Accurate measurements of the vital signs are a very important part of patient assessment. Vital signs include temperature, pulse, respirations, and blood pressure. They are abbreviated TPR and BP and may also be called cardinal signs. Other measurements called anthropometric measurements may be taken when the patient comes to the physician’s office. These are measurements of height, weight, BMI, body fat composition, and head and chest circumference. While measurements of vital signs are part of every office visit, they must not be considered routine or unimportant. Variation from normal can give important information about the patient’s state of health.
Vital signs can be altered by a number of factors other than illness. Caffeine intake, smoking, medications, emotional stress, eating or drinking foods that are hot or cold, or exercise are just a few factors that can influence a patient’s vital signs. The assessment of the patient’s pain is sometimes called the fifth vital sign. Pain is assessed using a numeric scale from 0 to 10. Zero indicates that no pain is present, while 10 reflects the worst pain the patient has experienced. For those patients unable to understand the numeric scale or to participate in an interview, there are facial expression scales that allow the observer to rate the level of pain based on behavior or facial expression.
| Age | Pulse | Respirations | Blood Pressure |
| Newborn | 120–160 | 30–50 | 60–76/30–45 |
| 1–3 years | 90–140 | 20–30 | 78–106/42–63 |
| 4–6 years | 80–110 | 18–26 | 78–112/50–72 |
| 7–11 years | 75–110 | 16–22 | 85–114/52–76 |
| 12–16 years | 60–110 | 14–20 | 94–130/58–83 |
| Adult | 60–100 | 12–20 | < 120/< 80 |
Temperature can be assessed with a variety of thermometers. Glass thermometers are no longer used according to OSHA guidelines due to the danger of breakage and need to disinfect between patients. Digital thermometers are used frequently and temperature can be measured in the mouth, axilla, rectum, or ear canal. Temporal thermometers are becoming increasingly more popular, as they provide accurate results in a short period of time. The thermometer is rubbed across the forehead from temporal artery to temporal artery, reading the infrared heat that comes off the patient's head. Disposable covers are used to prevent transmission of pathogens between patients. A separate probe is used for rectal temperature and color-coded in red to identify it. Rectal temperatures are the most accurate, but also the most invasive. Rectal temperatures should not be taken in patients with diarrhea, recent rectal surgery, or hemorrhoids, or if the patient is uncooperative. Tympanic or temporal readings are the least invasive but must be performed carefully in order to obtain accurate results.
Disposable thermometers can also be used to obtain body temperature using heat-sensitive material that changes color. These are good screening devices and are accurate if used correctly. Care must be taken to check for expiration dates prior to use. Disposable thermometers and probe covers must be disposed of according to biohazard waste regulations.
Health care providers in the United States use both Fahrenheit and Celsius (metric) measurement systems. Medical assistants must be familiar with conversion formulas in order to interpret and assess the observed results.
| °F to °C | Subtract 32, then multiply by 5, then divide by 9 |
| °C to °F | Multiply by 9, then divide by 5, then add 32 |
| Normal body temperature | 98.6°F = 37°C |
| Autoclave temperature | 250°F = 121°C |
| Incubator temperature | 95°F = 35°C |
| Refrigerator temperature | 41°F = 5°C |
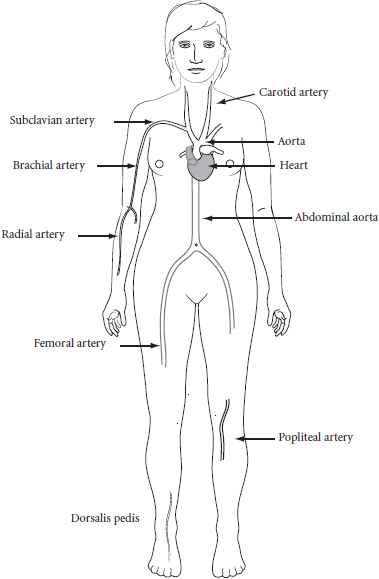
Pulse rates are the count of the palpable beats against the walls of the arteries. There are several areas in the body where the pulses can easily be palpated.
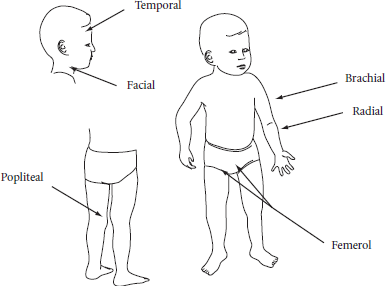
Respirations are measured as the complete cycle of inspiration and expiration being counted as one. The respiratory rate is controlled by the brain, but the individual can control the respiratory rate to some degree. For this reason, you should not inform the patient that you are counting his respirations during the procedure as to not affect the rate. Respirations may be counted by observing the rise and fall of the chest or by feeling the rise and fall by placing your hand on the chest or back of the patient. Observation can be done at the time that the pulse count is being done by continuing to keep the fingers on the pulse, remembering the pulse count, and then counting the respirations. The respirations can also be counted during the patient interview as you observe the patient. In an infant or a small child, both the pulse rate and the respirations may be counted by auscultation of the chest while the parent holds the child on their lap.
Careful evaluation of the blood pressure with comparison to previous readings is very important in evaluation of the patient. Comparison readings give information about changes in condition and effectiveness of medications. Changes in the blood pressure may indicate problems with the cardiovascular and other body systems. Hypertension is a serious health problem that does not have overt symptoms in the early stages except for elevated readings when the blood pressure is checked. The American Heart Association expanded upon the definition of hypertension by lowering the acceptable normal BP reading and by identifying individuals with systolic BP of 120–139 and/or diastolic BP of 80–89 as prehypertensive. Care must be taken to use correct technique and equipment when checking the blood pressure readings and recording them in the chart.
The arm should be at or about heart level and resting comfortably when the reading is taken. The cuff must be the correct size. The cuff should be checked for any defects and for correct calibration prior to using. The arterial markings should be used to make sure that it is applied to the arm correctly. If the reading is not what you expect it to be, you should ask the patient about medications taken, caffeine intake, or stress situations that may be affecting the reading. Never hesitate to have another practitioner in the office check the reading if you have any doubt about your results.
Heart sounds: Sounds heard when the blood pressure is measured are called heart sounds or Korotkoff sounds. These sounds are classified into five phases:
Blood pressure readings that are very weak or faint can be measured by palpation or by use of a Doppler device. In this case, there is only an initial systolic reading available and the blood pressure should be recorded as the systolic number over P for palpation or D for Doppler.
Height and weight are normally measured at every physician visit. These are very important measurements and must be carefully calculated and recorded in the patient chart. Results are measured in feet, inches, pounds, and ounces or in the metric system using kilograms and centimeters. You should be able to convert between the two systems to interpret results. Remember that 1 kg equals 2.2 lbs.
Weight should be measured in an area that ensures some privacy. Many people are sensitive about their weight and do not want to be weighed publicly or have the results of the measurement announced where others could overhear. Shoes may be taken off or not as the patient prefers, but if weight is done without shoes, measures should be taken to prevent transmission of pathogens to the surface of the scale, which could be passed on to the next patient.
Height is another important measurement that is taken at each office visit. In children, this measurement gives information about normal growth and development. In older adults, it can indicate bone loss with aging. Measurements are taken by using a ruler-type device attached to the scale or attached to the wall of the office.
Once height and weight are obtained, you can also calculate and record the BMI or body mass index of the patient. With obesity becoming a problem in all age groups, this measurement is used more often for evaluation. You can calculate the BMI by using a formula, online calculator, or app.