CHAPTER 30
Arthrocentesis of the Temporomandibular Joint
Robert M. Laughlin and James MacDowell
Department of Oral and Maxillofacial Surgery, Naval Medical Center San Diego, San Diego, California, USA
Procedure: Arthrocentesis of the Temporomandibular Joint
A highly successful minimally invasive procedure for the initial treatment of temporomandibular joint (TMJ) pain and dysfunction refractory to medical management.
Indications
- Medically refractory pain to TMJ muscles, headache, or earache impacting the patient's quality of life
- Altered jaw mechanics such as closed lock, joint hypomobility, and limited range of motion in maximal incisal opening, excursion, and/or protrusion
- Alterations of occlusion
- Joint noises associated with pain
Contraindications
- Presence of concomitant facial pain of separate etiologies
- Chronic pain disorders
- Presence of deformity or pathology of the TMJ
- Presence of local or systemic conditions that may interfere with normal healing process and subsequent tissue homeostasis
Anatomy
- Temporomandibular Joint (TMJ): A compound synovial ginglymoarthrodial joint with rotation of the condyle within the inferior joint space. The TMJ has an overlying highly vascular and innervated fibroelastic capsule, which is thickened on the lateral aspect to form the temporomandibular ligament. The vascular supply to the TMJ is supplied with branches from the superficial temporal and maxillary arteries with an extensive venous plexus within the bilaminar zone.
- Articular eminence: A prominent convexity lined with dense, compact connective tissue that is subject to loading during function.
- Glenoid fossa: A nonloading, concave structure lined with a thin layer of fibrocartilage separated from the middle cranial fossa by 1–2 mm thickness of temporal bone.
- Articular disc: A biconcave avascular fibrocartilage disc that divides the joint space into a 1.2 mL upper compartment and a 0.9 mL lower compartment and allows complex movements of rotation and translation.
- Auriculotemporal nerve: Provides sensation to the posterior and lateral capsule.
- Masseteric nerve: Provides sensation to the anteriomedial aspect of the joint.
- Deep temporal nerve: Provides anterolateral sensation to the joint.
- Holmlund–Hellsing line (H-H line): A line extending from the lateral canthus of the eye to a point bisecting the tragus of the ear (Figure 30.1 [all figures cited appear in Case Report 30.1]). The 10-2 point (10 mm anterior and 2 mm inferior to the mid-tragus along the line) correlates with the posterior recess/glenoid fossa. The 20-10 point (20 mm anterior to the mid-tragus point along the line and 10 mm below the line) correlates with the prominence of the articular eminence.
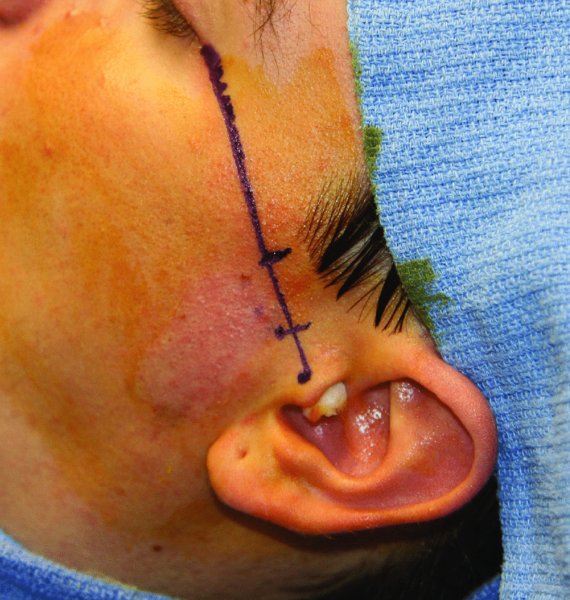
Figure 30.1. The H-H line and the 10-2 and 20-10 points are marked.
Technique
- Pre-procedural documentation of maximal incisal opening (MIO), excursive movements, and subjective details of pain and dysfunction are measured and recorded.
- Bacitracin-soaked cotton is placed within the auditory canal to obtund the canal from blood and fluid accumulation.
- Landmarks are identified and marked with a skin marker referencing the Holmlund–Hellsing line (H-H line), the 10-2 point, and the 20-10 point (Figure 30.1).
- Surgical skin prep of the area is performed, with the hair taped superior to the auricle with sterile drape.
- An auriculotemporal nerve block and local infiltration with a solution of 1% lidocaine with 1:100,000 epinephrine is performed at the marked 10-2 and 20-10 points (Figure 30.2).
- An 18-gauge needle attached to a 10 mL syringe containing normal saline is inserted in an anterior-superior direction at the 10-2 point into the superior joint space (Figure 30.3). The superior joint space is insufflated with enough normal saline to obtain bouncing-back pressure with the syringe and movement of the jaw.
- The first syringe is removed, leaving the 18-gauge needle in place to observe for a small amount of fluid backflow.
- A second 18-gauge needle is placed slightly anterior to the first 18-gauge needle along the same angulation to serve as an exit point for the saline lavage (Figure 30.4).
- Approximately 100 mL of normal saline lavage should be passed through the superior joint space.
- At the end of the procedure, 1 mL of betamethasone is injected with 1 mL of 0.5% Marcaine with epinephrine into the superior joint space.
- The inflow and outflow ports are removed, and pressure is applied over the joint for 5 minutes.

Figure 30.2. Local infiltration and an auriculotemporal nerve block is performed.

Figure 30.3. An 18-gauge needle attached to a 10 mL syringe is inserted in an anterior-superior direction at the 10-2 point to enter the superior joint space. Entry into the superior joint space is confirmed with superior joint space insufflation and lower jaw movement.

Figure 30.4. A second 18-gauge needle is placed slightly anterior to the first 18-gauge needle and along the same angulation to serve as an exit point for the saline lavage.
Postoperative Management
- Ice is applied over the joint for 15–20 minutes of every hour for the first 24 hours.
- Compression dressings are utilized for the first 24 hours for hemostasis and to minimize swelling.
- Patients are asked to sleep with 30° head-of-bed elevation for the first 48 hours.
- A soft mechanical diet is required for the first 72 hours postoperatively.
- Scheduled nonsteroidal anti-inflammatory drugs and as-needed (pro re nata, or PRN) narcotic analgesics are prescribed.
- Jaw-opening and range-of-motion exercises are begun the day of the procedure and are encouraged several times per day for the first week.
Complications
- Iatrogenic scuffing of fibrocartilage covering articular eminence and fossa
- Injury to temporal vessels or maxillary artery, and/or postsurgical bleeding
- Neuronal damage (CN V, VII, and VII)
- Damage to articular disk and/or retrodiskal tissue upon entering the joint space
- Intra-articular fibrosis and adhesions formed after hemorrhage
- Ear injury from middle-ear penetration
- Infection
References
- Carlson, E., 2012. Parameters of care: clinical practice guidelines for oral and maxillofacial surgery—temporomandibular joint surgery (AAOMS ParCare 2012). Journal of Oral and Maxillofacial Surgery, 70 (Suppl. 3), e204–31.
- Haddle, K., 2001. Arthrocentesis of the TMJ: oral and maxillofacial surgery knowledge update. TMJ, 3, 40–50.
- Holmlund, A., Hellsing, G. and Wredmark, T., 1986. Arthroscopy of the termporomandibular joint a clinical study. International Journal of Oral and Maxillofacial Surgery, 15, 715–21.
- Rohen, J.W., Lütjen-Drecoll, E. and Yokochi, C., 2011. Color atlas of anatomy: a photographic study of the human body. 7th ed. Philadelphia: Lippincott Williams and Wilkins.