Chapter 22: Circulatory and Respiratory Systems
Lesson 22.1: Circulatory System
Lesson Objectives
- Identify the functions and components of the cardiovascular system.
- Describe the structure of the heart.
- Outline the flow of blood through the heart.
- Compare the structures of arteries, veins, and capillaries.
- Compare pulmonary circulation and systemic circulation.
- Outline the functions of the lymphatic system.
- Describe the importance of the coronary arteries.
- Outline the process of atherosclerosis.
- Describe ways of preventing cardiovascular diseases.
Introduction
The cardiovascular system shown in Figure below is an organ system that moves nutrients, hormones, gases and wastes to and from body cells, and distributes heat to maintain homeostasis. The main components of the cardiovascular system are the heart, the blood vessels, and the blood.
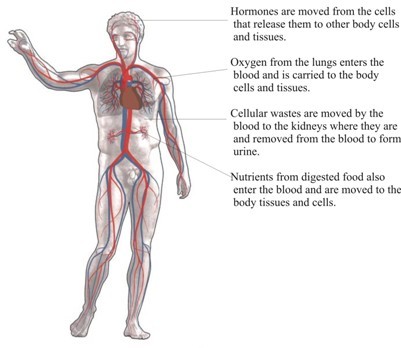
Figure 22.1
The main organs of the circulatory system. Blood acts as the transporter in the body, while blood vessels act like little (one way) roads. The figure is Michelangelos marble sculpture David, which does not actually have a circulatory system.
The Heart
The heart is the muscular organ that pumps blood through the blood vessels by repeated, rhythmic contractions. The term cardiac means "related to the heart" and comes from the Greek word kardia, for "heart." The heart is made up mostly of cardiac muscle tissue, (shown in Figure below) which contracts to pump blood around the body. In adults, the normal mass of the heart is 250-350 grams (9-12 oz), or about three quarters the size of a clenched fist, but badly diseased hearts can be up to 1000 g (2 lb) in mass due to enlargement of the cardiac muscle. For an animation of the heart's anatomy, see http://www.byrnehealthcare.com/animations/SutterAnatomy.htm.
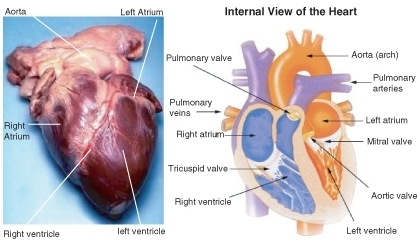
Figure 22.2
External and internal views of the human heart. The aorta in the photo cannot be seen clearly because it is covered by a layer of adipose tissue (fat).
The heart is usually found in the left to middle of the chest with the largest part of the heart slightly to the left. The heart is usually felt to be on the left side because the left ventricle is stronger (it pumps to all the body parts). The heart is surrounded by the lungs. The left lung is smaller than the right lung because the heart takes up more room in the left side of the chest. The position of the heart within the chest is shown in Figure below.

Figure 22.3
Position of the heart in relation to the lungs. The heart can be seen in the lower middle area of the figure, behind the lungs.
Blood Flow Through the Heart
Blood flows through the heart in two separate loops; you could think of them as a “left side loop” and a “right side loop.” The right side and left side of the heart refer to your heart as it sits within your chest. Its left side is your left side and, its right side is your right side.
The right side of the heart collects deoxygenated blood from the body and pumps it into the lungs where it releases carbon dioxide and picks up oxygen. The left-side carries the oxygenated blood back from the lungs, into the left side of the heart which then pumps the oxygenated blood throughout the rest of the body.
The heart has four chambers, the two upper atria and the two lower ventricles. Atria (singular, atrium) are the thin-walled blood collection chambers of the heart. Atria pump the blood into the ventricles. Ventricles are the heart chambers which collect blood from the atria and pump it out of the heart. On the right side of the heart, deoxygenated blood from the body enters the right atrium from the superior vena cava and the inferior vena cava, shown in Figure below. Blood enters the right ventricle which then pumps the blood through the pulmonary arteries and into the lungs. In the lungs, carbon dioxide is released from the blood and oxygen is picked up.
Pulmonary veins bring the oxygenated blood back to the heart and into the left atrium. From the left atrium the blood moves to the left ventricle which pumps it out to the body through the aorta. On both sides, the lower ventricles are thicker and stronger than the upper atria. The muscle wall surrounding the left ventricle is thicker and stronger than the wall surrounding the right ventricle because the left ventricle needs to exert enough force to pump the blood through the body. The right ventricle only needs to pump the blood as far as the lungs, which does not require as much contractile force.
Valves in the heart maintain the flow of blood by opening and closing in one direction only. Blood can move only forward through the heart, and is prevented from flowing backward by the valves. Such movement of the blood is called unidirectional flow. There are four valves of the heart:
- The two atrioventricular (AV) valves ensure blood flows from the atria to the ventricles, and not the other way. The AV valve on the right side of the heart is called the tricuspid valve, and the one on the left of the heart is called the mitral, or bicuspid valve.
- The two semilunar (SL) valves are present in the arteries leaving the heart, and they prevent blood flowing back from the arteries into the ventricles. The SL valve on the right side of the heart is called the pulmonary valve, because it is leads to the pulmonary arteries, and the SL valve on the left is called aortic valve because it leads to the aorta. The valves of the heart are shown in Figure below.
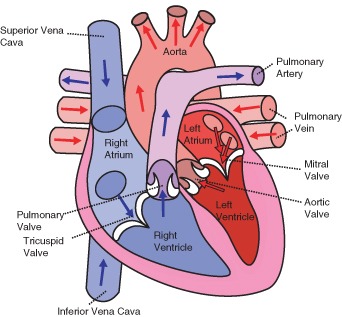
Figure 22.4
The direction of blood flow through the heart.
The Heartbeat
The heart is a meshwork of cardiac muscle cells that are interconnected by little channels called gap junctions. This interconnection allows the electrical stimulation of one cell to spread quickly to its neighboring cells. Cardiac muscle is self-exciting. This is in contrast to skeletal muscle, which needs nervous stimulation to contract. The heart's rhythmic contractions occur spontaneously, although the frequency of the contractions, called the heart rate, can be changed by nervous or hormonal signals such as exercise or the perception of danger.
Control of the Heartbeat
The rhythmic sequence of contractions of the heart is coordinated by two small groups of cardiac muscle cells called the sinoatrial (SA) and atrioventricular (AV) nodes. The sinoatrial node (SA node), often known as the "cardiac pacemaker", is found in the upper wall of the right atrium and is responsible for the wave of electrical stimulation that starts atrial contraction by creating an action potential. The action potential causes the cardiac cells to contract. This wave of contraction then spreads across the cells of the atrium, reaching the atrioventricular node (AV node) which is found in the lower right atrium, shown in Figure below. The AV node conducts the electrical impulses that come from the SA node through the atria to the ventricles. The impulse is delayed there before being conducted through special bundles of heart muscle cells called the bundle of His and the Purkinje fibers, which leads to a contraction of the ventricles. This delay allows for the ventricles to fill with blood before the ventricles contract. Heartbeat is also controlled by nerve messages originating from the autonomic nervous system.
There are important physiological differences between cardiac cells found in the nodes and cardiac cells found in the ventricles. Differences in ion channels and mechanisms of polarization give rise to unique properties of SA node cells, most importantly the spontaneous depolarizations necessary for the SA node's pacemaker activity.
The Bundle of His is a collection of heart muscle cells (fibers) specialized for electrical conduction that transmits the electrical impulses from the AV node. The bundle of His branches into Purkinje fibers. Purkinje fibers, shown in Figure below, are specialized cardiac muscle cells that conduct action potentials into the ventricles, causing the cardiac muscle of the ventricles to contract in a controlled way.
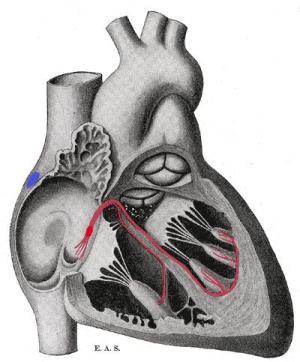
Figure 22.5
Schematic representation of the atrioventricular Bundle of His. The SA node is blue, and the AV node is red and visible in the right atrium. The AV node forms the Bundle of His. Sometimes the left and right Bundles of His are called Purkinje fibers.
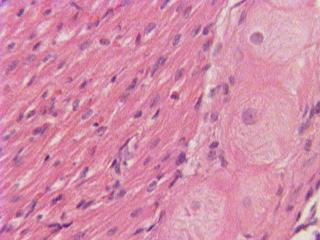
Figure 22.6
The larger round cells on the right are Purkinje fibers. Because of their specializations to rapidly conduct impulses (numerous sodium ion channels and mitochondria, fewer myofibrils than the surrounding muscle tissue), Purkinje fibers take up stain differently than the surrounding muscles cells, and on a slide, they often appear lighter and larger than their neighbors.
The heartbeat is made up of two parts; muscle contraction and relaxation. Systole is the contraction of the heart chambers, which drives blood out of the chambers. Diastole is the period of time when the heart relaxes after contraction. All four chambers of the heart undergo systole and diastole in a timed fashion so that blood is moved forward through the cardiovascular system. For example, ventricular systole is the point at which the ventricles are contracting, and atrial systole is the point at which the atria are contracting. Likewise, ventricular diastole is the period during which the ventricles are relaxing, while atrial diastole is the period during which the atria are relaxing. In general, when referring to systole and diastole, the chambers being referred to are the ventricles, which is shown in Figure below.
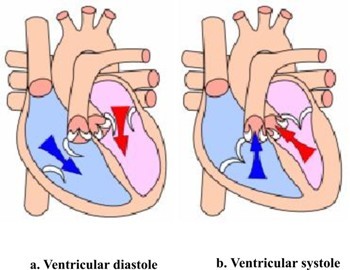
Figure 22.7
When the atria contract, the blood gets pushed into the ventricles which are in diastole. When the ventricles contract (ventricular systole), the blood gets pushed out of the heart.
Heart Sounds
In healthy adults, there are two normal heart sounds often described as a "lub" and a "dub" that occur with each heart beat (lub-dub, lub-dub). In addition to these normal sounds, a variety of other sounds may be heard including heart murmurs or clicks. A medical practitioner uses a stethoscope to listen for these sounds, which gives him or her important information about the condition of the heart.
The sound of the heart valves shutting causes the heart sounds, or a heartbeat. The closing of the mitral and tricuspid valves (known together as the atrioventricular valves) at the beginning of ventricular systole cause the first part of the "lub-dub" sound made by the heart as it beats. The second part of the "lub-dub" is caused by the closure of the aortic and pulmonic valves at the end of ventricular systole. As the left ventricle empties, its pressure falls below the pressure in the aorta, and the aortic valve closes. Similarly, as the pressure in the right ventricle falls below the pressure in the pulmonary artery, the pulmonic valve closes.
Blood Vessels
The blood vessels are part of the cardiovascular system and function to transport blood throughout the body. The two most important types are arteries and veins. Arteries carry blood away from the heart, while veins return blood to the heart.
There are various kinds of blood vessels, the main types are:
-
Arteries are the large, muscular vessels that carry blood away from the heart.
- An arteriole is a small diameter blood vessel that extends and branches out from an artery and leads to capillaries.
-
Veins are vessels that carry blood toward the heart. The majority of veins in the body carry low-oxygen blood from the tissues back to the heart.
- A venule is a small vessel that allows deoxygenated blood to return from the capillaries to veins.
-
Capillaries are the smallest of the body's blood vessels, that connect arterioles and venules, and are important for the interchange of gases and other substances between blood and body cells.
The blood vessels have a similar basic structure. The endothelium is a thin layer of cells that creates a smooth lining on the inside surface of blood vessels. Endothelial tissue is a specialized type of epithelium, one of the four types of tissue found in the body. Endothelial cells have an important structural role in blood vessels; they line the entire circulatory system, from the heart to the smallest capillary. Around the endothelium there is a layer of smooth muscle, which is well developed in arteries. Finally, there is a further layer of connective tissue that surrounds the smooth muscle. This connective tissue, which is mostly made up of collagen, contains nerves that supply the smooth muscular layer. The connective tissue surrounding larger vessels also contains capillaries to bring nutrients to the tissue. Capillaries, the smallest blood vessels, are made up of a single layer of endothelium and a small amount of connective tissue.
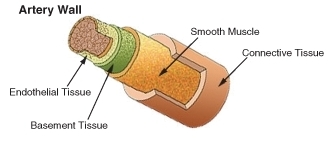
Figure 22.8
The structure of an artery wall.
Arteries and Arterioles
The arteries carry blood away from the heart. As shown in Figure above, arteries have thick walls that have three major layers; an inner endothelial layer, a middle layer of smooth muscle, and an outer layer of stretchy connective tissue (mostly collagen). The elastic qualities of artery walls allow them to carry pressurized blood from the heart while maintaining blood pressure.
The aorta is the largest artery in the body. It receives blood directly from the left ventricle of the heart through the aortic valve. The aorta branches, into smaller arteries and these arteries branch in turn, becoming smaller in diameter, down to arterioles. The arterioles supply the capillaries that carry nutrients to the body’s cells and tissues. The aorta is an elastic artery. When the left ventricle contracts to force blood into the aorta, it expands. This stretching gives the potential energy that will help maintain blood pressure during diastole when the aorta contracts passively.
An arteriole is a small-diameter blood vessel that branches out from an artery and leads to capillaries. Arterioles have thin muscular walls, composed of one or two layers of smooth muscle, and are the primary site of vascular resistance. Vascular resistance is the resistance to flow that blood must overcome to be pumped through your circulatory system. Increasing vascular resistance is one way your body can increase blood pressure.
Veins and Venuoles
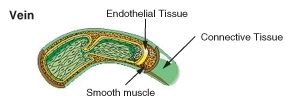
Figure 22.9
Internal structure of a vein.
Veins return deoxygenated blood to the heart. The thick, outer layer of a vein is made up of collagen-containing connective tissue, shown in Figure above. The connective tissue is wrapped around bands of smooth muscle while the interior is lined with endothelium. Most veins have one-way flaps called valves, shown in in Figure below, that prevent blood from flowing backward and pooling in the legs, feet, arms or hands due to the pull of gravity. The location of veins can vary from person to person.
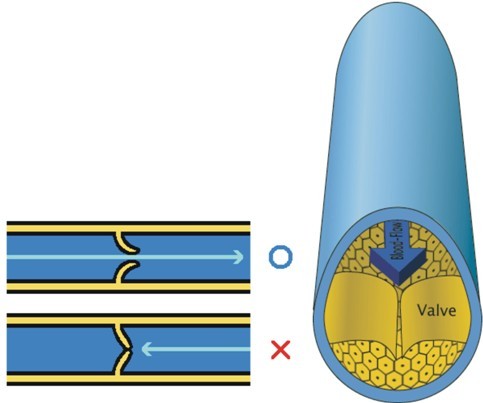
Figure 22.10
Valves found in veins prevent the blood from flowing backward and pooling in the lowest parts of the body, such as the legs and feet.
A venule is a small blood vessel that allows deoxygenated blood to return from the capillary beds to the larger blood vessels called veins. Venules have three layers: an inner endothelium composed of squamous epithelial cells that act as a membrane, a middle layer of muscle and elastic tissue, and an outer layer of fibrous connective tissue. The middle layer is poorly developed so that venules have thinner walls than arterioles.
Capillaries
Capillaries are the smallest of a body's blood vessels, measuring 5-10 μm in diameter. Their size is shown in relation to body cells in Figure below. Capillaries connect arterioles and venules, and they are important for the exchange of oxygen, carbon dioxide, and other substances between blood and body cells.
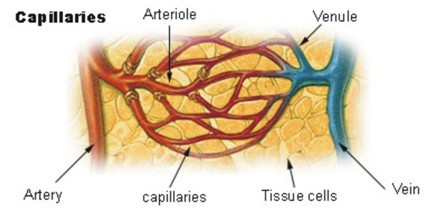
Figure 22.11
The structure of capillaries. Note their size in comparison to the cells around them.
The walls of capillaries are made of only a single layer of endothelial cells. This layer is so thin that molecules such as oxygen, water and lipids can pass through them by diffusion and enter the body tissues. Waste products such as carbon dioxide and urea can diffuse back into the blood to be carried away for removal from the body. Capillaries are so small the blood cells need to pass through it in a single file line. A capillary bed is the network of capillaries supplying an organ. The more metabolically active a tissue or organ is, the more capillaries it needs to get nutrients and oxygen.
Blood vessels are roughly grouped as arterial and venous. This grouping is determined by whether the blood in the vessel is flowing away from (arterial) or toward (venous) the heart. In general the term arterial blood is used to describe blood high in oxygen, although the pulmonary arteries carry deoxygenated blood and blood flowing in the pulmonary vein is rich in oxygen.
Roles of Blood Vessels
Blood vessels are not involved in regulating the transport of blood, the endocrine and nervous systems do that. However, arteries and veins can regulate their inner diameter by contraction of the smooth muscle layer. This widening or narrowing of the blood vessels changes the blood flow to the organs of the body. This process is controlled by the autonomic nervous system; it is not controlled consciously.
Vasodilation is a process by which blood vessels in the body become wider due to the relaxation of the smooth muscle in the vessel wall. This reduces blood pressure since there is more room for the blood to move through the vessel. Endothelium of blood vessels uses nitric oxide to signal the surrounding smooth muscle to relax, which dilates the artery and increasing blood flow. Nitric dioxide is a vasodilator.
Vasoconstriction is the constriction of blood vessels (narrowing, becoming smaller in cross-sectional area) by contracting the vascular smooth muscle in the vessel walls. Vasoconstriction is controlled by substances such as some hormones and neurotransmitters, which are called vasoconstrictors. For example, the “fight or flight” hormone epinephrine is a vasoconstrictor that is released by the adrenal glands.
Permeability of the endothelium is important for the release of nutrients to the tissue. Permeability is the ability of a membrane to allow certain molecules and ions to pass through it by diffusion. Permeability of the endothelium increases during an immune response, which allows white blood cells and other substances to get to the site of injury or irritation.
Oxygen, which is bound to hemoglobin in red blood cells for transport through the body, is the most critical nutrient carried by the blood. In all arteries apart from the pulmonary artery, hemoglobin is highly saturated (95-100%) with oxygen. In all veins apart from the pulmonary vein, the hemoglobin is desaturated at about 70%. (The values are reversed in the pulmonary circulation.)
Blood Vessels and Blood Pressure
Blood pressure refers to the force exerted by circulating blood on the walls of blood vessels. The pressure of the circulating blood gradually decreases as blood moves from the arteries, arterioles, capillaries, and veins. The term "blood pressure" generally refers to arterial pressure, which is the pressure in the larger arteries that take blood away from the heart. Arterial pressure results from the force that is applied to blood by the contracting heart, where the blood “presses” against the walls of the arteries.
The systolic arterial pressure is defined as the peak pressure in the arteries, which occurs near the beginning of the cardiac cycle; the diastolic arterial pressure is the lowest pressure (at the resting phase of the cardiac cycle).
Arterial pressure is most commonly measured by a sphygmomanometer, shown in Figure below. The height of a column of mercury indicates the pressure of the circulating blood. Although many modern blood pressure devices no longer use mercury, values are still universally reported in millimeters of mercury (mmHg).

Figure 22.12
The new and the classic ways to measure blood pressure. A digital sphygmomanometer, shown on the left, runs on electricity or batteries and measure blood pressure automatically. The cuff, which you can see behind the digital readout, is wrapped around the upper arm, just like the cuff of the older devices. The cuff then inflates automatically and measures blood pressure as the cuff deflates. The older, mechanical sphygmomanometer with a cuff and pressure reader and stethoscope is shown at right. The cuff is inflated and deflated manually while a medical technician listens for related changes in the sound of blood moving through arteries in the arm.
Blood Pressure Ranges
In the U.S., the healthy ranges for arterial pressure are:
- Systolic: less than 120 mm Hg
- Diastolic: less than 80 mm Hg
Blood pressure is usually written as systolic/diastolic mm Hg; for example, a reading of 120/80 mm Hg, is said as "one twenty over eighty." These measures of arterial pressure are not static, but go through natural variations from one heartbeat to another and throughout the day (in a circadian rhythm). Factors such as age, gender and race influence blood pressure values. Pressure also varies with exercise, emotional reactions, sleep, stress, nutritional factors, drugs, or disease.
Studies have shown that people whose systolic pressure is around 115 mm Hg rather than 120 mmHg have fewer health problems. Clinical trials have shown that people who have arterial pressures at the low end of these ranges have much better long term cardiovascular health for this reason some researchers say that 115/75 mm Hg should be the ideal measurement.
Hypertension is a condition in which a person’s blood pressure is chronically high. Hypertension is said to be present when a person's systolic blood pressure is always 140 mm Hg or higher, and/or their diastolic blood pressure is always 90 mm Hg or higher. Blood pressure readings between 120/80 mmHg and 139/89 mmHg are called prehypertension. Prehypertension is not a disease category; rather, it is a way to identify people who are at high risk of developing hypertension.
Arterioles and Blood Pressure
Arterioles have the greatest collective influence on both local blood flow and on overall blood pressure. They are the primary "adjustable nozzles" in the blood system, across which the greatest pressure drop occurs. The combination of heart output (cardiac output) and systemic vascular resistance, which refers to the collective resistance of all of the body's arterioles, are the principal determinants of arterial blood pressure at any given moment.
Pulmonary and Systemic Circulations
The double circulatory system of blood flow refers to the separate systems of pulmonary circulation and the systemic circulation in amphibians, birds and mammals, including humans. The adult human heart consists of two separated pumps, the right side which pumps deoxygenated blood into the pulmonary circulation, and the left side which pumps oxygenated blood into the systemic circulation. Blood in one circuit has to go through the heart to enter the other circuit, as shown in Figure below.
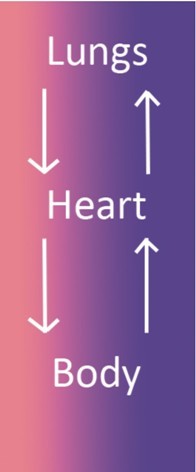
Figure 22.13
The double circulatory system. Blood in one circuit has to go through the heart to enter the other circuit. The heart-to-lungs-to heart portion is the pulmonary circulation, and the heart-to-body-to-heart portion is the systemic circulation.
Pulmonary Circulation
The pulmonary circulation is the portion of the cardiovascular system which carries oxygen-poor (deoxygenated) blood away from the heart, to the lungs, and returns oxygenated blood back to the heart. As shown in Figure below, deoxygenated blood from the body leaves the right ventricle through the pulmonary arteries, which carry the blood to each lung. The pulmonary arteries are the only arteries that carry deoxygenated blood. In the lungs, red blood cells release carbon dioxide and pick up oxygen during respiration. The oxygenated blood then leaves the lungs through the pulmonary veins, which return it to the left side of the heart, and complete the pulmonary cycle. The oxygenated blood is then distributed to the body through the systemic circulation before returning again to the pulmonary circulation.
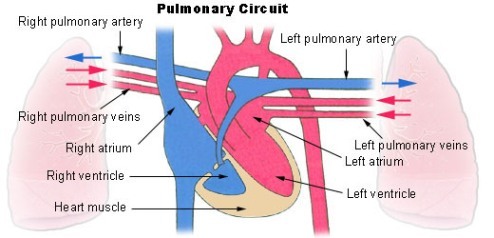
Figure 22.14
Pulmonary circulation. The pulmonary arteries carry oxygen-poor blood from the right ventricle to the lungs, and the pulmonary veins return oxygenated blood to the left side of the heart. This loop is called the pulmonary cycle.
The pulmonary circulation was first discovered by a Syrian physician, Ibn al-Nafis, in 1242. However, credit for the first description of blood circulation is given to an English medical doctor William Harvey, who in 1616 described in detail the pulmonary and systemic circulation systems.
Systemic Circulation
The systemic circulation is the portion of the cardiovascular system which carries oxygenated blood away from the heart, to the body, and returns deoxygenated blood back to the heart. Oxygenated blood from the lungs leaves the left ventricle through the aorta, from where it is distributed to the body's organs and tissues, which absorb the oxygen, through a complex network of arteries, arterioles, and capillaries. The deoxygenated blood is then collected by venules, from where it flows first into veins, and then into the inferior and superior venae cavae, which return it to the right heart, completing the systemic cycle, shown in Figure below. The blood is then re-oxygenated through the pulmonary circulation before returning again to the systemic circulation.
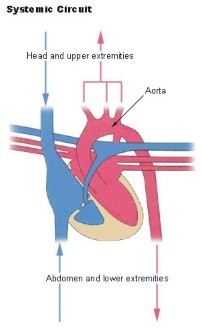
Figure 22.15
The systemic circulation. The systemic circulation brings oxygenated blood to the body cells and tissues and transports cellular wastes. It is also responsible for temperature regulation and transport of hormones and other substances around the body.
Just like every other organ in the body, the heart needs its own blood supply, which it gets through the coronary circulation. Although blood fills the chambers of the heart, the heart muscle tissue is so thick that it needs blood vessels to deliver oxygen and nutrients deep within it. The vessels that deliver oxygen-rich blood to the heart muscle are called coronary arteries, they branch directly from the aorta, just above the heart, shown in Figure below. The vessels that remove the deoxygenated blood from the heart muscle are known as cardiac veins.
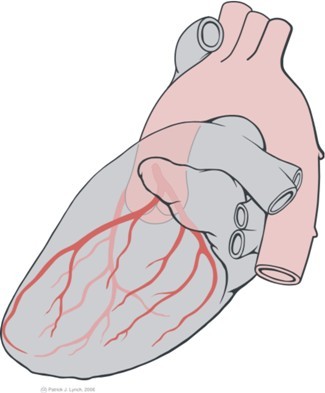
Figure 22.16
This side view (lateral view), of the heart shows how the coronary arteries (in red) branch directly from the aorta to bring oxygen and nutrients into the heart muscle.
Portal Venous System
A portal venous system occurs when a capillary bed drains into another capillary bed through veins. They are relatively uncommon as the majority of capillary beds drain into the heart, not into another capillary bed. Portal venous systems are considered venous because the blood vessels that join the two capillary beds are either veins or venules.
An example of a portal venous system is the blood vessel network between the digestive tract and the liver. The hepatic portal system is responsible for directing blood from parts of the gastrointestinal tract to the liver. Nutrients that have been absorbed into the blood from the small intestine are taken to the liver for processing before being sent to the heart. The term, "portal venous system" often refers to the hepatic portal system.
Lymphatic System
The lymphatic system, shown in Figure below, is a complex network of lymph nodes, lymph ducts, lymphatic tissues, lymph capillaries and lymph vessels that extend the length of the body. It serves as a conduit for a fluid called lymph. The lymphatic system is often called the secondary circulatory system.
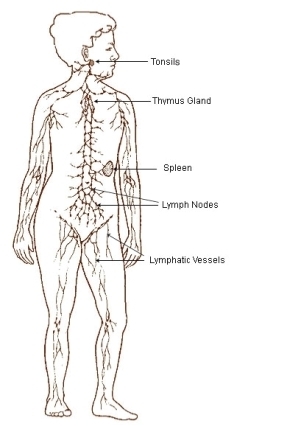
Figure 22.17
Lymphatic system
The lymphatic system has three related functions:
- The removal of excess fluids from body tissues.
- The absorption of fats, also known as fatty acids or lipids, and transport of fats to the cardiovascular system.
- The production of certain types of white blood cells, which aid in the body's immune response.
Lymph originates as blood plasma that leaks from the capillaries of the cardiovascular system. This blood plasma fills the space between individual cells of tissue where it becomes part of the interstitial fluid. Plasma is forced out of the capillaries and forced back in due to interactions of hydrostatic pressure. While out of the blood capillaries, the plasma increases the volume of the interstitial fluid. Most of the interstitial fluid is returned to the capillaries by osmosis. The excess interstitial fluid is collected by the lymphatic system by diffusion into lymph capillaries, and is processed by lymph nodes before to being returned to the circulatory system. Once within the lymphatic system the fluid is called lymph, and has almost the same composition as the original interstitial fluid.
Fatty acids, also known as fats or lipids, are transported through the cardiovascular system differently than other nutrients, such as proteins and sugars. Lipids are absorbed by cells in the villi of the small intestine where they form a complex with protein molecules. These lipo-proteins are called chylomicrons. The chylomicrons are transported via the lymphatic system and eventually rejoin the bloodstream to be processed by the liver.
The lymphatic system is a major component of the immune system. The lymphatic system has many lymph nodes. Lymph nodes are filters or traps for foreign particles and contain white blood cells. Human lymph nodes are bean-shaped and range in size from a few millimeters to about 1 to 2 cm. White blood cells are located within honeycomb structures of the lymph nodes. Lymph that moves through the lymph nodes is filtered so that microorganisms and tissue debris are removed. Lymph nodes swell and feel sore when the body is infected due to the increased production of white blood cells.
The spleen and tonsils are large lymphoid organs that serve similar functions to lymph nodes, though the spleen filters blood cells rather than bacteria or viruses.
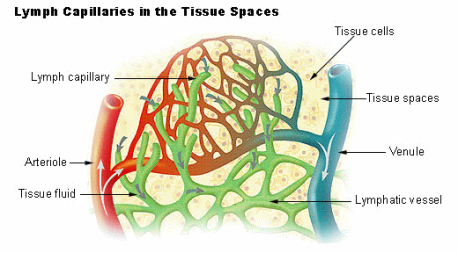
Figure 22.18
The movement of lymph from the interstitial fluid into the lymphatic vessels. Lymph moves in only one direction through the blood vessels.
Lymphatic Circulation
Unlike the blood system, the lymphatic system is not closed and has no central pump. Lymph movement occurs slowly with low pressure due to peristalsis, valves, and the squeezing action of skeletal muscles. Lymph travels through lymph vessels that are similar to capillaries and veins. Lymph moves in one direction only, due to valves in lymph vessels that are similar to the valves found in veins, shown in Figure above. The movement of lymph depends on the movement of skeletal muscles to squeezing the lymph through them, especially near the joints. Rhythmic contraction of the vessel walls through movements may also help draw fluid into the small lymphatic capillaries. The lymph is then transported to progressively larger lymphatic vessels that drain into the circulatory system at the right and left subclavian veins.
Homeostatic Imbalance of the Lymphatic System
In the disease known as elephantiasis, shown in Figure below, infection of the lymphatic vessels cause a thickening of the skin and enlargement of the underlying tissues, especially in the legs and genitals. It is most commonly caused by infection by parasitic roundworms.

Figure 22.19
Over a billion people are at risk for infection by filarial nematodes, the parasites that cause elephantiasis.
Lymphedema also causes abnormal swelling, especially in the arms and legs (though the face, neck, and abdomen can also be affected). It occurs if the lymphatic system is damaged, or underdeveloped in some way. An estimated 170 million suffer with the disorder.
Lymphoma, or lymphatic cancer, is cancer of the lymphatic system. According to the American Cancer Society, in 2007, lymphoma accounted for 4 percent of new cancer cases amongst men and women in the United States. In lymphoma, cells of the lymphatic system grow abnormally. They divide too rapidly and grow without any order or control. Because lymphatic tissue is present in many parts of the body, lymphoma can start almost anywhere. Lymphoma may occur in a single lymph node, a group of lymph nodes, or, sometimes, in other parts of the lymphatic system such as the bone marrow and spleen.
Homeostatic Imbalances of the Cardiovascular System
Cardiovascular disease (CVD) refers to any disease that affects the cardiovascular system, but it is usually used to refer to diseases related to atherosclerosis, which is a chronic inflammatory response in the walls of arteries that causes a swelling and buildup of materials called plaque. Plaque is made of cell debris, cholesterol, fatty acids, calcium, and fibrous connective tissue that build up around an area of inflammation. As a plaque grows it stiffens and narrows the artery, which reduces the flow of blood through the artery, shown in Figure below.
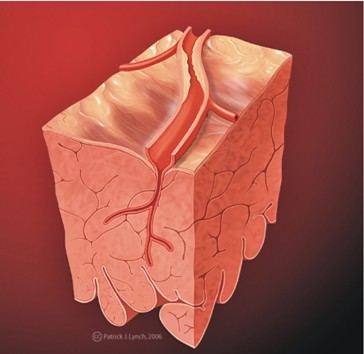
Figure 22.20
Atherosclerosis is sometimes referred to as hardening of the arteries.
Atherosclerosis
Atherosclerosis normally begins in later childhood, and is usually found in most major arteries. It does not usually have any early symptoms. Causes of atherosclerosis include a high-fat diet, high cholesterol, smoking, obesity, and diabetes. Atherosclerosis becomes a threat to health when the plaque buildup interferes with the blood circulation in the heart (coronary circulation) or the brain (cerebral circulation). A blockage in the coronary circulation, can lead to a heart attack, and blockage of the cerebral circulation (leading to, or within the brain) can lead to a stroke. According to the American Heart Association, atherosclerosis is a leading cause of CVD.

Figure 22.21
Autopsy specimen of an artery has been opened lengthwise to show the inside (lumen) which is completely blocked by many plaques. For a video depicting atherosclerosis, see . For an atherosclerosis animation, see
Coronary Heart Disease
Cardiac muscle cells are fed by the coronary arteries. Blocked flow in a coronary artery can result in oxygen starvation and death of heart muscle. Coronary heart disease is the end result of the buildup of plaques within the walls of the coronary arteries, shown in Figure above. Most individuals with coronary heart disease have no symptoms for many years until the first sign, often a heart attack, happens.
A symptom of coronary heart disease is chest pain. Occasional chest pain, called angina pectoralis (or angina) can happen during times of stress or physical exertion. The pain of angina means the heart muscle fibers need more oxygen than they are getting.
A heart attack, also called a myocardial infarction (MI), occurs when the blood supply to a part of the heart is blocked, as shown in Figure below. A heart attack can occur from the buildup and blockage of a coronary artery by plaque, or it can be caused by a small piece of plaque that breaks away when a larger plaque breaks apart. This piece of free-floating plaque, called an embolus, can get stuck in a coronary blood vessel, causing a blockage or embolism. Cardiac muscle fibers that are starved of oxygen for more than five minutes will die, and because they do not divide, dead cardiac muscle cells cannot be replaced. Coronary heart disease is the leading causes of death of adults in the United States. For an animation depicting a heart attack, see http://www.byrnehealthcare.com/animations/SutterHeartAttack.htm.
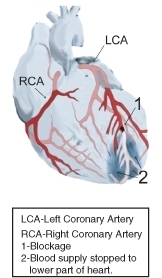
Figure 22.22
Diagram of a heart attack (myocardial infarction). The blood supply to the lower part of the heart is stopped after a blockage of the lower portion of the left coronary artery (LCA). For an animation depicting coronary artery disease, see
Stroke
Since atherosclerosis is a body wide process, similar events can also occur in the arteries to other parts of the body, including the brain. A stroke is a loss of brain function due to a stoppage of the blood supply to the brain. It can be caused by a blot clot (thrombosis), a free-floating object that gets caught in a blood vessel (embolism), or by bleeding (hemorrhage). For an animation depicting a stroke, see http://www.byrnehealthcare.com/animations/SutterStroke.htm.
Risk factors for stroke include advanced age, high blood pressure, previous stroke, diabetes, high cholesterol, and cigarette smoking. Reduction of blood pressure is the most important modifiable risk factor of stroke; however many other risk factors, such as quitting tobacco smoking, are also important.
Preventing Cardiovascular Diseases
There are many risk factors which are associated with various forms of cardiovascular disease, some of these you cannot control, but many you can control.
Non-controllable risk factors include:
- Age: The older a person is, the greater their chance of developing a cardiovascular disease.
- Gender: Men under age 64 are much more likely to die of coronary heart disease than women, although the gender difference declines with age.
- Genetics: Family history of cardiovascular disease affects a person’s chance of developing heart disease.
Controllable risk factors include:
- Tobacco Smoking: Giving up smoking is the single most effective way of reducing risk of heart disease.
- Diabetes: Having diabetes can cause metabolic changes (such as high cholesterol levels) which in themselves are risk factors.
- High cholesterol levels: High amounts of low density lipids (LDLs) in the blood, also called "bad cholesterol", are a significant risk factor.
- Obesity: Being obese, especially if the fat is deposited mostly in the torso, rather than the hips and thighs, increases risk significantly.
- High blood pressure: Hypertension can cause atherosclerosis.
- Lack of physical activity: Aerobic activities, including walking and vacuuming, that are done for 60 minutes a day, five days a week, help keep the heart healthy.
- Poor eating habits: Eating mostly foods that are nutrient poor (do not have many nutrients other than fat or carbohydrate) leads to high cholesterol levels and weight gain, among other things.
Although there are uncontrollable risk factors involved in CVD, a person whose family has a history of CVD is not destined to develop heart disease. There are many things such a person can do to help prevent CVD, even when predisposed to a disease. A person who is physically active every day, eats healthfully, and avoids tobacco can lower their chances of developing the disease.
Although men have a higher rate of cardiovascular disease than women, it is also the number one health problem for women in industrialized countries. After menopause, the risk for women is almost equal to that of men.
Cardiovascular Disease Awareness
Cardiovascular diseases are called "lifestyle diseases" because they are caused mostly by everyday choices that people make, such as what to eat for dinner, or what to do during their free time. For example, watching TV with your dog does not involve much moving around so it does not exercise the body, whereas bringing the dog for a walk outside exercises both of you. Decisions that you make today and everyday will affect your cardiovascular health many years from now, such as those shown in Figure below.
Many studies have shown that plaque buildup starts in early adolescence. However, teens are more concerned about risks such as HIV, accidents, and cancer than cardiovascular disease. One in three people will die from complications due to atherosclerosis. For this reason there is an emphasis on the prevention of CVD through risk reduction. For example, healthy eating, regular physical activity, and avoidance of smoking can greatly decrease a person’s chance of developing a CVD.

Figure 22.23
Limiting sedentary activities such as watching TV, and making more time for walking, hiking, cycling, or running will help develop a healthy heart.
Congenital Heart Defects
A congenital heart defect is a problem with the structure of the heart that is present at birth. Such heart defects are the most common type of major birth defect. Most heart defects either obstruct blood flow in the heart or vessels near it, or cause blood to flow through the heart in an abnormal pattern, although other defects affecting heart rhythm can also occur.
Treatment for a defect can include medicines, surgery, and other medical procedures and heart transplants. The treatment depends on the type and severity of the defect and the child's age, size and general health. Also, certain mild defects that some children are born with are repaired over time by the body.
Lesson Summary
- The main components of the cardiovascular system are the heart, the blood vessels, and the blood. It moves nutrients, hormones, gases and wastes to and from body cells, and distributes heat to maintain homeostasis.
- Deoxygenated blood enters the right atrium from the body through the vena cava; oxygenated blood coming from the lungs through the pulmonary vein enters the left atrium. The atria then contract, pushing the blood into the ventricles. After a short delay, the ventricles contract, the oxygenated blood gets pushed through the aorta to the rest of the body, and the deoxygenated blood gets pushed to the lungs through the pulmonary arteries.
- Arteries have thick walls that have three major layers; an inner endothelial layer, a middle layer of smooth muscle, and an outer layer of stretchy connective tissue (mostly collagen). The thick, outer layer of a vein is made up of collagen-containing connective tissue. The connective tissue is wrapped around bands of smooth muscle while the interior is lined with endothelium. Most veins have one-way flaps called valves that prevent blood from flowing backward and pooling in the legs, feet, arms or hands due to the pull of gravity. The walls of capillaries are made of only a single layer of endothelial cells.
- The lymphatic system has three related functions; the removal of excess fluids from body tissues, the absorption of fats and transport of fat to the cardiovascular system, and the production of certain types of white blood cells.
- Atherosclerosis, which may lead to a heart attack, is a chronic inflammatory response in the walls of arteries that leads to a buildup of plaque. Plaque is made of cell debris, cholesterol, fatty acids, calcium, and fibrous connective tissue that build up around an area of inflammation. As a plaque grows it stiffens and narrows the artery, which reduces the flow of blood through the artery.
- Eating nutritious food, being physically active for 60 minutes on most days of the week, and avoiding smoking are three of the most effective things a person can do to avoid cardiovascular disease.
Summary Animation
Review Questions
- Why is the left ventricle generally thicker than the right ventricle?
- At what point do the pulmonary and systemic circulation systems meet up?
- Why do veins have valves?
Use the heart Figure below to answer the following four questions:
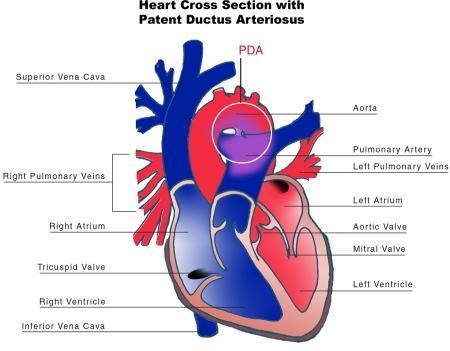
Figure 22.24
- What two structures are involved in the patent ductus arteriosus shown in this diagram. (Hint: The patent ductus arteriosus is the structure found inside the white circle at top center).
- Propose what might happen to blood flow around the site of the PDA.
- Would a PDA be considered a heart defect? Explain your answer.
- How might the PDA affect the body?
Use Figure below of the estimated prevalence of cardiovascular disease (CVD) in the U.S. population to answer the following three questions.
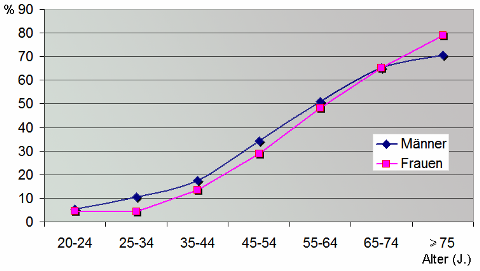
Figure 22.25
- What is the overall trend in the prevalence of CVD in the U.S. population?
- In what age group does the prevalence of CVD in the female population equal that of the male population?
- At what point does 50 percent of the male and female population have CVD?
Further Reading / Supplemental Links
Vocabulary
-
arteriole
-
Small diameter blood vessel that extends and branches out from an artery and leads to capillaries.
-
artery
-
Large, muscular vessels that carry blood away from the heart.
-
atria
-
Thin-walled blood collection chambers of the heart, pump blood into the ventricles (singular, atrium).
-
atrioventricular node
-
Conducts the electrical impulses that come from the SA node through the atria to the ventricles.
-
atrioventricular valves
-
Ensure blood flows from the atria to the ventricles.
-
blood pressure
-
The force exerted by circulating blood on the walls of blood vessels.
-
Bundle of His
-
A collection of heart muscle cells (fibers) specialized for electrical conduction that transmits the electrical impulses from the AV node.
-
cardiovascular system
-
An organ system that moves nutrients, hormones, gases and wastes to and from body cells, and distributes heat to maintain homeostasis.
-
capillary
-
Smallest of the body's blood vessels, connects arterioles and venules, and are important for the interchange of gases and other substances between blood and body cells.
-
coronary circulation
-
Supplies the heart tissue with blood.
-
diastole
-
Period of time when the heart relaxes after contraction.
-
heart
-
The muscular organ that pumps blood through the blood vessels by repeated, rhythmic contractions.
-
hypertension
-
Condition in which a person’s blood pressure is chronically high.
-
pulmonary circulation
-
Portion of the cardiovascular system which carries deoxygenated blood away from the heart, to the lungs, and returns oxygenated blood back to the heart.
-
Purkinje fibers
-
Specialized cardiac muscle cells that conduct action potentials into the ventricles, causing the cardiac muscle of the ventricles to contract in a controlled fashion.
-
semilunar valves
-
Present in the arteries leaving the heart, prevent blood flowing back from the arteries into the ventricles.
-
sinoatrial node
-
Known as the "cardiac pacemaker," found in the upper wall of the right atrium, is responsible for the wave of electrical stimulation that starts atrial contraction by creating an action potential.
-
sphygmomanometer
-
Measures arterial pressure.
-
systemic circulation
-
Portion of the cardiovascular system which carries oxygenated blood away from the heart, to the body, and returns deoxygenated blood back to the heart.
-
systole
-
Contraction of the heart chambers, which drives blood out of the chambers.
-
vascular resistance
-
Resistance to flow that blood must overcome to be pumped through your circulatory system.
-
vasoconstriction
-
Constriction of blood vessels by contracting the vascular smooth muscle in the vessel walls.
-
vasodilatation
-
Process by which blood vessels in the body become wider due to the relaxation of the smooth muscle in the vessel wall.
-
vein
-
Vessel that carries blood toward the heart.
-
ventricles
-
Heart chambers which collect blood from the atria and pump it out of the heart.
-
venule
-
Small vessel that allows deoxygenated blood to return from the capillaries to veins.
Points to Consider
- How may factors such as the region of the world in which you live or your type of employment contribute to your risk of developing cardiovascular disease?
- Hypothesize about the role of blood in your excretory system.
Lesson 22.2: Blood
Lesson Objectives
- List three functions of blood.
- Describe the composition of blood.
- Outline the process of blood clotting.
- Identify two major blood group systems.
- Outline the significance of blood type in transfusions.
- Describe two diseases of the blood.
Introduction
Blood is a fluid connective tissue. It circulates around the body through the blood vessels by the pumping action of the heart. Arterial blood carries oxygen and nutrient to all the body’s cells, and venous blood carries carbon dioxide and other metabolic wastes away from the cells.
In addition to the transport of gases, nutrients, and wastes, blood has many other functions that include:
- The removal of waste such as carbon dioxide, urea and lactic acid from the body tissues.
- The defense of the body against infection by microorganisms or parasites.
- The repair of damage to the body tissues.
- The transport of chemical messages, such as hormones and hormone-like substances.
- The control of body pH (the normal pH of blood is in the range of 7.35 - 7.45).
- The control of body temperature.
The Composition of Blood
Blood is a colloidal solution, it is made up of particles suspended in a fluid. It accounts for about 7% of the human body weight. The average adult has a blood volume of roughly 5 liters, composed of a fluid called plasma, and several kinds of cells. Within the blood plasma, are erythrocytes (red blood cells), leukocytes (white blood cells), thrombocytes (platelets) and other substances. The cells that make up the blood can be seen in Figure below.
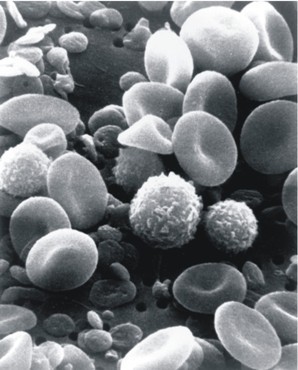
Figure 22.26
A scanning electron microscope (SEM) image of normal circulating human blood. One can see red blood cells, several white blood cells including knobby lymphocytes, a monocyte, a neutrophil, and many small disc-shaped platelets.
Plasma
Plasma is the golden-yellow liquid part of the blood. Plasma is 90% water and 10% dissolved materials including proteins, glucose, ions, hormones, and gases. It acts as a buffer, maintaining pH near 7.4. Plasma is about 54% the volume of blood; cells and fragments make up about 46% of the volume.
Red Blood Cells
Red blood cells, also known as erythrocytes, are flattened, doubly concave cells that carry oxygen. There are about 4 to 6 million cells per cubic millimeter of blood. Red blood cells make up about 45% of blood volume, as shown in Figure below. Each red blood cell has 200 million hemoglobin molecules. Humans have a total of 25 trillion red blood cells (about 1/3 of all the cells in the body). Red blood cells are continuously made in the red marrow of long bones, ribs, skull, and vertebrae. Each red blood cell lives for only 120 days, after which they are destroyed in liver and spleen.
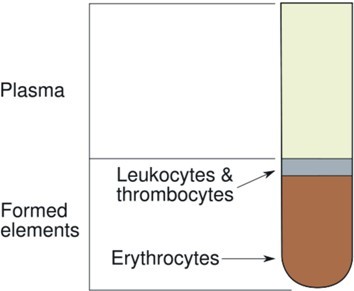
Figure 22.27
The components of blood. Red blood cells make up about 45% of the blood volume, white blood cells, about one percent, and platelets less than one percent. Plasma makes up the rest of the blood.
Mature red blood cells do not have a nucleus or other organelles. They contain the protein hemoglobin which gives blood its red color. The iron-containing heme portion of hemoglobin enables the protein to carry oxygen to cells. Heme binds to molecules of oxygen, which increases the ability of the blood to carry the gas.
Iron from hemoglobin is recovered and reused by red marrow. The liver degrades the heme units and secretes them as pigment in the bile, responsible for the color of feces. Each second two million red blood cells are produced to replace those thus taken out of circulation.
White Blood Cells
White blood cells, also known as leukocytes, are generally larger than red blood cells, as shown in Figure below. They have a nucleus, but do not have hemoglobin. White blood cells make up less than one percent of the blood's volume. They are made from stem cells in bone marrow. They function in the cellular immune response. There are five types of white blood cells. Neutrophils enter the tissue fluid by squeezing through capillary walls and phagocytizing (swallowing) foreign bodies. Macrophages also swallow and destroy cell debris and bacteria or viruses. In Figure below, a macrophage is shown phagocytizing two particles, possibly pathogens. Macrophages also release substances that cause the numbers of white blood cells to increase. Antigen-antibody complexes are swallowed by macrophages. Lymphocytes fight infection. T-cells attack cells containing viruses. B-cells produce antibodies. To learn more about the role of white blood cells in fighting infection, refer to the Immune System and Disease chapter.
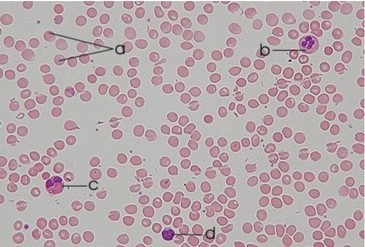
Figure 22.28
Relative sizes of red and white blood cells. a - red blood cells; b neutrophil; c - eosinophil; d lymphocyte. b, c, and d are different types of white blood cells.
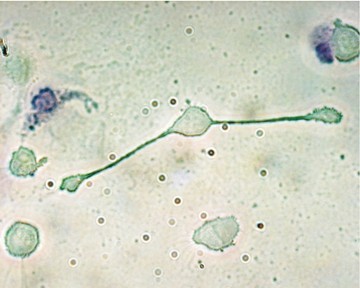
Figure 22.29
Macrophage showing cytoplasmic extensions that allow it to swallow particles or pathogens. In the image here, a mouse macrophage stretches its arms to engulf two particles at once.
Platelets
Platelets, also known as thrombocytes, are important in blood clotting. Platelets are cell fragments that bud off bone marrow cells called megakaryocytes. A platelet is shown in Figure below. They make up less than one percent of blood volume. Platelets carry chemicals essential to blood clotting. They change fibrinogen into fibrin, a protein that creates a mesh onto which red blood cells collect, forming a clot. This clot stops more blood from leaving the body and also helps to prevent bacteria from entering the body. Platelets survive for 10 days before being removed by the liver and spleen. There are 150,000 to 300,000 platelets in each milliliter of blood. Platelets stick to tears in blood vessels and they release clotting factors.
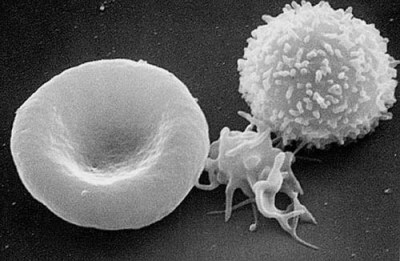
Figure 22.30
Cells of the blood. From left to right: Red blood cell, platelet, white blood cell. The concave side of red blood cells can be seen. Both sides of red blood cells are concave. The biconcave shape gives the red blood cells a smaller surface to volume ratio, which allows them to pick up large amounts of oxygen.
Other Blood Components
Blood plasma also contains other substances other than water. Some important components of blood include:
- Serum albumin: a plasma protein that acts as a transporter of hormones and other molecules.
- Antibodies: proteins that are used by the immune system to identify and destroy foreign objects such as bacteria and viruses.
- Hormones: chemical messengers that are produced by one cell and carried to another.
- Electrolytes such as sodium (Na+) and chloride (Cl-) ions.
Production and Breakdown of Blood Cells
Blood cells are produced in the red and yellow bone marrow in a process called hematopoiesis. Blood cells are broken down by the spleen and certain cells in the liver. The liver also clears some proteins, lipids and amino acids from the blood. The kidney actively secretes waste products of the blood into the urine.
Functions of Blood
Transport of Oxygen
The hemoglobin molecule is the major transporter of oxygen in mammals, including humans and many other species. About 98.5 percent of the oxygen in a sample of arterial blood in a healthy human is bonded with hemoglobin. Only 1.5 percent of the oxygen in blood is not carried by hemoglobin, instead it is dissolved in the plasma.
Under normal conditions in humans at rest, the hemoglobin in the red blood cells that are leaving the lungs is about 98 to 99 percent saturated with oxygen, and the blood is referred to as oxygenated. In a healthy adult at rest, deoxygenated blood returning to the lungs is still 75 percent saturated with oxygen. Oxygen saturation of arterial blood at or below 95 percent is considered dangerous in an individual at rest (for instance, during surgery under anesthesia)
Substances other than oxygen can bind to the hemoglobin; in some cases this can cause irreversible damage to the body. The gas carbon monoxide, for example, is very dangerous when absorbed into the blood. It bonds irreversibly with hemoglobin, which reduces the volume of oxygen that can be carried in the blood. Carbon monoxide poisoning can very quickly cause suffocation and death. Carbon monoxide is released during combustion (fire). It is released by cigarettes, barbeque grills, combustion of petrol products in cars and trucks, or anything else that can be burned.
Transport of Carbon Dioxide
When systemic arterial blood flows through capillaries, carbon dioxide diffuses from the tissues into the blood. Some carbon dioxide is dissolved in the blood. The remaining carbon dioxide is converted to bicarbonate and hydrogen ion which is then carried in the blood to the lungs, where it is converted back to carbon dioxide and released into the lungs.
Thermoregulation
Blood circulation transports heat through the body, and adjustments to this flow are an important part of thermoregulation. Increasing blood flow to the surface (e.g. during warm weather or strenuous exercise) causes warmer skin, resulting in greater heat loss. Decreasing surface blood flow conserves heat.
Blood Clotting
Coagulation, or blood clotting, is a complex process by which blood forms solid clots. Coagulation is important to stop bleeding and begin repair of damaged blood vessels. Blood clotting disorders can lead to an increased risk of bleeding or clotting inside a blood vessel. Platelets are important for the proper coagulation of blood.
Clotting is started almost immediately when an injury damages the endothelium of a blood vessel. Platelets clump together, forming a plug at the site of injury. Then, proteins in the plasma called coagulation factors, respond in a series of chemical reactions that form a tough protein called fibrin. The fibrin strands form a web across the platelet plug, trapping red blood cells before they can leave through the wound site. This mass of platelets, fibrin, and red blood cells forms a clot that hardens into a scab.
Certain nutrients are needed for the proper functioning of the clotting mechanism. Two of these are calcium and vitamin K. Luckily for you, bacteria that live in your intestines make enough vitamin K so you do not need to have extra in your food.
Blood Types
Blood type (also called a blood group), is determined by the presence or absence of certain molecules, called antigens, on the surface of red blood cells. An antigen is a molecule or substance that causes an immune response. Blood type antigens may be proteins, or carbohydrates, depending on the blood group system. The antigens on a person’s own body cells are recognized by their immune system as “self” antigens, and their immune system does not attack them. However, if a person is exposed to a blood group antigen that is different from their own blood group, the person’s immune system will produce antibodies against the donor blood antigens. These antibodies can bind to antigens on the surface of transfused red blood cells (or other tissue cells) often leading to destruction of the cells by the immune system.
The erythrocyte surface antigens that have one allele, or a group of very closely linked genes, are collectively called a "blood group system". There are 29 known blood group systems in humans, but the ABO blood group system and the Rhesus (Rh) blood group system are the most important for blood transfusions.
ABO Blood Group System
In 1875, a German physiologist, Leonard Landois reported that the blood cells of a human and an animal would clump together when mixed. In the early 1900s, Austrian biologist and physician Karl Landsteiner pointed out that a similar clumping reaction occurred when the blood of one person was transfused with another. He determined that this might be the cause of shock, jaundice, and release of hemoglobin that had followed some earlier attempts at person-to-person blood transfusions.
In 1909, Landsteiner classified blood into the A, B, AB, and O groups. He also showed that transfusions between of the same blood group did not result in the destruction of blood cells and that clumping occurred only when a person was transfused with the blood of a person belonging to a different blood group.
The "A" and "B" of the ABO blood group refer to two carbohydrate antigens found on the surface of red blood cells. There is not an O antigen. Type O red blood cells do not have either type A or B antigens on their surface, as listed in Table below. Antibodies are found in the blood plasma. The blood type of a person can be determined by using antibodies that bind to the A or B antigens of red blood cells.
Blood Types, Antigen Types, and Antibody Types
|
Blood Type
|
Antigen Type
|
Serum (Plasma) Antibodies
|
Can Receive Blood from Types
|
Can Donate Blood to Types
|
|
A
|
A
|
anti-B
|
A, O
|
A, AB
|
|
B
|
B
|
anti-A
|
B, O
|
B, AB
|
|
AB
|
A and B
|
none
|
AB, A, B, O
|
AB
|
|
O
|
none
|
anti-A, anti-B
|
O
|
AB, A, B, O
|
(Source: CK12 Foundation, License: CC-BY-SA)
Agglutination is the clumping of red blood cells that occurs when different blood types are mixed together, shown in Figure below. It involves a reaction between antigens on the surface of red blood cells and protein antibodies in the blood plasma. Mixing different blood types together can cause agglutination, a process that has been used as a way of determining a person’s blood type.
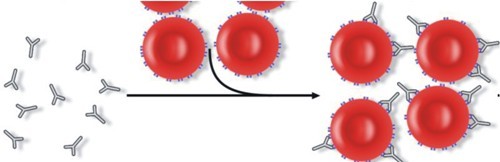
Figure 22.31
Antigens on the red blood cell surface. Antibodies attach to the antigens on the red blood cell, causing the blood cells to clump together. This leads to agglutination of the blood.
Rhesus Blood Group System
The Rhesus system is the second most significant blood group system in human blood transfusion. The most significant Rhesus antigen is called the RhD antigen, also called Rhesus factor. A person either has, or does not have the RhD antigen on the surface of their red blood cells. This is usually indicated by "RhD positive" (does have the RhD antigen) or "RhD negative" (does not have the antigen) suffix to the ABO blood group (see blood agglutination test in Figure below).
The Rhesus system is named after the Rhesus monkey, in which the antigen was first discovered by Karl Landsteiner and Alexander S. Wiener in 1937. The importance of the Rh factor was realized soon after. Dr. Phillip Levine, a pathologist who worked at a New York hospital, made the connection between the Rh factor and the incidence of a blood disease in newborn babies. The disease, called hemolytic disease of the newborn is a condition that develops while the fetus is in the womb. If a mother is RhD negative, and the father is RhD positive, the fetus may inherit the dominant RhD positive trait from the father. The RhD negative mother can make antibodies against the RhD antigens of her developing baby. This can happen if some of the fetus' blood cells pass into the mother's blood circulation, or if the mother has received an RhD positive blood transfusion.
The fetus’ red cells are broken down and the fetus can develop anemia. This disease ranges from mild to very severe, and fetal death from heart failure can occur. Most RhD disease can be prevented by treating the mother during pregnancy or soon after childbirth. The mother is injected with anti-RhD antibodies, so that the baby’s red blood cells are destroyed before her body can produce antibodies against them. If a pregnant woman is known to have anti-RhD antibodies, the RhD blood type of a fetus can be tested by analysis of fetal DNA in maternal plasma to assess the risk to the fetus of Rh disease.
The presence or absence of the ABO group antigens and the RhD antigens are always determined for all recipient and donor blood. Figure below shows a routine way in which a person’s ABO blood group is determined.
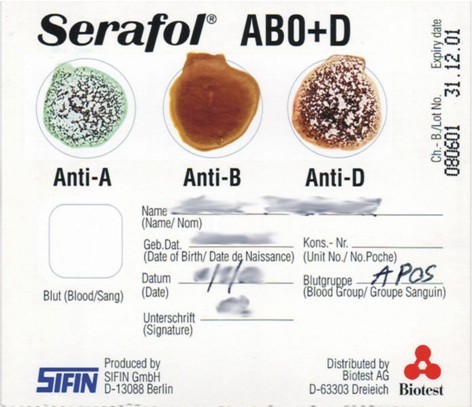
Figure 22.32
A bedside blood grouping card showing the agglutination of the blood with anti-A and anti-Rh(D), but not with anti-B. Therefore the blood group is A positive. This method of blood grouping relies on seeing an agglutination reaction to determine a persons blood group. The card has dried blood group antibody reagents fixed onto its surface. A drop of the persons blood is placed on each area on the card. The presence or absence of visual agglutination allows a quick method of determining the ABO and Rhesus group of the person.
Blood Products
In order to provide maximum benefit from each blood donation and to extend shelf-life, blood banks separate some whole blood into several different products. Some of the most common of these products are packed red blood cells, plasma, platelets, and fresh frozen plasma. Units of packed red blood cells are made by removing as much of the plasma as possible from whole blood units. Clotting factors made by genetic engineering are now routinely used for the treatment of the clotting disorder hemophilia, so the risk of possible infection from donated blood products is avoided.
Universal Donors and Universal Recipients
Regarding the donation of packed red blood cells, individuals with type O negative blood are often called universal donors, and those with type AB positive blood are called universal recipients. Type O red blood cells do not have the A or B antigens, and can be given to people with a different ABO blood group. The blood plasma of an AB person does not contain any anti-A or anti-B antibodies, so they can receive any ABO blood type. The possible reactions of anti-A and anti-B antibodies in the donor blood to the recipient’s red blood cells are usually not a problem because only a small volume of plasma that containing antibodies is given to the recipient. Refer to Table above for a complete listing of ABO antigens and antibodies that are involved in the ABO system.
In April 2007 researchers discovered a way to convert blood types A, B, and AB to O; the method used enzymes that removed the antigens on the surface of the red blood cells.
Other Blood Group Systems
You probably have heard a lot about the ABO and Rhesus (RhD) blood group systems by now, but you have probably not heard much about the other 27 other systems. Many other antigens are found on the cell membrane of red blood cells. For example, an individual can be AB RhD positive, and at the same time M and N positive (MNS system), K positive (Kell system), Lea or Leb negative (Lewis system), Duffy positive, or Duffy negative (Duffy system), and so on, being positive or negative for each blood group system antigen. Many of the blood group systems were named after the patients in whom the antibodies were first found.
Some blood group systems are associated with a disease, for example, the Kell antigen is associated with McLeod syndrome, a genetic disorder in which the red blood cells are spiky shaped. Certain other blood group systems may affect resistance to infections, an example being the resistance to specific malaria species seen in individuals who lack the Duffy antigen. The Duffy antigen is less common in ethnic groups from areas with a high incidence of malaria.
Rare blood types can cause supply problems for blood banks and hospitals. For example Duffy-negative blood occurs much more frequently in people of African origin, and the rarity of this blood type in the rest of the population can result in a shortage of Duffy-negative blood. Similarly, for RhD negative people, there is a risk associated with traveling to parts of the world where supplies of RhD negative blood are rare, particularly East Asia.
Homeostatic Imbalances of the Blood
Problems can occur with red blood cells, white blood cells, platelets, and other components of the blood. Many blood disorders are genetic, they are inherited from a parent, some are a result of nutrient deficiency, while others are cancers of the blood.
Sickle-cell disease is a group of genetic disorders caused by abnormally shaped hemoglobin, called sickle hemoglobin. In many forms of the disease, the red blood cells change shape because the abnormal hemoglobin proteins stick to each other, causing the cell to get a rigid surface and sickle shape, shown in Figure below. This process damages the membrane of the red blood cell, and can cause the cells to get stuck in blood vessels. This clotting causes oxygen starvation in tissues, which may cause organ damage such as stroke or heart attack. The disease is chronic and lifelong. Individuals are most often well, but their lives are punctuated by periodic painful attacks. Sickle-cell disease occurs more commonly in people (or their descendants) from parts of the world such as sub-Saharan Africa, where malaria is or was common. It also occurs in people of other ethnicities. As a result, those with sickle cell disease are resistant to malaria since the red blood cells are not favored by the malaria parasites. The mutated hemoglobin allele is recessive, meaning it must be inherited from each parent for the individual to have the disease.
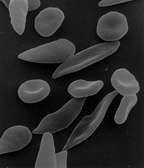
Figure 22.33
Sickle-cell disease. The abnormal shape of the red blood cells damages the red blood cells which causes them to get stuck in blood vessels. The blocked capillaries reduce the blood flow to an organ, and can result in pain and organ damage.
Iron deficiency anemia is the most common type of anemia. It occurs when the dietary intake or absorption of iron is less than what is needed by the body. As a result, hemoglobin, which contains iron, cannot be made. In the United States, 20 percent of all women of childbearing age have iron deficiency anemia, compared with only 2 percent of adult men. The principal cause of iron deficiency anemia in premenopausal women is blood lost during menstruation.
Leukemia is a cancer that originates in the bone marrow and is characterized by an abnormal production of white blood cells (rarely red blood cells) that are released into the bloodstream. Lymphoma is a cancer of the lymphatic system, which helps to filter blood. Lymphoma can be categorized as either Hodgkin's lymphoma or non-Hodgkin's lymphoma.
Hemophilia is the name of a group of hereditary genetic diseases that affect the body's ability to control blood clotting. Hemophilia is characterized by a lack of clotting factors in the blood. Clotting factors are needed for a normal clotting process. When a blood vessel is injured, a temporary scab does form, but the missing coagulation factors prevent the formation of fibrin which is needed to maintain the blood clot. Therefore, a person who has hemophilia is initially able to make a clot to stop the bleeding, but because fibrin is not produced, the body is unable to maintain a clot for long. The risks of the re-bleeding of an injury and internal bleeding are increased in hemophilia, especially into muscles, joints, or bleeding into closed spaces.
Haemochromatosis is a hereditary disease that is characterized by a buildup of iron in the body. Iron accumulation can eventually cause end organ damage, most importantly in the liver and pancreas, manifesting as liver failure and diabetes mellitus respectively. It is estimated that roughly one in every 300-400 people is affected by the disease, primarily of Northern European and especially people of Irish, Scottish, Welsh and English descent.
Lesson Summary
- The functions of blood include the removal of wastes such as carbon dioxide, urea and lactic acid from the body tissues; defense of the body against infection by microorganisms or parasites; repair of damage to the body tissues; transport of chemical messages, such as hormones and hormone-like substances; control of body pH; control of body temperature.
- Within the blood plasma are the red blood cells, white blood cells, platelets, and other substances. Red blood cells are the most common types of cells in the blood, they make up about 45 percent of blood volume.
- Blood clotting begins when the endothelium of a blood vessel is torn. Platelets clump together, forming a plug at the site of injury. Then, the coagulation factors cause a series of chemical reactions that form fibrin. The fibrin strands form a web across the platelet plug, trapping red blood cells before they can leave through the wound site. This mass of platelets, fibrin, and red blood cells forms a clot that hardens into a scab.
- There are 29 blood group systems, but the two major ones are the ABO and Rhesus systems.
- The ABO system is of great importance in blood transfusions. Individuals with type O negative blood are called universal donors, and those with type AB positive blood are called universal recipients. Type O red blood cells do not have the A or B antigens, and can be given to people with a different ABO blood group. The blood plasma of an AB person does not contain any anti-A or anti-B antibodies, so they can receive any ABO blood type.
- Iron deficiency anemia is the most common type of anemia. It occurs when the dietary intake or absorption of iron is less than what is needed by the body. As a result, hemoglobin, which contains iron, cannot be made. Hemophilia is the name of a group of hereditary genetic diseases that affect the body's ability to control blood clotting. Hemophilia is characterized by a lack of clotting factors in the blood.
Review Questions
- Name the four main components of blood.
- How does the structure of a red blood cell relate to its function?
- Name one other gas that can bind to hemoglobin, and identify an affect that such binding can have on homeostasis.
- Why might iron-deficiency anemia cause a person to feel tired?
- Identify two different types of human blood systems.
- Identify the processes involved in blood clotting.
- A sample of blood taken from a patient has elevated (higher than normal) levels of leucocytes. What could this mean?
- Identify where in the body red blood cells and white blood cells are made.
- Explain why taking erythropoietin (EPO), which stimulates the production of more red blood cells, is considered a form of cheating in sports.
Further Reading / Supplemental Links
Vocabulary
-
agglutination
-
The clumping of red blood cells that occurs when different blood types are mixed together.
-
antibodies
-
Proteins that are used by the immune system to identify and destroy foreign objects such as bacteria and viruses.
-
blood
-
A fluid connective tissue; arterial blood carries oxygen and nutrient to all the body’s cells, and venous blood carries carbon dioxide and other metabolic wastes away from the cells.
-
blood type (blood group)
-
Determined by the presence or absence of certain molecules, called antigens, on the surface of red blood cells.
-
coagulation
-
Blood clotting, a complex process by which blood forms solid clots.
-
coagulation factors
-
Proteins in the plasma which respond damage to a blood vessel; response includes a series of chemical reactions that form a tough protein called fibrin.
-
erythrocytes
-
Red blood cells; flattened, doubly concave cells that carry oxygen.
-
haemochromatosis
-
A hereditary disease that is characterized by a buildup of iron in the body; can eventually cause end organ damage, most importantly in the liver and pancreas, manifesting as liver failure and diabetes mellitus respectively.
-
hematopoiesis
-
The production of blood cells in the red and yellow bone marrow.
-
heme
-
The iron-containing portion of hemoglobin; enables the protein to carry oxygen to cells.
-
hemoglobin
-
Protein in red blood cells that carries oxygen.
-
hemophilia
-
The name of a group of hereditary genetic diseases that affect the body's ability to control blood clotting.
-
hormones
-
Chemical messengers that are produced by one cell and carried to another.
-
leukemia
-
A cancer that originates in the bone marrow and is characterized by an abnormal production of white blood cells.
-
leukocytes
-
White blood cells; function in the cellular immune response; includes neutrophils, eosinophils, and macrophages.
-
lymphoma
-
A cancer of the lymphatic system, which helps to filter blood; can be categorized as either Hodgkin's lymphoma or non-Hodgkin's lymphoma.
-
plasma
-
The golden-yellow liquid part of the blood; 90% water and 10% dissolved materials including proteins, glucose, ions, hormones, and gases.
-
serum albumin
-
A plasma protein that acts as a transporter of hormones and other molecules.
-
sickle-cell disease
-
A group of genetic disorders caused by abnormally shaped hemoglobin, called sickle hemoglobin.
-
thrombocytes
-
Platelets; important in blood clotting; cell fragments that bud off bone marrow cells called megakaryocytes.
-
universal donors
-
Individuals with type O negative blood.
-
universal recipients
-
Individuals with type AB positive blood.
Points to Consider
- How might the composition of your blood change during a 24-hour period?
- What do you think is the relationship between the cardiovascular system, blood, and the respiratory system?
Lesson 22.3: Respiratory System
Lesson Objectives
- Distinguish between external and internal respiration.
- Identify the structures of the respiratory system.
- Outline the process of inhalation.
- Describe how carbon dioxide is carried in the blood.
- Compare the causes of emphysema and asthma.
Introduction
Have you ever wondered what it would be like to have gills? You would breathe and look very different from the rest of us, but they would be great for swimming and diving! Despite such differences, the main functions of lungs and gills are the same: to obtain oxygen, and to release carbon dioxide.
The human respiratory system brings oxygen, O2, into the body and releases carbon dioxide, CO2, into the atmosphere. Oxygen is drawn in through the respiratory tract, which is shown in Figure below, and is then delivered to the blood. This process is called external respiration. The exchange of gases between the blood and the cells of the body is called internal respiration.
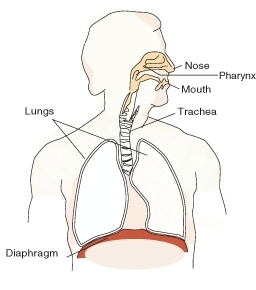
Figure 22.34
The respiratory system. Air moves down the trachea, a long straight tube in the chest. The diaphragm pulls air in and pushes it out. Respiratory systems of various types are found in a wide variety of organisms.
Comparing "Cellular Respiration" and "Respiration"
Respiration is the transport of oxygen from the outside air to the cells of the body, and the transport of carbon dioxide in the opposite direction. This is in contrast to the biochemical definition of respiration, which refers to cellular respiration. Cellular respiration is the metabolic process by which an organism obtains energy by reacting oxygen with glucose to give water, carbon dioxide and ATP (energy). Although respiration is necessary to sustain cellular respiration and thus life in animals, the processes are very different. Cellular respiration takes place in individual cells of the animal, while respiration involves the transport of metabolites between the organism and external environment.
Structures of the Respiratory System
The nose and nasal cavity filter, warm, and moisten the inhaled air. The nose hairs and mucus produced by the epithelial cells in the nose catch airborne particles and prevent them from reaching the lungs.
Behind the nasal cavity, air next passes through the pharynx, a long tube that is shared with the digestive system. Both food and air pass through the pharynx. A flap of connective tissue called the epiglottis closes over the trachea when food is swallowed to prevent choking or inhaling food. In humans the pharynx is important in vocalization
The larynx, also called the voicebox, is found just below the point at which the pharynx splits into the trachea and the esophagus, shown in Figure below. The voice is generated in the larynx. Air from the lungs is needed for the vocal folds to produce speech.
The trachea, or wind pipe, is a long tube that leads down to the chest where it divides into the right and left bronchi in the lungs. The bronchi branch out into smaller bronchioles, which are the first airway passages that do not contain cartilage. The bronchioles lead into the alveoli, which are the multi-lobed sacs in which most of the gas exchange occurs.
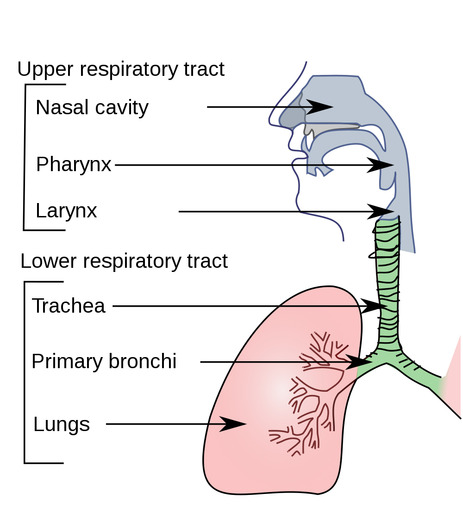
Figure 22.35
The structures of the respiratory system include the nasal cavity, the pharynx, larynx, which together are the upper respiratory tract. The trachea, bronchi, bronchioles and alveoli are part of up the lower respiratory tract.
The Journey of a Breath of Air
In air-breathing vertebrates such as humans, respiration of oxygen includes four stages:
- Ventilation from the atmosphere into the alveoli of the lungs.
- Pulmonary gas exchange from the alveoli into the pulmonary capillaries.
- Gas transport from the pulmonary capillaries through the circulation to the peripheral capillaries in the organs.
- Peripheral gas exchange from the tissue capillaries into the cells and mitochondria.
Ventilation: From the Air to the Alveoli
Air enters the body through the nose, is warmed, filtered, and passed through the nasal cavity. Air passes the pharynx (which has the epiglottis that prevents food from entering the trachea). The upper part of the trachea contains the larynx. The vocal cords are two bands of tissue that extend across the opening of the larynx. After passing the larynx, the air moves into the trachea. The trachea is a long tube that divides into two smaller tubes called bronchi which lead into each lung, shown in Figure above. Bronchi are reinforced to prevent their collapse and are lined with ciliated epithelium and mucus-producing cells. Bronchi branch into smaller and smaller tubes called bronchioles. Bronchioles end in grape-like clusters called alveoli. Alveoli are surrounded by a network of thin-walled capillaries, shown in Figure below.
Breathing in, or inhaling, is usually an active movement, contraction of the diaphragm muscles uses ATP. The diaphragm is a muscle that is found below the lungs (shown in Figure above). Contraction of the diaphragm causes the volume of the chest cavity to increase, and the air pressure within the lungs to decrease. The pressure difference causes air to rush into the lungs. Relaxation of the diaphragm causes the lungs to recoil and air is pushed out of the lungs. Breathing out, or exhaling, is normally a passive process powered by the elastic recoil of the chest, similar to letting the air out of a balloon.
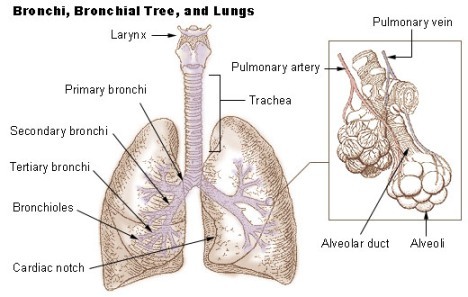
Figure 22.36
The alveoli are the tiny grape-like structures within the lungs, and are the site of pulmonary gas exchange.
Pulmonary Gas Exchange: From the Alveoli into the Pulmonary Capillaries
Breathing is only part of the process of delivering oxygen to where it is needed in the body. The process of gas exchange occurs in the alveoli by diffusion of gases between the alveoli and the blood passing in the lung capillaries, as shown in Figure below. Recall that diffusion is the movement of substances from an area of higher concentration to an area of lower concentration. The difference between the high concentration of O2 in the alveoli and the low O2 concentration of the blood in the capillaries is enough to cause O2 molecules to diffuse across the thin walls of the alveoli and capillaries and into the blood. CO2 moves out of the blood and into the alveoli in a similar way. The greater the concentration difference, the greater the rate of diffusion.
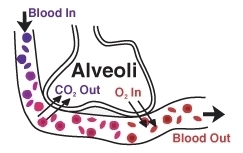
Figure 22.37
Gas exchange happens in the lungs through diffusion. Deoxygenated blood has a high concentration of CO and a low O concentration. CO moves out of the blood and into the alveoli, where the concentration of CO is lower. Likewise, O moves from an area of higher concentration (the alveoli), to an area of lower concentration (the blood).
Breathing also results in loss of water from the body. Exhaled air has a relative humidity of 100 percent because of the diffusion of water that from the moist surface of the breathing passages and the alveoli into the warm exhaled air.
In the lungs, oxygen is transported across the thin membranes of the alveoli and the border of the capillary and attracted to the hemoglobin molecule within the red blood cell.
After leaving the lungs, the oxygenated blood returns to the heart to be pumped through the aorta and around the body. The oxygenated blood travels through the aorta, to the smaller arteries, arterioles, and finally to the peripheral capillaries where gas exchange occurs.
Peripheral Gas Exchange: From Capillaries into Cells, and from Cells into Capillaries
The oxygen concentration in body cells is low, while the blood that leaves the lungs is 97 percent saturated with oxygen. So, oxygen diffuses from the blood into the body cells when it reaches the peripheral capillaries (the capillaries in the systemic circulation).
Carbon dioxide concentration in metabolically active cells is much greater than in capillaries, so carbon dioxide diffuses from the cells into the capillaries. Most of the carbon dioxide (about 70 percent) in the blood is in the form of bicarbonate (HCO3-). A small amount of carbon dioxide dissolves in the water in the plasma to form carbonic acid (H2CO3). Carbonic acid and bicarbonate play an important role in regulating the pH of the body.
In order to remove CO2 from the body, the bicarbonate is picked up by a red blood cell, and is again turned in to carbonic acid. A water molecule (H2O) is then taken away from the carbonic acid, and the remaining CO2 molecule is expelled from the red blood cells and into the alveoli where it is exhaled. The following equation shows this process:
HCO3- + H+ ⇌ H2CO3 ⇌ CO2 + H2O
Gas exchange between your body and the environment occurs in the alveoli. The alveoli are lined with pulmonary capillaries, the walls of which are thin enough to permit the diffusion of gases. Inhaled oxygen diffuses into the pulmonary capillaries, where it binds to hemoglobin in the blood. Carbon dioxide diffuses in the opposite direction, from capillary blood to alveolar air. At this point, the pulmonary blood is oxygen-rich, and the lungs are primarily holding carbon dioxide. Exhalation follows, thereby ridding the body of the carbon dioxide and completing the cycle of respiration.
Gas Exchange and Homeostasis
The equilibrium between carbon dioxide and carbonic acid is very important for controlling the acidity of body fluids. As gas exchange occurs, the pH balance of the body is maintained as part of homeostasis. If proper respiration is interrupted two things can occur:
- Respiratory acidosis, in which arterial blood contains too much carbon dioxide, causing a drop in blood pH.
- Respiratory alkalosis results from increased respiration (or hyperventilation) which causes a drop in the amount of carbon dioxide in the blood plasma. The drop in carbon dioxide concentration causes the blood pH to rise.
Control of Breathing by the Nervous System
Breathing is one of the few bodily functions which, within limits, can be controlled both consciously and unconsciously. Conscious attention to breathing is common in activities such as yoga, swimming, and karate. In speech or vocal training, a person learns to discipline his or her breathing for purposes other than life support.
Muscular contraction and relaxation controls the rate of expansion and constriction of the lungs. These muscles are controlled by the autonomic nervous system from the parts of the brainstem that control breathing: the medulla and the pons. This area of the brainstem forms the respiration regulatory center. When carbon dioxide levels increase in the blood (in the form of carbonic acid), such as during exercise, the pH level of the blood drops. This causes the medulla to send nerve impulses to the diaphragm and the muscles between the ribs, causing them to contract and increase the rate of breathing. This automatic control of respiration can be impaired in premature babies, or by drugs or disease.
Without breathing, the body’s oxygen levels drop dangerously low within minutes, leading to permanent brain damage followed by death. It is not possible for a healthy person to voluntarily stop breathing indefinitely. If we do not inhale, the level of carbon dioxide builds up in our blood and we experience great air hunger. Eventually, not breathing leads to a loss of consciousness at which time the autonomic nervous system takes control and initiates breathing.
Inhalation
Inhalation is started by the diaphragm and supported by the external intercostal muscles (the muscles that are between the ribs). It is an active process that needs ATP. When the diaphragm contracts, the ribcage expands and the contents of the abdomen are moved downward. This results in a larger thoracic (chest) volume, which in turn causes a decrease in air pressure inside the lungs. As the pressure in the chest falls, air from outside the body moves into the respiratory system. Normal resting respirations are 10 to 18 breaths per minute. During an average breath, an adult will exchange from 500 ml to 700 ml of air. The average breath capacity of a person is called lung volume, or tidal volume.
Exhalation
Exhalation is generally a passive process, however active, or forced, exhalation is carried out by the abdominal and the internal intercostal muscles. The lungs have a natural elasticity and as they recoil from the stretch of inhalation, air flows out of the lungs until the pressures in the chest and the atmosphere reach equilibrium. During forced exhalation, as when blowing out a candle, expiratory muscles including the abdominal muscles and internal intercostal muscles generate pressure in the chest and abdomen, which forces air out of the lungs.
Homeostatic Imbalances of the Respiratory System: Diseases and Disorders
Respiratory disease is the term for diseases of the lung, bronchial tubes, trachea and throat. These diseases range from mild, such as a cold, to being possibly life-threatening, such as bacterial pneumonia.
Respiratory diseases can be grouped as either obstructive (conditions which lower the rate of the airflow into and out of the lungs, such as in asthma) or restrictive (conditions that cause a reduction in the functional volume of the lungs, such as emphysema.)
Emphysema is a chronic lung disease caused by loss of elasticity of the lung tissue. The destruction of elastic structures that support the alveoli and the capillaries that feed the alveoli cause them to become hard and stiff. Eventually the walls of the alveoli break down and the alveoli become larger. The amount of oxygen that can enter the blood with each breath is reduced because the large alveoli cannot function efficiently; much of the oxygen that gets into the large alveoli cannot be absorbed into the blood so the oxygen is unused. Symptoms include shortness of breath on exertion (usually when climbing stairs or a hill, and later at rest), and an expanded chest. Damage to the alveoli, which can be seen in Figure below, is irreversible. Smoking is a leading cause of emphysema.

Figure 22.38
The inside of a lung showing the characteristics of emphysema due to smoking. Instead of alveoli, the cut surface shows multiple cavities lined by heavy black carbon deposits.
Bronchitis is an inflammation of the bronchi. Acute bronchitis is usually caused by viruses or bacteria and may last several days or weeks. Acute bronchitis is characterized by cough and phlegm (mucus) production. Symptoms are related to the inflammation of the airways and phlegm production, and include shortness of breath and wheezing. Chronic bronchitis is not necessarily caused by infection and is generally part of a syndrome called chronic obstructive pulmonary disease (COPD). Chronic bronchitis is defined clinically as a persistent cough that produces phlegm and mucus, for at least three months in two consecutive years.
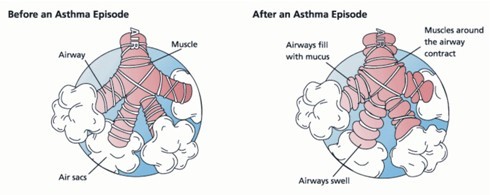
Figure 22.39
Asthma narrows the airways by causing allergy-induced spasms of surrounding muscles, narrowing of the airway, and excessive production of phlegm (mucus), which clogs the airways. The airway constriction responds to medicines called bronchodilators which relax the muscles. The feeling of breathlessness is somewhat like being able to breath only through a straw while walking.
Asthma is a chronic illness in which the airways narrow and becomes inflamed, as shown in Figure above. Excessive amounts of mucus are also made by the lungs. Asthma often happens in response to one or more triggers. It may be triggered by exposure to an allergen such as mold, dust, or pet hair. It can also be caused by cold air, warm air, moist air, exercise, or emotional stress. In children, the most common triggers are viral illnesses such as those that cause the common cold. This airway narrowing causes symptoms such as wheezing, shortness of breath, chest tightness, and coughing. Some people with asthma, especially children, can become very frightened by the symptoms, which may cause even more breathing distress. Between asthma attacks, most patients feel well but can have mild symptoms and may remain short of breath after exercise for longer periods of time than a person who does not have asthma. The symptoms of asthma, which can range from mild to life threatening, can usually be controlled with a combination of medicines and environmental changes.
Public attention in the developed world has recently focused on asthma because of the increasing numbers of cases, affecting up to one in four children who live in cities.
Pneumonia is an illness in which the alveoli become inflamed and flooded with fluid. Effective gas exchange cannot happen across the alveoli membranes. Pneumonia can result from a variety of causes, including infection with bacteria, viruses, fungi, or parasites, and chemical or physical injury to the lungs. Symptoms of pneumonia include cough, chest pain, fever, and difficulty in breathing. Treatment depends on the cause of pneumonia; bacterial pneumonia is treated with antibiotics.
Pneumonia is a common illness which occurs in all age groups, and is a leading cause of death among the elderly and people who are chronically and terminally ill. Vaccines to prevent certain types of pneumonia are available.
Tuberculosis (TB) is a common and deadly infectious disease caused by a type of bacteria called Mycobacterium tuberculosis. TB most commonly attacks the lungs (as pulmonary TB) but can also affect the central nervous system, the lymphatic system, the circulatory system, the genitourinary system, bones, joints and even the skin.
Over one-third of the world's population has been exposed to the TB bacterium. Not everyone infected develops the disease, so TB infection without symptoms (called a latent infection) is most common. However, one in ten latent infections will progress to active TB disease, which, if left untreated, kills more than half of its victims.
The rise in HIV infections and the neglect of TB control programs have led to an increase in cases of tuberculosis. The development of drug-resistant strains has also contributed to this new epidemic. For example, between 2000 and 2004, about 20 percent of TB cases were resistant to standard antibiotic treatments. TB incidence varies widely, even in neighboring countries, apparently because of differences in health care system standards. A TB vaccine, called Bacille Calmette-Guérin (BCG), is available to people in some countries. The BCG is prepared from a strain of weakened live mycobacterium, which has lost its virulence in humans. The effectiveness of the BCG is a matter of debate among researchers, and the governments in some countries, including the United States, do not require people to get the BCG vaccination.
Lung cancer is a disease where epithelial (internal lining) tissue in the lung grows out of control. This leads to invasion of nearby tissue and growth of the tumor beyond the lungs. Lung cancer, which is the most common cause of cancer-related death in men and the second most common in women, is responsible for 1.3 million deaths worldwide every year The most common symptoms are shortness of breath, coughing (including coughing up blood), and weight loss.
The most common cause of lung cancer is exposure to tobacco smoke. The occurrence of lung cancer in non-smokers, who account for less than 10 percent of cases, appears to be due to a combination of genetic factors. Radon gas, asbestos, and air pollution may also contribute to lung cancer.
Asbestos is a mineral that was once used as a fire retardant in buildings and electrical wiring. The inhalation of asbestos fibers can cause a variety of lung diseases, including lung cancer. Tobacco smoking and exposure to asbestos greatly increase a person’s chance of developing lung cancer.
Lesson Summary
- The main functions of lungs are to obtain oxygen, and to release carbon dioxide. Oxygen is drawn in through the respiratory tract and is then delivered to the blood in a process called external respiration. The exchange of gases between the blood and the cells of the body is celled internal respiration.
- The structures of the respiratory systems include the nose and nasal cavity, the pharynx, the larynx, ( also called the voicebox), the trachea (also called the wind pipe), the right and left bronchi in the lungs, and the bronchioles that end in the alveoli.
- During inhalation, the diaphragm contracts, causing the volume of the chest cavity to increase. As a result, the air pressure within the lungs decreases. The pressure difference causes air to rush into the lungs. Relaxation of the diaphragm causes the lungs to recoil and air is pushed out of the lungs, which causes exhalation.
- Most of the carbon dioxide (about 70 percent) in the blood is in the form of bicarbonate (HCO3-). A small amount of carbon dioxide dissolves in the water in the plasma to form carbonic acid (H2CO3). When CO2 enters the blood from body cells, it combines with water in the plasma to produce carbonic acid (H2CO3), which is then turned into bicarbonate (HCO3-). The bicarbonate is then picked up by a red blood cell and turned back in to carbonic acid. A water molecule (H2O) is then taken away from the carbonic acid, and the remaining CO2 molecule is expelled from the red blood cells and into the lungs.
- Emphysema is a chronic lung disease caused by loss of elasticity of the lung tissue. The destruction of elastic structures that support the alveoli and the capillaries that feed the alveoli cause them to become hard and stiff. It is often caused by smoking. Asthma is also a chronic condition, which is often triggered by such things as exposure to an allergen, cold air, warm air, moist air, exercise, or emotional stress. The airways can constrict and become inflamed, and an excessive amount of mucus is produced. Airway narrowing causes symptoms such as wheezing, shortness of breath, chest tightness, and coughing.
Review Questions
- Identify the respiratory structures through which air flows.
- How is the diaphragm involved in breathing?
- Compare respiration and cellular respiration.
- Outline how most carbon dioxide is carried in the blood.
- Why is it important for a pregnant woman to know her Rhesus blood type, and the Rh blood type of the father of her baby?
- What is the difference between internal and external respiration?
- What happens during an asthma attack?
- Outline how emphysema affects the absorption of oxygen.
- Where does the exchange of oxygen occur in the lungs?
- What factors regulate breathing rate?
Further Reading / Supplemental Links
Vocabulary
-
alveoli
-
Multi-lobed sacs in which most of the gas exchange occurs.
-
asthma
-
A chronic illness in which the airways narrow and becomes inflamed.
-
bronchitis
-
An inflammation of the bronchi.
-
diaphragm
-
A muscle that is found below the lungs; contraction of the diaphragm causes the volume of the chest cavity to increase, and the air pressure within the lungs to decrease.
-
emphysema
-
A chronic lung disease caused by loss of elasticity of the lung tissue.
-
external respiration
-
Process in which oxygen is drawn in through the respiratory tract and is then delivered to the blood.
-
gas exchange
-
The diffusion of gases between the alveoli and the blood passing in the lung capillaries; also the diffusion of gases from capillaries into cells, and from cells into capillaries throughout the body (peripheral gas exchange).
-
internal respiration
-
The exchange of gases between the blood and the cells of the body.
-
larynx
-
Found just below the point at which the pharynx splits into the trachea and the esophagus; also called the voice box.
-
lung cancer
-
A disease where epithelial (internal lining) tissue in the lung grows out of control; leads to invasion of nearby tissue and growth of the tumor beyond the lungs.
-
lung volume (tidal volume)
-
The average breath capacity of a person.
-
obstructive
-
Conditions which lower the rate of the airflow into and out of the lungs, such as in asthma.
-
pharynx
-
A long tube that is shared with the digestive system; both food and air pass through the pharynx.
-
pneumonia
-
An illness in which the alveoli become inflamed and flooded with fluid.
-
respiration
-
The transport of oxygen from the outside air to the cells of the body, and the transport of carbon dioxide in the opposite direction.
-
respiratory acidosis
-
Condition in which arterial blood contains too much carbon dioxide, causing a drop in blood pH.
-
respiratory alkalosis
-
Condition which results from increased respiration (or hyperventilation) which causes a drop in the amount of carbon dioxide in the blood plasma; the drop in carbon dioxide concentration causes the blood pH to rise.
-
respiratory disease
-
The term for diseases of the lung, bronchial tubes, trachea and throat.
-
restrictive
-
Conditions that cause a reduction in the functional volume of the lungs, such as emphysema.
-
trachea
-
A long tube that leads down to the chest where it divides into the right and left bronchi in the lungs; also called the windpipe.
-
tuberculosis (TB)
-
A common and deadly infectious disease caused by a type of bacteria called Mycobacterium tuberculosis; most commonly attacks the lungs, but can also affect the central nervous system, the lymphatic system, the circulatory system, the genitourinary system, bones, joints and even the skin.
Points to Consider
- How might the amount of oxygen in the air affect your respiratory and circulatory systems?
- Can you identify any structures that are part of both the respiratory and digestive systems?