1.1 Introduction
- 1.
Androgen-mediated stimulation of sebaceous gland activity
- 2.
Abnormal keratinization resulting in follicular plugging (comedone formation) in the pilosebaceous unit (PSU)
- 3.
Proliferation of Cutibacterium acnes (formerly Propionobacterium acnes) in the follicle
- 4.
Inflammation.
1.2 Epidemiology
Acne vulgaris is the most common skin disorder in the United States. Acne can be noted at any age; however, adolescence is by far the most affected age group. Greater than 80% of adolescents have acne vulgaris lesions.
1.3 Clinical Findings

Open comedones of the posterior neck
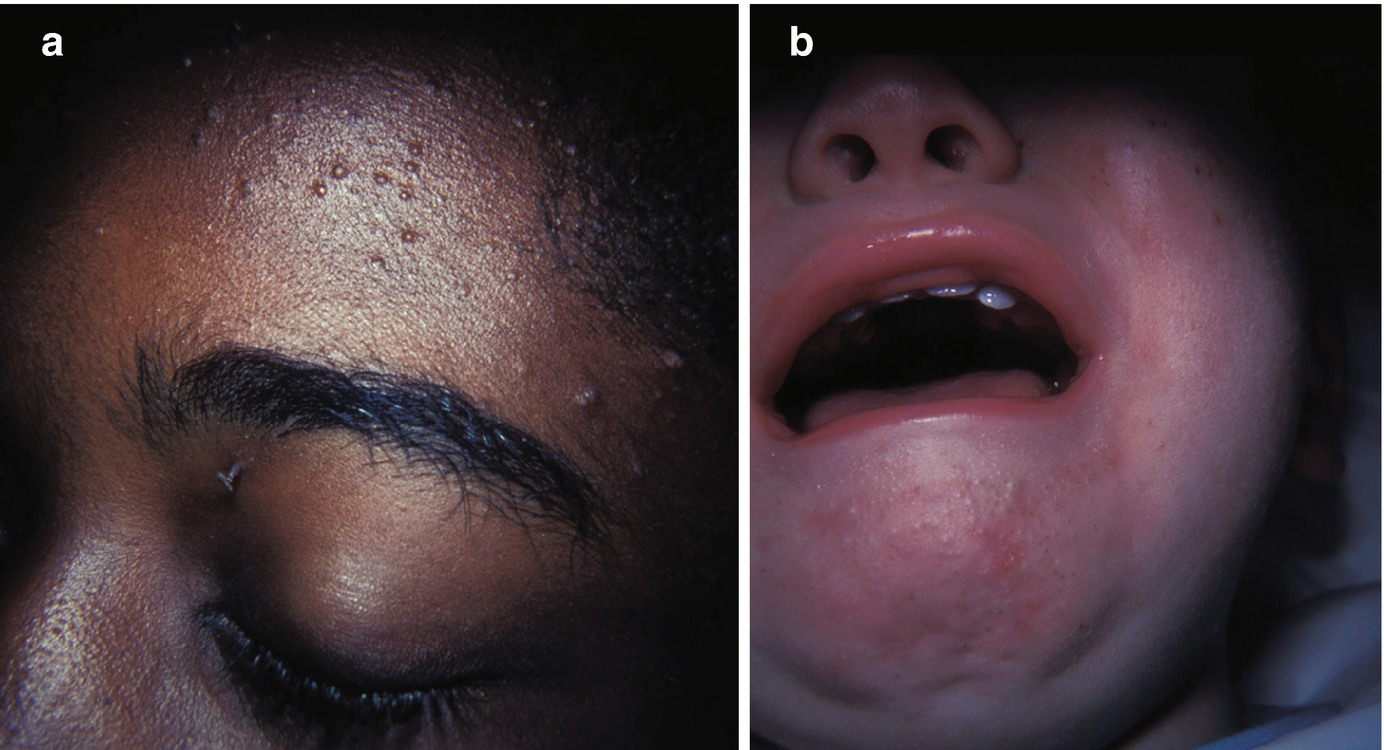
(a) and (b) Closed comedones of the forehead and chin

Acne papules and nodules with some scarring

Acne lesions of the back
1.4 Laboratory
Diagnosis is most often made based on clinical findings. No laboratory test is pathognomonic.
1.5 Treatment
This publication is not conducive for a comprehensive discussion of all available acne treatments. A summary will be provided and the reader is referred to the references below for guidelines for treatment options including algorithms, mechanisms of action, and side effects.
Many patients have already used OTC products when they arrive at the office. Nonprescription recommendations include gentle cleansing, use of non-comedogenic moisturizers and sunscreen, avoiding occlusion, and frequent pillow case changes.
Topical retinoids
Topical salicylic acid, benzoyl peroxide, topical antibiotics, and dapsone gel
Systemic antibiotics
Hormonal therapies
Oral isotretinoin
1.6 Prognosis
Prompt treatment of acne can minimize long-term scarring. Post inflammatory hyperpigmentation (PIH) (especially in skin of color) is typically bothersome. PIH can be treated in addition to meticulous sun protection.