Medication Administration
To safely administer medication in the office, the medical assistant must follow a series of routine procedures. Medications should be prepared in a quiet and well-lit environment. Always make sure that you go through all the steps of drug preparation no matter how busy the day is. Shortcuts will not save time and may lead to a medication error. Make sure that the medication order you are filling is complete and legible. If you are in any doubt, double-check with the prescribing provider. Be sure to check the patient’s allergies for any interaction with the ordered medication. Make sure that you check expiration dates on the medication labels prior to administration. Never substitute any medication without instruction from the physician. Always prepare the medication immediately prior to administering it and never ask anyone else to administer medication that you have prepared or administer medication that you have not prepared yourself. Patients should be observed for at least 20 minutes after a new medication is administered, unless ordered differently by the physician. In order to safely administer medications, the medical assistant should be familiar with and practice the Six Rights of Medication Administration:
- The right patient: identify the patient using two identifiers such as name and date of birth
- The right drug: check medication with the order three times when preparing the medication for administration. First check the medication when you have obtained it, then as you are preparing the dose for administration, and finally right before you administer to the patient.
- The right dosage: check for an appropriate dosage for the patient and if you have to perform calculations in order to prepare the medication, make sure you check your calculations with another person.
- The right route: how the medication is to be delivered
- The right time: usually given immediately in the office setting, but must be checked prior to administration
- The right documentation: immediate and complete documentation of all the details about the administration and patient tolerance of the medication
When administering medications to children, you should involve the caregiver if necessary. Explain the medication to the child and attempt to gain cooperation. Offer the child choices if possible. Do not make promises that you cannot keep such as, “This won’t hurt.” If you have to restrain the child
to administer the medication, make sure that the child is safe and that adequate assistance is available. Do not scold the child for failure to cooperate; acknowledge that the child is scared. When the medication has been given, offer a reward and encouragement even if the child was not cooperative with the procedure.
Geriatric patients are also likely to have some special needs when it comes to medication administration. They are most likely to have multiple physicians and to take over-the-counter medications and home remedies in addition to prescription medication. You must have a complete list of all medications that they are taking from all physicians and include questions about other nonprescription items they use when taking the patient history. Update the medication list every time the patient comes into the office to ensure the list is correct. If a family member accompanies the patient, he should be educated also about medication schedules, and instructions should be written down and sent home with patients.
The patient should be encouraged to drink adequate fluids. If there is a problem in swallowing medications, check to see if the medication could be crushed and placed in food for administration. Patients should be encouraged to discard medications that they are not currently taking to prevent confusion or taking the wrong medications. If elderly patients are taking a lot of medications, they may benefit from a medication-dispensing system that can be filled by family or a visiting nurse on a weekly basis.
Drug Forms
Oral administration of solid forms includes pills, caplets, gelcaps, spansules, powders, tablets, capsules, and lozenges. Some medications are enteric coated so that they are not dissolved in the stomach, but in the small intestine. This is to prevent stomach upset or irritation. Tablets and pills should not be split in pieces unless they are scored and this should be done with a device in order to cut them equally. Some tablets can be crushed in order to administer to patients that cannot swallow, as long as the tablets are not coated or sustained release. Capsules are coated with gelatin and dissolve within the digestive system. Some capsules have smaller capsules within them that are coated to be dissolved at different times so there is a sustained release of medication. Lozenges are made to dissolve in the mouth to coat the mouth, throat, or upper part of the digestive tract. Oral medications can also be given in the liquid form. There are several different types of liquid medications available. The most common include:
- Syrups: solutions of medication with sugar and water with a flavoring
- Elixirs: solutions of medication with alcohol, sugar, water, and a flavoring
- Suspensions: mixtures of insoluble drugs in liquid; the drug does not dissolve in the liquid, so the mixture must be shaken well prior to administration (includes emulsions and gels)
- Solutions: liquid preparations of one or more medications that are dissolved in a liquid
Oral medications should be given with a sufficient supply of water unless ordered otherwise. When administering oral medications, you must stay with the patient as they take the medication and verify that the medication has been swallowed. Liquid medications can be measured out into a medicine cup or in a syringe.
Parenteral medication forms are injectable medications. They must be sterile and are often provided in sterile water or normal saline. Some medications that are released slowly are supplied in an oil base. Prior to administration of parenteral medications, you must check the expiration date of the medication. The medication must be examined closely to check for any discoloration or sediment in the medication. You must also follow all OSHA standard precautions guidelines when administering parenteral medications. Parenteral medications are supplied in many different forms. An ampule is a small glass vial that contains a single dose of medication. Ampules are scored at the neck and broken prior to use. Single-dose vials are small vials with rubber stoppers that deliver one dose of medication. Before removing medication from the vial, you must first clean the stopper carefully with alcohol. Multi-dose vials are vials with rubber stoppers that contain more than one dose of medication. You must be very careful not to contaminate the remaining medication in the vial when withdrawing a single dose. If you have any doubt as to the integrity of the remaining medication in a vial, discard it and use another.
When you remove medication from a multi-dose vial, you should inject air in the same amount that you are going to withdraw as fluid. A prefilled syringe will contain one dose in a disposable syringe. Often the syringe will be attached to a plunger mechanism that is reusable, and a disposable needle may be attached if the syringe does not come with a needle attached.
It is important to know what type of medication and the preferred area of injection to use when determining which syringe and needle type you need. Syringes vary from 0.5 mL to 60 mL. You should use the smallest appropriate syringe for the injection you are going to administer. Syringes are available marked in units in order to administer insulin.
To administer small amounts of intradermal medications, 1-ml syringes are marked in 0.1 increments. The needle gauge must be appropriate for the medication that you are administering. The larger the gauge of the needle, the smaller the diameter of the needle is. Needle gauges range from 28 to 14. The smallest gauges are used for intradermal injections. The 25 and 26 gauges are commonly used for subcutaneous injection. The 20–23 gauge needles are the usual size for intramuscular injections, with the larger gauges used for thick or oil-based medications.
Needle length is based on the area where the medication is to be delivered and the size of the patient. The range is from
 inch to about 3 inches. Intradermal injections use the shortest needles. For subcutaneous injections, the needle length should be about
inch to about 3 inches. Intradermal injections use the shortest needles. For subcutaneous injections, the needle length should be about
 to
to
 of an inch. Intramuscular injections should use the longest needles, and needle length should correspond to the site being used and the size of the patient.
of an inch. Intramuscular injections should use the longest needles, and needle length should correspond to the site being used and the size of the patient.
Some medications have their own delivery method. Insulin injectors have been developed to reduce the need to use a syringe and needle each time to draw up a dose of insulin. These injectors can be set to administer the correct amount of insulin with the turn of a dial. They resemble a pen and can be easily carried in a shirt pocket. They are ideal for diabetic patients who must inject themselves with insulin frequently. The Epi-pen is also available to self-administer epinephrine for patients who have had anaphylactic reactions to allergens in the past. The dosage is ordered by the doctor and carried by the patient in the case of an emergency.
There are similarities to administering any type of injection. Once again, you must be sure to use the Rights of Medication Administration when preparing the medication and administering it. Additionally, you must pick the injection site and prepare the skin. Using standard precautions and wearing gloves along with aseptic preparation of the medication and safe disposal of the syringe after administration are very important. Alcohol is the most common antiseptic used and the site of the injection should be swabbed from inside to outside and allowed to dry without blowing or fanning prior to giving the injection. After the injection is given, unless contraindicated, the site should be massaged to facilitate absorption and the patient should be checked for bleeding and a bandage applied. When giving an injection to a small child, you should have assistance to make sure that the child does not move during the injection. Never promise that the injection will not hurt the child. There usually will be some discomfort and you will lose the trust of your patient.
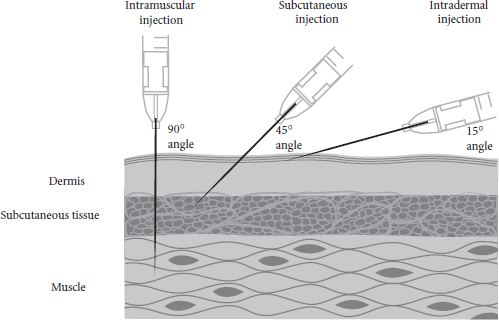
Giving an intradermal injection is accomplished by depositing the medication just under the epidermis. It is usually given in the forearm, upper back, or upper chest. When correctly administered, a raised white wheal will appear at the site of the injection. The needle should be inserted at a 15-degree angle and so the bevel is visible below the layer of skin. The medication is then injected. This method is used to perform the Mantoux test for tuberculosis and for allergy testing.
Subcutaneous injections are given in the subcutaneous layers underneath the skin, but above the muscle. The needle is inserted at a 45-degree angle. The most common drugs given in this manner are insulin and heparin. Insulin injections should be rotated between sites so that tissue damage is minimized to prevent problems with drug absorption. An injection site log can be kept
to make sure that the sites are rotated. Heparin is commonly administered in the abdomen. When administering heparin and insulin, you should not aspirate prior to injection and you should not massage the area after administering heparin to prevent bruising in the tissues.
Intramuscular injections are given in large muscles in the body. In the adult, the preferred sites are the dorsogluteal, the vastus lateralis, the ventrogluteal, and the deltoid muscles. In children, the vastus lateralis is the preferred site. You must make sure that the needle that you have selected to give the injection is long enough to deliver the medication to the muscle. The historical process of aspirating prior to injecting has been revised; since there are no major blood vessels located in sites where toxoids and vaccines are administered, aspiration is no longer necessary. In addition, aspirating can result in unnecessary pain during injection, especially in infants and small children.
Medications that are meant to be given in the muscle tissue may not adequately be absorbed if injected subcutaneously. IM injections should be given at a 90-degree angle, except in the vastus lateralis in small children. These should be given at 45 degrees.
Some medications that are given intramuscularly can be damaging to the subcutaneous tissues. They are given in the Z-track method to prevent leakage of the medication out of the muscle. This is accomplished by pushing the tissue to one side prior to inserting the needle, administering the injection, and then allowing the tissue to slide back into its original position once the needle has been removed. The Z-track method should only be used in large muscles.
Dosage Calculations
When preparing medications, it may be necessary to calculate dosage. The medical assistant should have a basic knowledge of the commonly used measurements in drug preparation. You should be able to convert between the systems of measurement, such as between ounces and pounds. Any calculations that you have to do
to administer the medication should be double-checked with a coworker prior to administration. The most common method to use to calculate the dosage uses a formula into which information about the medication is applied:

This formula sets up a proportion in which you can insert the information you have available to you to calculate correct dose.
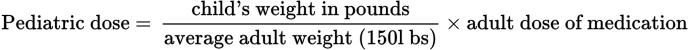
To administer medication to children when the adult dose of the medication is known, you can use Clark’s Law. Clark’s Law assumes the weight of the adult as 150 pounds.
Household
Measurements
Although
household measurements are the least accurate of all the measuring systems, they
are often used to instruct patients on how to administer medications because these
measures are typically accessible in the home. The medical assistant’s explicit
instructions are important in ensuring accurate dosage of medication.
The most common household equivalents that you should be
familiar with are identified here. You should memorize these equivalents, as your dosage
calculations will be much easier and you will be better equipped to instruct
patients appropriately:
- 30
mL = 1 ounce (oz)
- 240
mL = 8 ounces (oz) = 1 cup
- 5 mL
= 1 teaspoon (tsp)
- 15
mL = 1 tablespoon (tbs) = 3 teaspoons (tsp)
- 1
kilogram (kg) = 2.2 pounds (lb)
 inch to about 3 inches. Intradermal injections use the shortest needles. For subcutaneous injections, the needle length should be about
inch to about 3 inches. Intradermal injections use the shortest needles. For subcutaneous injections, the needle length should be about
 to
to
 of an inch. Intramuscular injections should use the longest needles, and needle length should correspond to the site being used and the size of the patient.
of an inch. Intramuscular injections should use the longest needles, and needle length should correspond to the site being used and the size of the patient.