11.1 Introduction
Atopic dermatitis (AD) (aka eczema) is a common inflammatory skin disorder of variable severity, characterized by pruritus and a chronic, relapsing course. It is associated with other atopic disorders, such as asthma, food allergy, and allergic rhinoconjunctivitis. Moderate to severe AD significantly affects the health, quality of life, and emotional well-being of adolescent patients.
11.2 Epidemiology
Childhood AD may persist or reemerge in adolescence. The prevalence of AD in the 13–17 age group in the United States is estimated to range from 7% to 8.6%, with up to one-third suffering from moderate to severe disease [1]. It affects all ethnic groups.
11.3 Clinical Findings

Inflamed eczema with weeping and crusting

Chronic atopic dermatitis with lichenification and dyspigmentation

Circular eczema lesion with mild erythema and scale
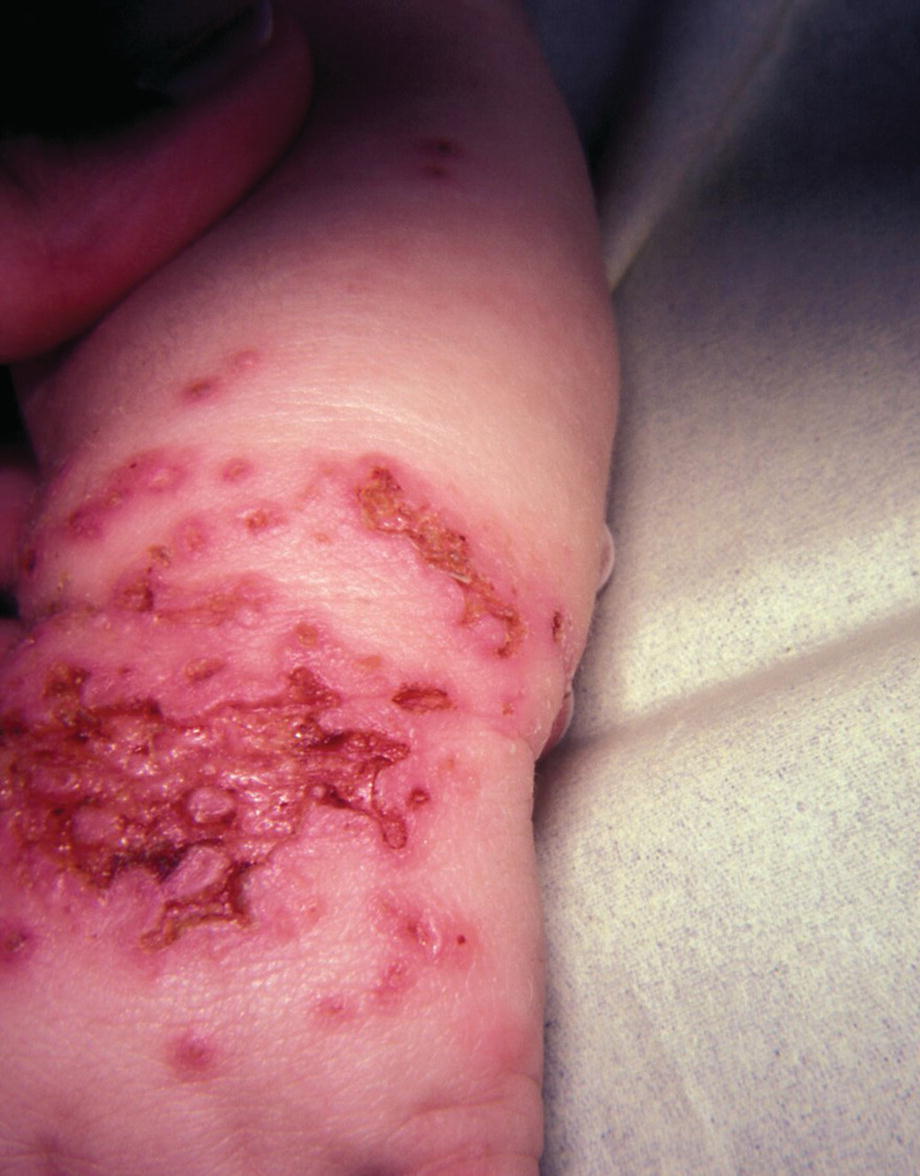
Eczema herpeticum: infection of an area of eczema with herpes simplex virus
11.4 Laboratory
Atopic diagnosis is a clinical diagnosis. Laboratory investigation may be indicated to investigate comorbidities. Skin cultures and viral studies are needed to identify secondary infections.
11.5 Treatment
Basic treatment of AD consists of avoidance of irritants, hydration of the skin by bathing and application of emollients, and judicious use of topical steroids. Topical calcineurin inhibitors are helpful for chronic dermatitis but are not suitable for acute flares. Secondary infection requires treatment with an antibiotic or antiviral medication.
Whereas treatment of mild AD is straightforward, moderate or severe AD in adolescents can be very challenging to manage. Teenagers are particularly susceptible to developing striae from application of topical steroids. Adherence to a topical treatment regimen may be difficult, and emotional distress and discouragement are common. It is necessary to determine a treatment plan that is safe and acceptable to the patient. Psychosocial support is important.
Oral steroids are only rarely justified as short-term therapy for generalized acute AD flares. Systemic anti-inflammatory agents for severe AD include low-dose weekly methotrexate, cyclosporine or azathioprine. Dupilumab, a human monoclonal antibody targeting the IL-4 receptor alpha subunit, has been shown to significantly improve AD signs and symptoms and quality of life in adolescents with moderate and severe AD [1].
11.6 Prognosis
The prognosis is very variable. Many patients show improvement with time. Others continue to suffer from eczema into adult life.