Chapter 5 – Step 1: Mobility
"All that man needs for health and healing has been provided by God in nature, the
challenge of science is to find it." Philippus Theophrastrus Bombast that of Aureolus Paracelsus (1493-1541)
Annie came to me in pretty bad shape. Her pain was the result of poorly applied therapy after a bad car accident when she was on college. She was now 45 years old and her husband had to help her to walk from the car to come see me. Listening to Anne talk you could sense the fatigue and desperation in her tone. She was tired of her back going out on her leaving her in bed or on the couch for sometimes up to two weeks. She was tired of missing out on the days her husband would take their two kids to the beach or on the boat to wakeboard. She was tired of all the worry she had surrounding her movement everyday. She had lost her motility and the plethora of practitioners she has visited over the years made for a pretty impressive conversation over cocktails, but that was about it. Nobody could figure out how to help her. Was she broken? That’s the first question she asked me. I assured her that as long as she could get to me she was not the least bit broken. “We are all different, but the
same,” I told her. We each have the same capacity for injury as we do to heal; we just need to be in the right care.
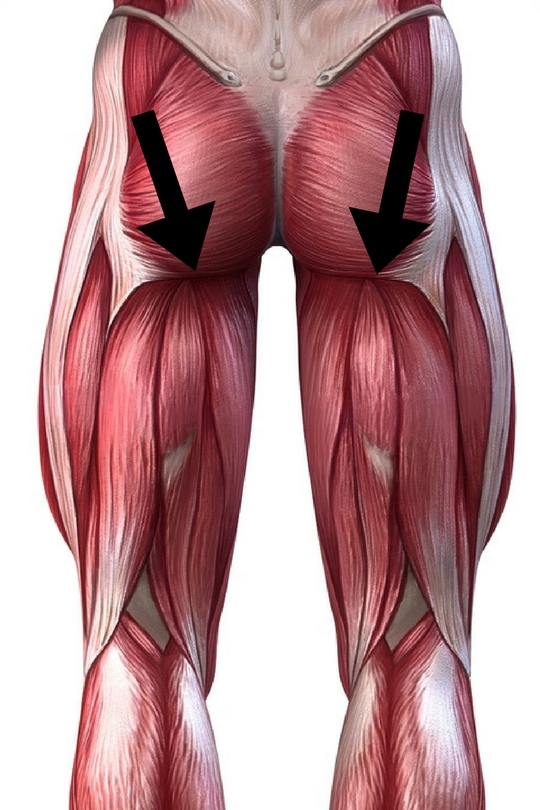
Careful inspection of Annie showed tightness in her right glute/hamstring complex, which carried up to her left shoulder. She had been favoring her left leg for 25 years! Through vigilant application of our mobility and motility exercises, Annie was pain free after four months and even became a member of my gym, dropping nearly 30 pounds and increasing her fitness to pre-college levels! Her story is one of my favorites to tell not because of the success we achieved, but because of the hardships she endured along the way.
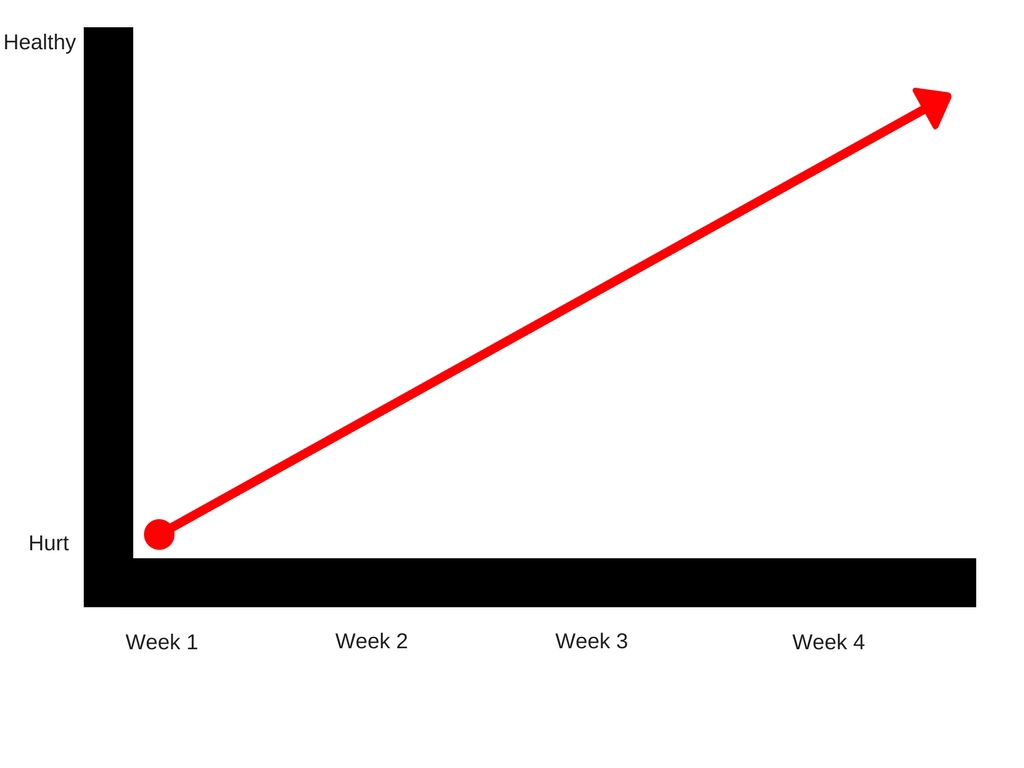
People feel a return to health should always be an ascending line, and this may be the case if your pain is just developing.
Sample timeline of a person with pain for less than 3 months
.
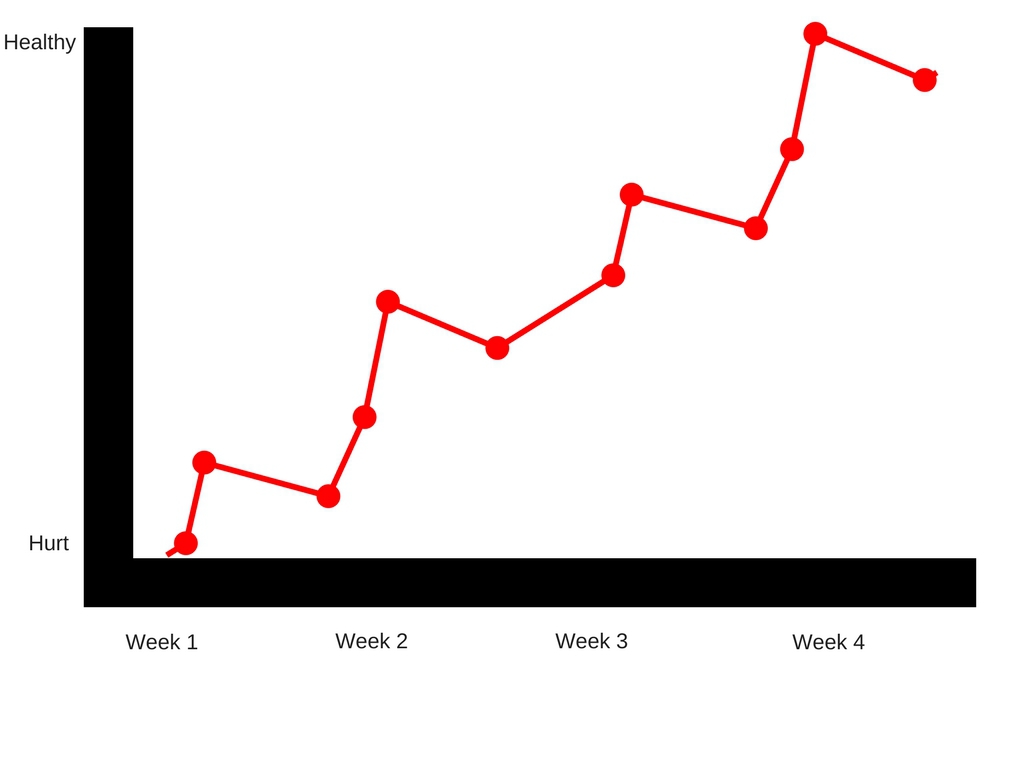
When you have been in pain for as long as Annie had been, your return to health will look a little more like this:
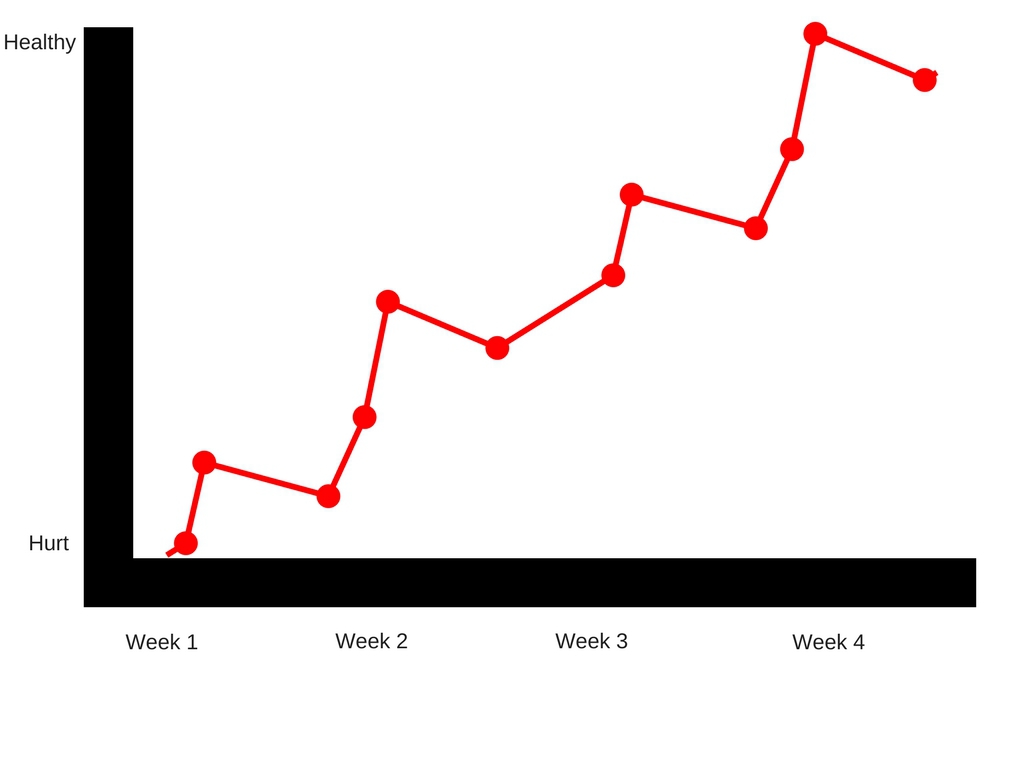
Did Annie have some setbacks? Absolutely! And I told her to expect them. Her body had created what I call “functioning chaos,” which meant anyway it could develop force for her to traverse the physical plane it did so at the expense of her muscles, tendons, ligaments, and ultimately her joints. We had to break this chaos down and restore order to her movement. This neuromuscular reeducation will sometimes cause a spasm, or the brain to go on high alert. This is because we are making swift changes to the body’s structure and if it does not calibrate just as quick, it will force you to slow your movement down. This is where our patience and persistence comes in. Even though we may be hurting, we are not hurting the body. I was providing a paradigm shift for Annie no other practitioner was willing to take her through. We adapted to her body’s responses and adjusted our exercises accordingly to the imposed demands. As we slowly put her blocks back together, her brain, and
central nervous system calmed down and stopped referring pain.
Called to Care
I love you. I love everyone who comes looking to me for care. That’s why this book is dedicated to you, the reader. I know it sounds cliché or corny, but there were plenty of times in my life I was in pain and there was no one there to help me. Those who tried, tried diligently, but just didn’t have the right answers and that’s okay. Fixing me wasn’t their calling, it was mine. I’m one of the lucky few who don’t question why I’m here, or what my purpose is. I am constantly called to care
for those who are looking to take their pain away for good. My success rate is dictated by holding the space for you to heal. With malpractice suits flying around like Boeing 747s these days, it’s no wonder doctors and physical therapists shake their heads and send the tough cases packing. If someone is treating you based off of fear first, your treatment will be limited. I’m not saying all practitioners are like this, but it’s safe to say some (if not a majority) are.
If you get anything out of this book know that I believe in you. I believe you are in pain, and I believe you want to be happy and healthy again, regaining your freedom of movement. While I do get stumped sometimes, our body will always show us signs of ways to heal it. Pay great attention because this could be as slight as a buzzing sensation, or in some cases may come as a loud crack or pop. Whatever the case is remember you always have me in your corner! Experience has shown
me that some of the movements I teach in this book can be quite tricky to understand through just pictures and text. As a result I created a video library of all of the movements so you can follow along and better understand how to perform them. Included with the videos is also a three month program to help accelerate your success. If you feel this is something you may want to take advantage of, please email me at
chris@influentialhealthsolutions.com
and I will give you directions on how to do so!
In other cases there are some people that don’t feel comfortable doing any of these exercises by themselves. I completely understand because the methods I put forth in this book are a completely new way of ridding pain not only in the lower back, but the entire body as well. That being said, if you would like a free consultation or to work one-on-one with me please e-mail me directly at
chris@influentialhealthsolutions.com.
Abdominal Mobilit
y
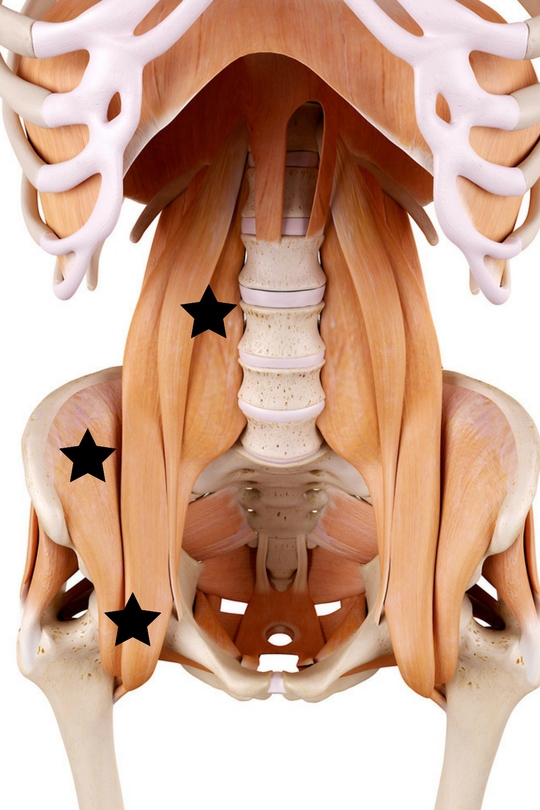
Remember how I told you that the abdominals are pretty much worthless when trying to heal your back? Well that wasn’t entirely true. It is well documented that there are some pretty serious trigger points in your abdominals that refer pain directly into your back as indicated by the pictures below:
Trigger Point Locations
Back Pain Referral Pattern
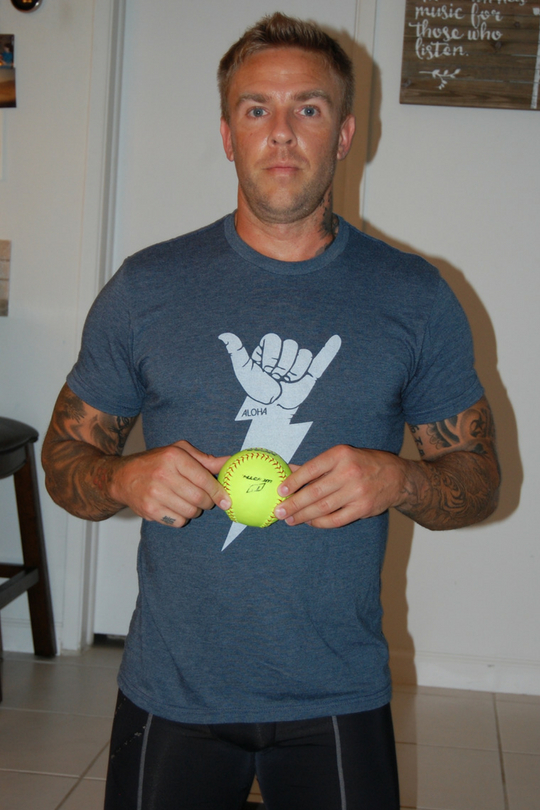
Rolling out your abdominals at first may seems strange and feel highly unpleasant, but I have had the most immediate relief in back pain, and increase in hamstring flexibility come as a result of doing so. This mobilization will pay off in big dividends and that is why I am putting it first. Here is your model for releasing your abdominal trigger points:
Method – Lying on your stomach placing direct pressure, or stirring the pot by rolling around searching for any tissue that sends pain into our back. Support yourself with your elbows or your hands, you do not want to swan dive on to the ball!
Modality – Softball.
Time – 6-10 minutes on the entire abdominal sheet
!
Ball Placement
Lying on your stomach with elbow support
If your results are limited on the ground, you may want to try using the back of a chair, or sofa and leaning into the ball to apply deeper pressure:
Trigger points are interesting due to the fact that they refer pain into seemingly unattached muscle groups. By now you, the reader knows this makes perfect sense because the body is a web and completely connected! By attacking the abdominal trigger points first, we loosen what may be causing the back to feel painful and tight before we roll the back, getting much more out of our back mobility exercises
!
Hip Flexor Mobility
Such a critical muscle for not only support, but also vitality, you know we were going to go hunting around in here to lengthen and restore their proper function. The flexor trigger points are deep and very difficult to get to. Due to their depth they must be stimulated slowly and carefully. Here is your model:
Method – Lying flat on your stomach, place the ball at the lowest trigger point area. Once you have found the spot lift the same leg of the side the ball is on, and the opposite arm, supporting yourself with the opposite arm and leg still on the floor. Return your arm and leg to the floor and repeat as many repetitions as possible.
Modality – Softball.
Time: 2 minutes for each trigger point.
Trigger point location
Back Pain Referral Pattern
Ball Placement
The ball is on my right hip flexor, so I raise my left arm
And my right leg
Be patient as we are using a pumping action to get the trigger points to release. If you feel comfortable enough while doing this mobilization, you can also relax
and apply some direct pressure to it. This is common sense but needs to be stated. Your gut along with a lot of major organs lie close to your hip flexors, which should dictate caution on your part. Do not press into any area that is referring intense pain into your gut. If you are on the trigger point and it is a normal muscle soreness that is fine. If the pain is going into your back even better! These are both great mobilizations, but because of their sensitive nature not a lot of practitioners will advocate their use. I on the other hand have found way too many problems in these muscles to omit them, and still be able to sleep as soundly as I do. Bottom line is to be gentle, and use caution and you will produce a win-win for your back!
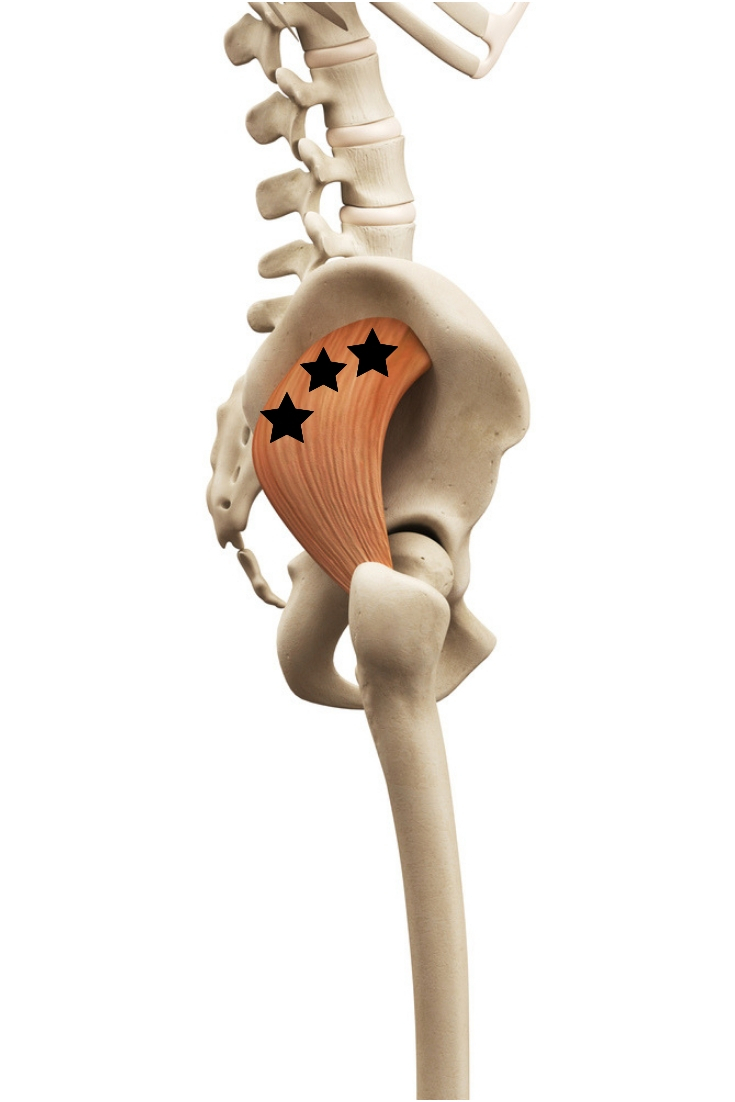
Gluteus Minimus Mobility
While most of the pain from a tight gluteus minimus will refer pain down the leg creating what I call “fake sciatica,” it will feel as though there is an inability to bend over fully and a slight pull on the lower back. We kill two birds with one stone utilizing this mobilization. If the trigger points are active, you may feel pain traveling down your leg. If the muscle is only tight, then the mobilization will still be sore, and your back will feel a lot looser when you stand up. Here is your model:
Method - Lying completely on your side, place the ball at your belt line slightly under the top of your hipbone. Keep that same leg straight, and bend the opposite leg placing that foot on the floor. Allow all of your weight to sink into the ball on the gluteus minimus and focus on breathing to release and relax that muscle
.
Modality – Ideally a lacrosse ball, but a baseball can be used at the beginning if a lacrosse ball is too sore.
Time – 4 minutes per side.
Gluteus Minimus Trigger Points
Ball placement
Lie on your side, opposite knee bent, and foot on the floor
I can’t over-emphasize how important this mobilization is, or how sore this overworked, and underappreciated muscle can be sometimes. Many people have never even heard of this muscle before, but never forget it again after their first time applying pressure to it. If the pain exceeds our 6-8 ranges, use a larger ball, or take breaks until you have achieved the prescribed amount of time.
Gluteus Medius Mobility
Flying low under the radar, gluteus medius trigger points can create a lot of pain in the back and the hamstring. This will cause both to feel tight and not function too well, which will prompt you to feel like you have to stretch them. Stretching will tighten the trigger points, but lengthen the muscle giving you a false positive which means you’ll feel looser, but more pain will develop. Not good. Here’s your model:
Method – Using a lacrosse ball, lie on your side like you are going to mobilize your gluteus minimus. From there,
turn your body slightly and roll it along the crest of your hip where the trigger points are located in the diagram below. This is a somewhat funny position because you are not on your back and you are not directly on your side. You are in between both of those positions.
Modality – Ideally a lacrosse ball, but a baseball may be used at the beginning if the area is sore and referring pain above our 6-8 tolerance scale.
Time – 4-6 minutes for this bad boy!
Gluteus Medius Trigger Points
Back Pain Referral Pattern
Ball position
Lie on your side and roll the ball into position while not directly on your side and not directly on your back.
Notice, my left hip is still off the ground, and the ball is on my right gluteus medius.
A tender gluteus medius will present itself very quickly. You may experience some pain traveling down the hamstring when on the ball, and also in the area of your coccyx. This is how you know you’ve hit pay dirt! Direct pressure works, and so does a little side-to-side motion. Be patient and listen to what your body is telling you, you are your own best therapist!
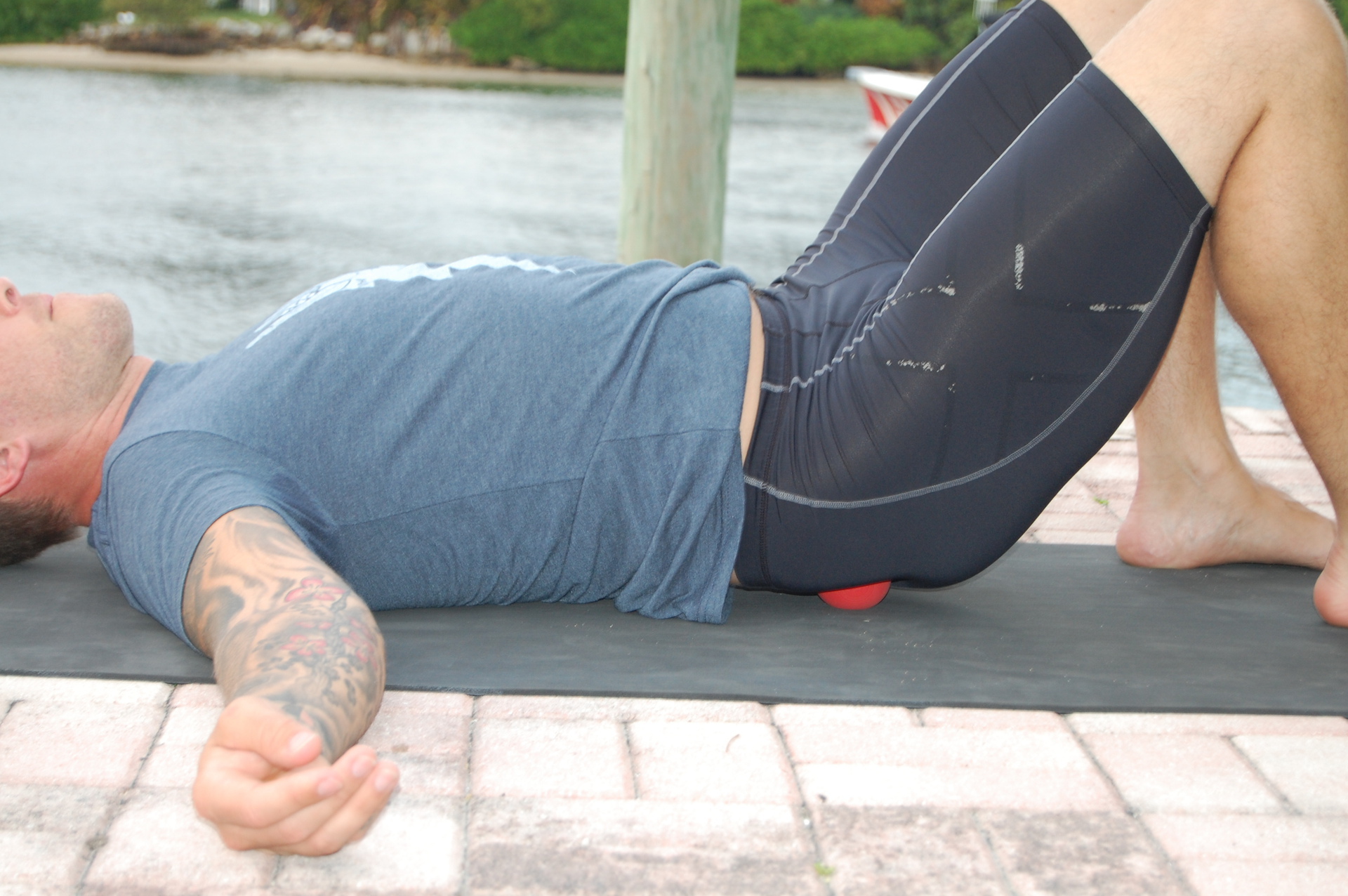
Gluteus Maximus Mobility
While not really a major contributor to back pain due to trigger points, a tight glute max can hinder our hip mobility, locking up our back and hamstring. Mobilizing the glute max is fairly easy, but also where most people go wrong missing the gluteus minimus and medius completely. No rocket science with this one, here’s your model
:
Method – Lying on your back, place a lacrosse ball squarely under your glute max and stir the pot moving the ball all over, utilizing your bodyweight for pressure.
Modality – Ideally a lacrosse ball, but you can start with a baseball or softball if your glute is on the sore side.
Time – 4 to 6 minutes of continuous pressure, moving the ball frequently!
Gluteus Maximus Trigger Points
Lying on your back, place the ball in the middle of your glute and roll with both feet on the floor.
This is one of the easiest mobilizations you will be doing and can often be passed up because of this. Make no mistake; a mobilized glute is much better off than a non-mobilized glute. The pressure will keep the tissue open and free from trigger points caused by excessive sitting and in some cases standing.
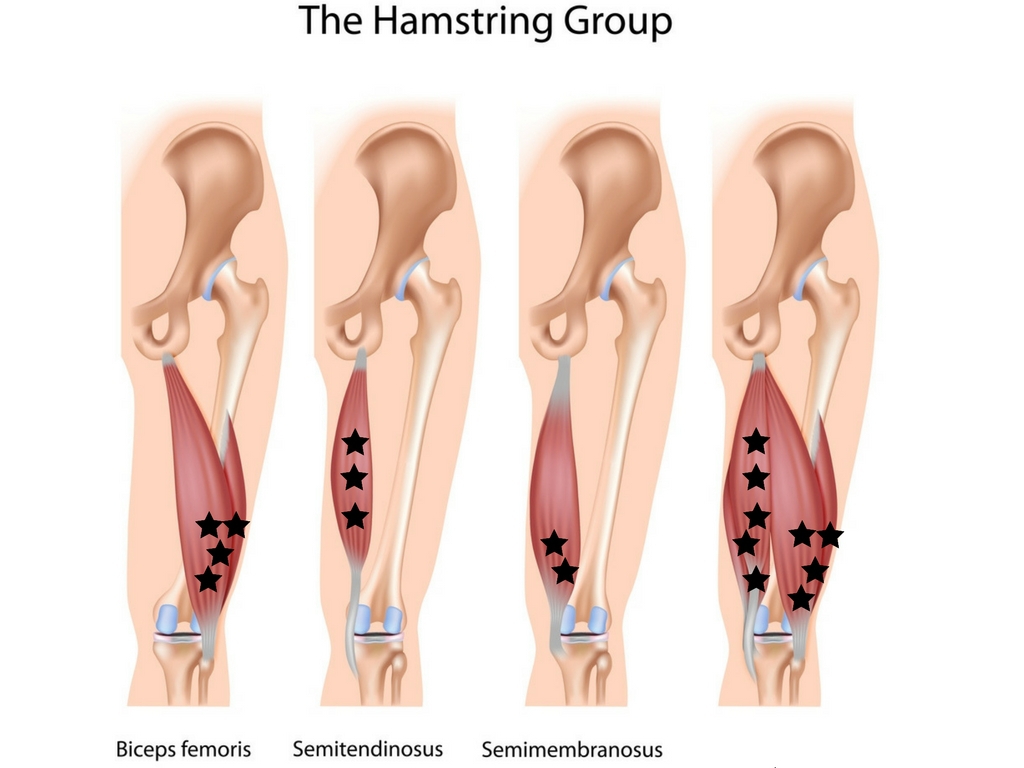
Hamstring Mobility
The hamstrings are second in charge to help the lower back do its job. Tight hamstrings create more work and more pressure for the low back muscles and disks to work with. Sitting for prolonged periods of time can
easily create trigger points in them, which automatically create a shorter, tighter muscle without us even realizing. Here’s your model:
Method – Seated on a counter where the foot can dangle. Place a softball under your thigh and relax your leg. Drag your hamstring on the ball from hip to knee repositioning the ball as necessary. Take note of any bumps, lumps, or hard tissue and focus your efforts in those areas.
Modality – Start off with a softball, then graduate to a baseball when it becomes ineffective.
Time – 4 minutes.
Hamstring trigger points
Sitting on the counter, position the ball under your thigh, directly on your hamstrings.
One of the best ways to get more pressure into this mobilization is to introduce movement by extending your lower leg while pinning a tight area down. This is a great way to release adhesions and “unglue” the fascia. Is it still not releasing? Decrease the pressure and increase the frequency at which you extend your leg. Like I said before, mobility is not just about how much pressure you can force on the muscle. The structures underneath (nerves, blood vessels, lymph tracts) are sensitive to pressure as well. Too much pressure and the body may think it is incurring an injury and lock the site down.
Into the mind of the coach: Knowing your “WHY.”
With the detail procured to write this book, by now I’m sure you know nothing to this program is random. There is order to everything. Will you get results by going out of order? Sure! However, by going in the order I tell you your results will be optimized
. Not only
are we following the firing patterns for human movement (hip flexors > glutes > hamstrings > low back), but we are also loosening and unlocking the hamstrings before we mobilize them directly. This is because the hamstring tendons emerge from under your gluteal muscles. Tight gluteals will clamp down and shorten your hamstring tendon, tightening the hamstring even though the muscle may not contain any trigger points!
Restoring these damaged, tight structures in order not only sends the right signal to our brain, but also makes the process of returning to health 3-5x easier. Now, let’s go see what lies in store for that ailing low back of yours!
Lower Back Mobility
Far from the workhorse, I would more so call your lower back command central. Not that it tells any other muscle group what to do or how to fire, but it commands that they do their part and function correctly or else! Truth be told, we do abuse our lower backs on a daily
basis. From the shoes we wear (ladies go above and beyond with their high heels), to the seats we sit in, to the posture we function in, to the way we pick things up without thinking. This is what makes the lower back muscles the workhorse – the sheer abuse they must endure! Your back muscles take very good care of you. They help you move to get to wherever you want to go. When someone comes to me complaining of acute back pain I say, “Your back does a lot for you, what are you doing for your back?” After my weightlifting accident I promised myself I would never entertain back pain again – once was enough. My routine now dictates around 7-10 minutes of daily back mobilization, which allows me to compete at a high level for my age without any back-related pain. This mobilization helps me relax and melt any weightlifting soreness away. Here’s your model:
Method – Lying on your back with the roller underneath your hips, start with your hands at your sides and palms down. As you roll up your back to the base of the neck, slowly move your hands overhead at a steady pace. Return down to the hips, moving your arms back to the start position.
Modality – Foam roller.
Time – 8 to 10 minutes
.
Start at the base of your spine, hands at your side
Next, coordinate your arms with the position of the roller
As the roller ends up at the base of your spine, your hands should be in the overhead position.

The reason we want to roll the entire back and not just the lower part is because our back is one big sheet of tissue called the thoracolumbar fascia. This layer of fascia attaches to our spine, ribs, pelvis and all of the small and large muscles attached to them, but also has an influence on the abdominal wall. We know pain travels, and as it travels it distorts muscle tissue. You may not have any pain in your middle or upper back, but because it is attached to this fascia, you can be sure there is something brewing in there. This technique is as much preventative as it is restorative and it truly shows the interrelatedness of all of the muscles and its fascia in the trunk of the body. As we said earlier the body is a closed loop; a continuous circle of intertwined tissue penetrating through all things – even bone and organs. It only makes sense that we start with the abdominals, then work the hip flexors, then work the glutes, then work the hamstrings, then work the back, which affects the abdominals again
.
When our back is in pain, it’s likely that more than one of these muscles is tight, irritated, or containing trigger points. Go through the entire system and check off where you have to work more, where you can work less, and which muscle, or muscles you may not have to work on at all. It’s good to stimulate all tissue with pressure from time to time, but if you’re hammering away at a glute minimus of yours for 6 minutes and there’s no tender areas or pain being referred, it’s safe to say that muscle is sound. Work smart, not hard because working smart is working hard!
Pro Tip: Roll out your back before and after the Chiropractor.
Many of the people I have worked with have asked me if I believe in chiropractors, or if they are worth going to. My response is absolutely, as long as you’re doing your part as well. What’s your part? Foam rolling your back for starters before you go to see the good doctor. Adding the gluteals to that list wouldn’t be such a bad idea either.
Vertebrae do not sublux on their own. Poor movement, which leads to muscle spasms, is to blame. What else attaches to the spine but our muscles? Rolling your low back and gluteals before seeing your chiropractor will gently warm the muscles up, loosening the grip they have on subluxed vertebrae making the adjustment more productive and easy. Rolling them after the adjustment helps keep the muscles calm now that the vertebrae are back in their normal place for optimal health
.
Ask The Coach: Sitting or Standing Desk?
Best selling author Kelley Starrett puts it plain as day in his new book Deskbound
when he said, “The typical seated office worker has more musculoskeletal injuries than any other industry sector worker, including construction, metal industry, and transportation workers.” The problem exists because the typical office worker does not exert enough physical force on a day to day basis to uncover these musculoskeletal injuries, so they stay hidden for years until chronic pain develops and by that time it is very challenging to reverse said injuries. I’m sure you’ve heard sitting is the new smoking several times, yet we continue to sit. What’s worse is prolonged sitting followed by intense exercise. For some, exercise is an afterthought or done with haste. You sit at work for nearly 8 hours, sit in traffic for an hour on the way home, then jump out of the car, change clothes in a rush, do a stretch or two and then pound the pavement as fast as you can for 20 minutes. Some of you may be saying, “But I don’t have time to warm up!” Ask yourself this: Will you have time to heal yourself when an injury strikes?
I’m guessing you won’t have time for that either. There are some staggering statistics surrounding the potential sitting has to create disease in the body when there was none. Here are some facts taken from standupkids.org showing what even 2 hours of sitting per day can do:
Sitting literally turns your brain, and your body to mush. The posture most of us sit hours with would not be sustainable for even 5 minutes standing, the pain would be too great to bear. A simple search on Amazon will produce a wide variety of standing desk options from $29 all the way up to over $5,000 in some cases. Choose which option is best for you and join your fellow rebel bipeds!
As always, we ask, “What can I do right now?” I’ve mentioned my 20/20 rule, but it bears repeating here again. Every 20 minutes get up and do something active or athletic for 20 seconds. Be silly and move every joint in a full range of motion. Do Burpees or a cartwheel. Stimulate your muscles and your brain to stop the subsequent decay of both. Your health is in your hands every day, don’t take your movement for granted, and realize this precious gift we have all been given and all have the ability to keep if we so choose.