CHAPTER 27
Cleft Lip Repair
Bart Nierzwicki1 and Thaer Daifallah2
1Private Practice, Millennium Surgical, Chicago, Illinois, USA
2Department of Oral and Maxillofacial Surgery, University of Missouri–Kansas City, Kansas City, Missouri, USA
A technique of repairing congenital lip defects utilizing a three-layer closure of skin, muscle, and mucosa to achieve nasal and labial symmetry and normal lip function with minimal visible scarring.
Indication
- Unilateral or bilateral, complete or incomplete cleft lip deformity
Contraindications
- No absolute contraindications
- Adequate patient's age, weight, and hemoglobin (“rule of 10s”)
Anatomy
- Orbicularis oris muscle
- Columella
- Philtral ridges and tubercle (procheilon)
- White skin roll (epidermis–vermilion junction line)
- Red line (vermilion–mucosa junction line)
- Alar cartilage
- Lower lateral cartilage
- Nasal septum
- Anterior nasal spine
Modified Millard's Rotation-Advancement Flap Technique
- The patient is placed supine on the operating table and orally intubated with a RAE endotracheal tube.
- The oral cavity and face are prepped with povidone–iodine and draped.
- A sterile marking pen or methylene blue on a 30G needle tip are used to mark the rotational flap (M flap), advancement flap (L flap), columella flap (C flap), and turbinate flap. Points of the Cupid's bow are marked on the epidermis–vermilion junction line (the white skin roll), and the vermilion–mucosa junction line (the red line) is also marked (Figure 27.1; see also Figure 27.3 in Case Report 27.1). Important landmarks in marking order:
- Landmark 2 is the top of the Cupid's bow on the noncleft side.
- Landmark 3 is the end of the white roll on the noncleft side.
- Landmark 1 represents the middle of the Cupid's bow.
- Landmark 3’ is the end of the white roll on the cleft side.
- Landmark 4 is the noncleft-side labial commissure.
- Landmark 5 is the cleft-side labial commissure.
- Landmark 6 is the center of the columella.
- Landmark 7 is the base of the columella on the noncleft side.
- Landmark 8 is the base of the columella on the cleft side.
- Ideally, the distance from 4 to 2 should be equal to that from 5 to 3’; however, it is not always possible.
- The distance from 2 to 7 must equal that from 3 (and 3’) to 8.
- Local anesthetic containing a vasoconstrictor is infiltrated into above flaps (weight-based dosage).
- The nasal cavities are packed with oxymetazoline-soaked cottonoids.
- Incisions are made with a #15c scalpel blade around the rotation flap and C flap, extending across the white roll into the vermilion.
- Elevation of mucosal flaps in the submucosal plane; all abnormal orbicularis oris attachments are removed from the premaxilla.
- The M flap is elevated in the submucosal plane, and the C flap in the subdermal plane.
- The orbicularis oris muscle is elevated from the overlying skin and mucosa within the rotation flap and completely detached from the nasal floor and anterior nasal spine for downward rotation.
- An incision from the C flap is extended into the caudal nasal septal base through the mucosa and partially through the mucoperichondrium with sharp dissection to perform septoplasty.
- A ligamentous attachment anterior to the caudal septum is detached, and submucoperichondrial dissection allows separation of the cartilaginous septum from the mucoperichondrium.
- Separation of the septum from the vomer and reduction into the midline position.
- The M flap is rotated to deepen the vestibule and sutured with 5-0 Monocryl.
- L flap elevation and orbicularis oris dissection.
- Attachment of the L flap to the inferior edge of the caudal septal mucoperichondrial incision with 5-0 Monocryl to create the nasal floor on the cleft side.
- Elevation of the inferior turbinate flap from the lateral nasal wall by incising in all areas except attachment to the anterior lateral nasal wall. This flap is then rotated from lateral to medial, and it is repaired to the superior edge of the caudal septal mucoperichondrial incision with 5-0 Monocryl to create the top layer of the nasal floor on the cleft side.
- Reconstruction of orbicularis oris continuity with 5-0 polydiaxanone horizontal mattress sutures.
- Insertion of the C flap into the nasal floor.
-
Suturing of mucosal and skin incisions (Figure 27.5, Case Report 27.1), and the placement of Dermabond along the skin incision edges.
- Insertion of lubricated nasal stents.
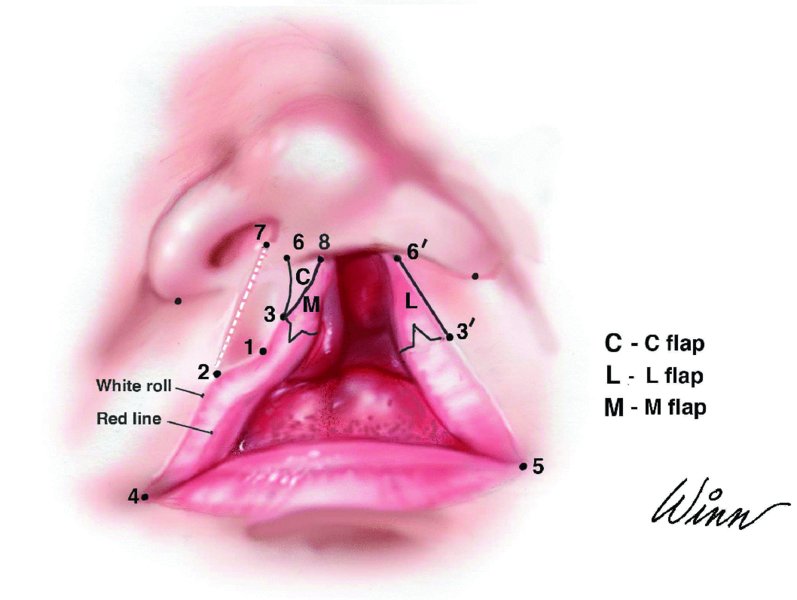
Figure 27.1. A pen and a 30G needle tip mark the rotational flap (M flap), advancement flap (L flap), columella flap (C flap), and turbinate flap of a cleft lip.

Figure 27.2. Complete left cleft lip at 4 months of age.

Figure 27.3. Preoperative markings. Note the interrupted line depicting the distance from the noncleft-side columellar base to the noncleft-side Cupid's bow peak. Landmarks 1, 2, 3, and 3’ are tattooed with methylene blue on a 30G needle tip.
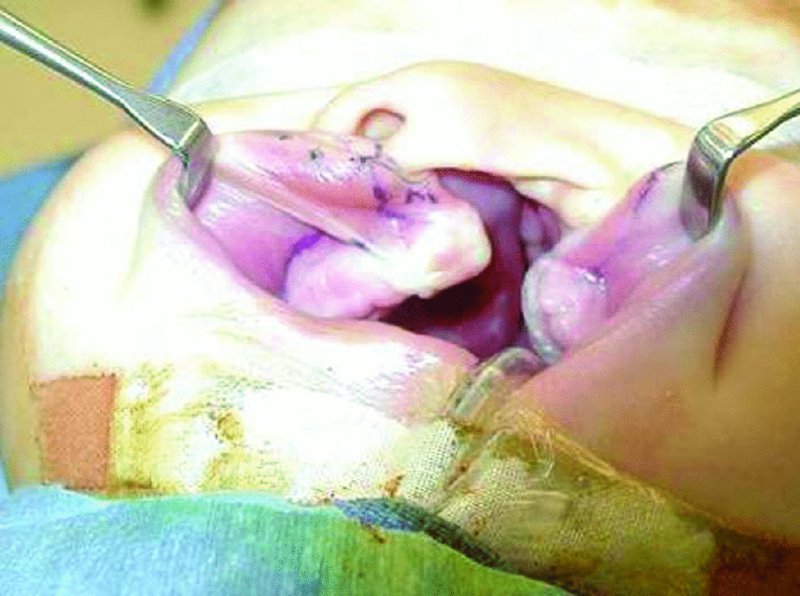
Figure 27.4. Mucosal flaps: the rotational M (medial; noncleft side) flap and advancement L flap (lateral; cleft side).

Figure 27.5. Immediate post-cheiloplasty: note alignment of the vermilion border, white skin roll, and red lines.
Postoperative Management
- Local wound care and topical antibiotic ointment to prevent crusting or drying.
- Arm restrains for 7–10 days to prevent accidental trauma to the lip; restraints can be removed when the infant is under supervision.
- Feeding utilizing a Brecht feeder (syringe with a small tube) for the first 2 days. Use of pacifiers are discouraged for a minimum of 2 days.
- Upper lip massaging with silicone creams (Scarzone) beginning 3 weeks postop.
- Nasal stents are removed after 1 week and then used for 12 hours in each 24-hour period for 3–6 months.
Complications
- Wound infection: Rare but can have devastating outcomes, resulting in contraction of tissue and scarring that makes revision more challenging.
- Excess scaring: Due to infection or closure under tension. Hypertrophic scars are managed by massaging the area and using topical steroids. Possible surgical revision or laser treatment after age 5.
- Wound dehiscence: Rare, but may result from trauma to the flap postoperatively and/or failure to achieve layered closure. More commonly seen with inexperienced surgeons.
- Poor cosmetic outcomes: Related to surgical planning, improper techniques, and the level of the surgeon's skill and experience.
Key Points
- Rule of 10s to qualify infant for early surgical repair. The infant should be at least 10 weeks old and 10 lbs. in weight, with a hemoglobin of at least 10 g/100 ml.
- Goals of repair: Continuity of the orbicularis oris muscle, and symmetry of the nasal ala, nostrils, philtral ridges, and Cupid's bow. Also, adequate nasal tip projection and fullness to the philtral tubercle.
- The surgeon should ensure that the distance between the nasal alar base and the vermillion white roll is equal between cleft and noncleft sides.
- The release of the periosteum covering the piriform aperture on the cleft side will allow elevation and superior placement of the nasal alar base on the cleft side for appropriate symmetry.

Figure 27.6. One year postoperatively.
References
- Millard, D.R., 1976. Cleft craft. The evolution of its surgery. I: the unilateral deformity. Boston: Little, Brown. P. 251.
- Millard, D.R., 1960. Complete unilateral clefts of the lip. Plastic and Reconstructive Surgery, 25, 595–605.
- Millard, D.R., 1964. Refinements in rotation advancement cleft lip technique. Plastic and Reconstructive Surgery, 33, 26–38.
- Nordoff, M.S., 1984. Reconstruction of vermillion in unilateral and bilateral cleft lips. Plastic and Reconstructive Surgery, 73(1), 52–61.
- Stal, S., Brown, R.H., Higuera, S., Hollier, L.H., Jr., Byrd, H.S., Cutting, C.B. and Mulliken, J.B., 2009. Fifty years of the Millard rotation-advancement: looking back and moving forward. Plastic and Reconstructive Surgery, 123, 1364–77.