CHAPTER 14
Le Fort Fractures
Shahid R. Aziz
Department of Oral and Maxillofacial Surgery, Rutgers University School of Dental Medicine, Camden, New Jersey, USA
Reduction of displaced fractures and restoration of occlusion and facial aesthetics.
Indications for Reduction of Le Fort Fractures
- Malocclusion
- Mobility at the fracture site: Le Fort I (mobility of the maxilla), Le Fort II (mobility of the nasal-maxillary complex), and Le Fort III (craniofacial disjunction—mobility of the facial skeleton from the lateral orbital rims to the maxilla)
- Significant aesthetic deformity
Contraindications
- Nondisplaced fractures with no malocclusion
- Contraindications to general anesthesia (medically unstable for treatment)
Anatomy
- Le Fort I fracture: Transverse fracture of the maxilla separating the maxillary alveolus from the pterygoid plates, lateral antral wall, lateral nasal wall, and lower third of the septum
- Le Fort II fracture: Pyramidal fracture extending from the pterygoid plates superiorly across the lateral antral wall, extending through the infraorbital foramen and medial orbital floor, and posterior to the lacrimal bone, through the nasal bones, and terminating at the nasofrontal suture
- Le Fort III fracture: “Craniofacial disjunction”—fracture extending from the pterygoid plates through the zygomaticotemporal and zygomaticofrontal sutures through the lateral orbital wall and posterior orbital wall, and posterior to the lacrimal bone, through the nasal bones, and terminating at the nasofrontal suture
See Figure 14.1 for a comparison of Le Fort fracture patterns.
Le Fort Fracture Signs and Symptoms
- Le Fort I fracture: Maxillary mobility, malocclusion, maxillary buccal vestibule and palatal ecchymosis, maxillary crepitus and upper lip and midface edema
- Le Fort II fracture: Nasal-maxillary complex mobility, malocclusion, maxillary buccal vestibule and palatal ecchymosis, V2 paresthesia or anesthesia, loss of anterior-posterior dimension of the midface, nasal asymmetry, epistaxis, cerebrospinal fluid (CSF) rhinorrhea, epiphora, subconjunctival hemorrhage, diplopia, enophthalmus, midface and periorbital edema, midface crepitus and ecchymosis
- Le Fort III fracture: Complete mobility of the anterior facial skeleton inferior to the zygomaticofrontal suture (craniofacial disjunction), V2 paresthesia or anesthesia, nasal asymmetry, epistaxis, CSF rhinorrhea, epiphora, subconjunctival hemorrhage, traumatic telecanthus, enophthalmus, diplopia, dystopia, increase in the vertical dimension of the face, tenderness and palpation of fractures at the lateral orbital rim, midface and periorbital edema and midface and periorbital crepitus and ecchymosis
Le Fort Reduction Technique
- Preoperative antibiotics are given to cover sinus flora and wound contamination.
- The airway is secured via nasal intubation, tracheostomy, or submental intubation.
- The patient is prepped and draped to include both the oral cavity and the maxillofacial skeleton.
- Local anesthesia containing a vasoconstrictor is injected into sites of incision placement.
- Maxillary and mandibular arch bars are placed, and the pre-traumatic occlusion is reestablished. The placement of maxillomandibular fixation (MMF) may be difficult, depending on the displacement of the fractures. For grossly displaced Le Fort fractures, Rowe disimpaction forceps may be used to aid in the mobilization and reduction of the maxilla. When placing the patient into MMF, the fractured maxilla is neutrally set to mandible to ensure proper seating of the condyles.
- Fractures are typically reduced and fixated with a bottom-to-top rationale. After the establishment of MMF, the mandible is internally fixated prior to fixation of the Le Fort fractures.
- After the occlusion has been reestablished (and, if necessary, the mandible has been fixated), all facial fractures are exposed. A high maxillary buccal vestibular incision is used in all three types of Le Fort fractures (Figure 14.3). Le Fort II and III fractures are approached through a variety of incisions to include subciliary, transconjunctival, superior blepharoplasty, lateral brow, and coronal. Care should be taken to identify and preserve the infraorbital neurovascular bundles.
- Once all fractures are exposed, manual reduction is employed, and the fractures are stabilized with rigid internal fixation. Fractures are ideally plated along the natural horizontal and vertical buttresses of the face. Depending on the surgeon's preference and the comminution of the fractures, MMF may be utilized for 4–6 weeks without internal fixation. However, from a functional and nutritional standpoint, rigid internal fixation of Le Fort fractures is preferred.
- Large anterior maxillary wall defects may be repaired with the use of titanium mesh.
- Once rigid fixation is completed, MMF is released and the occlusion is verified to be stable and reproducible. Light to medium guiding elastics are placed.
- All incisions are copiously irrigated and closed. Intraoral incisions are closed with 3-0 chromic sutures. Skin incisions are closed in a layered fashion. Transconjunctival incisions are either loosely closed or left open.
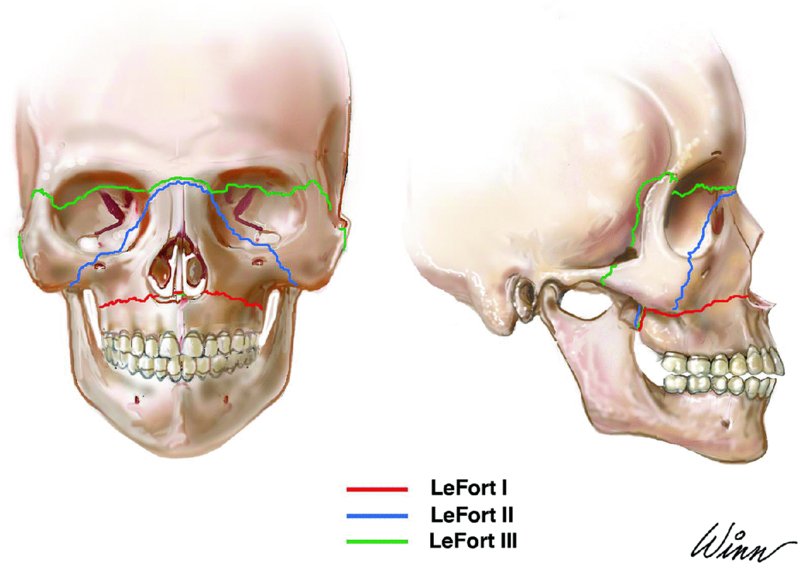
Figure 14.1. Le Fort fracture patterns.
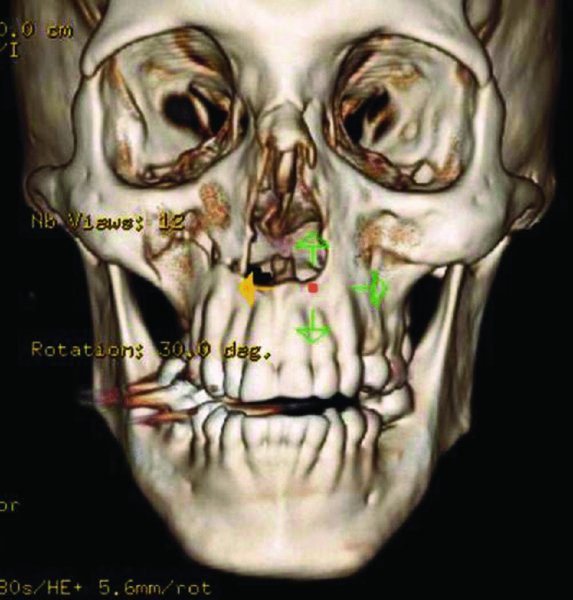
Figure 14.2. 3D reconstruction demonstrating a displaced Le Fort I fracture.
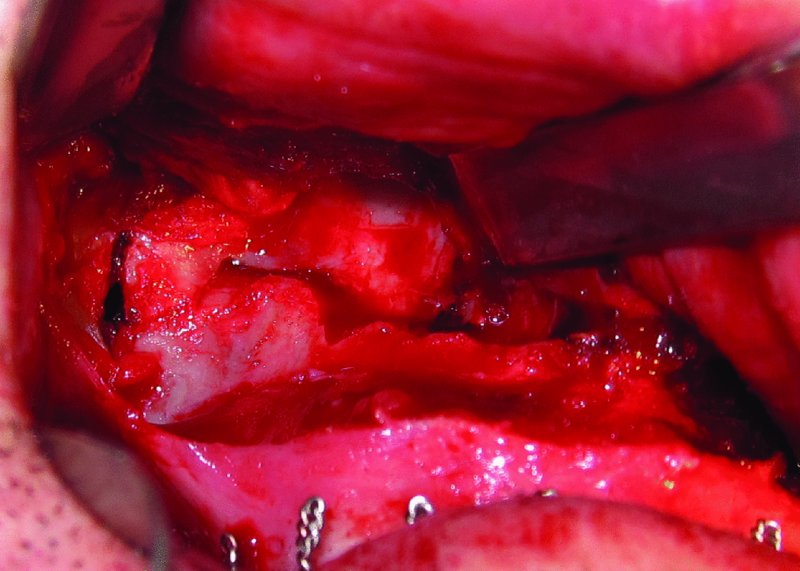
Figure 14.3. Exposure of Le Fort I fracture via maxillary vestibular incision.
Postoperative Management
- Patients are observed for at least 24 hours postoperatively to ensure airway stability, wound hemostasis, and pain control.
- Intravenous steroids are tapered and discontinued.
- Patients are placed on intravenous antibiotics during hospital admission. For patients with an abbreviated hospital course receiving less than 72 hours of intravenous antibiotics, 5 days of oral antibiotics are prescribed.
- Analgesics are prescribed in either a pill or liquid form depending on whether MMF is employed.
- Patients are placed on sinus precautions. Sneezing and nose blowing are minimized. Ocean nasal spray and decongestants are recommended.
- Patients in MMF via light elastics are maintained on a soft mechanical diet for 3–4 weeks. Arch bars are removed at 4–6 weeks post surgery.
Complications
- V2 paresthesia or anesthesia: Minimized with meticulous dissection of the infraorbital nerve.
- Enophthalmus: From inadequately reduced orbital fractures.
- Deviated septum or obstructed nasal breathing: From inadequately reduced fractures of the bony and cartilaginous nasal septum.
- Epiphora: Results from damage of the lacrimal drainage system.
- Infection: Minimized by obtaining sterile operating conditions and pre– and postoperative antibiotic coverage.
- Hematoma formation: Minimized with wound hemostasis prior to wound closure. Large hematomas require surgical exploration and drain placement.
- Sinusitis: Minimized with the use of appropriate antibiotic coverage and nasal decongestants.
- Malunion: Typically occurs due to hardware failure or early, excessive patient functioning.
- Malocclusion: Occurs in up to 20% of cases. Malocclusion may require future orthognathic surgery to correct. Patients typically present with a mild class 3 anterior open bite. Malocclusion is minimized with the use of adequate rigid internal fixation, passive articulation of the maxilla to mandible to prevent condyle malpositioning, the use of Rowe disimpaction forceps to completely mobilize the maxilla, the removal of bony interferences prior to the placement of MMF, and occlusal verification at the end of the procedure.
- Exposure of hardware: Typically occurs from inadequate tissue closure and the inability to obtain a tension-free closure.
Key Points
- Surgery is often delayed 4–7 days in order to allow for stabilization of the patient (if necessary) and resolution of facial edema.
- Because MMF will be utilized intraoperatively, oral intubation is contraindicated. Nasal intubation is performed for patients with fractures that do not involve nasal bone comminution, CSF rhinorrhea, or cribriform plate fractures. Submental intubation can be utilized for patients requiring short-term intubation when nasal intubation is contraindicated. Tracheostomy is utilized when nasal intubation is contraindicated, when prolonged ventilation support is required, and in cases of upper airway obstruction (i.e. edema or hematoma formation).
- The initial step in Le Fort fracture reduction is the restoration of the pre-traumatic occlusion. The occlusion will reestablish the horizontal and vertical dimensions of the face and reduce associated palatal fractures.
- After establishing MMF, mandible fractures (if present) are repaired prior to the reduction of maxillary and Le Fort fractures.
- Rigid fixation plates should be strong enough to resist occlusal forces and fracture displacement.
- Intravenous steroids are used (unless contraindicated) prior to surgery, intraoperatively, and postoperatively to reduce facial edema. Patients requiring long-term steroids require a taper of the medication.
- Edentulous patients and those with severe maxillary sinus pneumatization may require stabilization with gunning splints or preexisting dentures and skeletal fixation.
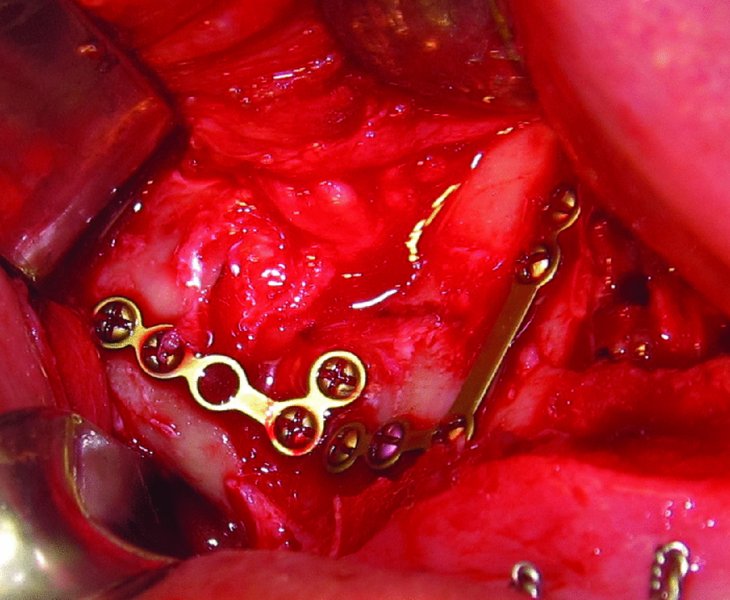
Figure 14.4. Le Fort I fracture reduced with 2.0 plates placed at the pyriform aperture and zygomaticomaxillary buttress.
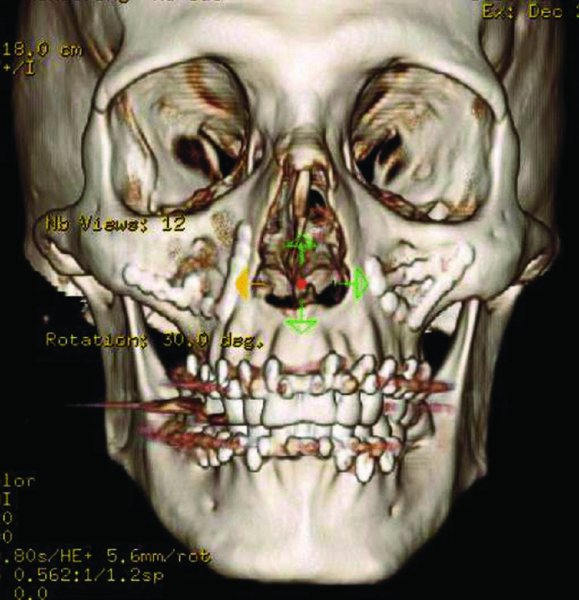
Figure 14.5. Postoperative 3D reconstruction demonstrating maxillomandibular fixation (MMF) and reduction of Le Fort I fractures.
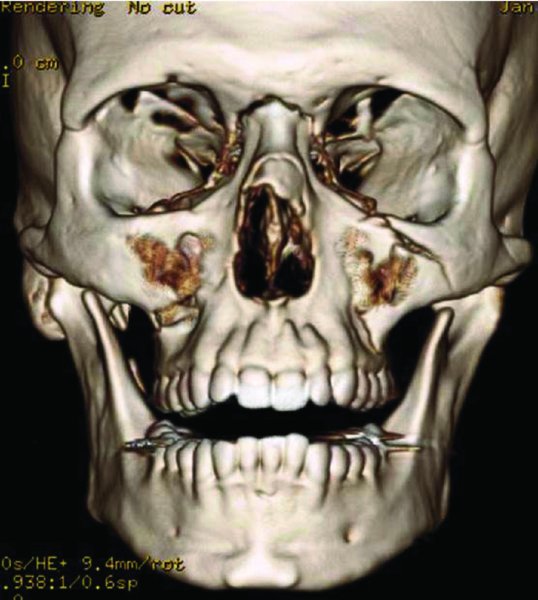
Figure 14.6. 3D reconstruction demonstrating a right-sided Le Fort I fracture and a left-sided Le Fort II fracture.
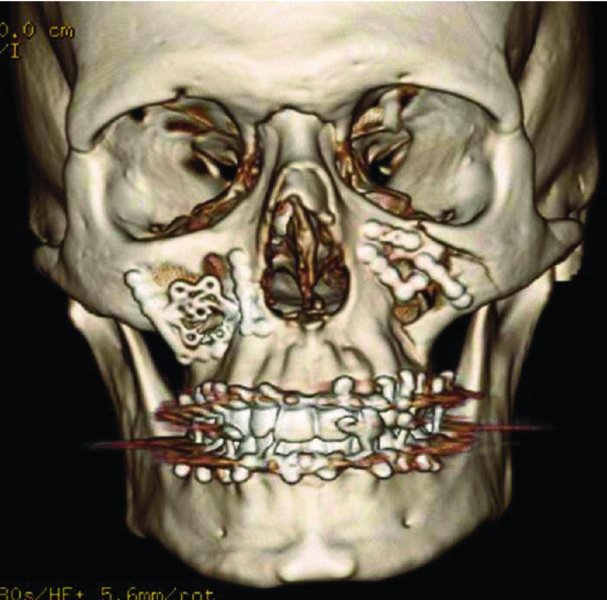
Figure 14.7. Postoperative 3D reconstruction demonstrating maxillomandibular fixation and reduction of the right Le Fort I fracture and the left Le Fort II fracture.
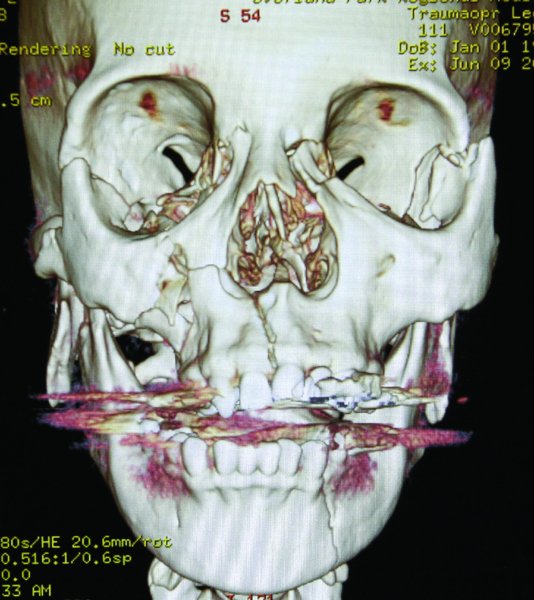
Figure 14.8. 3D reconstruction demonstrating a Le Fort III fracture, right comminuted zygomatic arch fractures, midline palatal fracture, bilateral condyle fractures, and a left parasymphysis fracture of the mandible.
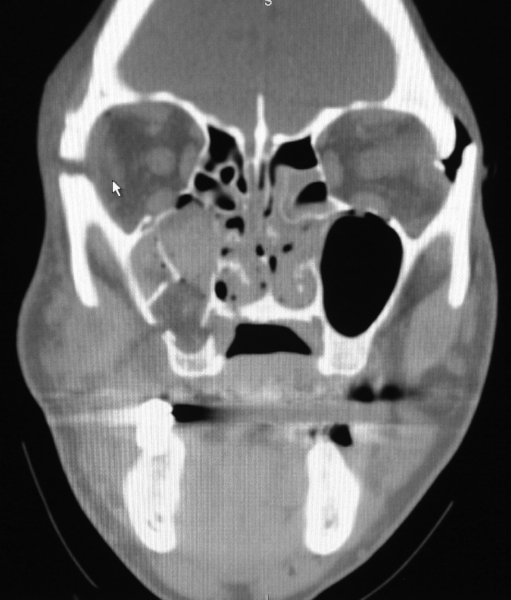
Figure 14.9. Coronal computed tomography (CT) image demonstrating a displaced Le Fort III fracture. Note displacement of the bilateral zygomaticofrontal sutures.
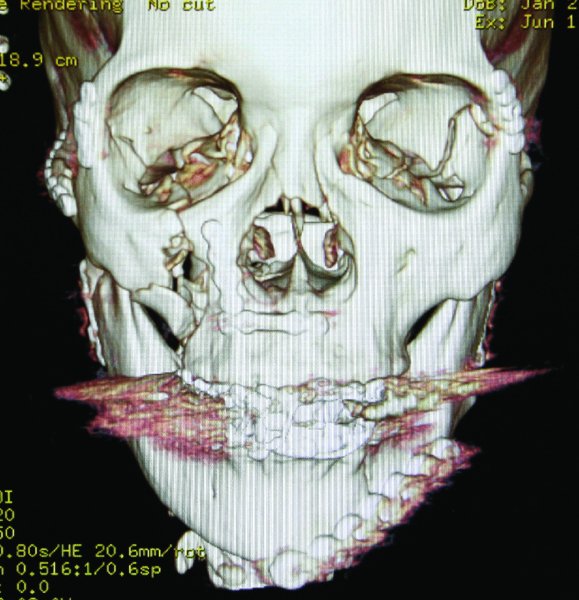
Figure 14.10. Postoperative 3D reconstruction demonstrating maxillomandibular fixation, reduction of Le Fort III, and associated facial fractures.
References
- Fraioli, R.E., Branstetter, B.F. 4th and Deleyiannis, F.W., 2008. Facial fractures: beyond Le Fort. Otolaryngologic Clinics of North America, 41(1), 51–76.
- Mehta, N., Butala, P. and Bernstein, M.P., 2012. The imaging of maxillofacial trauma and its pertinence to surgical intervention. Radiologic Clinics of North America, 50(1), 43–57.
- Meslemani, D. and Kellman, R.M., 2012. Recent advances in fixation of the craniomaxillofacial skeleton. Current Opinion in Otolaryngology and Head and Neck Surgery, 20(4), 304–9.
- Yu, J., Dinsmore, R., Mar, P. and Bhatt, K., 2011. Pediatric maxillary fractures. Journal of Craniofacial Surgery, 22(4), 1247–50.