Chapter 18
Dental Work
In order to completely recover your health and to go on to live into a vigorous old age, you may need to commit to having some dental work done (depending upon your current status). This aspect of treatment should not be undertaken lightly because:
• There are often significant costs involved.
• There is often quite a lot of trauma and discomfort involved in possibly having work that has been placed over a lifetime replaced wholesale, especially whilst you may be relatively unwell.
• You may need to travel some distance to see a dentist skilled and knowledgeable in this area.
• This work may also require a considerable commitment in terms of time, not only for yourself but for anyone who may need to accompany you.
• There may be additional expenses such as fees for laboratory testing, intravenous chelating agents or anaesthetist’s charges.
• You need to be on a systematic detoxification programme before, during and for some considerable time after dental treatment.
• If not managed effectively, your health can deteriorate even further.
Amalgam Replacement
Tolle causam. (Find the cause.)
The foundational principle of naturopathic medicine
The first common sense rule of treatment for any illness is to remove the cause of the problem, if possible. However, all studies show that the removal or placing of amalgam fillings increases the amount of mercury in circulation for many months afterwards. For this reason, a lot of dentists will not replace amalgam fillings without good reason and, of course, the current official line is that the mercury in amalgam does not pose a health threat. In any event, the replacement of amalgam fillings should not be attempted until a lot of your toxic metal load has been dealt with and you are substantially well enough. Careful replacement of amalgam fillings can help some people practically overnight, but if performed without due care or at the wrong time, it can also make some sick people a whole lot worse. This is a specialist job and whilst any dentist should have the technical ability to do the work, not all are aware of the serious health implications of what they are doing in someone whose health is already seriously compromised by mercury toxicity. Some specialist dentists will test the galvanic charges on your amalgam fillings and then remove them in sequence – from those with the strongest negative galvanic charge (which are thought to emit the most mercury vapour) to the least reactive. If you can’t afford to have all your fillings replaced, you may at least choose to address the worst offenders on this basis. Alternatively, some authorities recommend removing one filling at a time and spacing the appointments at least six weeks apart to reduce any single exposure to mercury vapour.
To find a dentist knowledgeable about amalgam replacement, either ask around, contact one of the organizations listed in the Useful Contacts section or try an Internet search. It is worth ringing the dental practice and asking for an information pack. The dentist concerned should have done amalgam removal courses and ideally would be running a dedicated amalgam-free practice. Any dentist who takes this work seriously should be equally serious about protecting themselves and their staff by taking supplements and using protective equipment. However much you may like your regular dentist, if you have decided to have your amalgam fillings replaced, go and see someone who is an expert in this area.
Recommended Technique
• The dentist should use a rubber dam (a rubber sheet that isolates the tooth/teeth being worked on and serves as a barrier).
• The dentist should provide oxygen while removing the filling(s), and use a nose piece or a damp cloth over the nose.
• Some test the galvanic charges on your amalgam fillings and then remove them in sequence.
• The dentist should have prescribed (or have referred you to someone who has prescribed) various supplements for use before, during and for quite a long time after removal of your amalgam fillings.
• It is thought by some that the immune system has a 7-day cycle and that it can overcome an insult on day 1, but if then further assaulted 14, or especially 21 days later, may be unable to recover. For this reason, try to avoid booking regular weekly appointments.
• Some dentists use intravenous chelating agents during amalgam removal such as 2,3-dimercapto-1-propane sulphonate (DMPS), dimercaptosuccinic acid (DMSA), ethylenediaminetetraacetic acid (EDTA) and/or vitamin C.
• The dentist may use an adrenaline-free local anaesthetic or Carbocaine, which contains only water and anaesthetic, because some FRS sufferers can react badly to regular local anaesthetics.
• Ideally, any replacement restorative materials and anaesthetics should be tested before use. This can be done by muscle testing samples, or a laboratory in the USA can conduct a metal-specific memory T-cell test (MSMT) which can determine the immune response to various dental materials.
Alternative Filling Materials
The most common of these is composite, with other more expensive alternatives including various ceramic, glass and cured-composite materials.
Composite
Composite filling material is the material that is most often used as an alternative to amalgam. It is a plastic material with grains of silica (glass) as a filler to give it durability, body and good aesthetics. It is usually placed in small increments and set with a light and then needs to be trimmed and polished.
The Advantages of Composite
Composite has several qualities to recommend it:
• It does not contain mercury, zinc, copper or silver.
• It is not a metal and so is not electrically active.
• Composite is tooth-coloured and so has good aesthetics.
• Composite fillings can be done in one visit directly in the mouth.
• Whilst it is more expensive than amalgam, it is cheaper than alternatives.
The Disadvantages of Composite
However, it is by no means an ideal filling material (because such a material does not exist) and it has problems of its own:
• Composite shrinks on setting and this can lead to leakage of the filling and ultimately to death of the nerve inside the tooth, whereas amalgam corrodes, sealing the gap. This can mean that your teeth are more likely to die and need a root-filling or extraction if you have composite fillings.
• Composite is also not as durable as amalgam. Teeth are not just for show, they are put under a lot of stress and strain over many decades. Composite fillings will most likely need replacing more often and with every replacement the cavity inevitably becomes larger, the tooth becomes weaker and the nerve inside the tooth becomes more and more compromised.
• Another issue is that the composite filling material is a monomer paste (contains short molecules) and the ultraviolet light sets it into a solid polymer (long molecules). The monomer is moderately toxic and it does not all convert to polymer and this can be an irritant to, and also effectively kill, the nerve inside the tooth. Teeth that die in this way can become incredibly painful and hard to anaesthetize.
• Sometimes, just the action of removing and replacing the filling is enough to push a (possibly not terribly healthy) tooth over the edge into requiring either a root canal filling or extraction.
• Composite can wear over time with consequent movement of opposing or adjacent teeth.
• If the filling is large, or cusps (corners) of the tooth are missing then it is not advisable to have a composite filling. This is because it may be necessary to place pins in the remaining tooth to support the filling (which crazes the tooth with cracks and may lead to the nerve dying) and these fillings tend not to survive very well.
• Bits can and do break off composite fillings, but these can usually be patched because composite can be bonded to itself (within reason).
• There is some question over the safety of composite (and some lining materials) because the plastic component may mimic oestrogen. Similar plastic pollutants are thought to be causing feminization of alligators in Florida, for instance. Many composites now contain aluminium so ensure that the composite to be used has been tested or is aluminium-free. Also, the owner will swallow the small glass particles as the filling wears and it is not known if this is safe.
• It is also technically more demanding to place a composite filling. It has to be placed in increments, ideally under a rubber dam, then trimmed and finished – which all means that they cost quite a lot more than an amalgam filling. It can also be difficult to contour the fillings between teeth and get a good contact which will prevent food from packing between adjacent teeth.
Laboratory-Made Composite Restorations
If your dentist suggests it (and finances permitting), tooth-coloured fillings can be made in a laboratory in much the same way as crowns or caps are and then cemented into place in the mouth. This is advisable for the larger fillings and especially if the tooth concerned is either a premolar or molar tooth that has been root-filled and/or has cusps (corners) missing. One material that can be used is a heat-and-light-cured version of the composite that is used in the mouth. This is more wear-resistant, is fully polymerized and cement seals any gap so that leakage is not an issue. Other options include using either a castable glass or a ceramic material. The finish achieved with these techniques will also be aesthetically pleasing, but these materials can fracture in thin section. Some ceramics also have radioactive elements added in order to simulate the fluorescence of natural teeth. Ceramics, in particular, tend to be harder than natural tooth and can lead to wear of the opposing tooth over time. However, because these techniques involve laboratory bills and extra appointments they usually work out to be many times the cost of composite, although they might save you replacement and root-filling costs in the long run. There are now also non-metal alternatives available for metal posts and ‘core’ materials (used to build up the tooth under a crown).
Some specialist anti-amalgam dentists may have an expensive piece of computerized kit that can scan the prepared tooth in your mouth and then machine a ceramic or glass restoration to fit while you wait. This means that the work can be completed at the same appointment and may work out somewhat cheaper than a laboratory-fabricated ceramic filling. It also saves having to have two lots of anaesthetic and temporary fillings.
Protocol for replacement of Amalgam Fillings
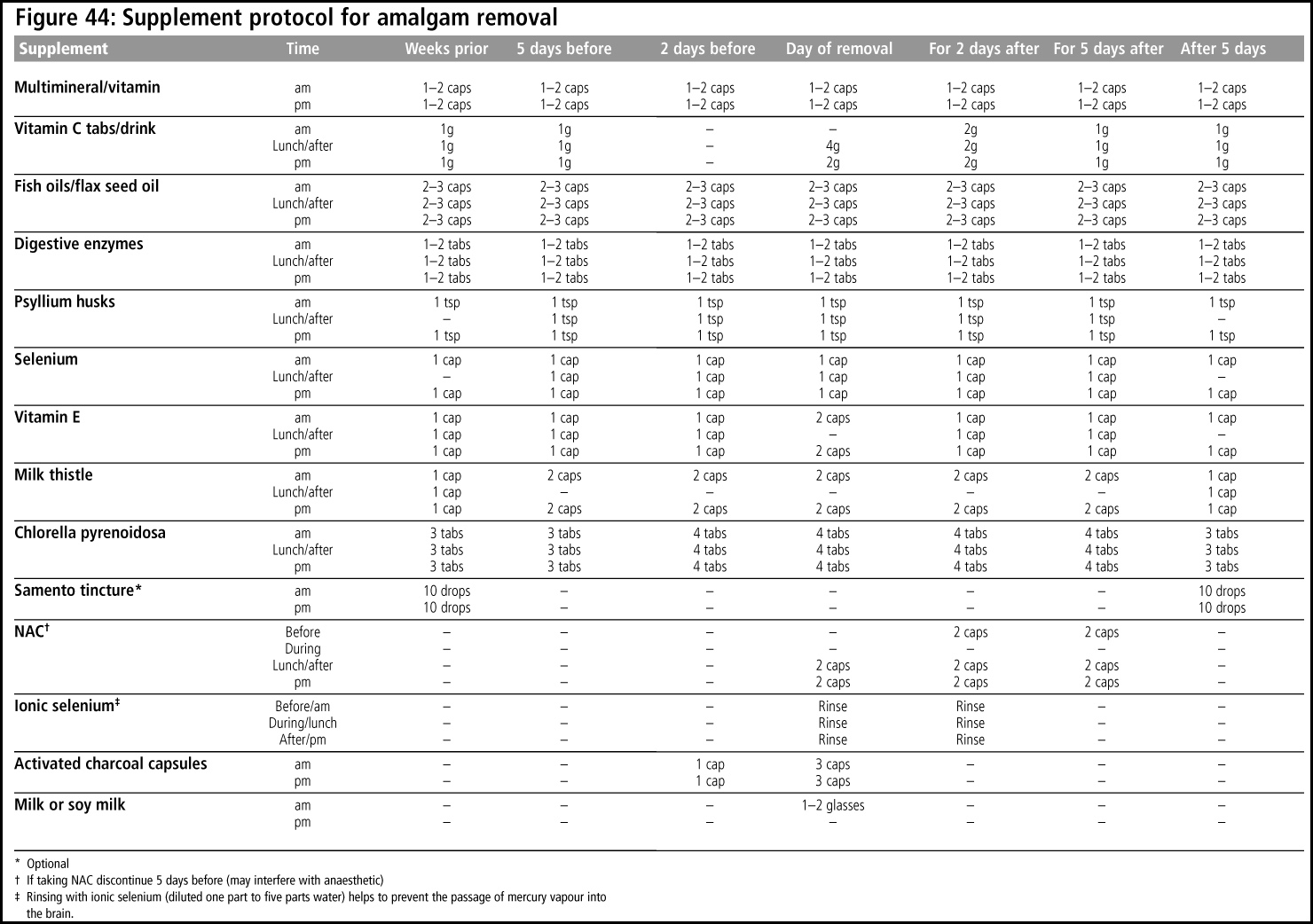
A protocol is suggested in figure 44 but you should follow the advice of your specialist holistic dentist or anyone they may have referred you to.
In particular, make sure that you are not constipated before, during or after amalgam removal, both by eating a fibrous diet and by supplementing with additional fibre such as psyllium husks. Also remember to follow the protocol for all the appointments at which you are having amalgam fillings replaced. If treatment involves extractions or any kind of surgery, the supplement Arnica when taken before, during and after treatment aids healing. Using Dr Bach’s Rescue Remedy on the day of, and for a few days after treatment, also diminishes the impact of the trauma on the body. If you are under ongoing treatment with a kinesiologist or naturopath, arrange to see them within one week of amalgam removal. Be aware that some people may have a delayed reaction months after their amalgam replacement for reasons explored earlier.
Beyond Amalgam Removal
Metals
It depends how sick you are and how much money you can throw at the problem, but some holistic dentists recommend removal of all metals and replacement with alternatives to eliminate galvanic currents (chapter 9), metal toxicity and interference with meridian energy flows. This means replacing not only amalgam fillings, but also all crowns, bridges, implants, posts, pins and any dentures incorporating metals.
Root-Fillings
Some authorities also suggest removal of all root-filled teeth. Again, it depends how sick you are, but it might be worth considering. A kinesiologist or a practitioner using some form of biofeedback such as the Vega machine might be able to give you an indication of whether a root-filled tooth is a likely causative factor or not before you take the irreversible step of extraction (also refer to figure 6). Certainly any teeth you know to be a problem such as those with an occasional infection, draining sinus (a little channel through the bone which will appear like an oozing pimple) or with compromised bone support should be extracted. Additionally, any teeth that appear on x-ray to have poor root-fillings should either be re-root-filled or considered for extraction. Dr Weston Price (see chapter 8) found that kidney and heart disease were the disorders that were most responsive to removal of root-filled teeth. More recent evidence also particularly implicates root-filled teeth as a causative factor in diabetes. Dentists who have specialized training in root-fillings are known as endodontists and you may need to request a referral for this treatment. If you have ever had a retrograde amalgam root-filling (a surgical treatment sealing the root canal from the root tip) you will need to decide whether repeating minor surgery to keep a compromised tooth is worth it in light of your general health.
Cavitations
Neuralgia-inducing cavitational osteonecrotic (NICO) lesions or cavitations are cavities within the jawbone that have been left by extracted teeth, most often wisdom teeth. If x-rays indicate that this might be an issue for you, find a specialist dentist who can perform the minor surgery of opening up and cleaning out the affected area. Some dentists with a special interest in this area may also have a piece of equipment known as a Cavitat. This provides an ultrasonographic print-out of the quality of the bone surrounding the teeth and indicates the presence of necrotic lesions or cavitations with a high degree of accuracy. A kinesiologist or muscle testing (see Appendix) may also be able to establish whether this is a causative factor in your FRS.
Joining the Dots
The US anti-amalgam dentist, Dr Hal Huggins, refers to doing all of the above as total dental revision (TDR) and claims to get good results for some very sick people. It might be worth trying to do some detective work and write down when you had dental work done (to the best of your recollection) and when your FRS symptoms appeared. See if there is any obvious culprit such as a recent root-filling, placement of a crown or bridge, or removal of a wisdom tooth that might have been associated with the onset of symptoms. Metal framework crowns and bridges (which may be covered in porcelain) placed over amalgam ‘cores’ may be particular suspects and your dental records will reveal whether this applies to you. Also consider that work done on a tooth that has subsequently been extracted may have initiated the causative processes of FRS. The development of white bands or Mees’ lines on the finger- or toenails and raised cholesterol levels may also occur in response to recent exposure to heavy metals and these may also act as clues to help point you in the right direction. Hal Huggins claims that the vast majority of his patients report relief of allergies, bloating, migraine, digestive and urinary tract problems and fatigue with removal of their amalgam fillings according to his protocols.