SEVEN
Sweet Dreams Are Made of This

MY PARENTS WERE PLENTY HOT FOR EACH OTHER, but they just couldn’t make it work in the domestic sphere. They met in Chicago in the early 1950s, when my mother was a teacher at a school for special-needs kids and my father was a medical student. He was doing a clinical rotation in pediatric neurology and was visiting my mother’s school together with the attending physician. They locked eyes across the room, met for a drink later, and were married a few months after that. But domestic bliss did not ensue. Within a year they were divorced, and both had moved from Chicago—she to New York City to work in publishing and he to Los Angeles to do a residency in psychiatry. After a few years apart, he called her on the phone and implored her to give it another try. He must have been persuasive, because she moved to Los Angeles and they were soon married for a second time. And then divorced again.
You might think that’s the end of this particular love story. Though twice divorced and living apart, they just couldn’t keep their hands off each other. One day when I was twelve, I was in the car with my mom, driving down Sepulveda Boulevard, a gritty, charmless commercial street in West Los Angeles. “You see that hot pillow joint over there?” she said. “That’s where you were conceived, back in 1961. In a motel bed with a coin-operated Magic Fingers attachment.1 Afterward, your father and I joined your Aunt Felice and Uncle Alan for dinner.”
That’s how I became an atypical child of divorce. My parents were indeed double divorced, but only before I was even conceived. There was no childhood divorce trauma for me. Living with mom on school days and with dad on weekends was all I ever knew. And it was just fine. They were both attentive, loving parents, and I never wished for a more conventional family situation.
I never saw my parents living together, but, based on their habits, I can’t imagine a more ill-suited couple. He was messy and she was a neatnik. She loved to cook but he preferred restaurants. She was supersensitive to background noise and he liked to monitor the news on the TV or radio. She didn’t even own a TV until 1974, when she bought one to watch Nixon resign. I can’t imagine them sharing a household.
I’ve often wondered if many small differences in lifestyle can accumulate so that a couple just can’t live happily together, even if things are otherwise OK. In my limited view, the traits that most separated my parents, and held the greatest potential for discord, had to do with time. My dad was a night owl while my mom was usually in bed by 9 p.m. and rose with the lark at 5 a.m., even on those days when she didn’t need to go to work. She was early to every appointment, while he ran notoriously late, annoying her to no end. Now, it may well be that even if their internal clocks had been aligned, they still would not have had a good marriage for any number of reasons. But a boy can wonder.

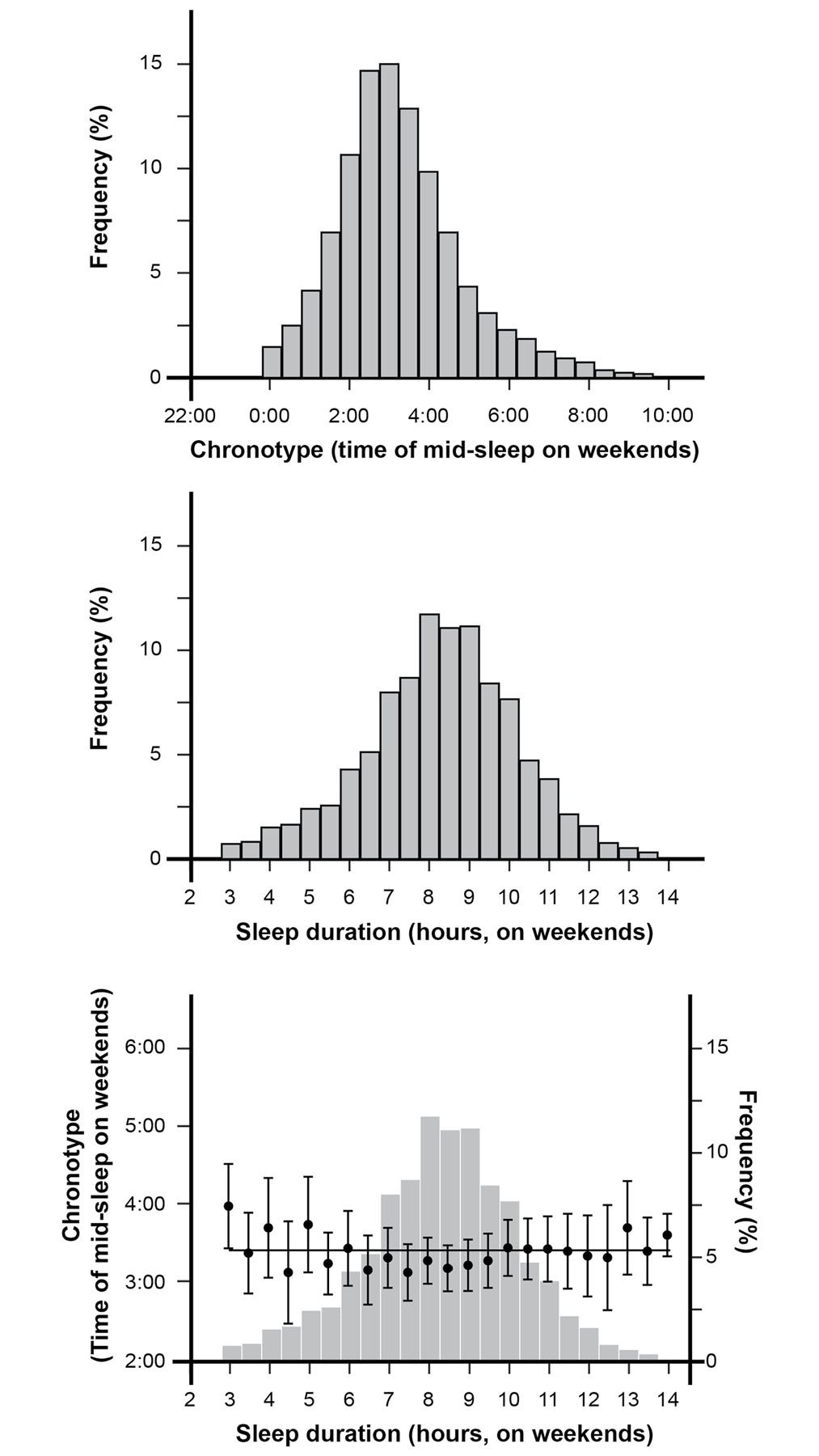
WE ALL KNOW PEOPLE who are extreme owls or extreme larks, and we know that most people fall somewhere in the middle. However, when sleep surveys of many thousands of people were conducted, some interesting trends emerged. In order to separate people’s natural inclinations from the demands of waking for work or school, the time of sleep and waking was calculated for Friday and Saturday nights. The midpoint of sleep on those nights is taken as an indication of how one’s activity rhythms relate to dawn and dusk, called a chronotype. Figure 14 shows the results from a survey of 53,689 adults in the United States.2 The midpoint of sleep ranged from about midnight to 9:30 a.m., with the average at about 3 a.m.
If we break this down, we find, not surprisingly, that high school and college students have the latest average chronotype of any age group. On average, women have slightly earlier chronotypes than men up to age forty, but slightly later chronotypes than men after that point. In both men and women, the variability in chronotype decreases with age; there are fewer extreme larks and extreme owls among older folks. This might be because there are biological factors that influence chronotype and change with aging. It might also be due to aging-related changes in lifestyle, like a reduced burden of childcare. Or, importantly, it might be that extreme larks and extreme owls are somewhat more likely to die young. If you are an extreme lark or an extreme owl, the likelihood that you will be able to find a work schedule that matches your chronotype is reduced, and there is evidence that this mismatch between chronotype and work schedule can have serious health implications. For example, in a large study of nurses, such a mismatch (owls working daytime shifts or larks working nighttime shifts) significantly increased the incidence of type 2 diabetes.3 Chronotype–work schedule mismatch was also statistically associated with higher incidence of cancer, cardiovascular disease, and stroke.
Chronotype is also influenced by cultural factors. Just ask any American who has walked into a restaurant in Spain at 8 p.m. for dinner and found it empty. In one recent smartphone-app-based worldwide survey, Belgians and Australians had the earliest average bedtimes (around 10:30 p.m.) while Spaniards, Brazilians, Singaporeans, and Italians had the latest ones (around midnight).4 One might imagine that chronotype and sleep duration would be affected by the use of artificial lighting and heating, not to mention more recent light-emitting diversions like smartphones and computers.
It is widely asserted that the technology of modern life leaves us sleep-deprived, but the evidence for this is not so clear. It should be noted that blaming sleep disturbance on the ills of modern life is not a recent innovation. When Henry David Thoreau retreated to an isolated cabin on Walden Pond in 1845, his main motivation was to alleviate his insomnia, which he blamed on trains and factories (it didn’t work).
It order to investigate how people slept before artificial lighting and heating became widespread, historian A. Roger Ekirch studied diaries, books, and accounts of travelers in preindustrial Europe. He has claimed, based on accounts of “first sleep” and “second sleep” in these writings, that “until the modern era, up to an hour of quiet wakefulness midway through the night interrupted the rest of most Western Europeans, not just napping shepherds and slumbering woodsmen. Families rose from their beds to urinate, smoke tobacco, and even visit close neighbors.” In Ekirch’s view, this “segmented sleep” was the norm, not just in Europe but in preindustrial societies generally, and that the present emphasis on “consolidated sleep” as the ideal form of rest is a recent and unnatural outgrowth of our technological age.5
If Ekirch’s assertion is correct, and, as he has claimed, it applies to people living in the tropics as well as the temperate latitudes, then one would expect that present-day preindustrial people, who mostly live in the tropics, would show segmented sleep as well.6 Unfortunately, this has not been borne out in wristband actimetry studies performed among the Hadza of Tanzania, the Tsimané of Bolivia, and the San people of Botswana and Namibia.7 Consolidated sleep was also found among the Toba/Qom people of Argentina,8 and in preindustrial quilombola dwellers in Brazil.9 To my knowledge, there are no reports that have found widespread segmented sleep in any population, either pre- or postindustrial. In the absence of such data, I remain deeply skeptical of Ekirch’s assertion that our ancestors typically slept in a segmented pattern.
However, beyond the dubious claims of a segmented pattern, are there some other differences in how preindustrial people sleep? There is general agreement that, on average, preindustrial people tend to have their chronotype shifted about an hour earlier, like Belgians compared to Italians. The question of sleep duration is less clear, with some researchers finding about an hour increase in sleep duration among preindustrial peoples,10 and others, working with different populations, finding no significant difference.11 It should be emphasized that there are many local influences on sleep duration besides electric lights, cell phones, and heaters (such as noise and social customs), and these could contribute to the variability of sleep-duration results in these studies.
In recent years, it has become popular for certain hard-charging leaders of government and industry to proudly assert that they need but a few hours of sleep every night. President Donald Trump, Prime Minister Margaret Thatcher, Tesla founder Elon Musk, and fashion designer Tom Ford have all claimed to get by on four hours or less. Those claims may be true, but, if so, they are very rare cases. Figure 14 shows that individual sleep duration ranges widely, from three to fourteen hours, with an average of about 8.5 hours. Only a small percentage of adults in the United States report four hours or fewer. Interestingly, there is no significant correlation between chronotype and sleep duration. You are just as likely to need a lot of sleep if you are a lark as if you are an owl. This lack of correlation suggests that chronotype and sleep duration are under mostly separate control in the brain.
FIGURE 14. Results from a recent sleep survey of adults in the United States. The top panel shows the distribution of chronotypes, measured as the midpoint of sleep on weekends. The middle panel shows the distribution of sleep duration and the bottom panel shows chronotype and mean sleep duration superimposed, illustrating that these two aspects of sleep are uncorrelated. Adapted from Fischer et al. (2017). Used with permission of a Creative Commons Attribution License (CC BY). © 2019 Joan M. K. Tycko.

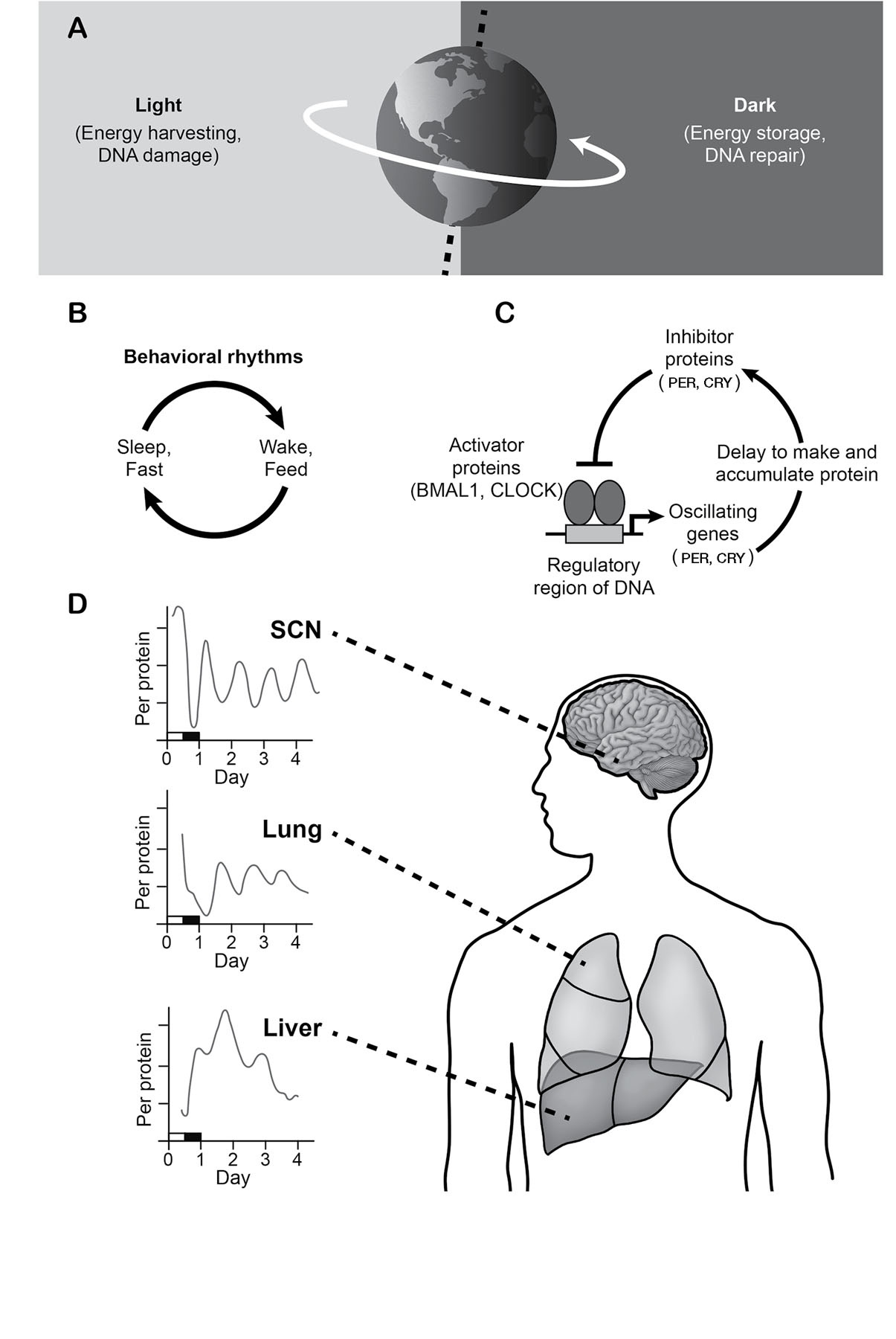
IT’S NOT JUST A human thing. Animals, bacteria, and fungi all match their biological rhythms to the solar cycle of day and night. Even many plants open and close their flowers at particular times of the day. Daylight provides energy to drive photosynthesis in plants, and warmth and light to see by, but those daytime photons can also damage DNA. Because DNA replication, which is part of cell division, renders DNA particularly sensitive to damage by light, nighttime is favored for cell division and cell repair. In humans, it’s not just sleeping and waking that are keyed to the solar cycle, but also body temperature, eating, digestion, mental focus, hormone secretion, growth, emotional state, and many other functions (figure 15). Even our most tender sentiments are influenced by the solar cycle—the most popular time for sex is reported to be 10 p.m.12
Do daily cycles of activity require a twenty-four-hour clock within the body, or are these behavioral and physiological rhythms solely driven by external cues like sunlight and ambient temperature? If you were to go live in a dark cave of constant temperature, without a watch (or Wi-Fi), your daily rhythms of sleeping and waking, body temperature, etc. would persist, but this cycle would become gradually desynchronized from the clock of the external world. For each twenty-four-hour period spent in the cave, your bedtime would shift about twenty minutes later. Similarly, if we were to take cells from your skin or liver and grow them in the dark in a culture dish filled with nutrient fluids, they would also show rough daily rhythms in their metabolic activity and in the expression of certain genes. These findings demonstrate that there is indeed an internal clock distributed throughout the body, but that it requires information from the outside world to remain synchronized with the solar cycle. Because your internal timekeeper runs approximately, but not exactly, twenty-four hours long, it’s called the circadian clock (from the Latin circa, meaning approximately, and dies, or day).
FIGURE 15. We contain biological clocks that serve to entrain our bodies to the daily cycle of darkness and light. The twenty-four-hour-long revolution of the earth imposes day and night cycles (A) that drive daily biological rhythms (B). Nearly all cells in the body have a circadian clock, a near twenty-four-hour rhythm of activity that must be synchronized with the environment by signals from the eyes. This clock depends on a negative feedback system that regulates gene expression (C). The brain region called the suprachiasmatic nucleus of the hypothalamus (SCN) serves as the master pacemaker and sends out biochemical signals to keep the other body clocks synchronized. This figure is adapted from Takahashi (2017) with permission of the publisher, Springer Nature. © 2019 Joan M. K. Tycko.
A tiny structure within the brain called the suprachiasmatic nucleus of the hypothalamus (which means “above the place where the optic nerves cross” and is abbreviated SCN) is the body’s master timekeeper. Laboratory animals like mice and monkeys that sustain damage to the SCN no longer have normal sleep-wake cycles (or any of the other circadian behavioral or physiological rhythms). Rather, they have brief periods of sleep and waking distributed randomly throughout the day and night.
For our purposes here, we don’t need to delve into the fine details of the molecular machinery that produces the circadian oscillation. In simplified terms, it works like this (illustrated in figure 15C). There are a set of genes that instruct the production of proteins with names like PER and CRY. These genes are turned on by activator proteins called BMAL1 and CLOCK, which work together. The crucial link to complete a loop of signals is that PER and CRY proteins feed back to inhibit the gene activation produced by BMAL1 and CLOCK. Because it takes a while for enough PER and CRY protein to accumulate in the cell to start inhibiting their targets, the amount of these proteins oscillates up and down, and it turns out that this feedback system is tuned to cycle every 24.3 hours or so. There are many more details of the circadian clock, but that’s the basic idea: it works through a negative feedback loop of gene expression.13
Light coordinates the timing of the internal circadian clock with the external world through light-sensing neurons in the retina. These include a group of large, spindly cells called intrinsically photosensitive ganglion cells. These neurons send their axons to the SCN to convey electrical information about the overall ambient light level. This stream of information from the eyes produces subtle daily adjustments in the SCN’s master clock. The SCN neurons then communicate this information to all of the tissues in the body, using both neural signals and circulating hormones (figure 15).14 In this way, activities in the various tissues of the body are at least approximately synchronized with the solar cycle. It’s not perfect: the kidney clock runs at about 24.5 hours, whereas the cells in the cornea oscillate with a period of about 21.5 hours. This rough synchrony appears to be good enough for healthy body function.

OVER TWENTY YEARS AGO, an adult patient entered a sleep clinic in Salt Lake City with a disabling problem. She was such a lark that she began to feel sleepy in the early evening. She was typically asleep in bed by 7:30 p.m., only to awaken at 4 a.m. She wasn’t able to have much of a social life with that schedule. During her treatment, she mentioned that several other members of her extended family had the same problem. There’s no statement that’s more likely to get the attention of a geneticist than that, and so Louis Ptáček and his colleagues soon tracked down her relatives. Eventually, they found twenty-nine people in three families with this extreme lark behavior, which they named familial advanced sleep phase syndrome (FASPS). This rare trait is dominant, so you only need to inherit a copy from one of your parents to have it. When FASPS patients were analyzed, it was found that many of their body rhythms were shifted three to four hours earlier, including the nighttime low point in body temperature and the time of day when the hormone melatonin begins to be secreted.15
A few years later, Ptáček’s group joined forces with Ying-Hui Fu’s lab,16 and together they found that his FASPS patients carried a single mutation in the PER2 gene, disrupting its function in the circadian clock.17 Since that time, additional FASPS families have been found bearing mutations in other genes encoding parts of the circadian clock: CRY2, PER3, and CK1DELTA (which interacts with the PER proteins). As another test, when these various mutations in circadian clock genes were introduced into mice using genetic engineering, the mice showed early-shifted activity and body temperature rhythms, similar to the FASPS patients. These results are very satisfying, but we should not rush to conclude that all extreme larks result from mutations in core circadian clock genes. There are some people with this trait who do not appear to have mutations in any of those genes.
Another rare sleep trait that runs in families is short sleep duration. The patients who have this trait are called familial natural short sleepers. They sleep about six hours per night and have no detrimental health consequences. Two different short-sleeping families have been analyzed, both of which bear mutations in the DEC2 gene, which may or may not be a regulator of the circadian clock system (there are conflicting reports in the literature) and for which the relationship to the brain’s sleep circuitry remains unclear.18 Another short-sleeping family was found to harbor a mutation in the ADRB1 gene. When Fu and Ptáček genetically engineered mice to bear this mutation, they too became short sleepers. Here, the link between the gene and the brain’s sleep circuits is better understood. ADBR1 directs the production of a neurotransmitter receptor called the beta-1-adrenergic receptor, which is involved in regulating the electrical activity in a brain stem region called the pons that is important in the transition from sleep to wakefulness.19 On the other end of the sleep duration distribution, when a particular mutation is created in SIK3, which is important for regulating the clock gene PER2, extreme long-sleeping mice are produced.20 However, as of this writing, it is not yet clear if genetic variation in SIK3 affects the duration of human sleep.
Both FASPS and familial natural short sleep are rare conditions that fall into the left-hand tails of the bell-shaped distributions for chronotype and sleep duration shown in figure 14. Could gene variation also underlie subtler variations in sleep found in the central portions of these two distributions? There are two lines of evidence that suggest a genetic component to normal sleep-cycle variation. First, a pilot study that used Fitbit activity trackers to monitor the sleep of identical versus fraternal twin pairs estimated that about 50 percent of the variation in sleep duration and about 90 percent of the variation in restless sleep incidence was heritable.21
Second, three recent large GWAS investigations sought to find gene variants associated with the continuum of lark-to-owl chronotypes.22 Impressively, variation in four genes was implicated in all three studies. Of these four, the aforementioned PER2 and another gene called RGS16 are known components of the circadian clock; a third gene, FBXL13, might be a regulator of the circadian clock (the literature remains unresolved on this point); and the last, AK5, has no known relationship to the circadian clock at all. In thinking about AK5 and other non-clock genes (which came up in two or three of the GWAS investigations), we should remember that the circadian clock is reset by light signals from the retina. As a result, variation in genes involved in that resetting process, perhaps those expressed in the intrinsically photosensitive ganglion cells that convey the luminance signal from the retina to the SCN, might also give rise to differences in chronotype.

EUGENE ASERINSKY WAS A graduate student in the sleep laboratory of Nathaniel Kleitman at University of Chicago, where he made EEG recordings from adults as they fell asleep. These recordings showed that after falling asleep, the EEG gradually changed from a noisy, jittery trace to one with large, slow oscillations. At this point, the researchers assumed that deep sleep had been achieved and it would remain in force until waking. Their standard procedure was to record for forty-five minutes to capture this transition to slow-wave sleep and then turn the EEG recorder off to save the chart paper that was piling up on the floor in huge drifts. One night in 1952, Aserinsky had the clever idea to bring his eight-year-old son, Armond, into the lab to be that night’s subject. About thirty minutes after Armond had fallen asleep, his father was watching the pens on the EEG chart recorder register the large, slow oscillations of deep sleep. Then, to his enormous surprise, the EEG shifted to a rhythm that looked more like the waking state, even though Armond was still clearly sleeping and totally immobile. This stage of sleep, associated with rapid eye movement (REM), does not usually occur in adults until about ninety minutes after falling asleep. However, in children like Armond, it occurs much sooner.
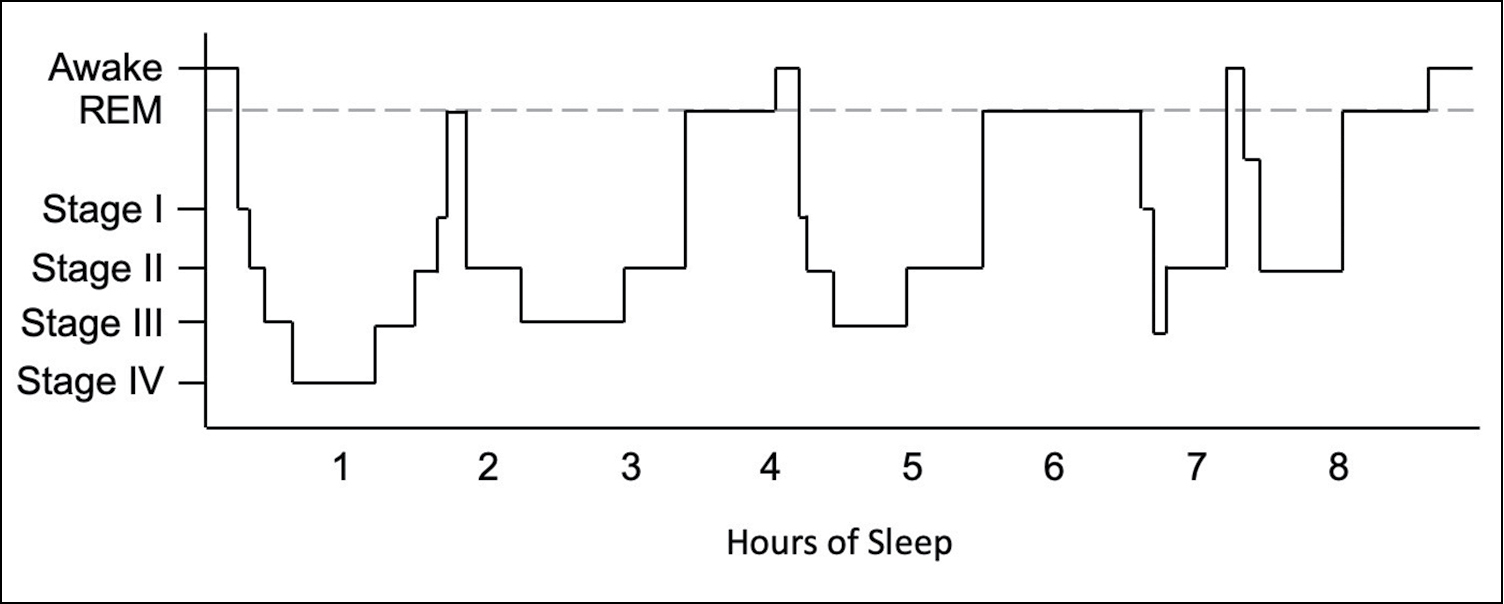
The publication of these findings by Aserinsky and Kleitman in 1953 was a watershed moment for sleep research, and in the following years a much more detailed picture of sleep emerged. When scientists left their EEG machines on all night (piling up gargantuan stacks of chart paper in the process), they found an adult sleep cycle of about ninety minutes. This consisted of the aforementioned gradual descent into deeper and deeper sleep, accompanied by gradual synchronization of the EEG. These stages of sleep are collectively called non-REM sleep, and they are further subdivided into four stages, ranging from drowsy or nodding off (stage I) to deep sleep (stage IV). Stage IV is followed by the transition into a period of REM sleep. The termination of the REM sleep period marks the end of one sleep cycle (figure 16). A typical good night’s sleep will consist of four or five of these cycles. As the night progresses, the composition of each sleep cycle changes so that there is proportionally more REM sleep. In the last cycle before waking, as much as 50 percent of the sleep cycle may be devoted to REM. Humans show changes in sleep over the lifespan, with the proportion of the time spent in REM sleep decreasing from about 50 percent at birth to 15 percent among the elderly.
FIGURE 16. Stages of sleep throughout the night in an adult. Note that REM sleep predominates in the second half of the night. This example shows four sleep cycles.
There are a host of physiological changes that accompany REM sleep, including increases in breathing rate, heart rate, and blood pressure, and a sexual response—penile erection in men, erection of the nipples and clitoris together with vaginal lubrication in women. Even more striking are changes in muscle tone. In the course of a night, the typical adult sleeper will change his or her position about forty times, mostly without being conscious of this action. However, in REM sleep, there is no movement at all because the body goes totally limp. As a result, is almost impossible to have REM sleep in anything other than a horizontal position.
REM sleep is sometimes called “paradoxical sleep” because the EEG resembles the waking state, yet the sleeper is essentially paralyzed. The movement-commanding centers of the brain are actively sending signals to the muscles, but these impulses are blocked at the level of the brain stem by an inhibitory synaptic drive from another part of the brain and so never reach the muscles. This blockade only affects the outflow of motion commands down the spinal cord, not those of the cranial nerves, which exit the brain stem directly to control eye and facial movements (and heart rate, through the vagus nerve).23 A failure in this blockade is seen in a condition called REM sleep behavior disorder, which is characterized by violent, presumably dream-enacting behaviors during REM sleep, often causing self-injury or injury to others. This may include punching, kicking, leaping, or even running from the bed. REM sleep behavior disorder is different than conventional sleepwalking, which only occurs during non-REM sleep.

NARCOLEPSY IS A RARE disorder that usually starts in the teenage years. Over the course of a few days or weeks, the urge to sleep during the day gets stronger and stronger. Despite having a good night’s sleep and normal alertness soon after waking, these kids fall asleep in class, while doing their homework, and, dangerously, while driving. Sometimes this onset of daytime sleepiness is associated with weight gain. In narcolepsy, REM sleep can occur suddenly, at any time, without first passing through the stages of non-REM sleep. It is accompanied by dreamlike hallucinations.
If the symptoms stop there, the diagnosis is type 2 narcolepsy.24 However, in a different form of the condition, type 1 narcolepsy, an additional terrifying symptom then develops. Here’s an excerpt from a typical case report:
An 18-year-old man presented with a 2-year history of severe excessive daytime sleepiness that began a few months after a vaccination for influenza A (H1N1). He had to repeat a school year because of the excessive daytime sleepiness. He was overweight and had frequent sleep paralysis and nightmares. Six months after the onset of excessive daytime sleepiness, he developed episodes of weakness in his limbs and neck triggered by various emotional stimuli, especially when he laughed with his brother. His brother had made a cell phone video that the neurologist was able to view, which led to the diagnosis of typical cataplectic attacks.25
Cataplexy, as found in type 1 narcolepsy, is a form of flaccid paralysis, typically lasting for a few seconds to two minutes, and usually begins in the face and neck and sometimes spreads outward to include the trunk and limbs.
Type 1 narcolepsy is associated with a complete loss of a small population of neurons in the lateral hypothalamus of the brain. These neurons produce the neurotransmitter orexin, which is important in regulating both alertness and feeding behavior. This explains while many patients gain weight as their narcolepsy develops. Type 2 narcolepsy involves only a partial loss of these neurons. In both types, the orexin-using neurons are destroyed by an autoimmune attack. There was an unusual increase in the incidence of type 1 narcolepsy coincident with the 2009–2010 H1N1 flu pandemic. It is suggested that some protein fragment in the H1N1 flu, or the vaccine designed to trigger immunity to it, cross-reacts with a protein on the surface of orexin-using neurons, leading to their destruction by T cells of the immune system.
Type 1 narcolepsy is a great example of gene-environment interaction. It is weakly heritable, with only about 1 to 10 percent of cases running in families. If your identical twin has narcolepsy, your chance of having it will be about 25 percent, which is much higher than the 0.05 percent overall rate in the population but far less than one would expect for an entirely heritable disease.26 Yet, more than 98 percent of patients with type 1 narcolepsy have a particular variant of an immune-system gene (with the mind-numbing name HLA-DQB1*0602), compared to only 12 percent of the general population. The most likely explanation is that, in order to develop type 1 narcolepsy, you must have both the unlucky variant of the HLA gene and be exposed to some antigen, like the H1N1 flu virus, that triggers the autoimmune response against the orexin neurons.27

EVEN IN SLEEP, WHEN it’s largely disconnected from sensation, the human brain can generate a complete world of conscious experience, all by itself. Some mornings you might awaken with no recollection of any dreams at all, while other times the night seems to be crowded with them. In general, unless you wake up during or within a few seconds of the end of a dream, you are unlikely to recall it. Once awake, the memory of a dream will often quickly dissolve unless written down, recorded, or spoken to someone else.
Dreams are dominantly visual, in full color and movement. They are built from the prior experience of waking life, with recognizable people, places, and objects. Sounds and speech are also common in dreams, but the senses of touch (including pain and temperature), smell, and taste tend to be diminished. Most dreams have a truly sensory character—they are not mere thoughts or ruminations, and yet they are famously different from the experience of waking life.
For many years it was thought that dreaming only occurred during REM sleep. Now we know that dreams can be reported following awakening from any stage of sleep, but that their character and duration tend to vary with different sleep stages. Dreams that occur in stage I, right after sleep onset, are usually brief and, although they have a strong sensory component, this sensation does not progress to form a continuing narrative. These dreams are typically scene fragments, without much detail and with little emotional content. They tend to be logical and congruent with waking experience. Importantly, sleep-onset dreams are very likely to incorporate experiences from the previous day’s events. In a classic study, subjects played the video game Tetris for several hours before sleep. When fitted with EEG recording gear and then awakened during stage I, more than 90 percent of the subjects reported scenes from the game, but only when they were awakened shortly after sleep onset, not during deep non-REM (stages III and IV) or REM sleep.28
The dreams that we tend to remember are the narrative ones that unfold in a storylike fashion and are rich in detail. They often incorporate weird blending and transformations of familiar people and places, and violations of physics like human flying. In our dreams, we can experience a different reality, but we have little control over it. We cannot pursue goals; instead, we are carried along and tend to accept sudden transformations and impossible objects as a given. There is a suspension of disbelief about otherwise illogical or bizarre experiences. Narrative dreams can often have strong emotional content, both positive and negative, but they don’t have to.
Narrative dreams are the ones we are most likely to remember and discuss. In part, this is because they make for good stories (though sometimes not as interesting to others as to the dreamer), but it also reflects the structure of the sleep cycle: you are most likely to awaken, and therefore remember your dream, toward the end of the night, when REM sleep predominates. While narrative dreams are most frequent during REM sleep, they are not exclusive to it. In sleep labs, narrative dreams can sometimes be recalled from awakenings during sleep stages III and IV, particularly during the second half of the night. Sometimes narrative dreams can be recalled when subjects are roused from naps in which no REM sleep has occurred. People with neurological damage to the brain stem, who have lost the ability to enter the REM stage, can still have narrative dreams.29 Conversely, people in REM sleep aren’t necessarily dreaming. On average, 20 percent of awakenings from REM sleep result in no dream report at all in adults, even in the lab where sleepers are awakened and immediately queried about their dreams.30
During REM sleep, information from the senses is almost, but not entirely ignored, due to a partial blockade of incoming electrical signals at the level of the thalamus. Olfactory information, because it does not pass through the thalamus, is still processed during REM sleep and so can serve as the basis for subconscious associative learning conducted entirely during sleep.
Nonolfactory stimuli, like the buzz of an alarm clock, can sometimes be incorporated into the end of a REM-stage dream. Rarely, stimuli like a spray of water on the face or pressure on the limbs can find their way into dream content.31 In one provocative set of experiments that would probably not be approved today, subjects fell asleep with their eyelids taped open, and objects were illuminated in front of their eyes during the REM stage. Even these manipulations did not reliably intrude on dream content.32
There are several lines of evidence to suggest that narrative dreaming is more related to imagination than perception. Dreaming is abolished in some patients who sustain damage to a part of the brain called the tempero-parietal-occipital (TPO) junction. These patients also have serious deficits in mental imagery while awake. In adults, the cognitive skill that most predicts dream recall is visuospatial imagery.33 Brain-imaging studies performed during REM sleep, when narrative dreams are most likely to occur, show activation in brain regions involved in mental imagery and visual or auditory memory. Interestingly, the brain regions involved in the initial processing of sensations like vision, touch, and sound are largely inactive during REM sleep. Also inactivated in REM sleep are regions associated with voluntary control (right inferior parietal cortex), self-monitoring, and reflective thought (posterior cingulate cortex, orbitofrontal cortex, and dorsolateral prefrontal cortex). Overall, the picture from both brain lesions and brain imaging shows that narrative dreaming is most similar to random imaginative thought in the waking state—that is, daydreaming.
Some people can report their narrative dreams every morning and others claim to rarely dream. However, if people who report rarely dreaming are taken to the sleep lab, awakened during REM sleep, and queried, most of them will report narrative dreams. As I mentioned earlier, some people with certain types of brain damage are truly lacking in narrative dreams, but they are few and far between. Most people who report rarely dreaming can train themselves to recall more dreams if they so choose. A good way to start is to keep a pad of paper or a voice recorder by the bed in order to make a note of dreams upon awakening. This will result in both more recall and, over time, more brief awakenings in the second half of the night to allow for potential dream recall.
Because dreams are formed from our past experiences, the raw material for our dreams is limited by our sensory worlds. For example, if you are born blind, you will not have visual memories and so you will not have visual dreams. However, if you are born sighted and become blind after age five or so, either from damage to the eyes or from damage to the early visual-processing stages of the brain, then you will be able to have visual dreams, built from the visual memories you have stored, albeit sometimes morphed and recombined in bizarre ways.
While you can still have visual dreams after damaging the early parts of the visual pathways in the brain, damage to the later parts of these processing pathways will affect dream content. For example, people who, as adults, have acquired brain lesions that impair their perception of faces when they are awake will not dream of particular faces. Likewise, people who have sustained damage in brain regions involved in color or motion perception have corresponding deficits in their dreams.34
The transitions between sleep stages are controlled by a complex interplay of neurotransmitters, including acetylcholine, norepinephrine, serotonin, histamine, and dopamine. We know that drugs that target these neurotransmitters can affect dreaming. For example, most antidepressants, which act on serotonin and norepinephrine signaling, seem to reduce the frequency of narrative-dream recall; some SSRI antidepressants enhance the emotional content of recalled dreams. Patients with Parkinson’s disease, which attenuates dopamine signaling, report reduced emotional content and bizarreness in their dreams.35 These findings make it likely that genetic variation in the receptors for these sleep-altering transmitters—as well the enzymes that make, degrade, and store them—could affect dream patterns, but at present, there’s not much solid evidence either for or against this idea.
Although we might like to imagine that, in our dreams, we can be fundamentally different from our waking selves, this does not appear to be entirely true. While dreams can meld and stretch and recombine our past experiences and inject fantastical alterations of time and place, the raw material from which dreams are made is our waking experience. Not only that, formal content analysis of many dreams, across cultures, has revealed that the predominant concerns, mood, curiosity, and cognitive capacity are highly correlated between our waking selves and our dreaming selves.36 The best predictor of the content of your dreams is your waking life.