CHAPTER 8
Zygomatic Implants
Luis Vega1 and Patrick J. Louis2
1Department of Oral and Maxillofacial Surgery, Vanderbilt University Medical Center, Nashville, Tennessee, USA
2Department of Surgery, University of Alabama, Birmingham, Alabama, USA
Procedure: Zygomatic Implants
A zygomatic implant is a long implant (30–62.5 mm) that obtains its main anchorage from the zygoma bone in the presence or absence of maxillary alveolar bone. Zygomatic implants were designed by Per-Ingvar Brånemark to allow for implant-supported prosthesis placement where maxillary bony support for prosthetic rehabilitation is inadequate.
Indications
- Severe atrophy of the posterior maxilla with sufficient bone support for dental implants within the anterior maxilla
- Generalized severely atrophic maxilla
- Acquired maxillary bony defects (benign or malignant pathological ablation, infectious debridement, and avulsive trauma)
- Congenital maxillary bony defects (cleft lip and palate)
- Previous failed dental implant and/or bony reconstructions
Contraindications
- Medically compromised patient
- Acute sinusitis
- Adequate maxillary alveolar bone for conventional dental implants
- Severe trismus (relative contraindication)
- Previous history of head and neck radiation treatment (relative contraindication)
Anatomy
The zygoma bone has a mean anterior-posterior length that ranges from 14.1 to 25.4 mm and a mean mediolateral thickness that ranges from 7.6 to 9.5 mm. When the zygoma bone is measured along the potential implant axis, the bone-to-implant contact ranges from 14 to 16.5 mm, and approximately 36% of the implant is in contact with the zygoma bone. Although poor trabecular bone density has been described, the zygoma bone has a strong cortex, which provides the primary stability of the zygomatic implant. The placement of zygomatic implants was originally described using an intrasinus approach. The main disadvantage of this approach is the palatal emergence of the implant platforms. The palatal emergence occurs because during the process of maxillary resorption, the residual maxillary basal bone is in a more posterior position than the alveolar bone, whereas the position of the zygoma bone remains unchanged. The palatal emergence of the zygomatic implant requires the fabrication of a bulkier prosthesis that is difficult to restore and requires greater buccal cantilevers. Several modifications have been described within the literature that allow for more favorable implant placement, and these are described in this chapter.
Implant Anatomy
Numerous companies have designed and market zygomatic implants worldwide. The implant most commonly used in the United States is available in eight different lengths (30, 35, 40, 42.5, 45, 47.5, 50, and 52.5). All implants have a diameter of 5 mm in the coronal third and 4 mm in the apical two-thirds. The difference of diameters within the coronal and apical portions compensates for the potential widening of the maxillary implant bed that occurs during the determination of the proper trajectory of the drill to engage the zygoma bone. Finally, a 45° platform allows the inclined insertion of the zygomatic implant and its restoration.
Original Surgical Technique
- This procedure is typically performed with either general anesthesia or intravenous deep sedation. Local anesthesia is given intraorally within the maxillary vestibule and the posterior hard palate to block the superior alveolar, infraorbital, and greater palatine nerves and to control bleeding during dissection. When the procedure is performed under deep sedation, additional extraoral anesthesia is infiltrated around the zygoma prominence.
- A crestal incision is initiated from tuberosity to tuberosity bisecting the keratinized gingiva. Vertical releases are placed posteriorly along the maxillary buttress and anteriorly within the midline region.
-
Mucoperiosteal flap elevation is used to expose the alveolar crest, the lateral maxilla, the maxillary antral wall, the infraorbital nerve, the zygomaticomaxillary complex, and the lateral surface of the zygomatic bone cephalically to the incisura (the point between the lateral and medial surfaces of the frontal process of the zygomatic bone and the zygomatic arch; see Figures 8.2 and 8.9 in the Case Reports). Exposure of the infraorbital nerve is important as it serves as the anterior limit for implant placement in cases in which two ipsilateral zygomatic implants are placed. Exposure of the infraorbital rim is not necessary. The palatal mucosa is elevated due to the palatal emergence of the zygomatic implants.
- A zygoma retractor is placed at the incisura. The zygoma retractor is used to retract the soft tissues and to assist with implant angulation during implant placement. Care must be taken to properly insert the zygoma retractor at the incisura as it can be easily malpositioned along the infraorbital rim.
- A sinus window is created within the supero-lateral portion of the maxillary sinus. The window should allow for the elevation of the sinus mucosa, providing direct vision to the roof of the sinus and the base of the zygoma bone. No special effort is made to keep the sinus membrane intact. A larger, trapezoid-shaped window is used when two ipsilateral zygomatic implants are indicated (Figure 8.2, Case Report 8.1).
-
Determination of the implant trajectory is performed with the aid of a properly placed zygoma retractor and direct visualization of the base of the zygoma bone and sinus roof. For better orientation of the implant trajectory, the measuring device or the drill bit can be placed over the lateral maxillary wall prior to initiating the drilling protocol. The zygomatic implant platforms generally emerge within the areas of the second bicuspid or first molar (Figure 8.12, Case Report 8.2) and within the canine region if a second ipsilateral zygomatic implant is placed (Figure 8.4, Case Report 8.1). The implant osteotomies are planned as far posteriorly as possible and with the crestal emergence located as close to the alveolar crest as possible.
- A 105° zygomatic implant hand piece with a round bur is used to enter the residual maxillary bone, penetrating through the atrophic maxillary alveolus and maxillary sinus and marking the area of the sinus roof and the base of the zygoma bone that the implant will engage. A 2.9 mm twist drill is used to penetrate both cortices of the zygoma bone. The zygoma bone osteotomy is enlarged using a 3.5 mm final drill. This final drill provides the implant site with the final width of the zygomatic implant.
- The osteotomy depth is measured using a specially designed depth gauge. The device utilizes a small hook to engage the superior cortex, and depth measurements are made with the aid of 5 mm markings along the depth gauge.
- Implant placement can be performed manually or by using a hand piece. During implant placement, soft tissue frequently wraps around the body of the implant. Care must be taken to avoid embedding these tissues within the osteotomy site as this may impede osseointegration of the zygomatic implant. The tip of the implant is placed 2 mm beyond the superior cortex of the zygoma bone, and the platform is placed as close as possible to the maxillary bone. Care should be taken to position the 45° platform parallel to the occlusal plane.
- The implant mount is retrieved, and cover screws are placed.
- Additional traditional dental implants are placed within the anterior maxilla. Anterior traditional implants are desirable but not necessary with the placement of two ipsilateral zygomatic implants.
- Wounds are evaluated for hemostasis, copious irrigation is applied, and primary closure is performed with 3-0 Vicryl sutures.

Figure 8.1. Preoperative orthopantomogram demonstrating pneumatized maxillary sinuses and inadequate maxillary bone for the placement of traditional dental implants.

Figure 8.2. Quad-zygomas placed using the original technique via the intrasinus approach.
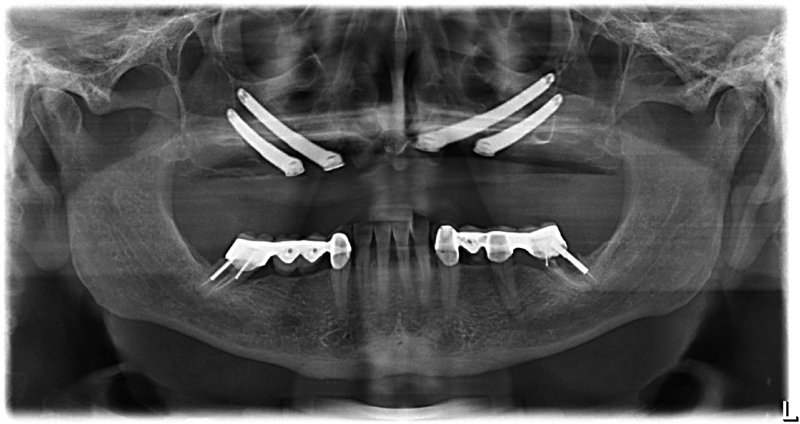
Figure 8.3. Postoperative orthopantomogram demonstrating ideal implant position.

Figure 8.4. Implants are uncovered and healing abutments are placed after 4 months of integration. Notice the palatal location of the implants.

Figure 8.5. Final prosthesis in place (courtesy of Dr William Gielincki, prosthodontist).

Figure 8.6. Preoperative orthopantomogram demonstrating adequate maxillary bone for the placement of six maxillary implants with sinus augmentation.

Figure 8.7. Computed tomography (CT) scan demonstrating a lack of bone height in the areas of the second premolar and first molar.

Figure 8.8. Computer-assisted virtual treatment planning showing the potential location of the zygomatic implants.

Figure 8.9. Placement of four anterior traditional dental implants and two zygomatic implants. No sinus window was used on the right zygoma implant as it was placed using the zygoma anatomy-guided approach (ZAGA) principal.
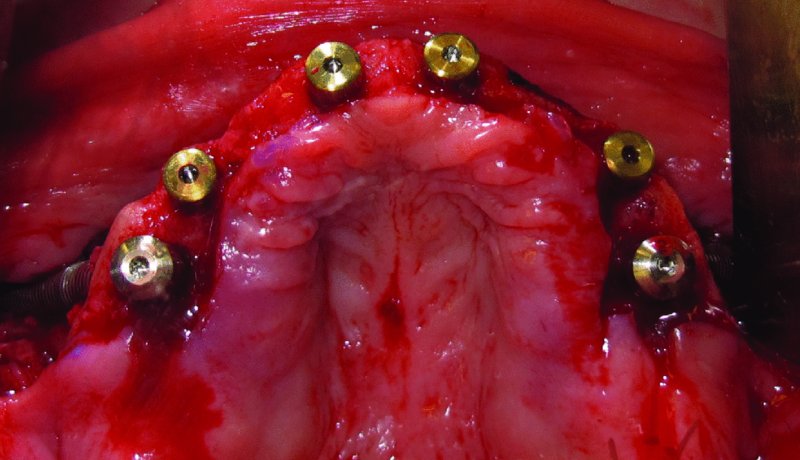
Figure 8.10. Occlusal view of implant placement. Note the crestal location of the implants.

Figure 8.11. Postoperative orthopantomogram demonstrating the ideal placement of implants.

Figure 8.12. Implants are uncovered and healing abutments are placed after 4 months of integration. Note the difference of the implant emergence compared to the original technique (Figure 8.4).

Figure 8.13. Final fixed-hybrid prosthesis in place (courtesy of Dr William Gielincki, prosthodontist).
Two-Zygomatic-Implant Placement
Special considerations when placing two ipsilateral zygomatic implants include:
- A larger sinus window is required to better identify the area in which both of the implants will be placed (Figure 8.2, Case Report 8.1).
- Implants are not placed parallel to each other. Instead, they are convergent in the apices. This allows for a better anterior-posterior spread to minimize cantilever forces. The most posterior implant should be placed as close as possible to the posterior lateral wall of the maxillary sinus, and the anterior implant should be placed as anterior as the infraorbital nerves permit.
Modifications of the Original Protocol
Several modifications of the original protocol have been described in the literature, including:
- Sinus slot technique: Simplifies the technique by eliminating the need for a sinus window, and improves the orientation of the zygomatic implant.
- Change implant design to a 55° platform: Uses a specially designed device to improve the orientation of the implant. The new implant platform decreases buccal cantilevers up to 20%.
- Immediate loading: Allows immediate function.
- Quad-zygomas: Placement of four zygomatic implants without traditional dental implants and immediate loading with a fixed prosthesis.
- Extrasinus implant placement: The remaining maxillary alveolar ridge is not engaged and the zygomatic implant completely bypasses the maxillary sinus, minimizing sinus complications and improving buccal cantilevers.
- Maxillary wall and sinus membrane preservation: The maxillary wall is preserved to protect the sinus membrane. Advantages of this technique include extra bone formation around the implant.
- Zygoma anatomy-guided approach (ZAGA): An anatomical– and prosthetically driven approach in which the preparation of the zygomatic implant osteotomy site is guided by the anatomy of the zygoma bone and the ideal site of the implant platform (Figure 8.9).
Postoperative management
Postoperative management is similar to that for patients who have undergone maxillary implant placement with a simultaneous sinus lift:
- Analgesics
- Antibiotics and chrohexidine mouth rinses
- Sinus precautions
- A soft diet
Complications
Intrasurgical Complications
- Invasion into orbit: Avoided by the proper placement of the zygoma retractor into the incisura.
- Invasion into the temporal fossa: Occurs when the trajectory of the implant is located too posterior at the base of the zygoma or when inadequate zygoma bone is present, especially if two implants are planned. This is corrected with repositioning of the implant bed into a more anterior location.
Postoperative Complications
- Sinusitis: Three different etiopathogenic mechanisms have been proposed: (i) a zygoma implant represents invasive surgery for the sinus, (ii) a zygoma implant is an intrasinusal foreign body, and (iii) a zygoma implant could create a oroantral communication. Sinusitis is typically treated via medical therapy with antibiotics and nasal decongestants. Failed medical management or recurrent events are better treated surgically via functional endoscopic sinus surgery (FESS).
- Oroantral communication.
- Peri-implantitis.
- Loss of implant.
Key Points
- Zygomatic implant reconstruction of the severely atrophic maxilla for acquired or congenital maxillary defects is a safe, predictable, and cost-effective treatment modality. Advantages of zygomatic implant reconstruction versus traditional implant reconstruction include shorter treatment time frames, avoidance of the need for bone grafting and its associated morbidity, fewer total implants required for a fixed prosthesis, and the fact that zygomatic implants allow the potential for immediate functioning. Disadvantages of zygomatic implants include the need for general or deep sedation, plus the facts that implant failures are more difficult to treat and the procedure is very technique sensitive.
- The single most important factor for treatment success is a team approach between the surgeon and the restorative dentist. As with any pre-prosthetic surgery, the treatment plan should be prosthetically driven. When possible, the placement of one or two extra traditional dental implants will improve the distribution of forces and increase the support of the final prosthesis.
- In cases with limited mouth opening, a contra-angle hand piece allows for improved access for osteotomy preparation and implant placement.
References
- Aparicio, C., 2011. A proposed classification for zygomatic implant patient based on the zygoma anatomy guided approach (ZAGA): a cross-sectional survey. European Journal of Oral Implantology, 4(3), 269–75.
- Balshi, T.J., Wolfinger, G.J., Shuscavage, N.J. and Balshi, S.F., 2012. Zygomatic bone-to-implant contact in 77 patients with partially or completely edentulous maxillas. Journal of Oral and Maxillofacial Surgery, 70, 2065–9.
- Brånemark, P-I., Gröndahl, K., Ohrnell, L-O., Nilsson, P., Petruson, B., Svensson, B., Engstrand, P. and Nannmark, U., 2004. Zygoma fixture in the management of advanced atrophy of the maxilla: technique and long-term results. Scandinavian Journal of Plastic and Reconstructive Surgery and Hand Surgery, 38, 70–85.
- Davó, R., Malevez, C., López-Orellana, C., Pastor-Beviá, F. and Rojas, J., 2008. Sinus reactions to immediately loaded zygoma implants: a clinical and radiological study. European Journal of Oral Implantology, 1(1), 53–60.
- Vega, L., Gielincki, W. and Fernandes, R., 2013. Zygoma implant reconstruction of acquired and maxillary bony defects. Oral and Maxillofacial Surgery Clinics of North America, 25, 223–39.