CHAPTER 31
Arthroscopic Arthroplasty of the Temporomandibular Joint
Joseph P. McCain1 and Reem Hamdy Hossameldin2
1Private Practice; Baptist Health Systems; and Oral and Maxillofacial Surgery, Herbert Wertheim College of Medicine, Florida International University Miami, Florida, USA; and Nova Southeastern School of Dental Medicine, Fort Lauderdale, Florida, USA
2Department of Oral and Maxillofacial Surgery, Faculty of Dental Medicine, Cairo University, Cairo, Egypt; and General Surgery Department, Herbert Wertheim College of Medicine, Florida International University, Miami, Florida, USA
A minimally invasive procedure used to diagnose and/or treat numerous joint pathologies.
Indications
- Disabling joint conditions refractory to medical management and primary arthroscopy alone that require internal structural modifications of the temporomandibular joint (TMJ)
- Wilkes stage II, stage III, and/or early stage IV of arthroscopic discopexy
Contraindications
- Skin infection
- Possible tumor seeding
- Medical and other circumstances unique to patients
Anatomy
- Temporomandibular joint (TMJ): The TMJ is a diarthrodial joint separated into inferior and superior compartments by the articular disc. The inferior joint space contains approximately 0.9 mL of synovial fluid, whereas the superior joint space contains approximately 1.2 mL of synovial fluid. The inferior joint space is responsible for hinge opening or rotation (ginglymoid), and the superior joint space is responsible for gliding or translation motion (arthrodial), which is the second phase of opening. When the hinge opens, it permits the mandible to open approximately 2 to 3 cm as measured from the edges of the maxillary and mandibular incisor teeth. Translation allows increased opening to a maximum of 4 to 6 cm. The average vertical opening is approximately 45 mm. Anterior translation of the condyle terminates at the anterior peak of the articular eminence.
- Articular disk: The articular disk is composed of dense, collagenous connective tissue. The articular disk is biconcave in shape with a length of approximately 22 mm and a width of approximately 16 mm. The disk is firmly attached to the lateral and medial poles of the condyle. The anterior and anterior medial attachments are to the lateral head of the pterygoid muscle. The anterior lateral attachment is to the capsule only. The posterior attachment blends into the retrodiskal tissue, which attaches to the posterior wall of the glenoid fossa. The posterior retrodiskal tissue attachment consists of synovial cells, collagen fibers, nerves, blood vessels, and elastic fibers.
- Lateral pterygoid muscle: The most influential muscle involved in TMJ function is the lateral pterygoid muscle due to its attachment to both the disk and the condyle. The lateral pterygoid muscle has an inferior and superior belly. The origin of the inferior belly is the inferior two-thirds of the outer surface of the lateral pterygoid plate, the pyramidal process of the palatine bone, and the maxillary tuberosity. The insertion is into the anterior fovea of the condylar head. The vector of contraction is anterior and medial. The origin of the superior belly is the upper one-third of the lateral pterygoid plate and the infratemporal surface of the greater wing of the sphenoid. The insertion is into the superior aspect of the pterygoid fovea, the articular capsule, the medial aspect of the articular disk, and the condyle. During protrusion and opening, the pterygoid muscle pulls the condyle and disk anteriorly. If the muscle contracts on the right, it causes lateral excursion of the mandible to the left and vice versa.
- Glenoid fossa: The mean thickness of the glenoid fossa is 0.9 mm with a range of 0.5 to 1.5 mm. The dura and the temporal lobe are located superior to the glenoid fossa.
Arthroscopic Arthroplasty (Discopexy) Technique
-
The patient is placed supine on the operating room table and nasally intubated. An examination is performed under general anesthesia to evaluate the bilateral joints for joint mobility, condylar translation, and joint sounds (Figure 31.4 [all figures cited appear in Case Report 31.1]). The patient is prepped, draped, and positioned, allowing for visualization of the entire ear and lateral canthus of the eye. An ear wick impregnated in antibiotic solution or ointment is positioned within the external auditory canal for protection. A Quinn drape is placed (Figure 31.5) to allow for visualization of the ear, TMJ, and lateral canthus of the eye and to provide for a conduit to allow for manipulation of the jaw through the oral cavity without contamination of the extraoral incisions with oral microbes.
- Standard landmarks are marked and include a line drawn from the lateral canthus of the eye and the tip of the tragus (Holmlund–Hellsing line) (Figure 31.5), the 10–2 point, and the 20–10 point (refer to Chapter 30).
- The superior joint space is insufflated with 0.5 % Marcaine on a 22-gauge needle. Good plunger rebound confirms adequate insufflation of the space (Figure 31.6). Standard fossa portal entry is obtained with the 2.0 Dyonics operative system. The joint is examined with a 1.9 Dyonics video arthroscope attached to a Stryker camera system.
- A patent irrigation system is established by placing a 22-gauge needle anterior to the fossa portal (Figure 31.7). Throughout the case, a patent irrigation system is maintained with irrigating fluid consisting of lactated Ringer's and 1:300,000 epinephrine.
- The superior joint cavity is explored and pertinent diagnostic arthroscopic findings are revealed (Figure 31.8). Operative maneuvers often follow diagnostic arthroscopy.
- A second cannula is placed at 25 mm anterior to the first, utilizing the vector measuring system (Figure 31.9). For this portal to be most effective in diagnostic and operative arthroscopy, the arthroscope should illuminate the most anterolateral aspect of the anterior recess. Then, swiveling the arthroscope along the intermediate zone and advancing into the anterior recess, identifying the disc synovial crease, the scope is swiveled to the most lateral and anterior aspect of the disc–synovial crease. The second puncture site is placed exactly in the most anterior and lateral corner of the superior joint space to ensure maximum flexibility of the operative cannula. Variations in the second puncture site and technique are dictated by the anterior recess volume and condition of the joint.
-
A 2.0 cannula is inserted into the anterolateral corner of the superior joint space. This second cannula will become the operative cannula, the device channel. The surgeon identifies the disk synovial crease with a straight probe and performs an anterior release (pterygoid myotomy) (Figure 31.10) by splicing the synovial membrane from the most medial component of the disk synovial crease to the vascular hump in the mid-portion of the anterior recess. The synovial membrane and pterygoid muscle are detached from the disk. The disk is reduced with a straight probe while holding the jaw forward (Figure 31.11).
- The retrodiscal tissue is contracted utilizing bipolar cautery. Occasionally, a superficial synovectomy (Figure 31.12) is performed, utilizing a stab incision within the posterior lateral gutter of the retrodiscal tissue using a banana blade, and then inserting the cautery into the deep retrodiscal tissues and contracting them.
- Disk fixation can be accomplished by one of two methods. The first and more traditional method is the suture discopexy. A second method involves rigid fixation with either resorbable or titanium screws.
-
In suture discopexy, the disk is held in reduction, and a 20-gauge needle with a single out poly Dexon suture is inserted through the skin and subcuticular tissues, touching the condyle, into the inferior joint space, and then it angles superiorly to target the superior lateral aspect of the posterior band of the disc (Figure 31.13). The needle is advanced through the posterior band of the disk entering the superior joint space. It is important that the 20-gauge needle is inserted underneath the reduction cannula. A straight meniscus mender is inserted in the pre-auricular crease 5 to 7 mm below the fossa portal into the superior joint space. The snare of the meniscus mender is then inserted through the meniscus mender cannula, and the suture is passed through the 20-gauge needle into the superior joint space to be captured by the snare. Now, both free ends of the suture exit the skin (Figure 31.14). Small skin incisions are made at the exit points of the suture superiorly with a #11 blade. Straight hemostat is used to dissect down the suture tracing anteriorly to the capsule. The dissection is along the course of the facial nerve. Posteriorly, the dissection is carried down halfway to the capsule along the tragal cartilage.
- A Mayo needle is used to thread the suture from anterior to posterior; both free ends of the suture now exit the skin posteriorly. While the disk is held in reduction, a tight surgeon's knot is tied, plicating the disk to the capsule and to the subcutaneous tissue (Figure 31.15).
- The joint is evaluated for function arthroscopically and by manual manipulation while the disk is reduced and the sutures are checked for suture tightness (Figure 31.16). After confirmation of no clicking noises and appropriate function or motion of the disk or condyle, the instruments are removed, and steps 15–17 are followed.
- In rigid screw disk fixation, after the anterior release is accomplished and posterior scarification and disk reduction have been completed, the disk is ready for placement of a fixation screw. The disk is maintained in reduction, and the condyle is held forward. A third puncture site is placed using the vector measuring system. Ideally, the puncture is approximately 20 mm inferior to the fossa portal. The size of the cannula depends on the size of the screw used. Typically, the authors use a 2.0-mm cannula. The cannula at its distal end has a window so that the screw is visible as it is delivered into the joint and enfacing the disk. The angle of placement of this cannula and screw hole should be from posterior to anterior, superior to inferior, and medial to lateral. This placement avoids angling the drill superiorly toward the glenoid fossa and perforating it. Once the disk is held in reduction and the cannula has been inserted, the target area is the posterior-lateral corner of the disc–condyle assembly. Holding the cannula still, a drill is delivered through the cannula to the disk, and a monocortical screw placed through the condylar head itself. The drill bit is removed, and the screw attached to the screwdriver is delivered through the cannula. The screw is inserted through the disc and into the condyle, screwing it tightly so that the disk is now fastened to the condylar head itself. The window on the cannula enables the surgeon to watch the screw actually being turned into position. Once the screw is rigidly fixated, the cannula is pulled back, and the position of the screw is verified arthroscopically to ensure that it is fully engaged and that its position is ideal. Additionally, one can take a straight probe from the working cannula and wiggle the screw to make sure it is nonmobile and fully engaged.
- Different types of screws can be applied to the joint. The authors have had success with the Osteomed cannulated screw (Osteomed, TX, USA), an Inion screw (Inion, Tampere, Finland), and a Smart nail (ConMed Linvatec, FL, USA). The ideal situation for rigid disc fixation is an average-sized joint space and a well-formed, nonperforated disc.
-
At the completion of the disk fixation procedure, the joint is lavaged, and one ampule of Healon (hyaluronic acid) is deposited (Figure 31.18) to act as an intra-articular Band-Aid to minimize small microbleeds and also to temporarily replenish the hyaluronic supply of the joint.
- The external wounds are closed with 5-0 fast-absorbing gut sutures or 6-0 nylon sutures (Figure 31.19). The wound is covered with a thin layer of bacitracin and a light dressing.
- The patient is positioned face up, and the jaw is manipulated under general anesthesia to confirm a tight motion without eminent subluxation. The TMJ is specifically evaluated for the absence of joint clicks and for smooth translations during functioning. At the completion of the procedure, the occlusion will be shifted to the opposite side as expected.

Figure 31.1. Patient with recurrent left-sided temporomandibular joint locking and pain with no facial asymmetries.
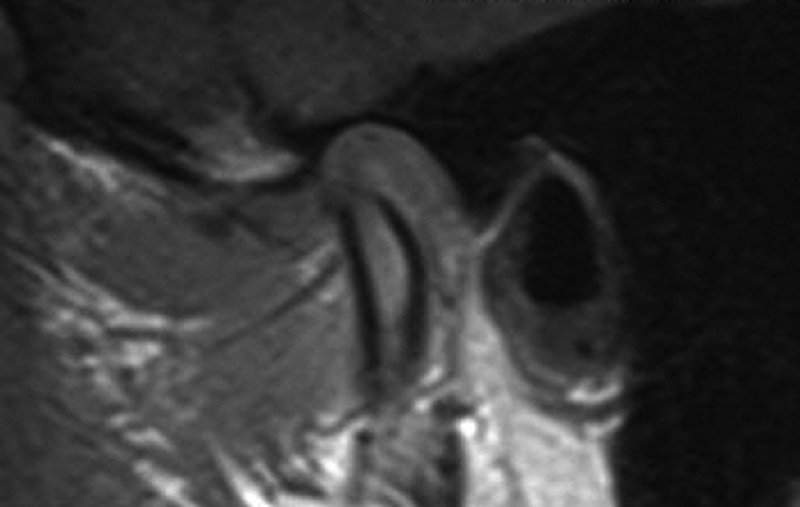
Figure 31.2. Sagittal T1-weighted open-mouth magnetic resonance imaging demonstrating an anteriorly displaced disk.
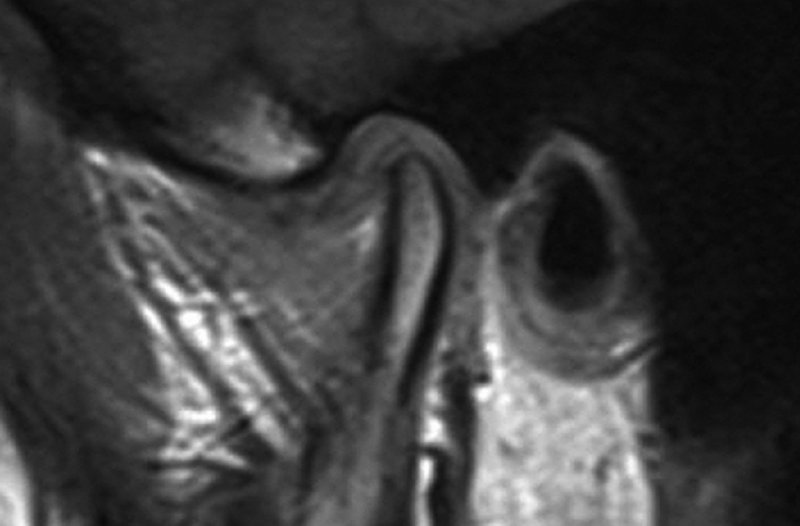
Figure 31.3. Sagittal T1-weighted closed-mouth magnetic resonance imaging demonstrating a nonreducing anteriorly displaced disk.

Figure 31.4. An examination of the joints is performed under general anesthesia.

Figure 31.5. The H and H line is marked, and a Quinn drape is placed to allow instrumentation of the left temporomandibular joint and manipulation of the oral cavity without contamination of the surgical site.

Figure 31.6. The superior joint space is insufflated with 0.5% Marcaine totaling 5 mL with good plunger rebound.
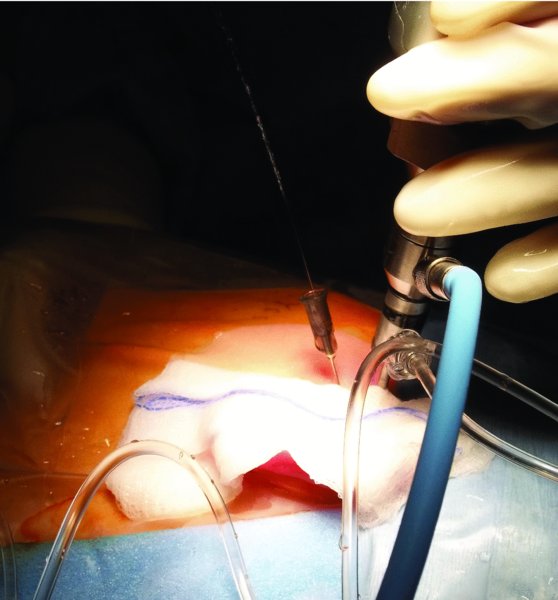
Figure 31.7. A patent irrigation system is established by placing a 22-gauge needle anterior to the fossa portal. The irrigation system is maintained with irrigating fluid consisting of lactated Ringer's and 1:300,000 epinephrine.

Figure 31.8. Findings consistent with a nonreducing disk and joint synovitis.

Figure 31.9. A second cannula is placed 25 mm anterior to the fossa portal into the anterolateral corner of the superior joint space with a 2.0 cannula.

Figure 31.10. The disk synovial crease is identified, and an anterior release is performed by splicing the synovial capsule and the pterygoid muscle at their insertion to the disk.

Figure 31.11. Conservative muscle resection is performed on the medial aspect of the disk to allow for reduction. The disk is reduced with a probe while the jaw is positioned forward.
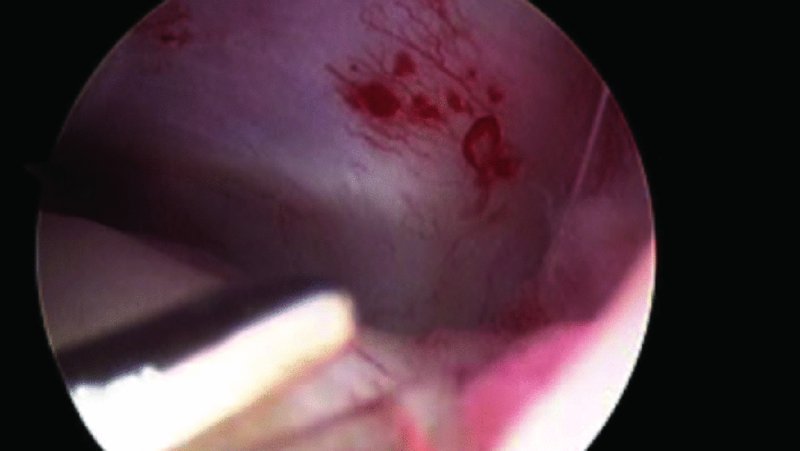
Figure 31.12. The retrodiskal tissue is shortened, and a partial arthrodesis is completed utilizing a holmium laser on low voltage. A superior synovectomy was also performed.
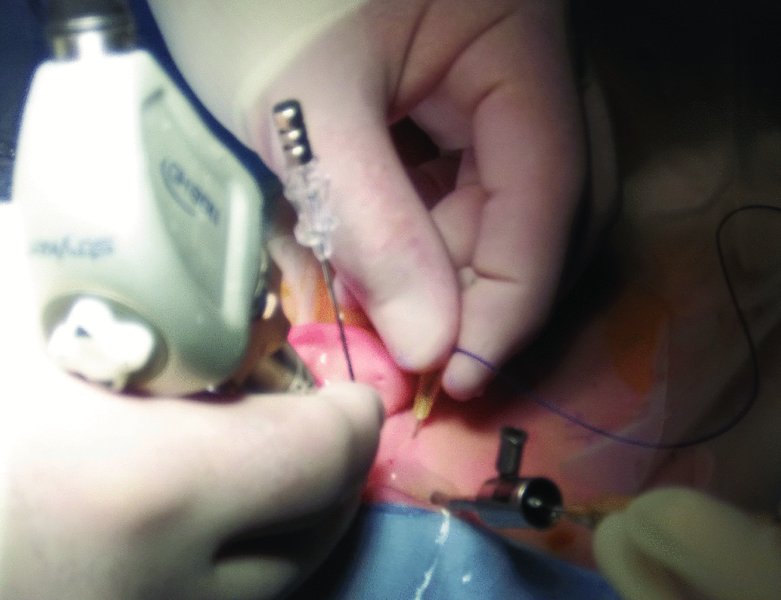
Figure 31.13. Disk fixation is accomplished by holding the disk in place and passing a #1 poly Dexon suture through a 20-gauge needle and through a separate puncture into the joint with a meniscus mender.

Figure 31.14. Both free ends of the suture exit the skin.
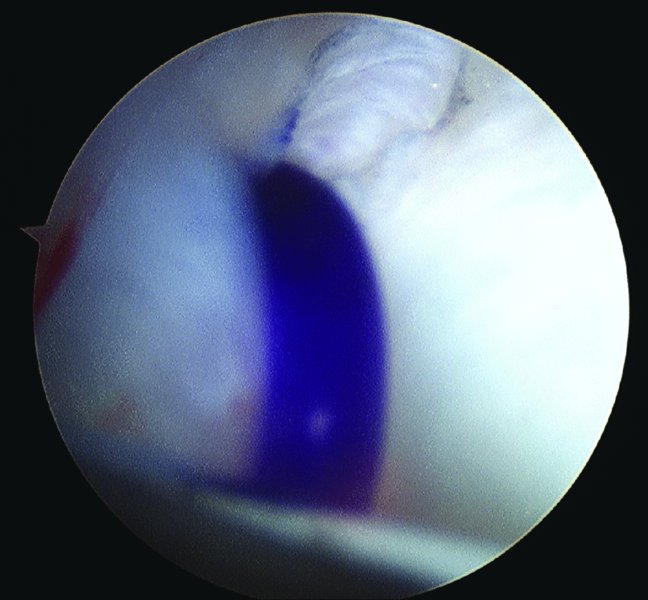
Figure 31.15. While the disk is held in reduction, a tight surgeon's knot is tied, plicating the disk to the capsule and to the subcuticular tissue.
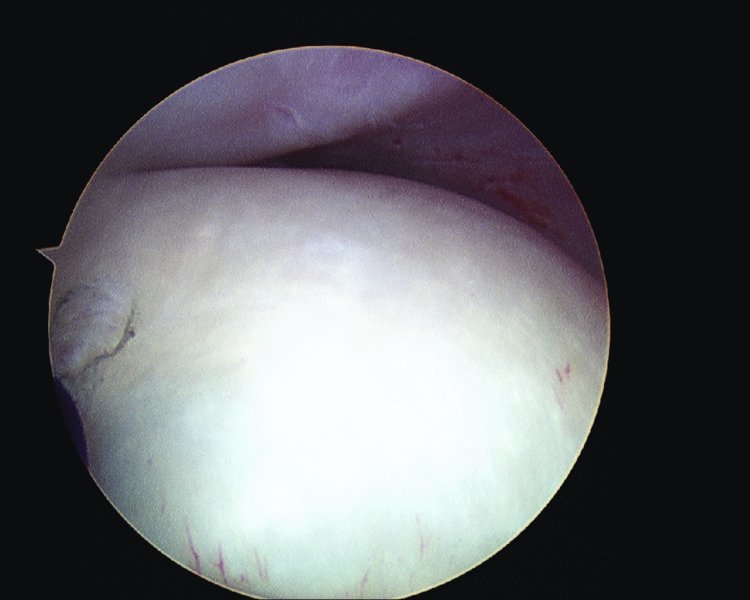
Figure 31.16. The disk position is verified arthroscopically and found to be ideal. The joint was functioned under arthroscopic visualization, and the disk maintained its position.
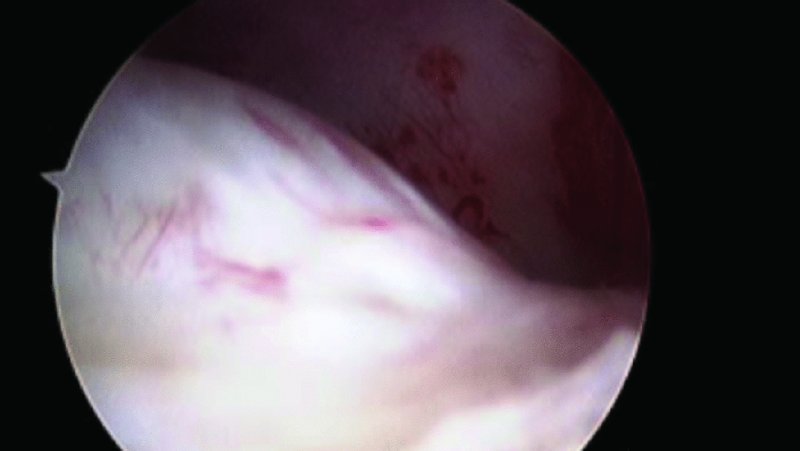
Figure 31.17. Additionally, a retrodiskal arthrodesis is completed on the redundant synovium with a low-voltage weld holmium laser.

Figure 31.18. One ampule of Healon is deposited at the completion of the procedure.

Figure 31.19. The external ports are closed with 6-0 nylon sutures.
Postoperative Management
- Ice packs are placed continuously within the TMJ region.
- Intravenous antibiotics are utilized during admission. Oral antibiotics are utilized upon discharge for a total antibiotic course of 5 days postoperatively.
- Corticosteroids are administered postoperatively.
- Wound care involving cleaning of the incision sites with a mixture of 50% hydrogen peroxide and 50% normal saline is begun on postoperative day 2. A thin layer of bacitracin is applied to all skin incisions after cleaning.
- A full liquid diet is employed for the first week and then gradually increased.
- For patients with occlusal appliances, they are instructed to not wear their appliances for the first week after surgery.
- Patients are instructed to begin physical therapy exercises beginning the day after surgery.
Complications
- Facial nerve damage: Weakness from inadvertent damage or stretching of the temporal and/or zygomatic branches of the facial nerves may occur with arthroscopic entry and manipulation, or from fluid extravasation into the surrounding tissues. Paralysis is typically transient, and most patients recover completely within 4–12 weeks.
- Pre-auricular anesthesia and paresthesia: The auriculotemporal nerve is typically posterior, but in close proximity to, the glenoid fossa puncture site. Damage to the pre-auricular nerve may occur during arthroscopic entry and manipulation, or from fluid extravasation into the surrounding tissues. Postoperative anesthesia around the entry sites is a common occurrence that typically spontaneously resolves within 2–4 weeks.
- Iatrogenic scuffing of the fibrocartilage lining: The cartilage covering the eminence and fossa is prone to iatrogenic damage during instrumentation. Significant scuffing impairs visibility during arthroscopic procedures and may lead to the misdiagnosis of chondromalacia by the inexperienced arthroscopist.
- Damage to the middle ear: The mechanism of entry into the middle ear is through either the bony external auditory canal (EAC) or the soft tissue EAC. Large perforations are identified intraoperatively with leakage of irrigation fluid from the EAC. Attention to detail when inserting the arthroscope and not inserting the arthroscope more than 20 to 25 mm without checking its position are keys to preventing canal perforations. The arthroscope should be inserted anterior and forward to the EAC, not parallel to its external surface. Small tears and perforations of the EAC and tympanic membrane typically heal without operative intervention and without future sequelae with the use of packings, antibiotics, and corticoid ointment. If the tympanic membrane is perforated and the ossicles appear in the field of view, immediate cessation of the procedure and intraoperative otolaryngologist consultation are warranted.
- Inadvertent perforation of the glenoid fossa: Rare. May occur during inappropriate entrance and instrumentation through the fossa port. Instrumentation toward the tubercle and away from the fossa i recommended to avoid injury to the contents of the cranial fossa. Intraoperative neurosurgical consultation is recommended. Most small cerebrospinal fluid (CSF) leaks will heal spontaneously. If CSF continues to collect within the wound or drain through the incision site, a pressure dressing should be applied and the patient hospitalized with head elevation and antibiotics. Persistence of a leak for more than 48 hours is an indication for consultation with potential lumbar subarachnoid drain placement. A computed tomography scan of the head with bone windows should be obtained to document the site. Surgical repair of the middle fossa dura is rarely necessary.
- Excessive hemorrhage within the joint space: Intracapsular hemorrhage has numerous etiologies to include excessive bleeding upon entering the capsule from tearing of the superficial temporal vessels, excessive bleeding from severely inflamed synovium or retrodiscal tissue upon joint entrance, and bleeding from the pterygoid artery when performing myotomy for anterior release procedures. In arthroscopic surgery, pressure irrigation typically clears the visual field adequately when persistent hemorrhaging occurs. Occasionally, pressure irrigation will not stop the hemorrhaging, leaving behind a joint congested with blood with poor visibility, which prolongs healing, increases postoperative discomfort, and extends recovery time. Several methods are used to control intracapsular bleeding that is refractory to pressure irrigation:
- Arthroscopic cautery can be applied to the bleeding site. If using laser, apply laser in the synovectomy mode until the tissue blanches. Cautery or laser application is successful in most cases of minor bleeding.
- Inject small amounts of local anesthetic with vasoconstrictor into the bleeding site. A 3 1/2-inch spinal needle on a 3 mL syringe is passed down the cannula and directly into the involved tissues.
- Insufflate the joint through the cannula with local anesthetic with vasoconstrictors, bathing all of the joint tissues.
- Insufflate the joint under pressure using irrigation fluid. Then, tamponade all outflow cannulae for 5 minutes, so the hydrostatic pressure of the irrigation fluid directly tamponades the bleeding site.
- If bleeding persists after A–D, remove instruments from the joint and apply direct, external tamponading pressure in the pre-auricular area for 5 minutes. For added pressure, seat the condyle into the fossa if the bleeding source is located in the posterior pouch. If it is in the anterior pouch, manipulate the mandible to a protrusive position. After 5 minutes, reinsert the instruments into the original punctures and assess the condition of the joint.
- Insert a No. 4 catheter balloon through the second portal, inflate the balloon with normal saline, and leave it in the area of bleeding for 5 minutes. Then deflate and reassess.
-
If bleeding persists, approach the joint via open surgery and pack the area.
The above steps should be performed in this order (A–G) until the bleeding stops or the procedure is terminated. It is important to examine the contents of the joint space for coagulums deposited in dependent areas and least accessible from the irrigation fluid such as the medial recess. If this is the case, aspiration of joint contents will remove the blood products. However, caution must be observed to not disturb the blood clot over the bleeding site.
- Damage to the superficial temporal vessels with or without formation of A-V fistulae: The superficial temporal vessels (STA and STV) are intimately related to the posterior aspect of the joint capsule. Damage to the STA and STV is initially managed by applying direct controlled pressure. Cases refractory to direct pressure are managed with suture ligation of the offending vessel. Although rare, other investigators have reported the formation of A-V fistulae after injury to the superficial temporal vessels. Typically, patients complain of a constant hissing and whishing sound over the operated TMJ. Superficial temporal A-V fistulae are managed with embolization and fistulectomy.
- Instrument failure or loose bodies within the joint: Instrument failure can be attributed to manufacturing defects, misuse of instruments, and wear of parts within the instrument itself, leading to instrument breakage. Instrument breakage and loose bodies within the joint can be minimized by checking the structural integrity of an instrument before use, using ferromagnetic instruments, having a “golden retriever” available, avoiding excessive force when placing and removing instruments, maintaining visualization of instruments at all times, and keeping movable instruments closed during removal. If breakage of instruments or material (suture) occurs, the following protocol should be followed:
- Stop the procedure. Maintain the position of the arthroscope and working cannulae.
- Keep the instrument in view (arthroscopic visualization).
- Check inflow bags to make sure there is sufficient irrigation fluid so that the joint is always distended.
- Record and measure the depth of the instrument with a scored cannula.
- Have adequate removal instruments available. Extra instruments are a must.
- Adjust inflow as to ensure optimal visibility.
- Take a radiograph of the joint if the instrument cannot be found arthroscopically.
- Consider fluoroscopic assistance to localize the piece if the instrument cannot be found arthroscopically.
- If using a grabber to remove a fragment, the tips might not fit in a working cannula upon removal. It might therefore be desirable to switch systems to a 3 mm diameter working cannula with a “switch stick” technique and retrieve the broken fragments with instruments or a “golden retriever.”
- If an instrument is broken and cannot be retrieved, the possibility of re-arthroscopy alone or with guided fluoroscopy or open surgery should be contemplated. The attempt should be made in the early postoperative phase (10 days after the first procedure) up to 6 weeks. If this fails, the doctor and the patient must review complications associated with leaving the piece within the joint space. The possibility of future osteoarthrosis or foreign body reaction occurring as a result of leaving the fragment within the joint space must be understood by the patient.
- Infection of the puncture sites: Rare. Minimized with proper sterilization techniques, sterile operating room conditions, prophylactic antibiotics, and a high volume of irrigation used during arthroscopic surgery. Most infections are successfully managed with exploration of the area under local anesthesia, removal of residual suture when found, or breakdown of the suture by the mechanical action of exploring the area and the administration of oral cephalosporin for 7–10 days.
- Noninfectious postoperative effusion: Effusions typically appear as edema of the pre-auricular area, resulting in a higher level of pain upon palpation than that normally encountered postoperatively. Patients are managed with joint rest, a soft diet, application of heat over the affected area, and nonsteroidal anti-inflammatory medication for pain management.
Key Points
- Ideal patients for discopexy include patients with a class I occlusion, suitable joint space, and an articular disc that dislocates but does not show remodeling. These conditions are typically found in Wilkes stage II, stage III, and early stage IV joint disease and have an 80% success rate with discopexy. Patients with Wilkes late stage IV and stage V joint disease have a discopexy success rate of only 60%.
- An efficient anterior release should be established through the disc synovial crease. All muscle fibers are resected from the disc under direct arthroscopic visualization. The cut through the superior belly of the pterygoid muscle is complete when a space between the superior belly of the pterygoid muscle and inferior belly of the pterygoid muscle is encountered and the inferior belly of the pterygoid muscle can be seen to be more purple in color than the superior belly. Care must be taken to avoid cutting to the vascular hump, or significant bleeding will be encountered.
- During disc reduction, the condyle should be in a closed position, the operative cannula and the scope are within the anterior recess, the anterior release has been completed, and the operative cannula and the scope are then walked back in the lateral sulcus to the posterior pouch. Once these two instruments reach the peak of the articular eminence, the condyle is pulled forward, and then both instruments can drop into the posterior pouch. The disc is reduced by compressing the retrodiscal tissue laterally with a straight probe, while the condyle is in a forward or forward and contralateral position, or occasionally it is necessary to reduce the disc by taking a hook probe and compressing the oblique protuberance.
- In suture disc fixation, the needle should be advanced through the lasso first, and then the suture is advanced beyond the needle approximately 1 cm. The suture needle is then withdrawn from the lasso, and the lasso is cinched down around the suture material. The disc should be held in reduction while the suture is being passed and retrieved.
- In order for the knot to be buried in the subcutaneous fatty tissue, a straight hemostat is used to dissect down the suture tracing anteriorly to the capsule through the slit incisions. The dissection is along the course of the facial nerve. Posteriorly, the dissection is carried down halfway to the capsule. The skin is closed primarily with 6–0 nylon interrupted sutures.
- Caution must be observed when making the myotomy at the most anteromedial corner (anterior release). When the anteromedial synovial drape is incised at the junction with the disk, an artery approximately 1 to 2 mm in diameter usually is found directly underneath this junction. Arthroscopically, it appears as a white tubular structure. If this vessel is incised during the anterior release, copious bleeding will occur.
References
- McCain, J.P., 1996. Principles and practice of temporomandibular joint arthroscopy. St. Louis, MO: Mosby.
- McCain, J.P. and Hossameldin, R.H., 2011. Advanced arthroscopy of the temporomandibular joint. Atlas of the Oral and Maxillofacial Surgery Clinics, 19 (2), 145–67.
- McCain, J.P., Podrasky, A.E. and Zabiegalski, N.A., 1992. Arthroscopic disc repositioning and suturing: a preliminary report. Journal of Oral and Maxillofacial Surgery, 50 (6), 568–79.
- Perez, R., 2007. Temporomandibular joint arthroscopic arthroplasty with rigid disc fixation—preliminary results in treatment of Wilkes internal joint derangement stages II–V: a 3-year retrospective study. Journal of Oral and Maxillofacial Surgery, 65 (9, Suppl.), 38.e3–38.
- Tarro, A.W., 1994. A fully visualized arthroscopic disc suturing technique. Journal of Oral and Maxillofacial Surgery, 52 (4), 362–9.