CHAPTER 59
Free Vascularized Fibula and Graft Harvest
Robert M. Laughlin1 and Christopher M. Harris2
1Department of Oral and Maxillofacial Surgery, Naval Medical Center San Diego, San Diego, California, USA
2Department of Oral and Maxillofacial Surgery, Naval Medical Center Portsmouth, Portsmouth, Virginia, USA
The harvest of a free vascularized fibula for the reconstruction of combined hard and soft tissue maxillofacial defects.
Indications
- Reconstruction of surgical defects following oncologic ablative surgery, traumatic defects, and congenital anomalies requiring cutaneous and/or osseous vascularized tissue
- Segmental continuity defects of the maxilla and mandible greater than 5 cm. A long segment of bone up to approximately 25 cm is available for harvest. The skin paddle has proven to be dependable if care is taken to preserve the fasciocutaneous perforators. Innervation of the flap is possible, and the flap has adequate bone stock to accept endosseous dental implants
Contraindications
- Medical conditions that would not be compatible with extended operative procedures
- Hypercoagulable states
- Relative contraindications:
- Vasculitis
- Connective tissue disorders
- Peripheral vascular disease
- Venous insufficiency
- Congenital anomalies of the peroneal artery
- Other disorders that may impact coagulation and wound healing
Note: Evaluation of the patient's physiologic status is more important than the chronologic age of the patient in determining the appropriateness of a free tissue transfer procedure.
Preoperative Studies
- Bilateral lower extremity angiogram or magnetic resonance angiography. The arteriogram should demonstrate normal three-vessel runoff of the right and left popliteal artery with normal patency of the anterior, posterior, and peroneal vessels bilaterally.
- Palpation of the dorsalis pedis (anterior tibial artery) and posterior tibial pulses.
Flap Anatomy
- Dominant-peroneal artery
- Length: 2.0 cm (2–4 cm)
- Diameter: 1.5 mm (1–2.5 mm)
- Minor-periosteal and muscular branches
- Length: 1.2 mm (0.8–1.7 mm)
- Diameter: 1.0 mm (0.8–1.7 mm)
Typically, 4–8 cutaneous arteries arise from the peroneal artery. These typically are septal or septo-muscular cutaneous perforators coursing through the posterior crural (lateral) septum.
Surgical Anatomy
The lower leg can be viewed as four compartments:
- Lateral compartment: Bordered by the posterior crural septum and the anterior crural septum and contains the peroneus longus and peroneus brevis muscles.
- Anterior compartment: Bordered by the anterior crural septum and the interosseous membrane and contains the extensor digitorium longus and extensor hallucis longus muscles. The anterior tibial vasculature and deep peroneal nerve lie on the superficial aspect of the interosseous membrane in the anterior compartment.
- Superficial posterior compartment: Bordered by the interosseous membrane and the intermuscular membrane of the flexor hallucis longus and soleus muscles. The peroneal vessels lie on the deep aspect of the interosseous membrane and course distal along the fibula. The posterior tibial vessels are deep to the tibialis posterior muscle.
- Deep posterior compartment: Bordered by the intermuscular membrane of the flexor hallucis longus and soleus muscles and the posterior crural septum; it contains the lateral aspect of the soleus muscle.
Preoperative Preparation
- A bump may be placed under the ipsilateral hip to aid in access to the lateral surface of the lower extremity.
- A heel bump (i.e., a 5 lb. sandbag or 1 L IV fluid bag) is placed on the operating room table that allows the lower extremity to maintain 90° of flexion at the knee; it will aid in the graft harvest.
- Doppler flow meter.
- Tourniquet (recommended but optional).
- A second set of instruments for the harvest team.
Surgical Procedure
- A normal preoperative arteriogram of bilateral lower extremities demonstrating three-vessel runoff of the right and left popliteal artery with normal patency of all distal vessels.
- The patient is placed in a supine position. The knee is flexed to 90°, and the hip is internally rotated with the use of a hip bump. The heel is then placed on a gel bumper, which is secured to the table. The patient is prepped and draped in a sterile fashion. A sterile tourniquet is applied.
- Anatomic landmarks are palpated and marked (Figure 59.1) to include the head of the fibula and the lateral malleolus of the ankle. The dorsalis pedis and posterior tibial pulses are palpated and marked with Doppler accordingly. With a surgical pen, a mark is placed 6–8 cm inferior to the head of the fibula and 6–8 cm superior to the lateral malleolus. This allows the proximal and distal 6–8 cm of the fibula and its ligamentous attachments to be preserved. A line is drawn along the posterior crural septum connecting the two marks.
- If a skin flap is to be harvested in conjunction with the fibula, the flap should be designed along the posterior septal crural. A Doppler will allow for the identification of septocutaneous perforating vessels (Figure 59.2). Typically, the skin flap is designed in the distal one-third of the flap.
- The extremity is exsanguinated, and the tourniquet inflated to 300 mmHg. Time of inflation must be recorded. Inflation time must be keep under 2 hours to avoid possible ischemic events.
-
A skin incision is made to the depth of the superficial fascia along the length of the incision to include the skin flap (Figure 59.3). A subfascial dissection is performed to elevate the skin island and expose the posterior crural septum (Figure 59.4). Septocutaneous perforators may be seen emerging from the posterior crural septum (Figure 59.5). If no septocutaneous perforators are seen, a muscle cuff is included to capture any musculocutaneous perforators. Anterior and posterior skin flaps are elevated superficial to the fascia, exposing the peroneus longus muscle anteriorly and the soleus muscle posteriorly. The superficial peroneal nerve should be identified and preserved.
- The peroneus longus muscle is elevated and retracted anteriorly and medially (Figure 59.6). This provided the approach through the lateral compartment of the fibula. The peroneus brevis is then identified and divided, maintaining a 5 mm cuff of muscle to protect and preserve the underlying periosteum, while allowing access to the fibular bone. Dissection then proceeds anteriorly medially along the fibula to the anterior crural septum marking the anterior compartment of the fibula.
- The anterior crural septum is divided to expose the extensor digitorium longus and extensor hallucis muscles. Maintaining a 5 mm cuff of muscle around the fibula, the digitorium longus and extensor hallucis muscles are divided to expose the interosseous membrane inferiomedially. The anterior tibialis vessels and the deep peroneal nerve are identified anteriomedial to the fibula in the anterior compartment and retracted medially.
- The interosseous membrane is incised 5 mm medially from the fibula in the proximal third and extended the length of the fibula. Care must be taken when incising the interosseous membrane due to the close proximity of the peroneal vasculature on the inferior aspect of the membrane.
-
A subperiosteal dissection is performed at the proposed proximal and distal osteotomy sites. Protecting the medial aspect of the fibula and peroneal vessels, the proximal and distal osteotomies are performed with a reciprocating or oscillating saw, ensuring that a minimum of 6–8 cm of fibula remains distal to the fibular head and proximal to the lateral malleolus (Figures 59.7 and 59.8).
- A bone clamp is used to retract the fibula laterally, allowing visualization of the peroneal vessels distally (Figure 59.9). The posterior tibialis muscle is divided distal to proximal to allow the pedicle to be visualized the entire length of the fibula.
- The tourniquet is let down and time recorded. The dorsalis pedis and posterior tibialis pulses are verified by palpation or Doppler ultrasound. The flow through the peroneal vessels is also verified. A vessel loop is placed circumferentially around the distal peroneal vessels to occlude flow. The flow through the dorsalis pedis and posterior tibialis vessels was again verified and should demonstrate strong signals. The distal peroneal vascular bundle is then ligated and divided.
- The dissection proceeds posteriolaterally in the deep and superficial posterior compartments dividing the flexor hallucis longus and soleus muscles while maintaining a 5 mm muscle cuff on the fibula. Doppler is then used to confirm a strong signal of the peroneal vessels. The proximal peroneal vascular bundle is then ligated and divided. The fibula and skin paddle are passed to the reconstruction team (Figure 59.10).
-
After adequate hemostasis is achieved, the deep muscle layers are reapproximated with 2-0 Vicryl interrupted sutures (Figure 59.11). Two suction drains are placed. The dermal layer is reapproximated. The skin is closed with staples or a nonresorbable suture (Figure 59.12). In the event that the skin flap is greater than 4 cm, a split-thickness skin graft may be required.
- The dorsalis pedis and posterior tibialis pulses are palpated, Dopplered, and marked. The foot is checked for warmth and adequate capillary refill.
-
Bacitracin is applied to the surgical site, and a Telfa dressing is placed over the incisions. The lower leg is circumferentially wrapped with cotton batting and an Ace bandage. The leg is then elevated. (See Figures 59.13 and 59.14 for postoperative images at 2 days and 6 weeks.)

Figure 59.1. Anatomic landmarks are palpated and marked to include the head of the fibula and the lateral malleolus of the ankle. Marks are placed 6–8 cm inferior to the head of the fibula and 6–8 cm superior to the lateral malleolus. This allows the proximal and distal 6–8 cm of the fibula and its ligamentous attachments to be preserved. A line is then drawn along the posterior crural septum connecting the two marks.

Figure 59.2. The dorsalis pedis and posterior tibial pulses are palpated and Dopplered accordingly and marked for future reference.

Figure 59.3. A skin incision is made to the depth of the superficial fascia along the length of the incision to include the skin flap.
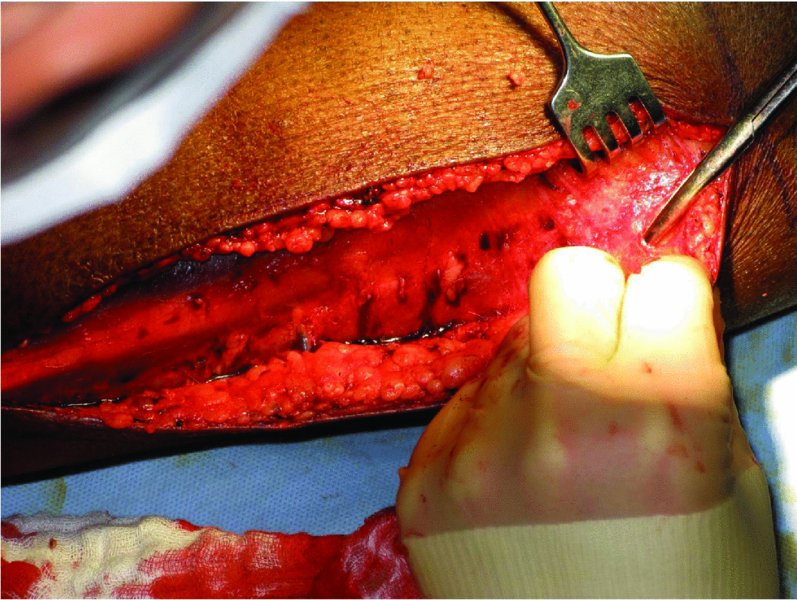
Figure 59.4. A septocutaneous perforator is seen emerging from the posterior crural septum. The superficial fascia is dissected to allow access to the lateral compartment.
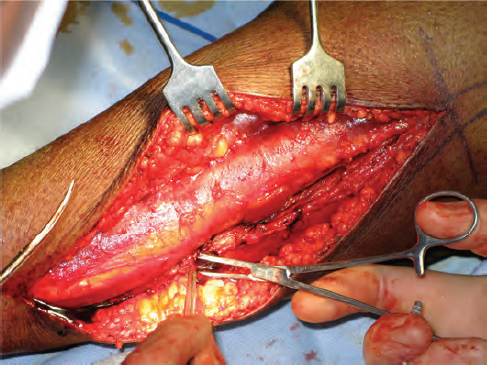
Figure 59.5. The septocutaneous perforator is ligated (a skin paddle was not utilized in this case).

Figure 59.6. The peroneus longus muscle is elevated and retracted anteriorly and medially. This provided the approach through the lateral compartment of the fibula. The peroneus brevis is then identified and divided, maintaining a 5 mm cuff of muscle to protect and preserve the underlying periosteum, while allowing access to the fibular bone.
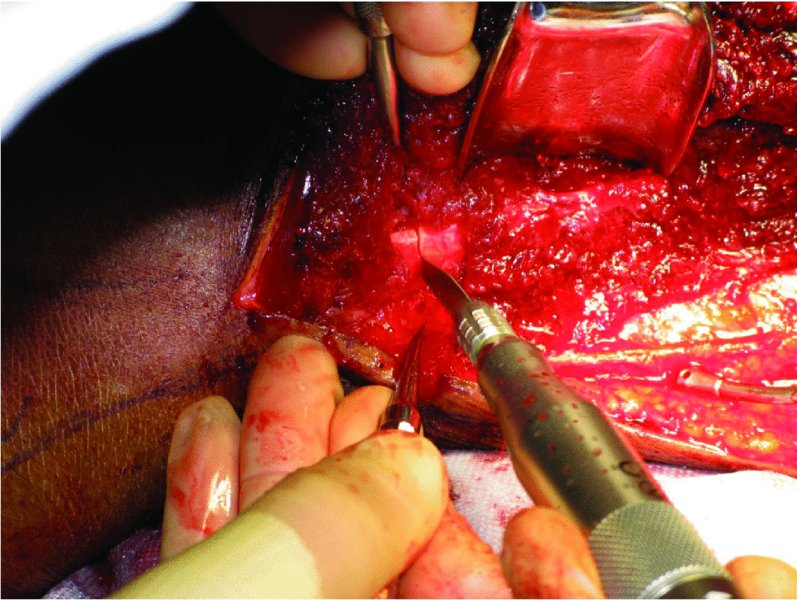
Figure 59.7. A subperiosteal dissection is performed at the proposed proximal and distal osteotomy sites. Protecting the medial aspect of the fibula and peroneal vessels, the proximal and distal osteotomies are performed with a reciprocating or oscillating saw, ensuring a minimum of 6–8 cm of fibula remains distal to the fibular head and proximal to the lateral malleolus.
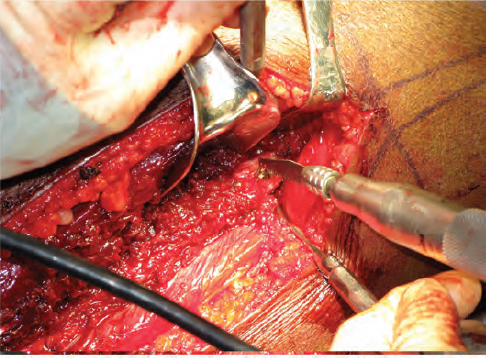
Figure 59.8. Proximal osteotomy performed with a reciprocating saw, ensuring a minimum of 6–8 cm of fibula remains distal to the fibular head.
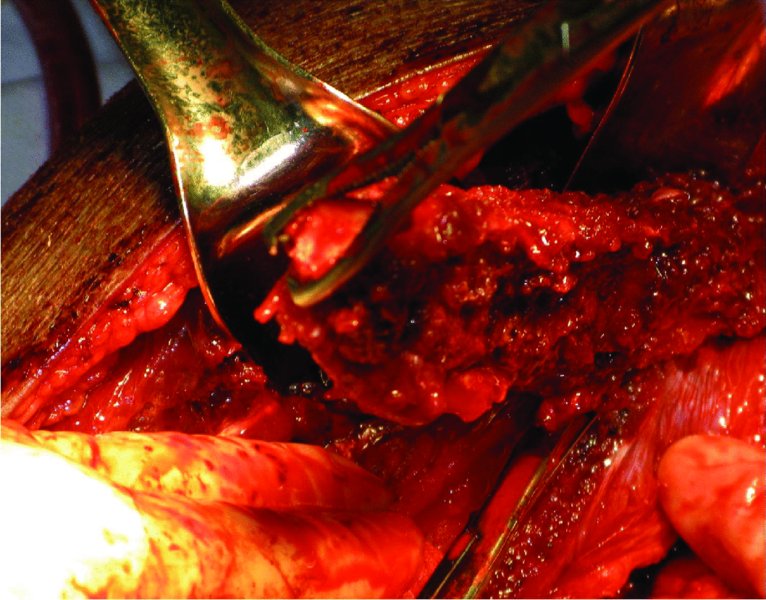
Figure 59.9. A bone clamp is used to retract the fibula laterally, allowing visualization of the peroneal vessels distally. The posterior tibialis muscle is divided distal to proximal to allow the pedicle to be visualized along the entire length of the fibula.
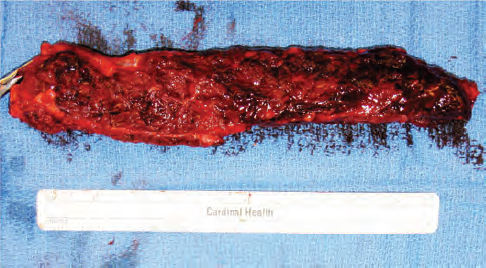
Figure 59.10. The fibula and skin paddle, if harvested, are passed to the reconstruction team for inset.
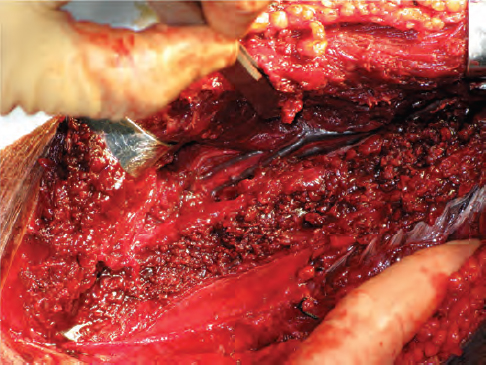
Figure 59.11. After adequate hemostasis is achieved, the deep muscle layers are reapproximated with 2-0 Vicryl interrupted sutures, and two suction drains are placed.

Figure 59.12. After the dermal layer is approximated, the skin is closed with staples or a nonresorbable suture. In the event that the skin flap is greater than 4 cm, a split-thickness skin graft may be required.

Figure 59.13. Plain radiographic film taken of the harvest site on postoperative day 2.

Figure 59.14. Surgical site 6 weeks postoperatively.
Complications
- Compartment syndrome
- Muscle weakness
- Ankle instability as the far end of the fibular forms part of the ankle joint and may become less stable
- Nerve damage to the peroneal nerves and muscle branches, leading to weakness and limitation of the range of motion of the foot
- Neurosensory damage with resultant numbness on the dorsal aspect of the foot
- Lower leg blood vessel damage to anterior or posterior tibia vessels
- Infection
- Chronic pain of lower extremity
- Loss of limb
Key Points
- Flap harvest requires meticulous dissection of the vascular pedicle. Magnification and an experienced, microvascular-trained assistant surgeon are ideal.
- Preoperative verification of collateral blood flow is required prior to flap harvest. Potential necrosis with loss of lower extremity function may occur with no collateral circulation.
- Perioperative antibiotic coverage is continued for 72 hours postoperatively. Sterile technique is used to change any dressings associated with the wound. Lower extremity infections can cause significant morbidity and disability.
References
- Eisele, D., 2009. Complications in head and neck surgery. 2nd ed. St. Louis, MO: Mosby.
- Grabb, W.C. and Strauch, B., 2009. Grabb's encyclopedia of flaps. 3rd ed. Philadelphia: Lippincott Williams & Wilkins.
- Urken, M., 2010. Multidisciplinary head and neck reconstruction: a defect-oriented approach. Philadelphia: Lippincott Williams & Wilkins.
- Wei, F-C., 2009. Flaps and reconstructive surgery. Philadelphia: Saunders Elsevier.