production by the mother’s mammary glands. In this case, a negative feedback loop would be unhelpful because the more the baby nursed, the less milk would be produced. Another example of a positive feedback loop is the blood-clotting cascade that happens after a blood vessel is cut.

Figure 20.52
Production of breast milk is controlled by a positive feedback mechanism.
Hormone Antagonists
Many hormones work with hormone antagonists to control the concentrations of substances in the body. The hormones have opposite actions on the body and so are called antagonistic.
Insulin and glucagon make up an antagonistic hormone pair. The action of insulin is opposite that of glucagon. For example, your blood glucose concentration rises sharply after you eat food that contains simple carbohydrates, such as the blueberry muffins shown in Figure below. The increase in blood glucose level stimulates beta cells in the pancreas to release insulin into blood. In response to signals by insulin most body cells take up glucose, which removes it from the blood, and the blood glucose concentration returns to the set point. Later, you have missed eating lunch, you are hungry and feel a little light-headed. Your blood glucose concentration has dropped below the set point, which causes the release of glucagon from the pancreas. Glucagon causes the release of glucose from liver cells, which increases your blood-glucose concentration. If glucagon did not do its job correctly, your blood glucose concentration would continue to drop, and you would develop hypoglycemia (low blood sugar). This antagonistic relationship between the two hormones helps to maintain the narrow range of blood glucose concentration.

Figure 20.53
Insulin and glucagon work as an antagonistic pair to keep your blood glucose concentration within a narrow range even after you eat food containing carbohydrates, such as a muffin.
The actions of growth hormone releasing hormone (GHRH) are opposed by another hypothalamic hormone, somatostatin, also known as "growth-hormone-inhibiting hormone" (GHIH). Somatostatin and GHRH are secreted alternatively by the hypothalamus, which causes an increase and decrease in the secretion of growth hormone (GH) by the pituitary.
Many endocrine glands also work together as a group to control body processes. The major endocrine glands coordinate the control of various regulatory systems, such as metabolism, osmoregulation, and reproduction. Many individual glands are directly controlled by the nervous system, and all are in some way controlled by the pituitary and hypothalamus. Some of these glands and their hormone products are listed in Table below.
Coordination of the Endocrine Glands in the Control of Body Systems
|
Function
|
Organ or Glands
|
Hormones
|
Nervous System Control
|
|
Control of the Endocrine System
|
Hypothalamus Pituitary Gland
|
-
Adrenocorticotropic hormone (ACTH)
-
TSH, FSH, LH, GH, prolactin (PRL)
|
ANS (sympathetic and parasympathetic nervous system)
|
|
Regulation of Metabolism
|
-
Liver
-
Pineal Gland
-
Pancreas
-
Parathyroid Glands
-
Thyroid Gland
|
-
Melatonin
-
Glucagon
-
Insulin
-
Parathyroid hormone
-
T3 and T4
|
ANS (sympathetic and parasympathetic nervous system)
|
|
Response to Stress
|
Adrenal Glands
|
-
cortisol
-
norepinepherine,
-
Epinepherine,
|
ANS (sympathetic nervous system)
|
|
Reproduction
|
Gonads (ovaries, testes)
|
-
progestins (progesterone)
-
Androgens (testosterone), estrogens,
|
ANS (parasympathetic nervous system)
|
|
Osmoregulation
|
-
Liver
-
Kidneys
-
Adrenal Glands
|
-
Angiotensin
-
ADH
-
Aldosterone
|
ANS (sympathetic and parasympathetic nervous system)
|
Homeostatic Imbalance: Endocrine System Disorders
Diseases of the endocrine system are common, and include diseases such as diabetes, thyroid disease, and obesity. An endocrine disease is usually characterized by hyposecretion or hypersecretion of hormones and an inappropriate response to hormone signaling by cells.
Cancer can occur in endocrine glands, such as the thyroid, and some hormones are involved in signaling distant cancer cells to multiply. For example, the estrogen receptor has been shown to be involved in certain types of breast cancers.
Hyposecretion
Hyposecretion is the production no hormone or too little of a hormone. It can be caused by the destruction of hormone-secreting cells, such as in Type 1 diabetes, or by a deficiency in a nutrient that is important for hormone synthesis. Hyposecretion can be treated with hormone-replacement therapies. Type 1 diabetes is an autoimmune disease that results in the destruction of the insulin-producing beta cells of the pancreas. A person with Type 1 diabetes needs insulin replacement therapy, usually by injection or insulin pump, in order to stay alive. An insulin pump is shown in Figure below.

Figure 20.54
In the treatment of Type 1 diabetes, an insulin pump is an alternative to multiple daily injections of insulin. The pump is usually used along with the monitoring of blood glucose concentration and carbohydrate intake.
Diabetes insipidus is characterized by excretion of large amounts of very dilute urine, even if liquid intake is reduced. It is caused by an inability of the kidney to concentrate urine due to a lack of antidiuretic hormone (ADH) also called vasopressin, or by an insensitivity of the kidneys to that hormone. Blood glucose levels are not affected in diabetes insipidus.
Growth hormone deficiency is caused by a lack of GH production by the pituitary. GH deficiency affects bone growth development, and people with growth hormone deficiency tend to have, among other things, low bone density and small stature, a condition called pituitary dwarfism. GH deficiency is treated by growth hormone replacement.
Hypothyroidism is the state in which not enough thyroid hormones are made. Thyroiditis is an autoimmune disease where the body's own antibodies attack the cells of the thyroid and destroy it. Thyroid hormones play an important role in brain development during fetal growth. Cells of the brain are a major target for the T3 and T4 hormones. As a result, hypothyroidism in children, either due to a thyroid problem from birth or a lack of iodine in the diet, is a major cause of physical and mental growth impairment in developing countries. In fact, iodine deficiency disorders are the single most common cause of preventable mental retardation and brain damage in the world.
Figure 20.55
There are many causes of goiter, but the most common is the world is iodine deficiency. Today, iodine deficiency remains mostly a problem in poorer countries which lack the means to add iodine to foods. Iodized salt has helped reduce the amount of iodine deficiency in the developed world. Governments of some countries add iodine to cattle feed to ensure that dairy foods will contain iodine.
Hypersecretion
Hypersecretion of a hormone happens when the body produces too much of a hormone. A hormone can be hypersecreted if the gland develops a tumor and grows out of control, or if the gland is signaled to produce too much of a hormone.
Hyperthyroidism is the result of excess thyroid hormone production, which causes an overactive metabolism and increased speed of all the body's processes. Hyperthyroidism is the most common cause of goiter in the developed world, shown in Figure above.
Hypersecretion of growth hormone causes acromegaly. A common cause of acromegaly is a benign tumor of the pituitary glands that releases too much GH. In some cases, acromegaly is also caused by overproduction of the hypothalamus hormone growth hormone release hormone (GHRH). Acromegaly most commonly affects middle-aged adults and can result in serious illness and premature death. Symptoms include enlarged hands and feet, protruding brow and chin, and enlarged internal organs. However, the disease is hard to diagnose in the early stages and is frequently missed for many years due to its slow progression. If the pituitary produced too much GH during childhood, the person will be taller than normal, a condition called pituitary gigantism. Pituitary gigantism is very rare, and some of the tallest people on record had this condition.
Hormone Insensitivity: Type 2 Diabetes
In some cases, the body makes enough hormones, but body cells do not respond. This can be due to missing or defective hormone receptors, or the body cells become resistant to normal concentration of the hormone, and do not respond to it.
Type 2 diabetes is characterized by hyperglycemia (high blood glucose concentrations), body cells that do not respond to normal amounts of insulin (insulin resistance), and the resulting inability of the pancreas to produce enough insulin. Insulin resistance in cells results in high amounts of free fatty acids and glucose in the blood. High plasma levels of insulin and glucose due to insulin resistance often lead to metabolic syndrome and Type 2 diabetes. Type 2 diabetes can be controlled by improving the diet, increasing levels of activity, and sometimes medication.
Gestational diabetes is a form of diabetes that affects pregnant women. There is no known single cause, but it's believed that the hormones produced during pregnancy reduce the ability of the cells in the pregnant woman's body to respond to insulin, which results in high blood glucose concentrations.
Hormones as Medicines
Many hormones and molecules like them are used as medicines. The most common type of therapy is called hormone-replacement therapy. The most commonly-prescribed hormones are estrogens and synthetic progesterone (as methods of hormonal contraception and as HRT therapy for post-menopausal women), thyroxine (as levothyroxine, for hypothyroidism) and corticosteroids (for autoimmune diseases and several respiratory disorders). Progestin, a synthetic progesterone, is also used to prolong pregnancy in women who have experienced a miscarriage due to a premature drop in progesterone levels. Hydrocortisone is a synthetic form of cortisol that is used to treat allergies and inflammation as well as cortisol production deficiencies. Hydrocortisone cream is a common over-the-counter medication for the topical treatment of rash. Insulin is used by many people with diabetes.
Epinephrine
Because of its anti inflammatory effect on the immune system, epinephrine is used to treat anaphylaxis. Anaphylaxis is a sudden and severe allergic reaction that involves the entire body. After an initial exposure to a substance like a certain food (such as peanuts), or bee sting, a person's immune system can becomes sensitized to that substance, which is called an allergen. Upon second exposure, an allergic reaction occurs.

Figure 20.56
An EpiPen epinephrine autoinjector. Auto injectors like this one can help save a persons life during an anaphylactic reaction.
Histamine and other substances that are released by body cells cause the blood vessels to dilate, which lowers blood pressure, and fluid to leak from the bloodstream into the tissues, which lowers the blood volume. The release of histamine causes the face and tongue to swell. Swelling of the lining of the throat can lead to breathing difficulties. The hormone epinephrine causes blood vessels to constrict which reduces swelling and causes blood pressure to increase. Epinephrine is used as a medicine in auto-injectors, shown in Figure above, which a person can use themselves should they have an anaphylactic reaction.
Anabolic Androgenic Steroids
Synthetic androgens, in the form of anabolic androgenic steroids (anabolic steroids), have many medical uses. It is used to stimulate bone growth and appetite, induce puberty in boys, and treat muscle-wasting conditions in patients that have diseases such as cancer and AIDS. In general, androgens, including testosterone, promote protein synthesis and the growth of muscle tissue and other tissues that have androgen receptors. Androgens also block the effects of the stress hormone cortisol on muscle tissue, so the breakdown of muscle is greatly reduced.

Figure 20.57
Athletes involved in sports that emphasize strength, weight, and shape may feel pressure to take anabolic steroids, however, the majority of school athletes do not take them.
Anabolic Steroid Abuse
As a result of their muscle-building action, anabolic steroids are used in sport and bodybuilding to increase muscle size and strength, to gain a competitive edge or to assist in recovery from injury. Steroids used to gain competitive advantage are forbidden by the rules of the governing bodies of many sports. Serious health risks can be produced by long-term use or excessive doses of anabolic steroids. Most of these side effects are dose dependent, the most common being an increase in low density lipoprotein (bad cholesterol), and a decrease in good high density lipoprotein (good cholesterol). Anabolic steroids also increase the risk of cardiovascular disease in men with high risk of bad cholesterol. Acne is fairly common among anabolic steroid users, mostly due to increases in testosterone which stimulates the sebaceous glands to produce more oil. High doses of anabolic steroids have been linked to liver damage.
Teenagers, particularly boys, who take anabolic steroids, are more likely to be involved in sports that emphasize weight and shape, (such as football or wrestling, which is shown in Figure above). Such teens also have higher rates of disordered eating, drug abuse, and generally have poorer attitudes towards health. Severe side effects can occur if a teenager uses anabolic steroids. For example, the steroids may prematurely stop the lengthening of bones, resulting in stunted growth. Other effects include, but are not limited to, accelerated bone maturation, increased acne outbreaks, and premature sexual development.
In addition to dangerous side effects of the steroids themselves, dangerous drug-taking habits that have been reported by abusers include: unsafe injection practices such as reusing needles, sharing needles, and sharing multidose vials. A common practice among anabolic steroid abusers is self–medicating with other hormones such as growth hormone and insulin, which in itself can lead to serious health consequences. Testosterone and other anabolic steroids are classified as a controlled substance in the United States (US), Canada, the United Kingdom (UK), Australia, Argentina, and Brazil.
Lesson Summary
- The endocrine system is a system of organs that release hormones into the blood. Unlike the nervous system whose action helps the body react immediately to change, the endocrine system controls changes that happen to the body over a long period of time.
- Hormones are made and secreted by cells in endocrine glands. The body produces many different hormones, but each hormone is very specific for its target cells.
- The hypothalamus links the nervous system to the endocrine system by the pituitary gland. The pituitary gland secretes hormones that regulate homeostasis and also secretes hormones that stimulate other endocrine glands. Together the two glands serve as the major control centers of the endocrine system.
- The ovaries of females and the testes of males are the gamete producing organs, or gonads. In addition to producing gametes, an exocrine action, the gonads are endocrine glands that produce steroid sex hormones.
- The rate of hormone production and secretion is often regulated by homeostatic feedback control mechanisms, and the effect of hormones is controlled by hormone antagonists. In these ways, the concentration of hormones and their products is kept within a narrow range so as to maintain life.
- A feedback control mechanism, or a feedback loop, is a signaling system in which a product or effect of the system controls an earlier part of the system, either by shutting the process down or speeding it up.
- Diseases of the endocrine system are common, and include diseases such as diabetes, thyroid disease, and obesity. Many hormones and hormone-like molecules are used as medicines. The most common type of therapy is called hormone-replacement therapy.
Review Questions
- How does a hormone initially activate a target cell?
- What is the main difference between the locations of the receptors for amino acid-based hormones and steroid-based hormones?
- List five main endocrine glands, and identify their locations.
- Name the two glands that control the nervous system.
- Name three hormones that are involved in the stress response and identify their function.
- Outline the role of the parathyroid glands in regulation of blood calcium levels.
- What hormone is secreted by the pineal gland, and what is the function of the hormone?
- How do feedback mechanisms help maintain homeostasis?
- How does negative feedback differ from positive feedback?
- Identify an antagonistic pair of hormones and describe their action.
- Why do you think the pituitary has two lobes?
- What is the purpose of hormone replacement therapy?
- Why might a problem with the pituitary gland affect many different parts of the body?
- Your friend says that he’s pretty sure that the adrenal medulla is controlled by hormones from the pituitary. Do you agree? Explain your answer.
- Outline the feedback mechanism involved in glucose metabolism. Is this feedback mechanism positive or negative?
- Positive feedback mechanisms are harmful to the body. Do you agree with this statement? Explain your answer.
- Goiter is a swelling of the thyroid gland, which is commonly caused by a lack of iodine in the diet. Why do you think a lack of iodine causes the thyroid to swell?
- Use the image of the feedback mechanisms to answer the two questions that follow.

Figure 20.58
Identify three endocrine glands are involved in the feedback mechanisms shown in the figure.
- Identify four hormones involved in these feedback mechanisms.
Further Reading / Supplemental Links
Vocabulary
-
amino acid-based hormones
-
Hormones made of amino acids; not fat-soluble and therefore cannot diffuse through the plasma membrane of their target cell; usually bind to receptors that are found on the cell membrane.
-
antagonistic
-
Hormones that have opposite actions on the body, such as insulin and glucagons.
-
cholesterol-based hormones
-
Hormones made of lipids such as phospholipids and cholesterol; also called steroid hormones; are fat soluble and are able to diffuse through the plasma membrane; bind to receptors that are found within the cell cytosol and nucleus.
-
circadian rhythm
-
A roughly-24-hour cycle in the biological processes carried out within organisms, including plants, animals, fungi and certain bacteria.
-
cortisol
-
A steroid hormone produced by the adrenal glands; often called the "stress hormone" as it is involved in the body’s response to stress; increases blood pressure, blood sugar levels and has an immunosuppressive action.
-
direct gene activation
-
A system in which a fat-soluble hormone diffuses across the membrane and binds to the receptor within the cytosol or nucleus. The hormone-receptor complex then acts as a transcription factor that affects gene expression.
-
endocrine glands
-
Ductless organs that make and secrete hormones directly into the blood or the fluid surrounding a cell rather than through a duct.
-
endocrine system
-
A system of organs that releases chemical message molecules, called hormones, into the blood.
-
exocrine glands
-
Organs that secrete their products into ducts (they are duct glands); do not secrete hormones; secrete products such as water, mucus, enzymes, and other proteins through ducts to specific locations inside and outside the body.
-
feedback control mechanism
-
A signaling system in which a product or effect of the system controls an earlier part of the system, either by shutting the process down or speeding it up; also known as a feedback loop.
-
glucagon
-
An important hormone involved in carbohydrate metabolism; released when the glucose level in the blood is low which causes the liver to change stored glycogen into glucose and release it into the bloodstream.
-
gonads
-
The gamete producing organs; the ovaries of females and the testes of males.
-
hormone-like substances
-
Refers to a group of signaling molecules that are derived from certain types of fatty acids and proteins.
-
hormones
-
Chemical messenger molecules that are made by cells in one part of the body and cause changes in cells in another part of the body.
-
hypersecretion
-
The production of too much of a hormone.
-
hyposecretion
-
The production of no hormone or too little of a hormone.
-
hypothalamus
-
Area of the brain that coordinates many seasonal and circadian rhythms, complex homeostatic mechanisms, and the autonomic nervous system (ANS).
-
islets of Langerhans
-
Areas of the pancreas with groupings of endocrine cells; produce the amino acid-based hormones insulin, glucagon, and somatostatin.
-
negative feedback
-
A reaction in which the system responds in such a way as to reverse the direction of change.
-
neuropeptides
-
Hormone-like substance; signaling peptides found in nervous tissue.
-
positive feedback
-
A reaction in which the system responds in such a way as to speed up the direction of change.
-
prostaglandins
-
Hormone-like substance made from essential fatty acids; produced by most cells in the body; have many different effects such as causing constriction or dilation of blood vessels but they are all are localized within the target cells and tissues.
-
puberty
-
The process of physical changes during which the sex organs mature and a person become capable of reproducing.
-
second messenger system
-
A system in which a water-soluble hormone molecule does not enter the cell, instead it binds to the membrane-bound receptor molecule, which triggers changes within the cell. These changes are activated by second messenger molecules.
-
sex hormones
-
Hormones that are responsible for the secondary sex characteristics that develop at puberty.
-
signal transduction pathway
-
Process initiated by the binding of a hormone to its receptor; a process of molecular changes that turns the hormone’s extracellular signal into an intracellular response.
-
target cell
-
The cell on which a hormone has an effect; has receptor proteins that are specific to the hormone.
Points to Consider
- Think about some of the problems people may have to their muscular systems if their nervous system is not functioning correctly.
- Propose what would happen if the hypothalamus did not produce ADH.
- Why are negative feedback loops more common than positive feedback loops?