The purpose of the physical examination is to determine the state of health of the individual and to evaluate health problems. A diagnosis is then made by the physician and a plan of care is developed. Testing and medication may be ordered. Follow-up is scheduled to evaluate the results of treatment.
Your role as the medical assistant in the physical examination includes the following steps:
Several screening exams can be done in the physician’s office. While not complete exams, they may point out areas that need further investigation.
Visual acuity is performed with a Snellen chart to measure distance vision. The Snellen chart uses predetermined numbers that indicate the distance from which an individual with normal vision can see a particular line of letters. For testing, the patient stands 20 feet from the chart. The patient covers one eye and reads the lowest line possible. Normal vision is expressed as 20/20 and is considered normal for an individual viewing a particular line of the chart from 20 feet away. The results are recorded as a fraction. For example, in the fraction 20/60, the first number denotes that the patient was standing at 20 feet and the second number is the distance an individual with normal vision could view those same images. Pictorial eye charts are used to test vision of children and nonreading adults. Both eyes are tested independently and then together. The patient should be given an eye shield to prevent squinting while reading the chart. If the patient wears corrective lenses, the testing can be done with the corrective lenses. Modified charts are available for patients who cannot read and for children. If the patient’s vision at maximum correction is 20/200 or greater, the patient is considered legally blind. The results should be recorded in the chart and carefully labeled.
Near vision testing can also be done using a chart that approximates the size of print in several different types of reading material. The chart is held about 14 to 16 inches away.
Colorblindness is mainly an inherited condition, and it occurs 20 times more often in males than females. Inheritance is sex-linked, meaning that the defective gene resides on the X chromosome, so females can carry the gene for colorblindness without ever developing the condition. The most common deficiency is red/green colorblindness, but there are other forms in which yellows and blues are distorted or the patient perceives only black and white. To evaluate color vision, illustrations such as the Ishihara color system are used. This system contains numbers or symbols made up of colored dots that appear among other colored dots. The patient is asked to identify what item is seen. A patient who is colorblind is unable to see the number or symbol within the colored dots. To test, you will need to have the patient trace the pattern that they see using their finger. In the chart, you will document how many patterns the patient is able to distinguish.
Evaluation of hearing can be done using audiometer or tuning-fork testing in the office. The Weber test is done to test if hearing is better in one ear than the other. The audiometer measures the sound intensity in decibels (dB) and the tone in cycles per second (cpc) or hertz (Hz). The patient is asked to indicate when they hear a tone, usually by raising a hand. A tuning fork is struck on the palm of the hand to facilitate vibration. The tuning fork is then placed on the center of the head and the patient is asked if there is a difference in the sound in one ear or the other. The tuning fork can also be used to compare bone conduction with air conduction. This test is called the Rinne test. The tuning fork is made to vibrate and then placed on the mastoid process. When the sound disappears, the tuning fork is turned to the front of the ear canal and the sound will normally still be able to be heard.
Tympanometry is a noninvasive procedure designed to evaluate the mobility of the eardrum and ascertain middle ear function through inducing air pressure variations into the ear canal. It is not a test of hearing and should not be confused with audiometry. This test is often used to screen tympanic membrane function in infants and small children who would be unable to complete audiometry and assist in diagnosing otitis media. Tympanometry also aids in diagnosing sensory or conductive hearing loss.
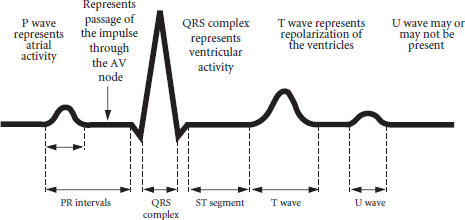
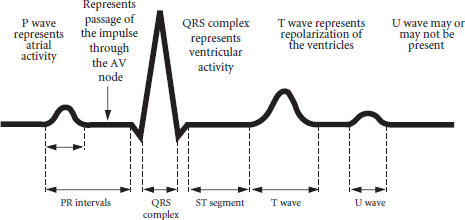
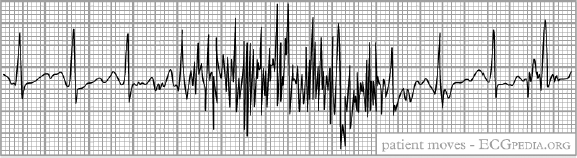
An electrocardiogram (EKG) is a visual picture of the electrical activity of the heart created by placing electrodes on the body. Ten electrodes are placed, six on the chest and one on each limb. Each electrode, or lead, presents a picture of the electrical activity at its particular position on the body. Positions are identified as bipolar, augmented, unipolar, or precordial. Care must be taken to place the electrodes precisely and make sure they are attached securely. It may be necessary to remove hair or otherwise prepare the skin to make sure that there is good connection to the skin. Other things that can interfere with recording are patient movement, tremor, talking, and electrical interference.
The EKG machine uses specialized paper that is heat and pressure sensitive. It is marked in 1-mm squares, which are also marked in groups of five by five squares. In normal mode, the paper will move through the EKG machine at 25 mm per second.
| Lead | Polarity | Electrical Conduction Location |
| I | Bipolar | Left arm/right arm |
| II | Bipolar | Right arm/left leg |
| III | Bipolar | Left leg/left arm |
| AVR | Augmented | Midpoint between the left arm and left leg to right arm |
| AVL | Augmented | Midpoint between the left leg and right arm to left arm |
| AVF | Augmented | Midpoint between the left arm and left leg to the left foot |
| V1-V6 | Unipolar | See Figure 11.5 above |
Terminology. It is important for the medical assistant to know common terminology related to EKGs in order to support patient education and document information accurately.
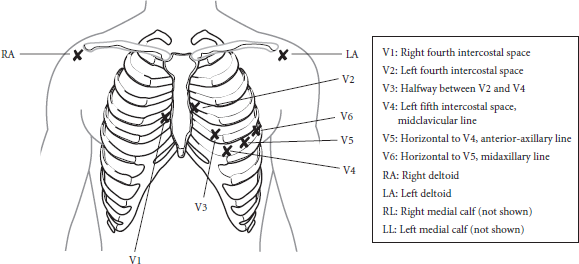
Artifacts. Artifacts are unwanted disturbances that can interfere with accurate interpretation of an EKG tracing. Machine malfunction, body movements, electrical interference, or poor contact of the electrodes can lead to artifacts. The medical assistant needs to know what these artifacts are and how to troubleshoot them in order to produce a clear EKG recording for interpretation by the health care provider.
Body movements cause an EKG tracing artifact known as somatic tremor. Sources of somatic tremor include shivering, coughing, sneezing, talking, and moving, as well as disorders that cause uncontrollable movement, such as Parkinson’s disease. It is important that you properly instruct the patient to limit movement during the procedure, ensure the patient stays covered and warm, and (if needed) have the patient slip their hands, palms down, under the buttocks. These measures tend to promote relaxation and reduce somatic tremors.
Alternating current (AC) interference is caused by improper grounding or by a machine that is not equipped to filter out extraneous electrical currents. A tracing with AC interference will have a thickened appearance, with relatively even, sharp spikes. To reduce electrical interference, confirm that the ground wire on the right leg is attached appropriately and that the EKG machine has a three-pronged outlet connector, and move the patient away from the source of electricity (for instance, walls with electrical wiring or other electrical equipment in the room). Note that if a total break in the tracing, the likely problem is a broken lead wire or loss of connection of one of the electrodes.
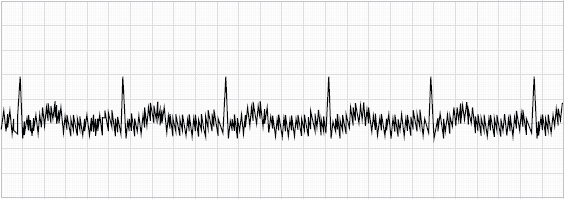
Poor lead contact with the skin produces a wandering baseline in the EKG tracing. In this artifact, the baseline “wanders” up and down on the EKG paper, interfering with accurate recording. Possible sources of wandering baseline (sometimes called “baseline drift”) include lotions, powder, oils, or ointments on the client’s skin; nylon stockings that the client is wearing (stockings should be removed along with the client’s other clothing prior to EKG testing); and expired or poor-quality electrolyte gel, dry electrolyte pads, or dirty/loose wires or electrodes. Wiping the attachment areas with alcohol to ensure that the skin is clean and dry will often reduce this unwanted tracing artifact. A related artifact that may be seen is an interrupted baseline, in which there is a sharp break in the tracing. This artifact is typically seen when a wire is broken or a lead becomes disconnected.

There are a variety of positions that facilitate patient examination. You must be able to instruct the patient on how to assume the correct position and assist him with the positioning. You will then drape the patient in a manner to maintain dignity and privacy while allowing the physician to do the examination. If it is necessary for the patient to wear a gown for the examination, you must be sure that it fits correctly and is in good repair. If the gown is disposable, it is used for one patient only and then discarded in the appropriate waste container. The exam table should be cleaned with disinfectant and covered with clean paper prior to the patient entering the exam room. The exam table should be checked periodically to make sure that all features are in good working order and the covering is intact.
The primary purpose of draping is to provide the patient privacy and dignity. Only the parts being examined should be exposed. A blanket should be available for the patient to keep him warm and comfortable. The medical assistant should be available to assist the patient in assuming positions on the exam table and to prevent falls.
In an erect position, the patient is standing. This position is used for evaluation of gait and neurological testing. No draping is needed. If the patient is wearing a gown for this position, make sure that is it secured for dignity and privacy.
In a sitting position, the patient sits on a chair or on the edge of the exam table. This position can be used for a number of examinations including the nervous system, head and neck, lower extremities, chest, upper extremities, and the back. Draping may be necessary to cover the lower extremities for patient comfort.
The supine position, also called horizontal recumbent, is when the patient is lying flat on the back with arms at the sides. This position can be used to assess the chest, breasts, abdomen, heart, and extremities. It is also the position of choice if the patient experiences syncope (that is, the patient has fainted). Draping is done from under the arms downward.

In the dorsal-recumbent position, the patient is supine with the legs bent at the knees and feet flat on the exam table and spread about shoulder width. This position can be used to examine the abdomen, genital, and rectal areas. It may be more comfortable than the supine positions for patients with back or abdominal pain. Draping is done in a diamond fashion with a point facing toward the head and the feet. The points that extend to the sides can be positioned to wrap around the legs when the patient is being examined.

The lithotomy position is similar to the dorsal-recumbent, except that the feet are placed in stirrups. This is done for vaginal exams, pap smears, and pelvic exams and procedures. Draping is done in the same manner as the dorsal-recumbent position.
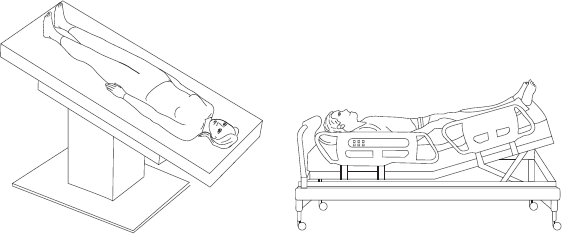
The patient is positioned with the head lower than the feet in the Trendelenburg position. It is used for shock or to delay a precipitous delivery. Draping is done from the shoulders downward. Alternatively, the modified Trendelenburg position may be used, in which the feet are elevated 45 degrees and the head remains level with the rest of the body. Research has shown that cardiac output does not improve significantly when using the Trendelenburg position, and it may adversely increase intracranial pressure. Therefore, this position is only used in extreme situations.
Sims’s position is also called the left lateral position and calls for the patient to be on his left side with the left arm behind the body and the right arm in front of the face. The legs are flexed; the right more than the left so that access to the rectal area is exposed. This position is used for enemas, suppositories, rectal temperature, and rectal exams. It may be used for proctologic exams in those patients who cannot tolerate the knee-chest position.
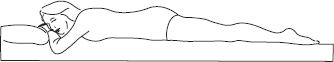
In the prone position, the patient lies flat on the abdomen with neck turned to one side. Arms are down by the side. This position is used to examine the spine, back, and lower extremities. The patient is draped from the mid-back downward.

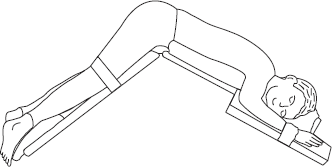
In knee-chest position, the patient is positioned on the knees with the head and chest on the table and the buttocks elevated. This position may be assumed with or without the use of a special table. It is used for rectal exams and proctologic exams and procedures. This position is difficult to assume for a large patient or an elderly patient. You should stay by the patient’s side and assist the patient when moving out of this position to prevent falls. Orthostatic hypotension may be a problem after assuming this position for a period of time. Draping is done to cover the buttocks.
The “jack-knife” position is used for surgical procedures involving the rectal area.
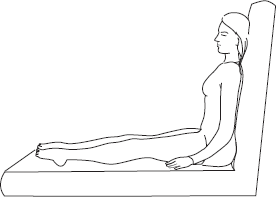
When in Fowler’s position, the patient is sitting at a 90-degree angle with lower extremities elevated. The table supports the back. It is used for examination of the chest, head, and neck. It may also be used for someone who has problems breathing in a flat position. Draping is done from the mid-chest downward.
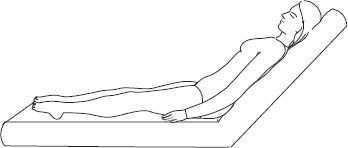
Semi-Fowler’s position is similar to Fowler’s position, but the head is elevated at a 45-degree angle. It is used for the same procedures in which Fowler’s position is used and draping is the same.
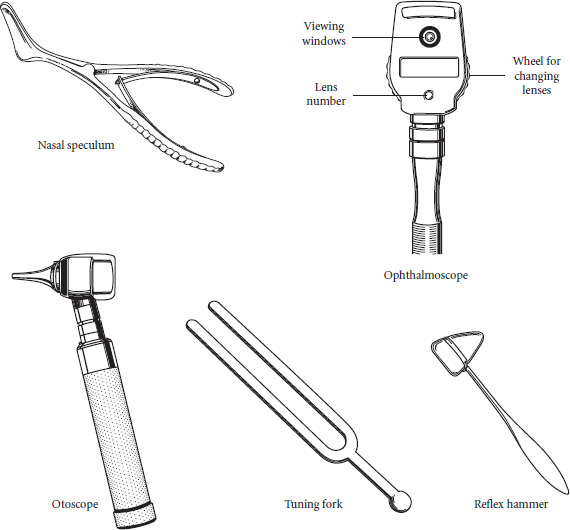
Otoscope and ophthalmoscope: used to examine the ears and eyes. Disposable covers should be used prior to examining the ears with the otoscope. These instruments may be handheld or wall-mounted. If they are portable, you must make sure that they are fully charged and ready to use.
Nasal speculum: dilates the nares for examination of the internal structures
Tongue depressor: a flat wooden stick used to depress the tongue for examination of the throat
Reflex hammer: a small hammer with a rubber head used to test reflexes in a neurological examination
Tuning fork: used to test for bone vibration and auditory acuity
Stethoscope: used to take blood pressure and listen to the heart, lung, and abdominal sounds
Gloves: disposable exam gloves of various sizes
Lubricant: a water-soluble lubricant available to be used for rectal or vaginal exams
Hemocult cards and developer: to check stools for blood after a rectal exam
Tape measure: disposable paper measures can be used to measure body parts, wounds, areas of skin rash or excoriation, ulcers, and other areas of the body
Other objects that should be available are gauze sponges, waste containers, specimen containers with labels, plastic bags with biohazard labeling for specimen transport, culture tubes, cotton applicators, and any other supplies that are relevant to the physician practice or exam being done.
You must protect yourself while caring for and moving patients and equipment. Learning and practicing proper lifting and moving techniques may help prevent injury. You must also make sure that equipment in the office is in proper working order. That will include the exam table, scales, wheelchairs, and other equipment used for patient care.