When a new patient comes to the doctor’s office, a medical record must be established. The medical record or chart is a legal document. There are different systems used to document patient information. One method is source-oriented. The information is arranged according to the professional who supplied the data. This type of record describes all problems and treatments on the same page. The record contains physician notes, nursing/assistant notes, laboratory records, radiology reports, and insurance information.
The problem-oriented medical record (POMR) is another way to document patient information. This method makes it easier for the physician to follow a patient’s progress and treatment. The information in the POMR is the history and physical exam database; a detailed patient problem list; an educational, diagnostic, and treatment plan; as well as the progress notes.
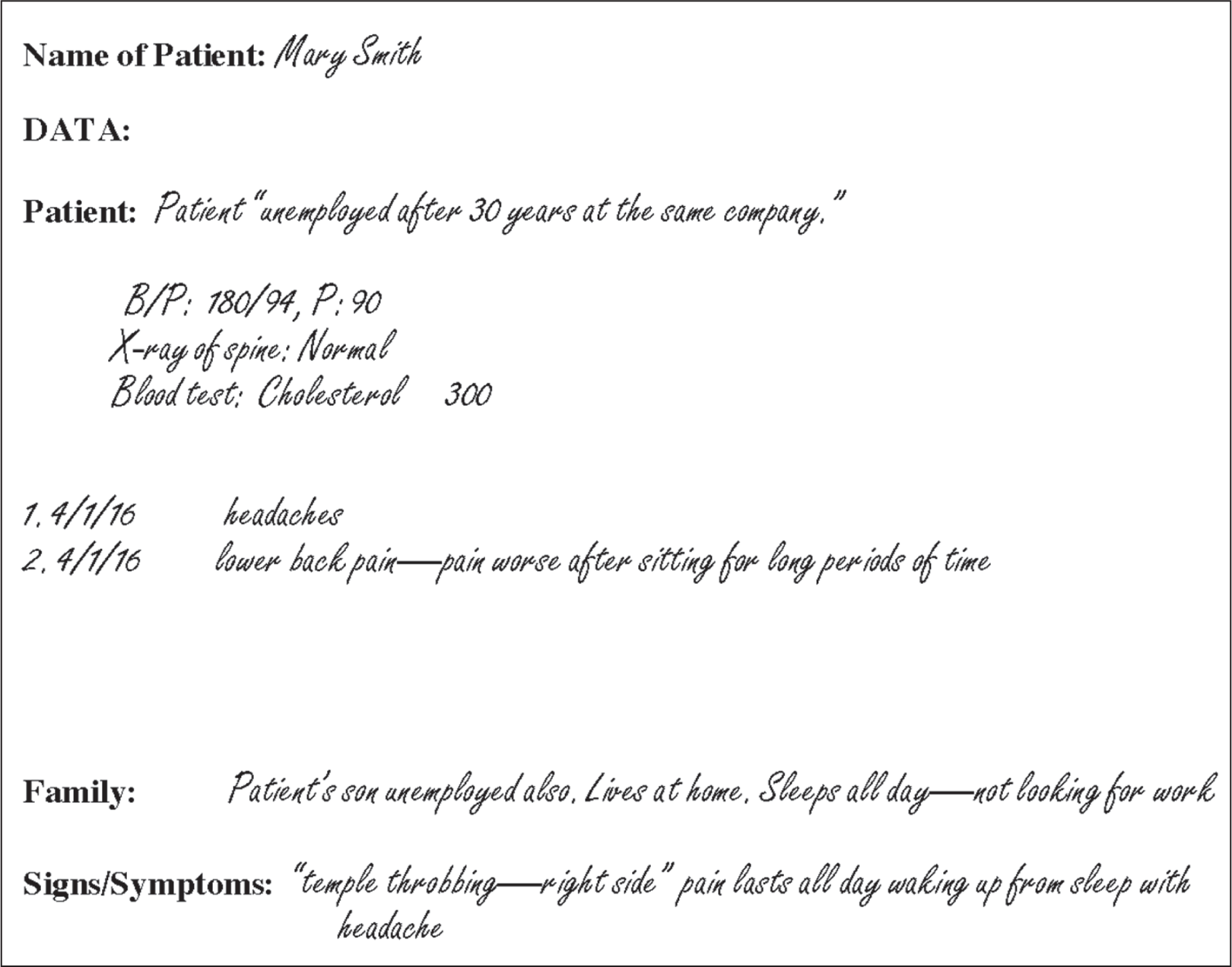
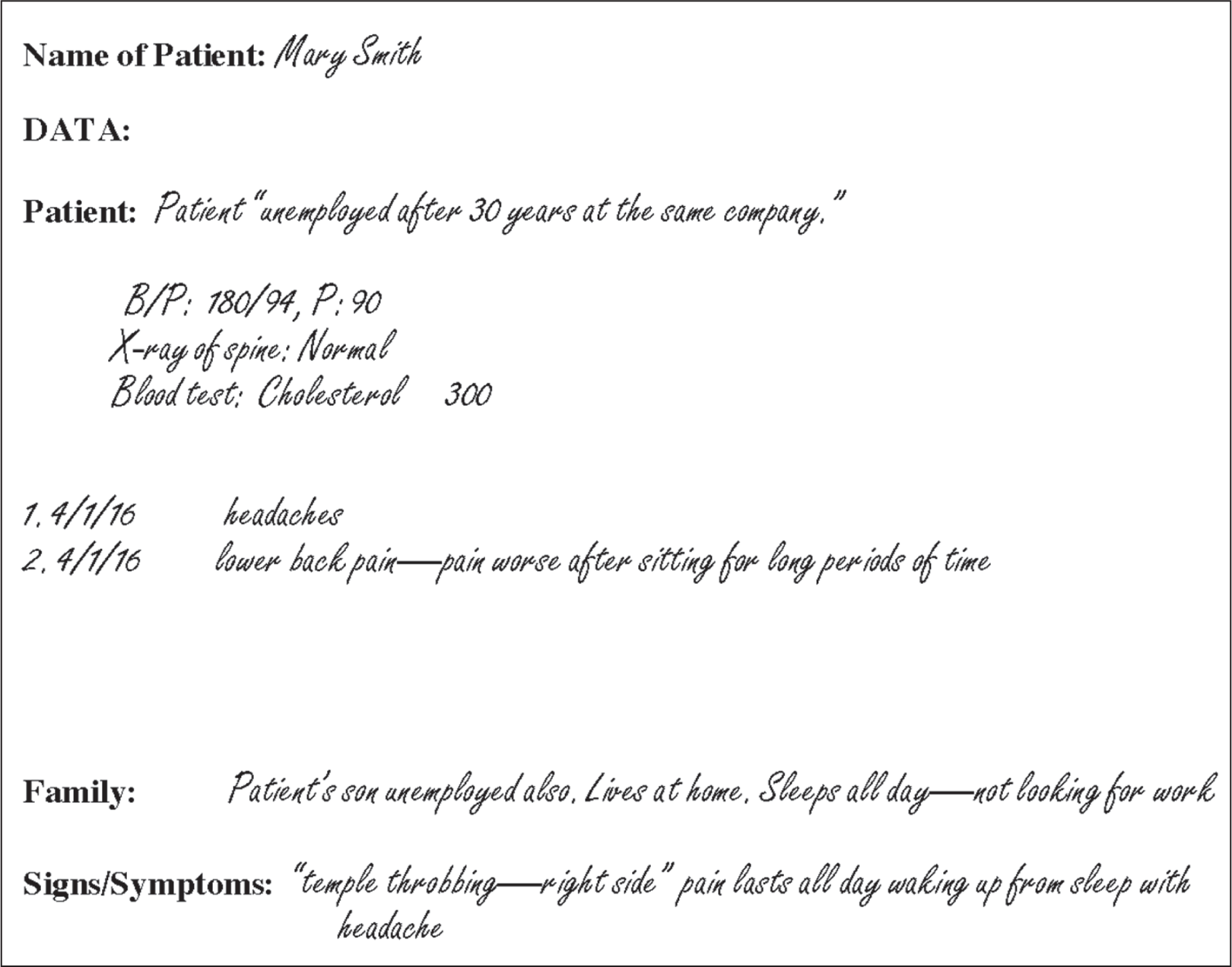
The database includes a record of the patient’s history, information from the initial interview with the patient, and all findings and results from examinations, any tests, and other procedures.
Each problem the patient presents is listed separately, given its own number, and dated when it was identified. The physician must be aware if the patient has personal problems or family issues, such as marital problems, that may interfere with treatment. Along with each patient problem, there should be a detailed diagnostic and treatment summary in the record. Subsequent visits are documented by listing the problem and describing the current status, new complaints or symptoms, treatment, and the patient’s response to the treatment plan. You should review the problem list and make sure that age- and gender-specific health promotion and disease prevention problems are noted and tracked in the POMR.
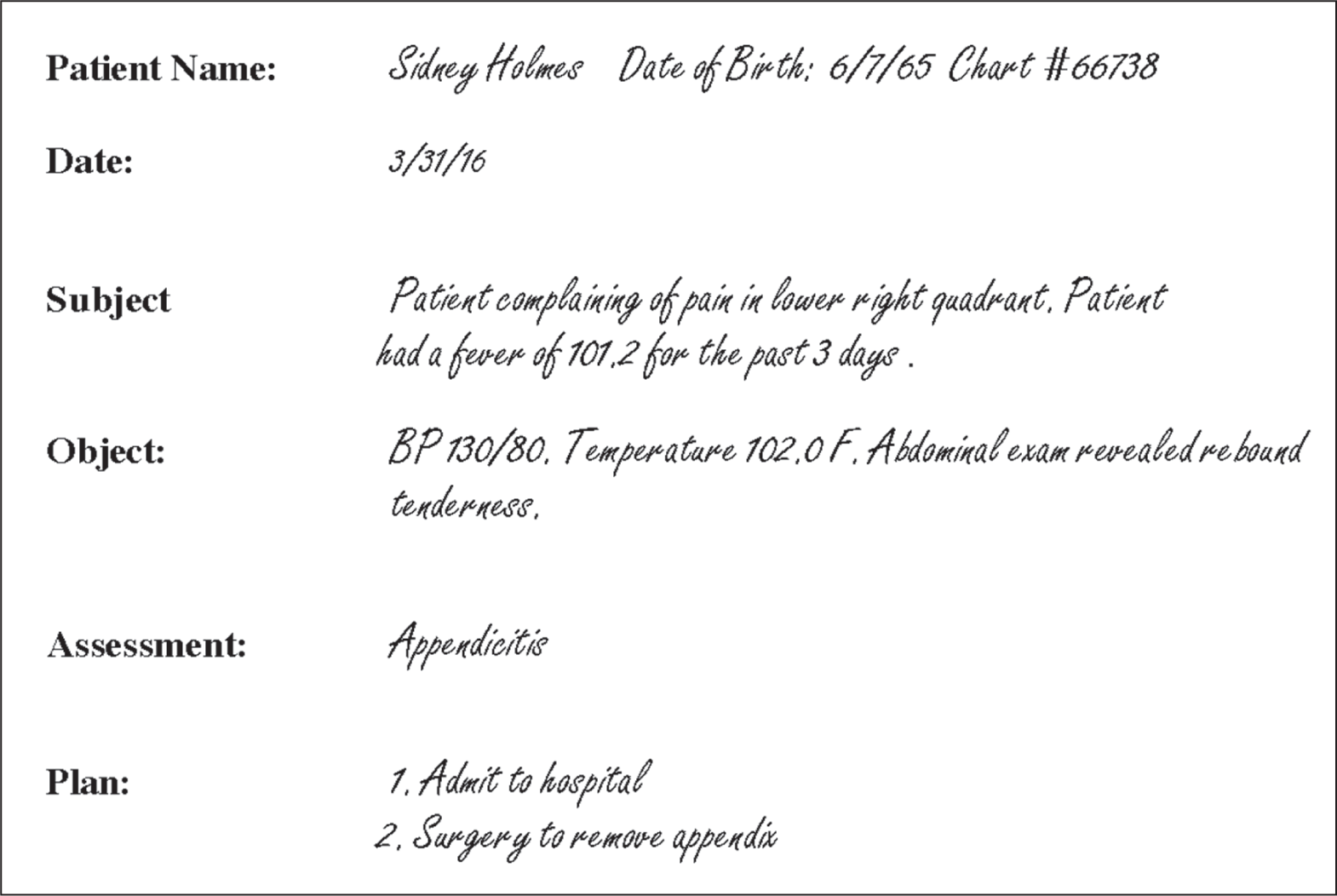
The SOAP approach, which is used in many medical records, gives orderly steps for documentation of clinical information. SOAP is an acronym that stands for the following items:
When documenting in a paper record, it is important to keep it neat, legible, and complete. Never use correction fluid or tape in medical records. If an error is made, cross out the word(s) using one line, make the correction above the corrected word, initial it, and date it.
Record information in the patient’s own words when appropriate, using quotation marks. Do not record your personal opinions, comments, or speculation.
Medical records are legal documents and must be handled accordingly. Patients who see the doctor must have the chart up-to-date and patients who have not seen the doctor in a year can be placed in the inactive file cabinet. Records of patients who are deceased or have moved away should be placed in a closed file cabinet. With the implementation of electronic storage, records can be housed in a system for an indefinite period of time, which relieves the staff from the task of purging files. The medical file belongs to the physician or medical group, but the information in it belongs to the patient. Patients who are changing doctors will request to have their records sent to the new physician. A signed release of records must be obtained prior to transferring the medical record. Federal guidelines recommend retaining medical records for 7–10 years or according to the policy in your practice. If you treat children, records should be retained until the child reaches the age of 21, plus the statute of limitations for adult records. Some physicians do not want the records destroyed and have the inactive charts placed in storage or computerized. When a hard-copy medical record is discarded, it must be shredded or burned.
There are several options for maintaining (physical) patient files. With each type of system, color coding can be helpful.
There are some good practices that are recommended when working with files.
Implementation of electronic health records (EHRs) was included as part of the Centers for Medicare and Medicaid Service's meaningful use requirements. The Health Information Technology for Economic and Clinical Health (HITECH) Act, enacted as part of the American Recovery and Reinvestment Act of 2009, provided $19 billion to fund the adoption of information technology into health care, thus creating financial incentives for physicians, hospitals, and other health care providers to adopt EHRs. The goal of this initiative was to improve the overall health of the U.S. population. Failure to implement EHRs results in a decrease in the reimbursement from Medicare for services performed.
Some of the barriers to full implementation of EHRs include high costs, lack of system integration, and deficiencies in staff knowledge of computer systems. As a medical assistant, you may be part of the effort to implement an EHR, assisting your practice office in the transition to this new and much-improved system of data collection, storage, and retrieval.
At a minimum, EHRs save space and money. By living “electronically,” medical files will be maintained indefinitely and with integrity. Despite some concerns, EHRs are the primary source of patient records in health care today, with numerous software and hardware vendors entering the market.
If you are planning to implement a new EHR system in your practice, first identify the budget available and get input from all staff about their needs. Then, interview vendors and request hands-on demonstrations. Lastly, once a new system has been chosen and implemented, train staff.
One consideration with implementation is how to manage existing patients and their historical information. Some companies choose to go back and enter all patient data from their historical paper files so their entire facility can be electronically based. Others convert patients to EHR as they come into the office. Either way, it is important to train staff properly. Having an electronic record that is easily accessed, fully integrated, and legible is a reminder that the effort is worthwhile.
The benefits and challenges of EHRs are detailed here.