Chapter 4 - An Intricate Marriage
"Disease is the warning, and therefore the friend - not the enemy - of mankind."
–Dr. George S. Weger
Tom was a competitive bodybuilder for quite some time. He never really trained for the national competitions; rather he just stuck to the local ones, but was competitive nonetheless. With his days of competing behind him, he still hit the gym pretty hard as staying in shape was deeply ingrained in him by now. The day Tom got hurt was just like any other. He slept great, ate well, warmed up, and started to hit the weights when he noticed a disturbingly sharp pain in his left lower back. His body seized up and Tom was left there lying on the floor wondering what had happened. Tests and MRIs showed three disk herniations. Therapy wasn’t helping. Tom couldn’t sleep, sit, lie, or stand without incredible pain. He ended up finding me through a business associate of ours.
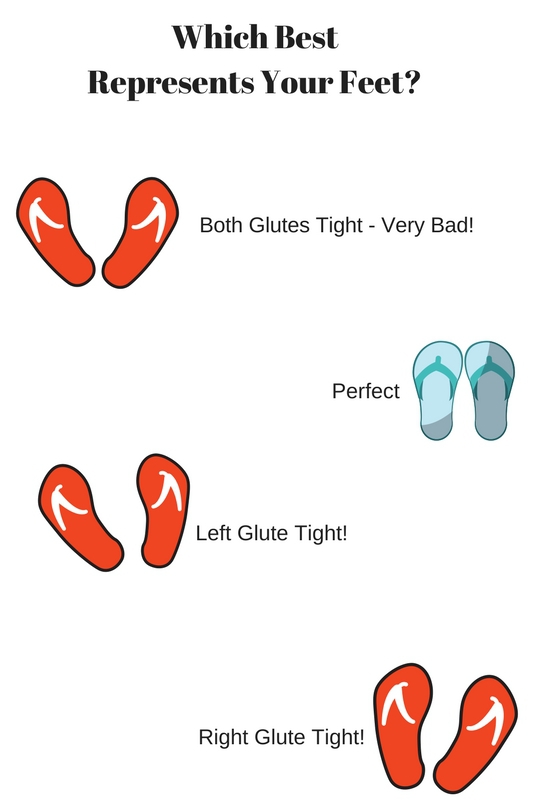
The day Tom came to see me, I could already see the problem the minute he got out of his car and started walking towards me. His right foot was facing straight ahead, and his left foot was turned out at 75 degrees. Tests showed extreme left glute tightness, and extreme right hip flexor tightness; he had what we call in physiology a lower-cross syndrome
.
Utilizing our mobility and motility drills, we loosened up Tom’s left glute with some rolling on a lacrosse ball followed by the proper stretches. Next, we had Tom roll on his right hip flexor to loosen it up, followed by the hip flexor stretch you are going to learn later in this book. Reversing a lower cross syndrome is all about time because it is a rotational problem. Because your body works in a spiral/rotational pattern, as you loosen the pattern up it will start to get tight again when you start to move. While this particular case was not a quick fix, Tom was pain free in three months’ time and still enjoys pain free exercise to this day.
We Don’t Know What We Don’t Know
After my 30th
birthday, I told myself I was going to stop lifting heavy, give my joints a break and start doing more marathons and triathlons. I did this for about three years and in that time went through about 6 bikes. The first one wasn’t light enough, the second didn’t have the right components, and the third had some aluminum instead of being all carbon. After every race I became more and more unsatisfied with my bike time so I kept switching out the bike. Finally, after taking my bike in for a tune-up one day, the mechanic asked me if I ever had my bike fitted to me and I said, “No, what is that?” He explained it is a service they offer where they adjust everything on my bike to optimize it for me to be as fast as possible. It was $80 and compared to the cost of a new bike at $3000 I guessed that it was a good idea. After having my bike fit for me, I had my best bike split ever in my next race
.
What does this story illustrate? The entire time I was blaming my bike for being slow, it wasn’t my bike, it was the fact I didn’t know how to ride a bike. More specifically I didn’t know how to optimize my bike for performance and this led to a lot of wasted time, and money on my part.
The first concern I always hear from my clients/athletes is, “I don’t know why my back hurts.” I tell them it’s because they don’t know how the back works. The purpose of this chapter is to help you understand what you don’t know you don’t know
about how the back functions, and what an intricate marriage
the muscles that comprise your midsection are in. Upset one of these bad boys and it’s the back that suffers. Armed with this knowledge, we can better understand our condition, which will then help us to better treat ourselves.
Your Feet Tell All
In my opinion, Ida Rolf is the Godmother of pain management. In her amazing book Rolfing: Reestablishing the natural alignment and structural integration of the human body for vitality and well-being,
she says, “Only by bringing peace from the ground up, can problems higher in the body be understood.” So if we want to fully understand our back pain, we first need to look at our feet. If you ever go to the mall, or the beach, or any one large area where people congregate, I want you to look down and watch how people walk. Where are their feet
facing? Where are your feet facing? More than likely they are facing out and this is where problem numero uno is.
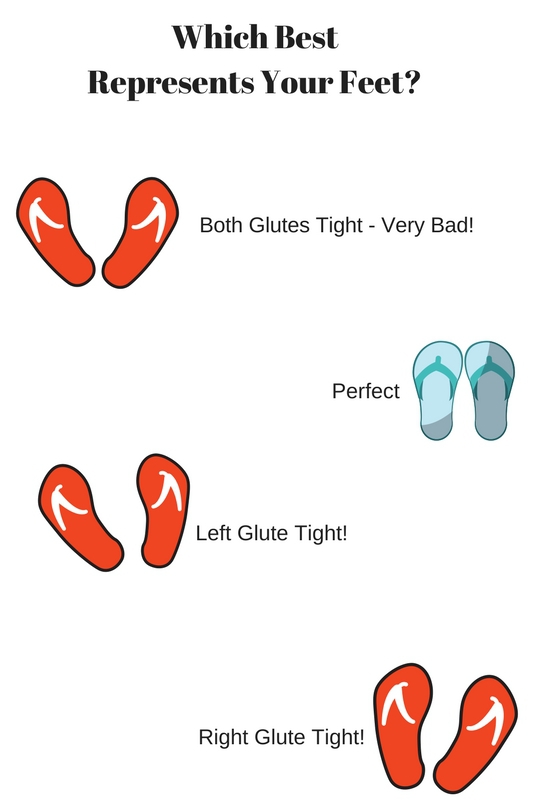
If you remember in chapter one I said we humans are machines, but we are not robots. If a robot is broken, that area just wore out too fast, that’s all. With the human body being a web, if one area, in this case our feet, is not functioning correctly, this will largely affect the area that is translating the force the feet are producing. In this case, you guessed it: it’s our back! Regardless if one foot or both feet are turned out, the back feels the dysfunction in the form of pain. The ankle and the knee are hinge joints meaning they function best through straightforward flexion and extension. By turning the foot out, the ankle becomes strained, the knee becomes strained, and the thigh now has to rotate in order to move forward.

We need to understand that as human beings we walk with our low back, abdominals, and hip flexors, on
our legs. We do not walk with
our legs! When we are not pointing our feet in the direction of our movement, the back muscles will suffer. The back muscles simply were not designed for such wear and tear.
Being conscious of our foot position is the first step in eradicating our back pain. You can do everything else in this book to the best of your ability, but if you do not fix your foot position the pain will return. It’s just that simple. An exercise I used to do in my gym was called walking Wednesday. I instructed all of my athletes to take their shoes off and walk feet forward for 3-5 minutes. Correcting your feet will take more than just 3-5 minutes, but it’s a start. I recommend to walk barefoot as much as possible to allow you to actually feel what proper movement is like. It’s also a great stimulus for your feet and helps ground us to the earth which syncs our sleep
cycle. The second consideration we need to be aware of is our footwear. The lower the drop and the harder the sole the better. “But wait Chris, I need arch support!” No you don’t, and you’ll learn more towards the end of this book about why.
Your foot has not one, not two, but three arches, 26 bones, 33 joints, 109 ligaments, and 19 muscles and tendons. I’d say that’s some decent support! Inhibiting the expansion and contraction of our foot’s arch sends the wrong signal to the rest of our body from the ground up. In my experience, the best types of shoes have a very hard sole, and have a 3-4 degree drop. If you like zero drop shoes then go for it. Shoes that have high heels combined with cushiony air, or gel may be comfortable for your feet, but strain these mechanisms we depend on to move. Depending on which type of shoes you decide to buy, we need to be aware that a lower drop in the sole of the shoe will increase foot activity, which will increase calf activity as well. If you’re a runner, be careful to not start off too quickly or you’ll wake up the next day with some pretty tender calf muscles!
A question I pose to my clients is, “Can you start today?” If you can’t go buy new shoes today, can you start walking with your feet forward today? Surely there’s nothing stopping you from doing that. Like I said earlier, there is no magic bullet, no miraculous cure. Just a bunch of little changes we are going to make that will produce big results
!
Your Sacred Seat: The Hip Flexors

Your pelvis is actually referred to in anatomy as your sacred seat. The sacred seat I am referring to is the one you are sitting on right now! Sitting is quickly becoming the new smoking and has been found to have many links to heart disease, and even cancer. In Jo Ann Staugaard-Jones’ book The Vital Psoas Muscle: Connecting physical, emotional, and spiritual well-bei
ng she wrote about a case study where 12 adult volunteers recorded sitting for a minimum of 5 hours on good days to a maximum of 11 hours on bad days! Sitting is a destroyer of the proper function of your psoa and illiacus muscles, which are more commonly called your hip flexors. Your hip flexors are at their longest which is about 16 inches in length when you are standing up. When seated they shorten considerably. Remaining in this position causes your hip flexors to lock in a shorter position than they can function well in. This causes not only back pain (they
originate at the 12th
thoracic vertebrae which is the major rotational joint in the back to the 5th
lumbar vertebrae, descending down and attaching to your femur) but can also create problems with our breathing and circulation as well.
Continuing with our fascial web ideology, what we find with the hip flexors is even more amazing. The fascia from our hip flexors continues along and connects to our diaphragm, our heart, our lungs, our kidneys, and several other organs. Having dysfunctional or tight hip flexors not only means our back will hurt from its improper length, but our respiration will suffer, as well as our hearts ability to pump blood. Those are two key elements I just don’t want to change in my body, if you ask me! Since locomotion is first initiated with your hip flexors, it makes no wonder that they are also directly linked to your brain’s fight or flight response. Chronic negative thinking puts your hip flexors in a chronically contracted state. This negative feedback loop can in some cases create severe anxiety, and is also why many believe that your emotions have a huge correlation with back pain. The healing methods we will be using for the hip flexors are not very comfortable and I urge you to take them on slowly, but neglecting these muscles will also, once again, not allow you to heal your back pain fully. There are going to be days where you will want to take the day off from those exercises, but those will be the days that will benefit you the most!
I know what you are thinking: “What can I do to start right now?!?!” I have my athletes and clients abide by the 20/20 rule. Every 20 minutes you are sitting, stand
up and do something for 20 seconds. Do a squat, walk to the water fountain, go to the fridge, or even stand up and do some light stretching – just don’t get stuck in that position!
Your Abs Are Not Your Core

Who doesn’t love the way a chiseled six-pack looks on a handsome man or woman? It’s been labeled as the holy grail of fitness in some circles. You can have chicken legs and a spaghetti back, weigh 110 pounds soaking wet, but if you have a six-pack you must be fit! I hate to break it to you guys, but in 18 years of coaching I have never done a single abdominal exercise that helped me run faster, lift heavier, or jump higher, and when my back was
hurting doing anything abs related was the furthest from my mind. Yet we live in a culture that glorifies the abdominals and we have practitioners who tell people their back pain is stemming from ab weakness and advise them to do “core exercises,” which translates to a bunch of sit ups. Sit-up type of exercises can be disastrous for those who have tight hip flexors because the hip flexors will initiate most of the movement. You are now working chronically tight and stressed out hip flexors even harder thus persisting your back pain. A simple stretching of the hip flexors, combined with a strengthening of the lower lumbar muscles, glutes, and hamstrings is a much more effective option. Now does this mean we totally neglect the abdominal muscles and never train them? No! Every muscle in the body should be trained to be strong and effective, sit-ups and direct abdominal training is simply not the best way to get rid of your back pain.
Your real “core” is what I call your hip flexors, quadratus lumborum (lower back muscle), gluteal (butt) muscles, and your hamstrings (back of the thigh muscle). Take one of those muscles away and you take away your movement. Think about it – nobody calls into work sick with sore abdominals. No one says, “This chair is really killing my abs.” Tight hip flexors bring your head closer to your hips, rendering the abdominals ineffective at supporting your organs, and your lower back. Strengthening them without addressing your tight hip flexors will not improve your posture or position. Oh, and one last thing, stop referring to them as your core
!
You Don’t Have Back Pain, You Have a Butt Proble
m
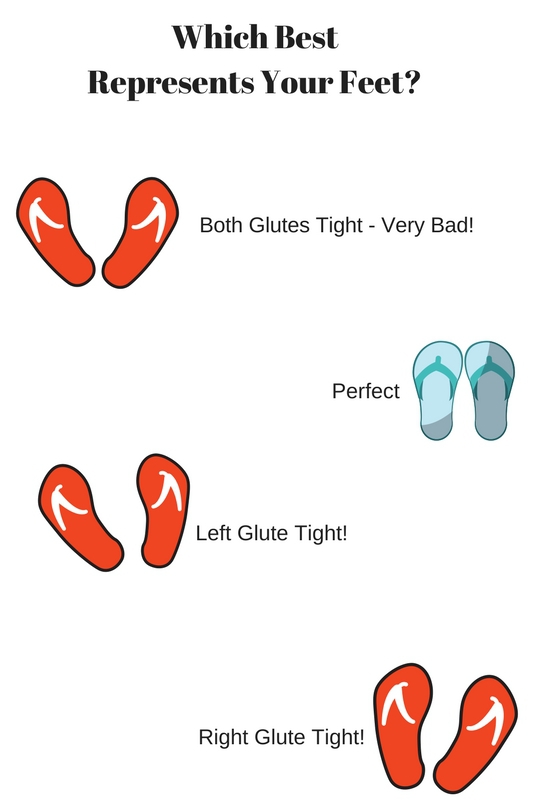
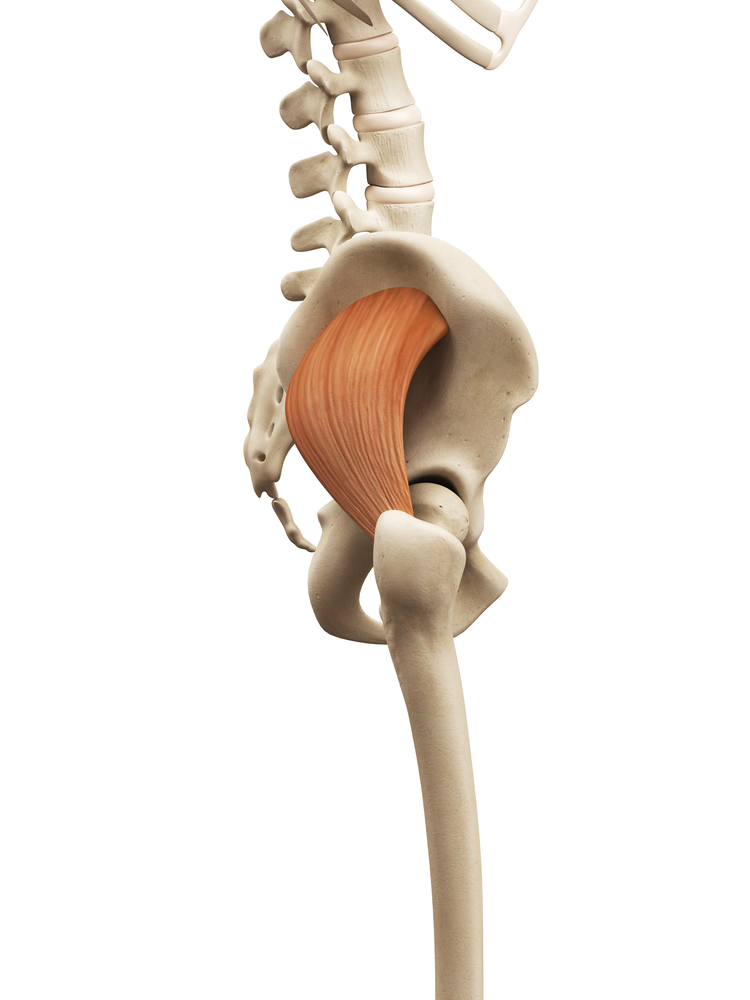
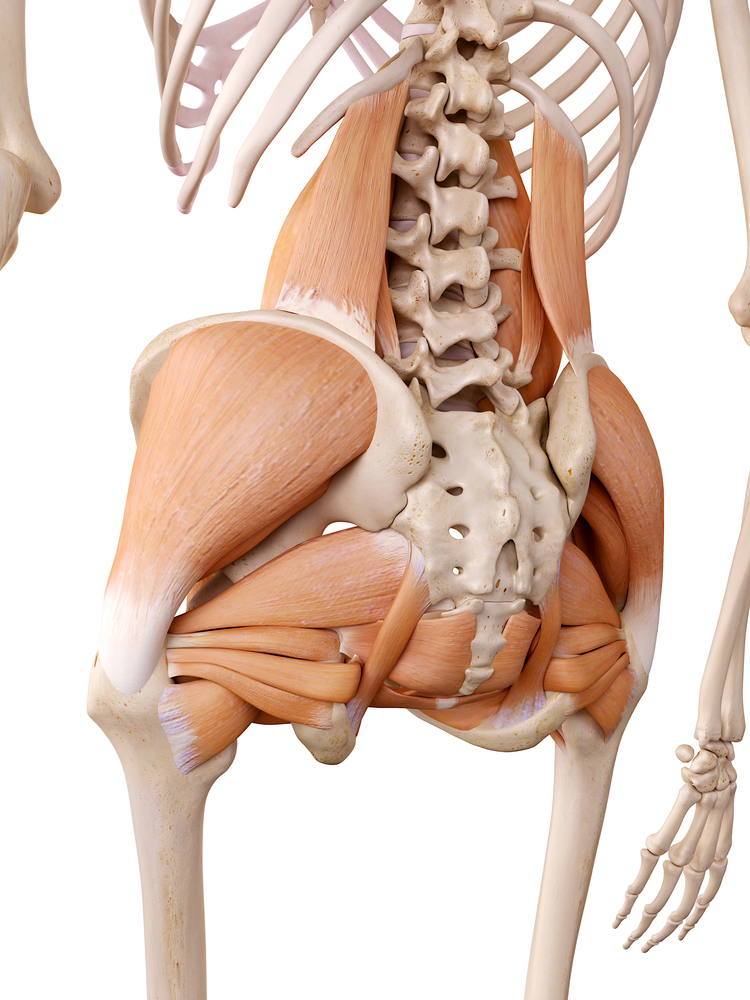
You have heard me refer to these mysterious muscles known as the “glutes” for a while now. If you knew what I was talking about – great, this will expand your knowledge. If you had no idea what I was talking about, you are in for a treat! The glutes are comprised of three muscles: the gluteus minimus, gluteus medius, and gluteus maximus. To make things more interesting we have four parts to our gluteus maximus, which are the lateral part of the lateral, the medial part of the lateral, the lateral part of the medial, and the medial part of the medial. We will learn how to target these areas in our strengthening section. The primary point we need to understand in this section is how our glutes affect the function of our low back. When we take a step, muscular force is not transferred straight up the body, rather when it reaches the glute of the side that the foot is in contact with the floor, it then crosses over to the other side of the back on up to the shoulder. To put it plainly, our bodies function in an X pattern, as illustrated in the diagram below:

You can test this very easily if you want by walking with the backs of your hands on your lower back. Feel which side of your back contracts when you walk compared to which foot you have on the ground. When your left foot strikes the ground, you will feel a contraction in you right lower back, and when you right foot hits the ground you will feel a contraction in your left lower back. Having your body function this way is very efficient and allows for a smooth gait pattern. If the right glute and right low back fired at the same time we would all be walking like penguins and penguins do not walk very fast or very efficiently!
As we discussed earlier though, human beings do not move correctly 100% of the time. We all have faults, myself included and when we rely too much on one leg, or have trauma incurred on one side of the body, we develop a deficiency that will then hinder how our back functions. When the dysfunction first occurs, the back says, “Hey, no problem, I got this!” But after a couple of months or a couple of years depending on how much stress you put on your back, it will eventually come to a breaking point where pain is produced. Remember, your entire body’s system is a yes man; it will keep doing what you ask of it till the structure no longer holds. When we start feeling pain, we have had a problem for some time, and this then takes time for us to reverse.
In most cases what happens is one glute will get tight, the other glute will get weak and the more unilaterally we become imbalanced the more taxing it becomes on the lower back. Close to 95% of all back pain cases I treat are cured by not even touching the back. We
spend most of our time correcting our hips. When the hips are corrected, the stress on the back alleviates and you become a happy camper. Correcting the glutes is tricky as there are three separate areas we need to work on with absolute precision. Just rolling around on your butt without an objective will get you nowhere. With that said, let’s take a close look at each one of these muscles starting with my favorite – the gluteus minimus.
The Gluteus Minimus
To get a feeling of what it is like when this muscles is tight, think about putting on a pair of pants that are two sizes too small for you. Then put a belt on and tighten that sucker as much as you can, sucking in your stomach even. Once all of that is accomplished, try bending over or even doing a simple squat. Impossible, right? That is the damage this little guy can cause. Many people will also
suffer from what I call “Fake Sciatica” in which the subject will have pain radiating down their leg sometimes to their foot, yet their flexibility checks out. No tight hamstrings, no tight glute muscles, or hip muscles. These people are prescribed painkillers and muscle relaxers and sent on their way, when a little pressure at their hip would cure all. Too simple I suppose.
The gluteus minimus internally rotates your thigh, and also abducts it, which means it moves your leg away from the midline of your body. It is a very, very active muscle stabilizing the pelvis to the femur (thigh bone) and contracts every time you shift your weight from side to side. Shifting your weight to one leg while standing will stress this guy out, so will long trips in planes, trains, and automobiles. Releasing it can be very entertaining because of where it will send pain. It is somewhat of a rogue muscle in that respect, but when we do get it to release it will feel like you squirted a quart of oil in your back!
The Gluteus Medius
The gluteus medius muscle—as you can see by where it originates and where it inserts—can hugely affect the health of our back. If one side decides to get tighter than the other, our pelvis will become uneven and BOOM! We have back pain. The gluteus medius wears many hats. It helps to flex and internally rotate the hip, as well as extends and externally rotates the hip. It also abducts the leg (moving it away from the midline of the body) as well as stabilizes the pelvis when shifting weight (i.e. placing all of your weight on one leg while waiting in line at Macy’s). We can develop trigger points in the gluteus medius that will send pain right into our lower back and coccyx region. This guy will also refer a lot of pain down into the hamstring as well and can be very tender to even lay a finger on, but doing so will reap big rewards lessening our back and hip pain.
The Gluteus Maximus
Development of the gluteus maximus is what has allowed human beings to stand upright and separate us from our primate ancestors. The gluteus maximus is one of the strongest muscles in the body and also consumes the most calories when being activated but you wouldn’t know it looking at contemporary American society. As an outsider looking in you would think it was just a large pad to cushion our pelvis as we sit all day long in various seats of either modalities of transportation or workspaces. While it does not contain any trigger points that will actively cause back pain, neglecting to stimulate the gluteus maximus muscle will cause it to atrophy (decrease in size), and weaken which will place more stress on the lower back muscles to keep the spine erect. Case in point, you never see an elderly person who has C-spine and large gluteus muscles. Their back literally blends in with their tush!
The primary gig of the gluteus maximus is to extend the hips, which makes it a prime mover in walking and standing from a seated position. I hope you like your rump nice and hot because we will be doing plenty of exercises that will stimulate it in ways you never thought possible
!
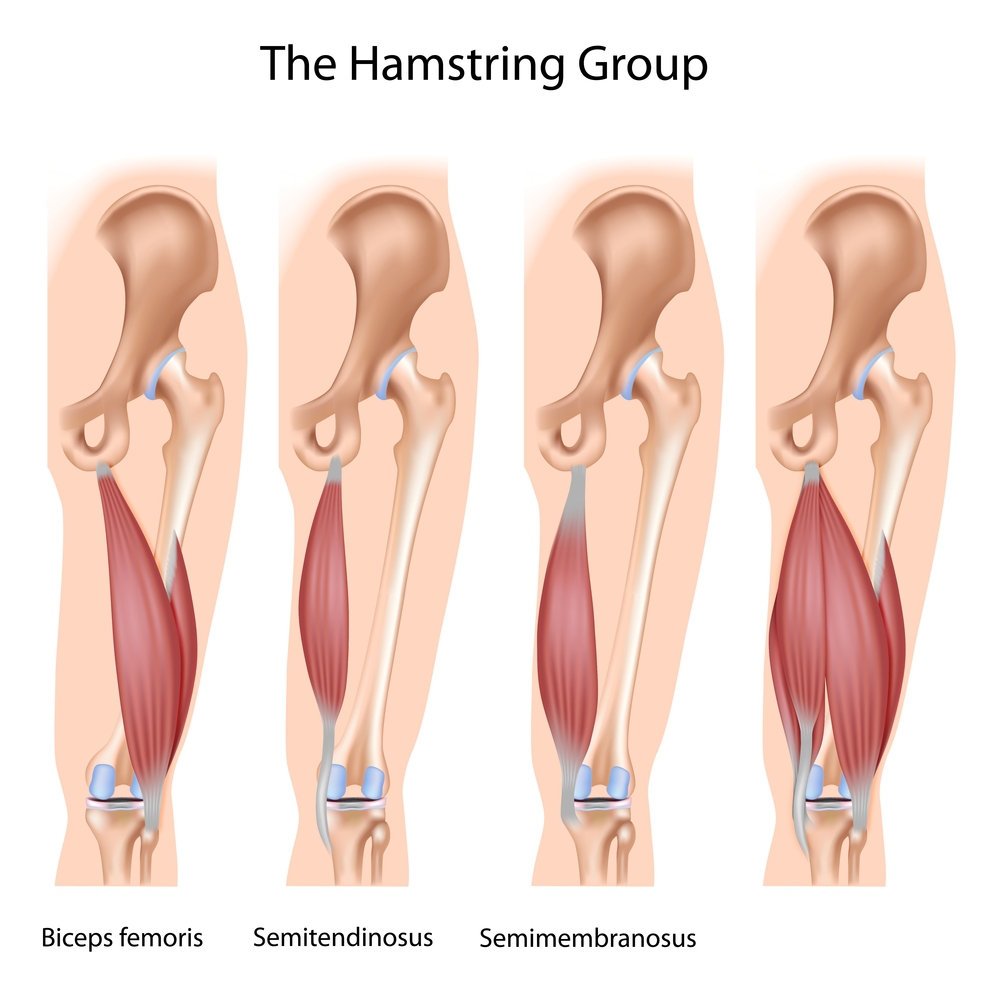
The Hamstrings
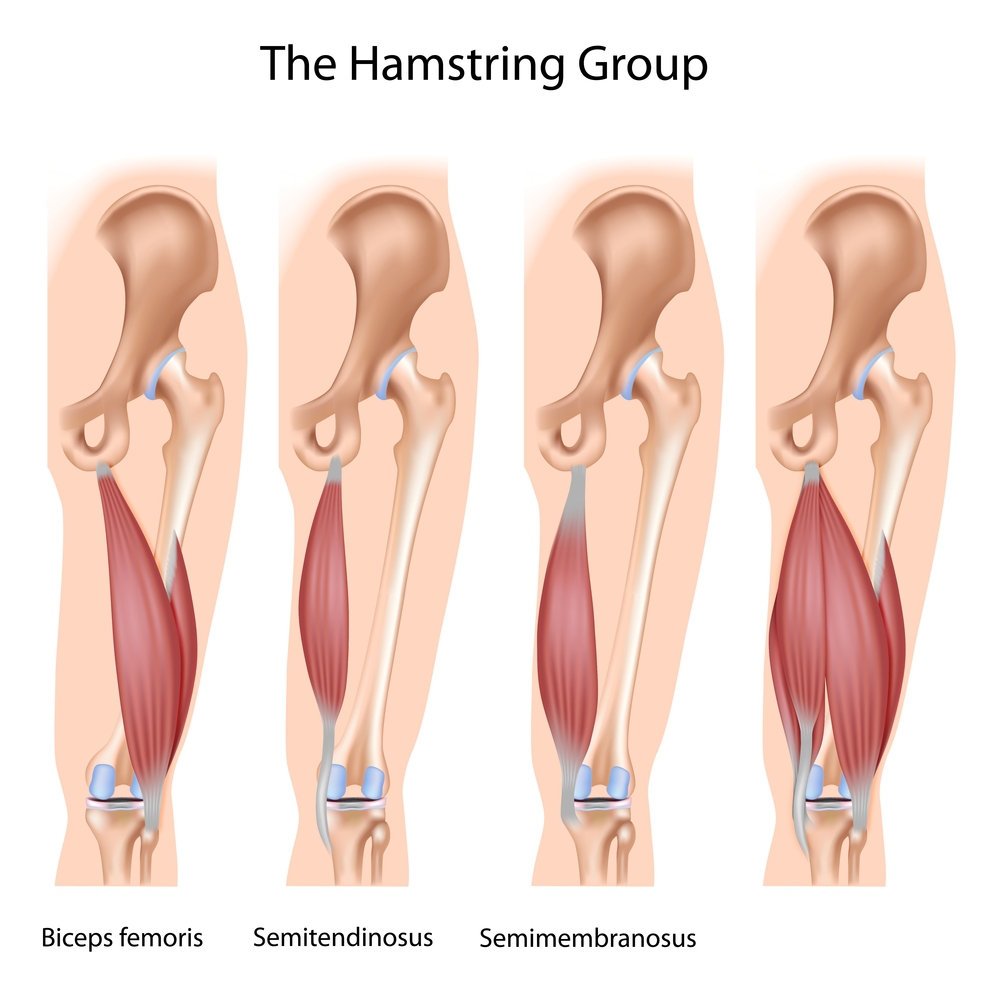
Technically called the biceps femoris, the hamstrings, have not two, not even three, but four muscles as you can see in the picture. I think it was one of those times where we may have named something before we actually studied it, but I digress. The hamstrings are important because they are called upon second to help the glutes do their job before the back is. The correct firing order is glute first, ipsilateral (same side) hamstring second, contralateral (opposite side) low back muscles third. When the hamstring is tight, or weak and not doing its job properly, who do you think picks up the slack? Your good old friend the low back, that’s who. Frequent and prolonged sitting can easily create trigger points in your hamstrings, tightening them more and more, rendering them completely useless. Doing a yoga class or two may show signs of improvement, but continued stretching of trigger point laden hamstrings will only tighten and compress the knots which will then start sending pain into the calf muscle leaving practitioners really confused and you really frustrated. We need
pressure to release the trigger points; only then can we start to stretch them and return them to a happy length.
Bonus: The Deep Muscles of the Pelvis
While not contributors to too much back pain, the deep muscles are worth noting because if they are tight, they will cause the foot to turn out in our no-no duck walking fashion. Traditional tests for glute tightness will check out okay, but subjects will only be able to achieve partial ranges of motion in a squat at best. Forcing beyond a 90-degree knee position in a squat will be impossible unless one turns their feet out sharply. This will cause a tremendous amount of instability at the knee, and way more than normal hip flexion in order to get down deep enough. Access to these guys is tough because of the thickness of the gluteus maximus and is best addressed by a manual therapist. This doesn’t mean you can’t roll a lacrosse ball on them in your spare time though and get
acquainted. I call them generically your deep rotators, but here are their specific names:
Piriformis
– most of you have heard of this guy because when he tightens, he puts pressure on the sciatic nerve, which is not so fun.
Superior and Inferior Gemellus
– These guys laterally rotate your thigh. When these tighten, your foot position will become altered to the dreaded duck position.
Obturator Internus
– Laterally rotates femur (pointing the toes out again!)
Quadratus Femoris
– Another lateral rotator of the thigh and hip stabilizer.
Although this section may seem pretty straightforward, there are plenty of gems hidden in here. The better you understand this chapter, the better you will be able to sense your own tightness and ultimately your own path to wellness. Without further adieu, let’s get to the fun stuff now!
Ask the Coach: What About Icing My Back?
Without any of this prior knowledge I made one of the greatest mistakes of my life when my back was hurt. I actually used heat, not ice. With all the confusion surrounding my injury I reduced myself to electrical stim treatments in the athletic training room, and combined it with some stretches I found on the Internet. I would do these twice a day, after my 6 a.m. women’s basketball team, and then before I exercised (upper body only obviously) at 4 p.m. The reason I used heat was simple;
for comfort. Who wants a massive bag of ice thrown on their back at 7 in the morning? After the first day I used ice I got up from the table and started walking stiff as a board – my back almost hurt more! When I switched to heat however, it was not only more comfortable, but when I stood up from the table I couldn’t believe how loose my back felt. As a budding young physiologist, rather than overthinking the situation, I just went with what felt better. Surely I’m not just telling you to stop using ice based off of a feeling? Nope, I’m sure not!
In November of 2005 an athlete of mine had a received word that the Chicago Bears were coming down to watch him practice and then play in the upcoming season finale game against nationally ranked Washington State. The problem was the scouts from the Bears were coming down to see him Thursday, and he had just twisted his ankle badly in practice on Monday. He called me in a panic and I quickly took to the World Wide Web to find a quick, reliable solution.
All of my research led me to a book by Coach Dick Hartzell, the creator of Jump Stretch Bands who wrote a book called Don’t Ice That Ankle Sprain!
In the book, Coach Hartzell explains how ice constricts blood vessels, restricting blood flow to the ankle as it tries to heal. He recommended heat, and some mobility work with bands in order to free up the ankle from its injury and help return its much-needed proprioception. The technique worked like a charm. My athlete hobbled into my apartment, and after about an hour of the band work and some light massage around the calf and ankle, he was
sprinting at 90% capacity up and down my hallway. I was amazed.
If you haven’t gotten the feeling by now, let me come right out and tell you – I’m a physiology rebel! I don’t really like tradition, or following in someone else’s footsteps. I want to be on the cutting edge of treatment, or blazing a path for others to follow. I love debunking myths and succeeding where others with more illustrious credentials have failed. I’ve had my athletes and patients practice what I have taught them in a public gym and they always come back to me and tell me how someone with some kind of certification told them what they are doing to their shoulder/knee/back etc. is not good for them. I instruct those who work with me to politely say, “Thank you for the help,” and never to argue with them. They don’t know what they don’t know, and it’s not their fault.
I now never use ice in any situation except post injury, or post operation to 12 hours after and in the knee only. All other situations I instruct people to use heat and mobility, or self-applied massage only and here’s why: In 2012,
a study in the British Journal of Sports Medicine
showed that there is no clinical evidence ice improves the healing of muscle strains. Consequently, there was also a study published in the 2013
Journal of Strength and Condition Research
showing that icing can actually hinder recovery from eccentric muscle work. In another 2013 study involving eleven 20-year-old male baseball players, topical cooling caused a significant increase in muscle damage markers during recovery from eccentric exercise. All of the pictures you see of athletes jumping in ice baths post workout, or post game seem silly now
doesn’t it? In all honesty it should be illegal. A 20-million-dollar-a-year athlete doing damage to his body willingly! Let us continue though.
A research study published in 2012 by the
Journal of Sports Medicine
showed that in 25 separate studies, 75% of them reported a decrease in muscular strength following icing. There was also evidence from six studies that cooling adversely affected speed, power, and agility-based running tasks. So when Jimmy, the high school running back, bangs his knee, gets a pile of ice thrown on it, and then returns to the game like a champ, we are asking for further injury to the area.
Icing is really just a great placebo effect. It is great at decreasing pain—no doubt—but in the process we are not letting our body heal correctly. When an injury occurs, the body's repair mechanism comes in the form of inflammation, which contains all of the healing components. Why do we want to decrease the availability of these healing components by using ice and shunning inflammation? Why do we think our wisdom is greater than 4 million years of evolution? As I said before, the only time ice should be permitted is post-operation when inflammation needs to be controlled due to the invasive process of surgery. All other injuries should be heated to increase circulation and nerve conductivity (researchers believe ice slows down nerve impulses), mobilized in a somewhat pain-free manner, and continuously massaged to prevent the formation of scar tissue and help move along the process of draining the inflammation into the lymph nodes
.
We also find out in an article on
caringmedical.com
that peripheral blood perfusion can be reduced while icing which means that blood vessels constrict and shut off blood flow that brings in healing cells. Depending on the duration of the icing, it can take up to several hours for the blood vessels to open back up again. This can in effect cause the damaged tissue to die, and permanently damage the nerve. I don’t know about you guys, but I like my nerves alive, not dead.
There is a gigantic difference between speculation and experimentation. I have had nothing but phenomenal results treating injuries, sore muscles, and joints, as well as post-op patients with heat, movement, and foam rolling for over 11 years now! So there you have it, you are under strict orders to get in the hot tub, or your favorite Swedish or infrared sauna to help relax your pain away. Leave the ice baths for the polar bears!